Abstract
Background
Previous mobile health (mHealth) studies have revealed significant links between depression and circadian rhythm features measured via wearables. However, the comprehensive impact of seasonal variations was not fully considered in these studies, potentially biasing interpretations in real-world settings.
Objective
This study aims to explore the associations between depression severity and wearable-measured circadian rhythms while accounting for seasonal impacts.
Methods
Data were sourced from a large longitudinal mHealth study, wherein participants’ depression severity was assessed biweekly using the 8-item Patient Health Questionnaire (PHQ-8), and participants’ behaviors, including sleep, step count, and heart rate (HR), were tracked via Fitbit devices for up to 2 years. We extracted 12 circadian rhythm features from the 14-day Fitbit data preceding each PHQ-8 assessment, including cosinor variables, such as HR peak timing (HR acrophase), and nonparametric features, such as the onset of the most active continuous 10-hour period (M10 onset). To investigate the association between depression severity and circadian rhythms while also assessing the seasonal impacts, we used three nested linear mixed-effects models for each circadian rhythm feature: (1) incorporating the PHQ-8 score as an independent variable, (2) adding seasonality, and (3) adding an interaction term between season and the PHQ-8 score.
Results
Analyzing 10,018 PHQ-8 records alongside Fitbit data from 543 participants (n=414, 76.2% female; median age 48, IQR 32-58 years), we found that after adjusting for seasonal effects, higher PHQ-8 scores were associated with reduced daily steps (β=–93.61, P<.001), increased sleep variability (β=0.96, P<.001), and delayed circadian rhythms (ie, sleep onset: β=0.55, P=.001; sleep offset: β=1.12, P<.001; M10 onset: β=0.73, P=.003; HR acrophase: β=0.71, P=.001). Notably, the negative association with daily steps was more pronounced in spring (β of PHQ-8 × spring = –31.51, P=.002) and summer (β of PHQ-8 × summer = –42.61, P<.001) compared with winter. Additionally, the significant correlation with delayed M10 onset was observed solely in summer (β of PHQ-8 × summer = 1.06, P=.008). Moreover, compared with winter, participants experienced a shorter sleep duration by 16.6 minutes, an increase in daily steps by 394.5, a delay in M10 onset by 20.5 minutes, and a delay in HR peak time by 67.9 minutes during summer.
Conclusions
Our findings highlight significant seasonal influences on human circadian rhythms and their associations with depression, underscoring the importance of considering seasonal variations in mHealth research for real-world applications. This study also indicates the potential of wearable-measured circadian rhythms as digital biomarkers for depression.
Keywords: circadian rhythm, biological rhythms, mental health, major depressive disorder, MDD, wearable, mHealth, mobile health, digital health, monitoring
Introduction
Depression is a globally prevalent mental disorder with various negative impacts, including reduced quality of life, disability, premature mortality, and an increased risk of suicide [1-6]. However, current depression diagnostic methods face several critical limitations: (1) reliance on individuals’ subjective recall of past behaviors, which introduces recall bias and neglects day-to-day fluctuations [7,8]; (2) dependence on skilled and experienced clinicians [9,10]; and (3) evaluations often delayed until the mental health issues have progressed to a more severe, difficult-to-treat stage [11]. Consequently, these limitations result in the underdiagnosis and delayed treatment for those with depression [12,13], underscoring the critical need for objective and timely methods for early detection.
Previous research has found significant links between circadian rhythms and depression [14,15]. Circadian rhythms are approximately 24-hour endogenous oscillations, controlled by the master clock in the suprachiasmatic nucleus of the hypothalamus, that regulate many aspects of human behavior and physiology, such as sleep-wake cycles, hormone secretion, and body temperature [16-18]. Disturbances in circadian rhythms have been associated with an increased risk of both physical and mental diseases [15,19-21]. Therefore, tracking human circadian rhythms is a potential objective method for early-stage depression identification. Traditional methods for circadian rhythm assessment involve tracking melatonin in bodily fluids (such as saliva, urine, or blood samples) in a constant light environment to prevent external light from altering melatonin production and biasing the assessment of the circadian phase [22,23]. However, this traditional approach is expensive, labor-intensive, and impractical for large cohort studies and long-term monitoring in real-world settings [24,25].
With the development of ubiquitous sensors and mobile technologies, wearable devices provide a convenient and cost-effective way to continuously monitor individuals’ daily behaviors and physiological signals in real-world settings [26]. Previous mobile health (mHealth) studies have explored the approximation of human circadian rhythms through wearable-measured patterns, including sleep-wake cycles, rest-activity patterns, and circadian rhythms in heart rate (HR) [24,27-32]. Higher depression severity has been found to be associated with later sleep onset and offset times, higher sleep variability, lower amplitude of activity, lower intradaily stability, and later acrophase of activity and HR [24,27-32].
However, previous mHealth studies have not fully accounted for seasonal variations, possibly due to their short study durations. Seasonal changes in sunlight and temperature are crucial environmental zeitgebers for the internal circadian clock, impacting human circadian rhythms [33-35]. Prior research has reported significant seasonal effects on sleep patterns and activity levels [36-39]. Ignoring these seasonal impacts may introduce bias into the associations between depression and wearable-measured circadian rhythms in real-world settings. Thus, examining the effects of seasonality on wearable-measured circadian rhythms and their connections to depression in a comprehensive longitudinal data set is needed.
The primary aim of this study was to explore the associations between depression severity and wearable-measured circadian rhythms, accounting for seasonal effects and investigating potential variations across seasons. Our secondary aim was to quantify the seasonal changes in wearable-measured circadian rhythms within a European mHealth study for depression [40].
Methods
Data Set
Participants and Settings
The data analyzed in this study were sourced from the Remote Assessment of Disease and Relapse Major Depressive Disorder (RADAR-MDD) research program, which aimed to investigate the utility of remote technologies for monitoring depression and understanding factors that could help predict relapse in MDD [40]. A total of 623 participants were recruited from 3 study sites across 3 European countries (United Kingdom, Spain, and the Netherlands) and followed for up to 2 years [41]. The first participant was enrolled in November 2017 and the last participant was enrolled in June 2020, and the data collection was completed in April 2021. Due to this rolling enrollment process, participants’ involvement in the study varied from 11 months to 24 months [41]. The RADAR-MDD program used the RADAR-base open-source platform to concurrently gather both active (eg, questionnaires) and passive (eg, wearable) data [42]. Comprehensive details of the study protocol and data set have been documented in publications [40] and [41], respectively.
Patient Involvement
The RADAR-MDD protocol was co-developed with a patient advisory board who shared their opinions on several user-facing aspects of the study including the choice and frequency of survey measures, the usability of the study app, participant-facing documents, selection of optimal participation incentives, selection and deployment of wearable devices, and the data analysis plan.
Ethical Considerations
Ethical approvals were obtained from the Camberwell St. Giles Research Ethics Committee (17/LO/1154) in the United Kingdom, the Fundacio Sant Joan de Deu Clinical Research Ethics Committee (CI: PIC-128-17) in Spain, and the Medische Ethische Toetsingscommissie VUmc (2018.012- NL63557.029.17) in the Netherlands. All participants provided their written informed consent. Before the data collection, participants were assured of their privacy protection, informed of their right to withdraw at any time without needing to justify their decision, and allowed to request the deletion of all their collected data. The data from participants were pseudonymized and stored in a research database, adhering to the General Data Protection Regulation. Participants were compensated with £15 (US $19.09)/€20 (US $21.68) for enrollment, £5 (US $6.36)/€10 (US $10.84) for each clinical assessment conducted every 3 months, and an additional £10 (US $12.73)/€10 (US $10.84) for each qualitative interview they completed. No participant is identifiable in any images in the manuscript or the supplementary materials. Further details can be found in the study protocol and data description papers [40,41].
Measures
Depression Symptom Severity
Participants’ depression symptom severity was measured using the 8-item Patient Health Questionnaire (PHQ-8) [43] conducted via mobile phones every 2 weeks. The PHQ-8 comprises 8 questions, and the total score of PHQ-8 ranges from 0 to 24, indicating increasing severity [43].
Fitbit Data
Participants were asked to wear a Fitbit Charge 2/3 wrist-worn device throughout the whole study. Participants’ sleep, step count, and HR were continuously (24/7) measured and recorded.
Sleep data: Fitbit provided sleep labels (“awake,” “light sleep,” “deep sleep,” and “rapid eye movement”) along with the corresponding local clock times every 30 seconds.
Step data: Participants’ accumulated steps were counted every minute.
HR data: Fitbit provided an estimate of HR every 5 seconds, using an embedded photoplethysmography sensor. However, technical issues resulted in the absence of some sample points. To obtain the robust HR trend and align with step data, we calculated the average HR over 1 minute.
Season
The seasonal division used in this study was based on European Union astronomical seasons: spring (March 20 to June 20), summer (June 21 to September 22), autumn (September 23 to December 20), and winter (December 21 to March 19).
Covariates
In accordance with findings from previous studies [44-46], we considered several covariates that could potentially influence participants’ circadian rhythms, including age, gender, and employment status. Because the COVID-19 pandemic and relevant restrictions had some significant impacts on individuals’ behavior [47], we introduced a covariate “lockdown” to indicate the presence of a national lockdown. Furthermore, as the experience of seasons can be different across countries, the study site was also considered as a covariate. These covariates were considered in our statistical analysis.
Feature Extraction
PHQ-8 Interval
To link human circadian rhythms with depression severity, we extracted circadian rhythm features from each 14-day PHQ-8 interval—specifically, 14 days of Fitbit data preceding a completed PHQ-8. This feature window aligns with the PHQ-8’s purpose of evaluating depressive symptom severity over the past 2 weeks [43] and is consistent with both the existing literature in the mHealth field [48-50] and our previous studies [51,52]. Figure 1 shows an example of a participant’s processed HR, step, and sleep data in a 14-day PHQ-8 interval.
Figure 1.
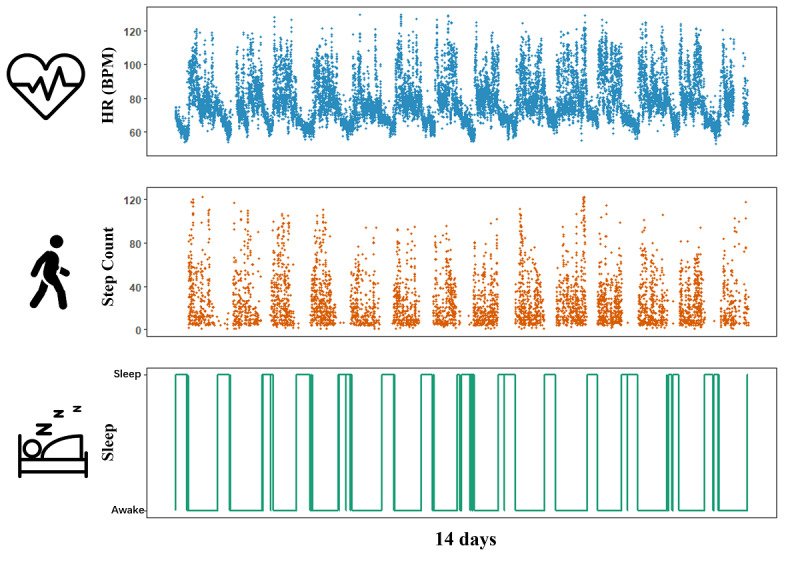
An example of a participant’s processed heart rate (HR), step, and sleep Fitbit data during the preceding 14 days of an 8-item Patient Health Questionnaire assessment collected via the RADAR–base platform.
Data Inclusion Criteria
Some Fitbit data were missing in our data set for several reasons, including device damage, low battery level, and not being worn. Building on insights from our prior research [53], which discussed the sufficient days for stable feature calculation, we focused on 14-day PHQ-8 intervals with at least 8 days having more than 80% of step and HR data and a sleep recording in this study. Considering the potential impact of daylight saving time on individuals’ behaviors [54], we excluded the first 14-day PHQ-8 interval after the time switching [37]. We then extracted a total of 12 features for reflecting the circadian rhythms from sleep, step count, and HR data.
Sleep-Wake Rhythms
Fitbit shows promise in identifying sleep-wake status [55,56]. Therefore, to reflect the sleep-wake rhythms, we computed four features: (1) sleep duration (the mean total sleep time), (2) sleep variability (the SD of total sleep time), (3) sleep onset (the mean clock time of falling asleep), and (4) sleep offset (the mean clock time of wake-up) [51].
Rest-Activity Rhythms
We extracted five nonparametric features from the Fitbit step count recordings to characterize the stability, fragmentation, timing, and mean activity level of participants’ rest-activity rhythms, using the R package nparACT (R Foundation for Statistical Computing) [57,58]. These features include (1) intradaily variability of steps (step IV), quantifying the fragmentation in the rest-activity cycle; (2) interdaily stability of steps (step IS), quantifying the stability of rest-activity patterns over a 14-day PHQ-8 interval; (3) L5 onset, representing the onset of least active continuous 5-hour period; (4) M10 onset, representing the onset of the most active continuous 10-hour period; and (5) daily step, representing the mean of daily total steps in a 14-day PHQ-8 interval [57,58].
Circadian Rhythm in HR
For estimating circadian rhythms in HR, we used cosinor analysis—fitting a cosine wave to time series behavioral data through least-squares regression, which has been widely used in previous mHealth studies [59-61]. Using the R package cosinor, we performed the cosinor analysis on Fitbit HR data of each 14-day PHQ-8 interval and extracted the following parameters: (1) HR MESOR, the midline estimating statistic of the fitted cosine wave for HR; (2) HR amplitude, the difference between the peak value and MESOR of the fitted cosine wave for HR; and (3) HR acrophase, the timing of the HR peak [59-61].
Statistical Analysis
Given the longitudinal nature of our data set, that is, each participant had repeated measurements, we used the linear mixed-effects model [62] with a participant-specific random intercept in this study, implemented using the R package lmerTest. To investigate whether disregarding seasonal effects biases the associations between depression severity and circadian rhythms, we established and compared the following 3 models for each of circadian rhythm features.
Model 1: A linear mixed-effects model was established to regress each circadian rhythm feature with only the PHQ-8 score as the independent variable.
Model 2: Season was included as an independent variable in addition to the PHQ-8 score, considering seasonal effects on the circadian rhythms feature.
Model 3: To further explore potential variations in the association between depression severity and circadian rhythms across seasons, an interaction term between the PHQ-8 score and season was added to the main-effects model (model 2).
All models were adjusted by covariates: age, gender, study site, lockdown, and employment status. The equations of these 3 models are outlined as follows:
Model 1: Circadian rhythm = β1 PHQ‑8 + COVs
Model 2: Circadian rhythm = β1 PHQ‑8 + β2 season + COVs
Model 3: Circadian rhythm = β1 PHQ‑8 + β2 season + β3 PHQ‑8 × season + COVs
where COVs represents all covariates mentioned above and circadian rhythm is one of the wearable-measured circadian rhythm features.
Likelihood ratio tests were then performed to examine whether including more variables (season and the interaction term) can significantly improve the fitting of the regression model. The Benjamini-Hochberg method was used for the correction of multiple comparisons [63]. Despite the inclusion of lockdown as a covariate, we also repeated our analysis on the subset of data before the COVID-19 pandemic (before January 31, 2020).
Results
Data Summary
In accordance with our data inclusion criteria (see the Methods section), we analyzed a total of 10,018 PHQ-8 records alongside corresponding Fitbit data from 543 participants, with an average of 16 recordings per participant. The cohort selected for this study had a median age of 48 (IQR 32-58) years, was predominantly female (n=414, 76.2%), and included 230 (42.4%) employed participants. The distribution of PHQ-8 records was approximately uniform across the seasons, with winter accounting for 26.9%, spring 23.6%, summer 25.5%, and autumn 23.9%. We observed that demographics and data collection varied across study sites, with participants at the CIBER (Centro de Investigación Biomédica en Red) site in Spain being older and more likely to be retired, whereas the King’s College London site in the United Kingdom had the highest number of participants and PHQ-8 records collected. Table 1 summarizes participant demographics and PHQ-8 records for the entire cohort, with site-specific comparisons. Figure 2 visualizes the variations of wearable-measured circadian rhythm features across a year.
Table 1.
A summary of demographics of participants and PHQ-8a questionnaires in the present study, with the site-specific comparisons.b
| Characteristic | Total | CIBERc (Spain) | KCLd (UK) | VUMCe (Netherlands) |
| Participants, n | 543 | 126 | 303 | 114 |
| Age (years), median (IQR) | 48.00 (32.00-58.00) | 53.00 (47.25-60.00) | 44.00 (30.00-56.00) | 39.50 (26.00-57.75) |
| Female, n (%) | 414 (76.2) | 91 (72.2) | 233 (76.9) | 90 (78.9) |
| Employed, n (%) | 230 (42.4) | 30 (23.8) | 164 (54.1) | 36 (31.6) |
| PHQ-8 records, n | 10,018 | 1990 | 5899 | 2129 |
| Records in winter, n (%) | 2699 (26.9) | 541 (27.2) | 1519 (25.8) | 639 (30.0) |
| Records in spring, n (%) | 2363 (23.6) | 450 (22.6) | 1504 (25.5) | 409 (19.2) |
| Records in summer, n (%) | 2559 (25.5) | 520 (26.1) | 1508 (25.6) | 531 (24.9) |
| Records in autumn, n (%) | 2397 (23.9) | 479 (24.1) | 1368 (23.2) | 550 (25.8) |
| Participants before the COVID-19 pandemic, n | 442 | 115 | 259 | 68 |
| Records before the COVID-19 pandemic, n (%) | 4202 (41.9) | 999 (50.2) | 2650 (44.9) | 553 (26.0) |
aPHQ-8: 8-item Patient Health Questionnaire.
bDue to the private issue, participants’ specific geographic information was not collected.
cCIBER: Centro de Investigación Biomédica en Red.
dKCL: King’s College London.
eVUMC: Vrije Universiteit Medisch Centrum.
Figure 2.
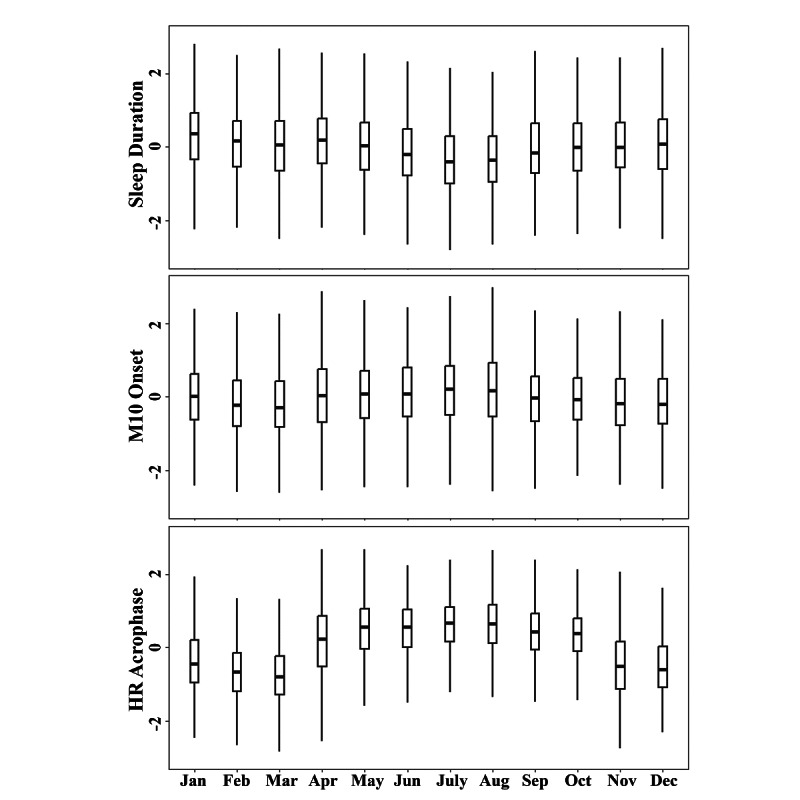
Variations of wearable-measured circadian rhythm features across a year. For each participant, circadian rhythm features were normalized to reduce the individual differences. HR: heart rate.
Associations Between the PHQ-8 score and Wearable-Measured Circadian Rhythm Features
The results of models 1 and 2 are displayed in Table 2. The likelihood ratio tests revealed that incorporating seasonal effects (model 2) significantly improved the model fit for all 12 circadian rhythm features. Specifically, model 2 demonstrated significant positive associations of the PHQ-8 score with several features: sleep duration (β1=0.46, P<.001), sleep onset (β1=0.55, P=.001), sleep offset (β1=1.12, P<.001), sleep variability (β1=0.96, P<.001), L5 onset (β1=0.43, P=.04), M10 onset (β1=0.73, P=.003), and HR acrophase (β1=0.71, P=.001). Conversely, significant negative associations were observed with daily step (β1=–93.61, P<.001), step IS (β1=–0.001, P<.001), HR MESOR (β1=–0.03, P<.001), and HR amplitude (β1=–0.04, P<.001). However, the effect sizes of PHQ-8 on step IS, HR MESOR, and HR amplitude are small, according to their practical meanings.
Table 2.
Effects of PHQ-8a and seasonality on wearable-measured circadian rhythm features estimated by mixed-effects regression models (models 1b and 2c).d
| Feature | Model 1 | Model 2 | Likelihood ratio test (P values) | ||||
|
|
PHQ-8, β1 (SE) | PHQ-8, β1 (SE) | Spring, β2 (SE) | Summer, β2 (SE) | Autumn, β2 (SE) |
|
|
| Sleep duration | 0.51 (0.14)*** | 0.46 (0.14)*** | –6.48 (1.32)*** | –16.63 (1.31)*** | –6.13 (1.31)*** | <.001 | |
| Sleep onset | 0.52 (0.17)** | 0.55 (0.17)** | 3.68 (1.61)* | 7.16 (1.59)*** | –4.64 (1.60)** | <.001 | |
| Sleep offset | 1.13 (0.15)*** | 1.12 (0.15)*** | –0.25 (1.44) | –6.91 (1.43)*** | –8.32 (1.43)*** | <.001 | |
| Sleep variability | 0.97 (0.14)*** | 0.96 (0.14)*** | –8.48 (1.36)*** | –5.29 (1.35)*** | –2.82 (1.35)* | <.001 | |
| Daily step | –94.71 (6.43)*** | –93.61 (6.41)*** | –19.21 (61.28) | 394.46 (60.81)*** | 186.16 (60.75)** | <.001 | |
| Step IVe | 0.001 (0.0006) | 0.0007 (0.0006) | 0.001 (0.006) | –0.026 (0.006)*** | –0.021 (0.006)*** | .006 | |
| Step ISf | –0.001 (0.0002)*** | –0.001 (0.0002)*** | 0.002 (0.002) | –0.006 (0.002)* | 0.004 (0.002) | .007 | |
| L5 onsetg | 0.43 (0.21)* | 0.43 (0.21)* | –1.10 (2.13) | –3.84 (2.12) | –3.98 (2.12) | .002 | |
| M10 onseth | 0.66 (0.25)** | 0.73 (0.25)** | 11.94 (2.45)*** | 20.51 (2.43)*** | 1.61 (2.44) | <.001 | |
| HRi MESORj | –0.03 (0.01)*** | –0.03 (0.01)*** | –0.47 (0.09)*** | –0.01 (0.09) | 0.04 (0.09) | <.001 | |
| HR amplitude | –0.04 (0.01)*** | –0.04 (0.01)*** | 0.19 (0.05)*** | 0.92 (0.05)*** | 0.39 (0.05)*** | <.001 | |
| HR acrophase | 0.51 (0.24)* | 0.71 (0.22)** | 43.35 (2.15)*** | 67.94 (2.13)*** | 24.09 (2.13)*** | <.001 | |
aPHQ-8: 8-item Patient Health Questionnaire.
bModel 1: Circadian rhythm = β1 PHQ‑8 + COVs.
cModel 2: Circadian rhythm = β1 PHQ‑8 + β2 season + COVs, where COVs represents covariates mentioned in the Methods section. Note that winter is the reference season.
dThe exact P values are reported in the main text.
eIV: intradaily variability.
fIS: interdaily stability.
gL5 onset: the onset of least active continuous 5-hour period.
hM10 onset: the onset of the most active continuous 10-hour period.
iHR: heart rate.
jHR MESOR: midline estimating statistic of the fitted cosine wave for heart rate.
*P<.05, **P<.01, ***P<.001.
The results of model 3, along with the likelihood ratio comparison with model 2, are summarized in Table 3. We found that the inclusion of the interaction term between PHQ-8 and seasonality significantly improved the model fit for daily step, step IV, step IS, M10 onset, HR MESOR, and HR amplitude. Notably, the negative association between the PHQ-8 score and daily step exhibited greater strength in spring (β3 of PHQ-8 × spring = –31.51, P=.002) and summer (β3 of PHQ-8 × summer = –42.61, P<.001) than in winter. Additionally, a significant positive association between M10 onset and PHQ-8 was observed exclusively in summer (β3 of PHQ-8 × summer = 1.06, P=.008), with no significant associations observed in other seasons.
Table 3.
Coefficients, SE, and significancea of PHQ-8b, seasonality, and the interaction term between PHQ-8 and seasons in model 3c for the entire data set.
| Feature | PHQ-8, β1 (SE) | Spring, β2 (SE) | Summer, β2 (SE) | Autumn, β2 (SE) | PHQ-8 × spring β3 (SE) | PHQ-8 × summer, β3 (SE) | PHQ-8 × autumn, β3 (SE) | Likelihood ratio test (P values) |
| Sleep duration | 0.49 (0.18)** | –4.55 (2.49) | –16.27 (2.45)*** | –7.2 (2.46)** | –0.20 (0.22) | –0.04 (0.22) | 0.11 (0.21) | .50 |
| Sleep onset | 0.79 (0.22)*** | 4.57 (3.04) | 11.14 (2.98)*** | 0.55 (3) | –0.09 (0.26) | –0.41 (0.26) | –0.53 (0.26)* | .49 |
| Sleep offset | 1.01 (0.20)*** | –2.88 (2.71) | –7.28 (2.67)** | –9.74 (2.68)*** | 0.27 (0.24) | 0.04 (0.23) | 0.15 (0.23) | .53 |
| Sleep variability | 1.23 (0.19)*** | –4.32 (2.56) | 0.19 (2.52) | –1.43 (2.53) | –0.42 (0.22) | –0.57 (0.22)** | –0.14 (0.22) | .26 |
| Daily step | –73.21 (8.55)*** | 289.04 (115.3)* | 804.05 (113.32)*** | 311.21 (113.92)** | –31.51 (10.01)** | –42.61 (9.95)*** | –12.66 (9.87) | <.001 |
| Step IVd | –0.001 (0.0008) | –0.02 (0.01) | –0.06 (0.01)*** | –0.04 (0.01)*** | 0.002 (0.001)* | 0.004 (0.001)*** | 0.002 (0.001) | <.001 |
| Step ISe | –0.001 (0.0003)** | 0.01 (0.005)* | –0.001 (0.004) | 0.005 (0.004) | –0.001 (0.0004)* | –0.001 (0.0004) | –0.0001 (0.0004) | <.001 |
| L5 onsetf | 0.51 (0.29) | –4.11 (4.02) | 1.26 (3.95) | –2.89 (3.98) | 0.31 (0.35) | –0.54 (0.35) | –0.11 (0.34) | .23 |
| M10 onsetg | 0.26 (0.34) | 4.86 (4.63) | 10.33 (4.54)* | –0.44 (4.57) | 0.72 (0.41) | 1.06 (0.40)** | 0.21 (0.40) | .04 |
| HRh MESORi | –0.03 (0.01)* | –0.57 (0.16)*** | 0.05 (0.16) | 0.28 (0.16) | 0.01 (0.01) | –0.01 (0.01) | –0.03 (0.01) | .003 |
| HR amplitude | –0.04 (0.01)*** | 0.36 (0.1)*** | 0.87 (0.1)*** | 0.38 (0.1)*** | –0.02 (0.01)* | 0.01 (0.01) | 0.002 (0.008) | .001 |
| HR acrophase | 0.50 (0.30) | 40.39 (4.05)*** | 62.99 (3.98)*** | 23.3 (4)*** | 0.30 (0.35) | 0.52 (0.35) | 0.08 (0.35) | .75 |
aThe exact P values are reported in the main text.
bPHQ-8: 8-item Patient Health Questionnaire.
cModel 3: Circadian rhythm = β1 PHQ‑8 + β2 season + β3 PHQ‑8 × season + COVs, where COVs represents covariates mentioned in the Methods section. Note that winter is the reference season.
dIV: intradaily variability.
eIS: interdaily stability.
fL5 onset: the onset of least active continuous 5-hour period.
gM10 onset: the onset of the most active continuous 10-hour period.
hHR: heart rate.
iHR MESOR: midline estimating statistic of the fitted cosine wave for heart rate.
*P<.05, **P<.01, ***P<.001.
Seasonal Effects on Wearable-Measured Circadian Rhythm Features
Our results reveal significant seasonal impacts on various circadian rhythms, as indicated by the seasonal coefficients in model 2 (Table 2). Notably, HR acrophase varied significantly across seasons, delayed by 43.4 minutes in spring (P<.001), 67.9 minutes in summer (P<.001), and 24.1 minutes in autumn (P<.001) compared with winter (the reference season).
In terms of rest-activity rhythms, compared with winter, summer was associated with 394.5 more daily steps (P<.001) and 0.03 lower step IV (P<.001), and M10 onset was 20.5 minutes later (P<.001); autumn was associated with 186.2 more daily steps (P=.002) and 0.02 lower step IV (P<.001); and spring was associated M10 onset being 11.9 minutes later (P<.001).
Regarding sleep-wake rhythms, compared with winter, we found that (1) sleep duration decreased by 6.5 minutes in spring (P<.001), 16.6 minutes in summer (P<.001), and 6.1 minutes in autumn (P<.001); (2) sleep onset was 4.6 minutes earlier in autumn (P=.004), 3.7 minutes later in spring (P=0.02), and 7.2 minutes later in summer (P<.001); (3) sleep offset was 6.9 minutes earlier in summer (P<.001) and 8.3 minutes earlier in autumn (P<.001); and (4) sleep variability was 8.5 minutes lower in spring (P<.001), 5.3 minutes lower in summer (P<.001), and 2.8 minutes lower in autumn (P=.04).
Site-to-Site Analysis
Results of our subset analyses across 3 study sites are shown in Tables S1-S3 in Multimedia Appendix 1. Despite a reduction in sample sizes leading to some nonsignificant coefficients, the overall direction of associations between the PHQ-8 and circadian rhythm features remained consistent with the results in the entire data set. Notably, the seasonal changes in sleep-related features and HR acrophase are larger in the Spain site than the sites in the United Kingdom and Netherlands. For instance, during summer compared with winter, participants from the Spain site experienced a significant decrease in sleep duration by 36.6 minutes, whereas participants from the sites in the United Kingdom and Netherlands experienced reductions in sleep duration by 18.9 and 8.5 minutes, respectively. Furthermore, compared with winter, the HR acrophase for participants in Spain was delayed by 123.2 minutes in summer, significantly more than the delays of 58.2 minutes in the UK site and 64.0 minutes in the Netherlands site during summer.
Pre–COVID-19 Subset Analysis
The pre–COVID-19 subset analysis (Table 4) indicated that the directions and significances of associations between depression severity and circadian rhythm features were consistent with results in the entire data set. The seasonal effects on most circadian rhythm features (except for daily step) were similar between the entire data set and the pre–COVID-19 subset. Notably, daily step exhibited larger seasonal fluctuations in the pre–COVID-19 period. Specifically, compared with winter, participants in the pre–COVID-19 subset exhibited 657.2, 1096.4, and 321.6 more daily steps in spring, summer, and autumn, respectively.
Table 4.
Coefficients, SE, and significancea of PHQ-8b, seasonality, and the interaction term between PHQ-8 and seasons in model 3c for the pre-COVID subset.
| Feature | PHQ-8, β1 (SE) | Spring, β2 (SE) | Summer, β2 (SE) | Autumn, β2 (SE) | PHQ-8 × spring, β3 (SE) | PHQ-8 × summer, β3 (SE) | PHQ-8 × autumn, β3 (SE) |
| Sleep duration | 0.97 (0.26)*** | –3.01 (3.99) | –14.86 (3.67)*** | –6.88 (3.45)* | –0.01 (0.34) | –0.05 (0.31) | 0.11 (0.29) |
| Sleep onset | 0.87 (0.36)* | –2.1 (5.46) | 9.84 (5.02) | 0.58 (4.73) | –0.25 (0.46) | –0.51 (0.43) | –0.64 (0.39) |
| Sleep offset | 1.43 (0.31)*** | –6.17 (4.65) | –7.6 (4.27) | –10.04 (4.03)* | –0.24 (0.39) | –0.22 (0.36) | 0.07 (0.34) |
| Sleep variability | 1.47 (0.26)*** | 1.94 (4.09) | 2.29 (3.76) | 0.62 (3.55) | –0.76 (0.35)* | –0.89 (0.32)** | –0.33 (0.3) |
| Daily step | –71.62 (12.05)*** | 657.17 (179.07)*** | 1096.36 (164.67)*** | 321.63 (155.06)* | –20.45 (15.21) | –48.65 (13.99)*** | 1.49 (12.91) |
| Step IVd | –0.001 (0.001) | –0.04 (0.02)* | –0.03 (0.02) | –0.01 (0.02) | 0.004 (0.002)* | 0.003 (0.001)* | 0.0007 (0.0013) |
| Step ISe | –0.0003 (0.0005) | –0.004 (0.0072) | 0.0021 (0.0066) | 0.0035 (0.0063) | –0.0003 (0.0006) | –0.0007 (0.0006) | –0.0002 (0.0005) |
| L5 onsetf | 0.57 (0.45) | –17.84 (7.16)* | –6.74 (6.58) | –2.26 (6.22) | 0.4 (0.61) | –0.2 (0.56) | –0.17 (0.52) |
| M10 onsetg | 0.09 (0.51) | –7.37 (7.89) | 4.83 (7.25) | 1.28 (6.84) | 1.14 (0.67) | 1.22 (0.62)* | 0.07 (0.57) |
| HRh MESORi | –0.08 (0.02)*** | –0.4 (0.27) | –0.53 (0.25)* | –0.38 (0.23) | 0.01 (0.02) | 0.04 (0.02)* | 0.04 (0.02)* |
| HR amplitude | –0.05 (0.01)*** | 0.31 (0.17) | 0.58 (0.15)*** | 0.07 (0.14) | –0.01 (0.01) | 0.02 (0.01) | 0.02 (0.01) |
| HR acrophase | 0.52 (0.38) | 35.11 (5.77)*** | 68.14 (5.3)*** | 22.2 (5.0)*** | 1.15 (0.49)* | 0.26 (0.45) | 0.19 (0.42) |
aThe exact P values are reported in the main text.
bPHQ-8: 8-item Patient Health Questionnaire.
cModel 3: Circadian rhythm = β1 PHQ‑8 + β2 season + β3 PHQ‑8 × season + COVs, where COVs represents covariates mentioned in the Methods section.
dIV: intradaily variability.
eIS: interdaily stability.
fL5 onset: the onset of least active continuous 5-hour period.
gM10 onset: the onset of the most active continuous 10-hour period.
hHR: heart rate.
iHR MESOR: midline estimating statistic of the fitted cosine wave for heart rate.
*P<.05, **P<.01, ***P<.001.
Discussion
Primary Findings
Our study, derived from a large European longitudinal mHealth study focused on depression, revealed significant seasonal effects on wearable-measured circadian rhythms and their associations with depression.
One of our key findings is that the associations between depression severity and certain wearable-measured circadian rhythms varied across different seasons. Specifically, we found a stronger negative association between depression and daily step count during the warmer seasons of spring and summer compared with winter. Additionally, a significant positive association was identified between depression severity and the onset of the most active continuous 10-hour period exclusively in summer. This may be attributed to the more favorable weather conditions for outdoor activities in summer [64], which could increase the observable relationship between rest-activity rhythms and depression. Furthermore, we found that the inclusion of seasonal effects can significantly improve the model fit for all wearable-measured circadian rhythms. These findings highlight the critical importance of including seasonal effects in longitudinal mHealth studies.
On adjusting for seasonal effects, we found that higher depression severity was significantly associated with lower levels of physical activity (daily step), more irregular activities (sleep variability and step IS), and later circadian rhythm timings (sleep onset and offset, M10 onset, and HR acrophase). These relationships are consistent with prior research. The linkage between reduced physical activity levels and worsened depression severity was reported in both survey-based and mHealth studies [65,66]. The preventive and therapeutic roles of physical activity against depression have been well-documented [67,68]. Moreover, there is extensive evidence linking depression with more irregular daily behaviors, including increased sleep variability [51,69-71], less stable rest-activity rhythms [72], and irregular patterns in Bluetooth [52] and GPS [73] data. The delayed circadian rhythm timings have been found to be associated with higher depression severity in multiple data streams, such as sleep recordings [51,69-71], activity logs [61], and HR recordings [74]. These consistent findings highlight the close associations between circadian rhythms and depression severity.
This study also revealed significant seasonal impacts on circadian rhythms, most notably between summer and winter. The cohort demonstrated shorter and later sleep patterns, increased daily step counts, reduced intradaily step variability, and delayed circadian rhythm timings during summer compared with winter. Especially, the circadian phase (HR acrophase) was delayed by 67.9 minutes in summer. These findings mostly align with previous laboratory and survey-based studies, which suggested that people tend to sleep longer in winter, possibly due to the effects of light exposure on melatonin production [75-78]. Previous studies have similarly observed higher activity levels [36,38,39], lower intradaily variability [79,80], and delayed hormone secretion rhythm [81,82] in summer compared with winter, further supporting our findings.
Conducted on a large cohort over an extended period using 3 wearable data modalities, this study aligned with some previous survey and laboratory findings, highlighting the precision of mobile technology in tracking behavioral rhythms. Our findings suggest that wearable-measured circadian rhythms have the potential to be digital biomarkers for depression detection. Furthermore, this study could inform the future design of seasonal, context-sensitive mHealth interventions, such as tailored activity recommendations and light exposure therapy.
Limitations
This study has several limitations that may impact its findings and interpretations. First, the presence of missing data may introduce bias, as our previous study indicated data compliance is associated with depression severity and other personal traits (eg, age) [83]. Second, the specificity of our cohort, characterized by a history of depression and a predominantly female composition, may limit the generalizability of our findings, highlighting the need for validation in more general populations. Third, while we accounted for national lockdowns as a covariate in the regression models and conducted analysis on the pre–COVID-19 subset, the complexities and varied impacts of COVID-19 necessitate additional validations in the postpandemic data sets. Fourth, our study relied on PHQ-8 scores as depression labels, which may introduce subjective biases.
Lastly, while we adjusted for study sites (in different countries) as a covariate in our regression models and conducted the site-to-site analyses, the influence of geographical location on circadian rhythms and their relationship is still needed to be explored in future research, ideally through the randomized controlled trials.
Conclusions
Our analysis of longitudinal wearable data from a large cohort reveals the significant seasonal impact on circadian rhythms and their associations with depression, emphasizing the importance of accounting for seasonal variations in longitudinal mHealth research. Additionally, we found that wearable-measured circadian rhythms are significantly linked to depression severity, indicating their potential to be digital biomarkers for depression detection. These findings enrich our understanding of the mechanisms and pathology underlying depression and could inform the future design of mental health monitoring and interventions.
Acknowledgments
The Remote Assessment of Disease and Relapse–Central Nervous System (RADAR-CNS) project has received funding from the Innovative Medicines Initiative (IMI) 2 Joint Undertaking under grant agreement No. 115902. This Joint Undertaking receives support from the European Union’s Horizon 2020 Research and Innovation Program and the European Federation of Pharmaceutical Industries and Associations (EFPIA). This communication reflects the views of the RADAR-CNS consortium, and neither IMI nor the European Union and EFPIA are liable for any use that may be made of the information contained herein. The funding bodies have not been involved in the design of the study, the collection or analysis of data, or the interpretation of data. This study represents independent research partly funded by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre (BRC) at South London, and Maudsley National Health Service (NHS) Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. We thank all the members of the RADAR-CNS patient advisory board for their contribution to the device selection procedures, and their invaluable advice throughout the study protocol design. This research was reviewed by a team with experience of mental health problems and their careers, who have been specially trained to advise on research proposals and documentation through Feasibility and Acceptability Support Team for Researchers (FAST-R), a free, confidential service in England provided by the NIHR Maudsley BRC via King’s College London and South London and Maudsley NHS Foundation Trust. We thank all GLAD Study volunteers for their participation and gratefully acknowledge the NIHR BioResource, NIHR BioResource centers, NHS Trusts, and staff for their contribution. We also acknowledge NIHR BRC, King’s College London, South London and Maudsley NHS Trust, and King’s Health Partners. We thank the NIHR, NHS Blood and Transplant, and Health Data Research UK as part of the Digital Innovation Hub Program. Participants in the CIBER site came from the following 4 clinical communities in Spain: Parc Sanitari Sant Joan de Déu Network services, Institut Català de la Salut, Institut Pere Mata, and Hospital Clínico San Carlos. Participant recruitment in Amsterdam was partially accomplished through Hersenonderzoek.nl, a Dutch online registry that facilitates participant recruitment for neuroscience studies. Hersenonderzoek.nl is funded by ZonMwMemorabel (project No. 73305095003), a project in the context of the Dutch Deltaplan Dementie, Gieskes-Strijbis Foundation, the Alzheimer’s Society in the Netherlands, and Brain Foundation Netherlands. RJBD is supported by the following: (1) NIHR BRC at South London and Maudsley NHS Foundation Trust and King’s College London; (2) Health Data Research UK, which is funded by the UK Medical Research Council (MRC), Engineering and Physical Sciences Research Council (EP/Y035216/1), Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation, and Wellcome Trust; (3) the BigData@Heart Consortium, funded by the IMI 2 Joint Undertaking (which receives support from the European Union’s Horizon 2020 research and innovation program and EFPIA, partnering with 20 academic and industry partners and European Society of Cardiology); (4) the NIHR University College London Hospitals BRC; (5) the NIHR BRC at South London and Maudsley (related to attendance at the American Medical Informatics Association) NHS Foundation Trust, and King’s College London; (6) the UK Research and Innovation (UKRI) London Medical Imaging & Artificial Intelligence Centre for Value Based Healthcare (AI4VBH); and (7) the NIHR Applied Research Collaboration (ARC) South London at King’s College Hospital NHS Foundation Trust.
Abbreviations
- BRC
Biomedical Research Centre
- EFPIA
European Federation of Pharmaceutical Industries and Associations
- HR
heart rate
- IMI
Innovative Medicines Initiative
- mHealth
mobile health
- MRC
Medical Research Council
- NHS
National Health Service
- NIHR
National Institute for Health Research
- PHQ-8
8-item Patient Health Questionnaire
- RADAR-MDD
Remote Assessment of Disease and Relapse Major Depressive Disorder
Results of the subset analyses across 3 study sites.
Footnotes
Conflicts of Interest: SV is an employee of Janssen Research and Development LLC. VAN was employed by Janssen Research and Development LLC during this study. PA was employed by the pharmaceutical company H. Lundbeck A/S during this study. DCM has accepted honoraria and consulting fees from Apple Inc, Otsuka Pharmaceuticals, Pear Therapeutics, and the One Mind Foundation; received royalties from Oxford Press; and an ownership interest in Adaptive Health Inc. MH is the principal investigator of the Remote Assessment of Disease and Relapse–Central Nervous System project, a private public precompetitive consortium that receives funding from Janssen, UCB, Lundbeck, MSD, and Biogen. CO is supported by the UK Medical Research Council (MR/N013700/1) and King’s College London, member of the MRC Doctoral Training Partnership in Biomedical Sciences. AAS holds shares in Alphabet, owner of FitBit devices. All other authors declare no competing interests.
References
- 1.Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJL, Vos T, Whiteford HA. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547. doi: 10.1371/journal.pmed.1001547. https://dx.plos.org/10.1371/journal.pmed.1001547 .PMEDICINE-D-13-01260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Depression and other common mental disorders: global health estimates. WHO: World Health Organization; 2017. [Google Scholar]
- 3.Lenox-Smith A, Macdonald MTB, Reed C, Tylee A, Peveler R, Quail D, Wildgust HJ. Quality of life in depressed patients in UK primary care: the FINDER study. Neurol Ther. 2013;2(1-2):25–42. doi: 10.1007/s40120-013-0006-1. https://europepmc.org/abstract/MED/26000214 .6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lerner D, Adler DA, Chang H, Berndt ER, Irish JT, Lapitsky L, Hood MY, Reed J, Rogers WH. The clinical and occupational correlates of work productivity loss among employed patients with depression. J Occup Environ Med. 2004;46(6 Suppl):S46–S55. doi: 10.1097/01.jom.0000126684.82825.0a. https://europepmc.org/abstract/MED/15194895 .00043764-200406001-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of "subthreshold" depressive symptoms. J Abnorm Psychol. 2000;109(2):345–351. [PubMed] [Google Scholar]
- 6.Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17–28. doi: 10.1016/j.jad.2013.01.004.S0165-0327(13)00036-0 [DOI] [PubMed] [Google Scholar]
- 7.Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211–217. doi: 10.2147/JMDH.S104807. https://europepmc.org/abstract/MED/27217764 .jmdh-9-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Devaux M, Sassi F. Social disparities in hazardous alcohol use: self-report bias may lead to incorrect estimates. Eur J Public Health. 2016;26(1):129–134. doi: 10.1093/eurpub/ckv190. https://europepmc.org/abstract/MED/26585784 .ckv190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells KB, Hays RD, Burnam MA, Rogers W, Greenfield S, Ware JE. Detection of depressive disorder for patients receiving prepaid or fee-for-service care. Results from the Medical Outcomes Study. JAMA. 1989;262(23):3298–3302. [PubMed] [Google Scholar]
- 10.Schulberg HC, Saul M, McClelland M, Ganguli M, Christy W, Frank R. Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry. 1985;42(12):1164–1170. doi: 10.1001/archpsyc.1985.01790350038008. [DOI] [PubMed] [Google Scholar]
- 11.Ben-Zeev D, Scherer EA, Wang R, Xie H, Campbell AT. Next-generation psychiatric assessment: using smartphone sensors to monitor behavior and mental health. Psychiatr Rehabil J. 2015;38(3):218–226. doi: 10.1037/prj0000130. https://europepmc.org/abstract/MED/25844912 .2015-14736-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatr Serv. 2004;55(12):1379–1385. doi: 10.1176/appi.ps.55.12.1379.55/12/1379 [DOI] [PubMed] [Google Scholar]
- 13.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55.yoa20071 [DOI] [PubMed] [Google Scholar]
- 14.Carpenter JS, Crouse JJ, Scott EM, Naismith SL, Wilson C, Scott J, Merikangas KR, Hickie IB. Circadian depression: a mood disorder phenotype. Neurosci Biobehav Rev. 2021;126:79–101. doi: 10.1016/j.neubiorev.2021.02.045.S0149-7634(21)00107-X [DOI] [PubMed] [Google Scholar]
- 15.Crouse JJ, Carpenter JS, Song YJC, Hockey SJ, Naismith SL, Grunstein RR, Scott EM, Merikangas KR, Scott J, Hickie IB. Circadian rhythm sleep-wake disturbances and depression in young people: implications for prevention and early intervention. Lancet Psychiatry. 2021;8(9):813–823. doi: 10.1016/S2215-0366(21)00034-1.S2215-0366(21)00034-1 [DOI] [PubMed] [Google Scholar]
- 16.Partch CL, Green CB, Takahashi JS. Molecular architecture of the mammalian circadian clock. Trends Cell Biol. 2014;24(2):90–99. doi: 10.1016/j.tcb.2013.07.002. https://europepmc.org/abstract/MED/23916625 .S0962-8924(13)00113-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster RG, Kreitzman L. The rhythms of life: what your body clock means to you! Exp Physiol. 2013;99(4):599–606. doi: 10.1113/expphysiol.2012.071118. [DOI] [PubMed] [Google Scholar]
- 18.Refinetti R. Circadian rhythmicity of body temperature and metabolism. Temperature (Austin) 2020;7(4):321–362. doi: 10.1080/23328940.2020.1743605. https://europepmc.org/abstract/MED/33251281 .1743605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, Rosner B, Stampfer MJ, Schernhammer ES. Association between rotating night shift work and risk of coronary heart disease among women. JAMA. 2016;315(16):1726–1734. doi: 10.1001/jama.2016.4454. https://europepmc.org/abstract/MED/27115377 .2516715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knutsson A, Kempe A. Shift work and diabetes--a systematic review. Chronobiol Int. 2014;31(10):1146–1151. doi: 10.3109/07420528.2014.957308. [DOI] [PubMed] [Google Scholar]
- 21.Musiek ES, Bhimasani M, Zangrilli MA, Morris JC, Holtzman DM, Ju YES. Circadian rest-activity pattern changes in aging and preclinical Alzheimer disease. JAMA Neurol. 2018;75(5):582–590. doi: 10.1001/jamaneurol.2017.4719. https://europepmc.org/abstract/MED/29379963 .2670749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duffy JF, Dijk DJ. Getting through to circadian oscillators: why use constant routines? J Biol Rhythms. 2002;17(1):4–13. doi: 10.1177/074873002129002294. [DOI] [PubMed] [Google Scholar]
- 23.Keijzer H, Smits MG, Duffy JF, Curfs LMG. Why the dim light melatonin onset (DLMO) should be measured before treatment of patients with circadian rhythm sleep disorders. Sleep Med Rev. 2014;18(4):333–339. doi: 10.1016/j.smrv.2013.12.001.S1087-0792(13)00113-5 [DOI] [PubMed] [Google Scholar]
- 24.Bowman C, Huang Y, Walch OJ, Fang Y, Frank E, Tyler J, Mayer C, Stockbridge C, Goldstein C, Sen S, Forger DB. A method for characterizing daily physiology from widely used wearables. Cell Rep Methods. 2021;1(4):100058. doi: 10.1016/j.crmeth.2021.100058. https://europepmc.org/abstract/MED/34568865 .100058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cui S, Lin Q, Gui Y, Zhang Y, Lu H, Zhao H, Wang X, Li X, Jiang F. CARE as a wearable derived feature linking circadian amplitude to human cognitive functions. NPJ Digit Med. 2023;6(1):123. doi: 10.1038/s41746-023-00865-0. doi: 10.1038/s41746-023-00865-0.10.1038/s41746-023-00865-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zapata-Lamana R, Lalanza JF, Losilla JM, Parrado E, Capdevila L. mHealth technology for ecological momentary assessment in physical activity research: a systematic review. PeerJ. 2020;8:e8848. doi: 10.7717/peerj.8848. https://europepmc.org/abstract/MED/32257648 .8848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smagula SF, Krafty RT, Thayer JF, Buysse DJ, Hall MH. Rest-activity rhythm profiles associated with manic-hypomanic and depressive symptoms. J Psychiatr Res. 2018;102:238–244. doi: 10.1016/j.jpsychires.2018.04.015. https://europepmc.org/abstract/MED/29705489 .S0022-3956(17)31005-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White KH, Rumble ME, Benca RM. Sex differences in the relationship between depressive symptoms and actigraphic assessments of sleep and rest-activity rhythms in a population-based sample. Psychosom Med. 2017;79(4):479–484. doi: 10.1097/PSY.0000000000000434. https://europepmc.org/abstract/MED/27922568 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slyepchenko A, Allega OR, Leng X, Minuzzi L, Eltayebani MM, Skelly M, Sassi RB, Soares CN, Kennedy SH, Frey BN. Association of functioning and quality of life with objective and subjective measures of sleep and biological rhythms in major depressive and bipolar disorder. Aust N Z J Psychiatry. 2019;53(7):683–696. doi: 10.1177/0004867419829228. [DOI] [PubMed] [Google Scholar]
- 30.Robillard R, Hermens DF, Naismith SL, White D, Rogers NL, Ip TKC, Mullin SJ, Alvares GA, Guastella AJ, Smith KL, Rong Y, Whitwell B, Southan J, Glozier N, Scott EM, Hickie IB. Ambulatory sleep-wake patterns and variability in young people with emerging mental disorders. J Psychiatry Neurosc. 2015;40(1):28–37. doi: 10.1503/jpn.130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carr O, Saunders KEA, Bilderbeck AC, Tsanas A, Palmius N, Geddes JR, Foster R, De Vos M, Goodwin GM. Desynchronization of diurnal rhythms in bipolar disorder and borderline personality disorder. Transl Psychiatry. 2018;8(1):79. doi: 10.1038/s41398-018-0125-7. doi: 10.1038/s41398-018-0125-7.10.1038/s41398-018-0125-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ávila Moraes C, Cambras T, Diez-Noguera A, Schimitt R, Dantas G, Levandovski R, Hidalgo MP. A new chronobiological approach to discriminate between acute and chronic depression using peripheral temperature, rest-activity, and light exposure parameters. BMC Psychiatry. 2013;13:77. doi: 10.1186/1471-244X-13-77. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-13-77 .1471-244X-13-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wright KP, McHill AW, Birks BR, Griffin BR, Rusterholz T, Chinoy ED. Entrainment of the human circadian clock to the natural light-dark cycle. Curr Biol. 2013;23(16):1554–1558. doi: 10.1016/j.cub.2013.06.039. https://linkinghub.elsevier.com/retrieve/pii/S0960-9822(13)00764-1 .S0960-9822(13)00764-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khalsa SBS, Jewett ME, Cajochen C, Czeisler CA. A phase response curve to single bright light pulses in human subjects. J Physiol. 2003;549(3):945–952. doi: 10.1113/jphysiol.2003.040477. doi: 10.1113/jphysiol.2003.040477.2003.040477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Minors DS, Waterhouse JM, Wirz-Justice A. A human phase-response curve to light. Neurosci Lett. 1991;133(1):36–40. doi: 10.1016/0304-3940(91)90051-t.0304-3940(91)90051-T [DOI] [PubMed] [Google Scholar]
- 36.Tucker P, Gilliland J. The effect of season and weather on physical activity: a systematic review. Public Health. 2007;121(12):909–922. doi: 10.1016/j.puhe.2007.04.009.S0033-3506(07)00140-0 [DOI] [PubMed] [Google Scholar]
- 37.Mattingly SM, Grover T, Martinez GJ, Aledavood T, Robles-Granda P, Nies K, Striegel A, Mark G. The effects of seasons and weather on sleep patterns measured through longitudinal multimodal sensing. NPJ Digit Med. 2021;4(1):76. doi: 10.1038/s41746-021-00435-2. doi: 10.1038/s41746-021-00435-2.10.1038/s41746-021-00435-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamilton SL, Clemes SA, Griffiths PL. UK adults exhibit higher step counts in summer compared to winter months. Ann Hum Biol. 2008;35(2):154–169. doi: 10.1080/03014460801908058.791850521 [DOI] [PubMed] [Google Scholar]
- 39.Clemes SA, Hamilton SL, Griffiths PL. Summer to winter variability in the step counts of normal weight and overweight adults living in the UK. J Phys Act Health. 2011;8(1):36–44. doi: 10.1123/jpah.8.1.36. [DOI] [PubMed] [Google Scholar]
- 40.Matcham F, Barattieri di San Pietro C, Bulgari V, de Girolamo G, Dobson R, Eriksson H, Folarin AA, Haro JM, Kerz M, Lamers F, Li Q, Manyakov NV, Mohr DC, Myin-Germeys I, Narayan V, BWJH P, Ranjan Y, Rashid Z, Rintala A, Siddi S, Simblett SK, Wykes T, Hotopf M. Remote assessment of disease and relapse in major depressive disorder (RADAR-MDD): a multi-centre prospective cohort study protocol. BMC Psychiatry. 2019;19(1):1–11. doi: 10.1186/s12888-019-2049-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matcham F, Leightley D, Siddi S, Lamers F, White KM, Annas P, de Girolamo G, Difrancesco S, Haro JM, Horsfall M, Ivan A, Lavelle G, Li Q, Lombardini F, Mohr DC, Narayan VA, Oetzmann C, Penninx BWJH, Bruce S, Nica R, Simblett SK, Wykes T, Brasen JC, Myin-Germeys I, Rintala A, Conde P, Dobson RJB, Folarin AA, Stewart C, Ranjan Y, Rashid Z, Cummins N, Manyakov NV, Vairavan S, Hotopf M, RADAR-CNS consortium Remote Assessment of Disease and Relapse in Major Depressive Disorder (RADAR-MDD): recruitment, retention, and data availability in a longitudinal remote measurement study. BMC Psychiatry. 2022;22(1):136. doi: 10.1186/s12888-022-03753-1. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-022-03753-1 .10.1186/s12888-022-03753-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ranjan Y, Rashid Z, Stewart C, Conde P, Begale M, Verbeeck D, Boettcher S, Hyve. Dobson R, Folarin A, RADAR-CNS Consortium RADAR-Base: open source mobile health platform for collecting, monitoring, and analyzing data using sensors, wearables, and mobile devices. JMIR Mhealth Uhealth. 2019;7(8):e11734. doi: 10.2196/11734. https://mhealth.jmir.org/2019/8/e11734/ v7i8e11734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163–173. doi: 10.1016/j.jad.2008.06.026.S0165-0327(08)00282-6 [DOI] [PubMed] [Google Scholar]
- 44.Huang YL, Liu RY, Wang QS, Van Someren EJW, Xu H, Zhou JN. Age-associated difference in circadian sleep-wake and rest-activity rhythms. Physiol Behav. 2002;76(4-5):597–603. doi: 10.1016/s0031-9384(02)00733-3.S0031938402007333 [DOI] [PubMed] [Google Scholar]
- 45.Duffy JF, Cain SW, Chang AM, Phillips AJK, Münch MY, Gronfier C, Wyatt JK, Dijk DJ, Wright KP, Czeisler CA. Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc Natl Acad Sci USA. 2011;108 Suppl 3(Suppl 3):15602–15608. doi: 10.1073/pnas.1010666108. https://europepmc.org/abstract/MED/21536890 .1010666108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones SH, Hare DJ, Evershed K. Actigraphic assessment of circadian activity and sleep patterns in bipolar disorder. Bipolar Disord. 2005;7(2):176–186. doi: 10.1111/j.1399-5618.2005.00187.x.BDI187 [DOI] [PubMed] [Google Scholar]
- 47.Sun S, Folarin AA, Ranjan Y, Rashid Z, Conde P, Stewart C, Cummins N, Matcham F, Dalla Costa G, Simblett S, Leocani L, Lamers F, Sørensen PS, Buron M, Zabalza A, Guerrero Pérez AI, Penninx BW, Siddi S, Haro JM, Myin-Germeys I, Rintala A, Wykes T, Narayan VA, Comi G, Hotopf M, Dobson RJ, RADAR-CNS Consortium Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J Med Internet Res. 2020;22(9):e19992. doi: 10.2196/19992. https://www.jmir.org/2020/9/e19992/ v22i9e19992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saeb S, Zhang M, Karr CJ, Schueller SM, Corden ME, Kording KP, Mohr DC. Mobile phone sensor correlates of depressive symptom severity in daily-life behavior: an exploratory study. J Med Internet Res. 2015;17(7):e175. doi: 10.2196/jmir.4273. https://www.jmir.org/2015/7/e175/ v17i7e175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saeb S, Lattie EG, Schueller SM, Kording KP, Mohr DC. The relationship between mobile phone location sensor data and depressive symptom severity. PeerJ. 2016;4:e2537. doi: 10.7717/peerj.2537. https://europepmc.org/abstract/MED/28344895 .2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Farhan AA, Yue C, Morillo R, Ware S, Lu J, Bi J, Kamath J, Russell A, LLC S, Wang B. Behavior vs. introspection: refining prediction of clinical depression via smartphone sensing data. 2016 IEEE Wireless Health (WH); October 25-27 2016; Bethesda, MD, USA. IEEE; 2016. [DOI] [Google Scholar]
- 51.Zhang Y, Folarin AA, Sun S, Cummins N, Bendayan R, Ranjan Y, Rashid Z, Conde P, Stewart C, Laiou P, Matcham F, White KM, Lamers F, Siddi S, Simblett S, Myin-Germeys I, Rintala A, Wykes T, Haro JM, Penninx BW, Narayan VA, Hotopf M, Dobson RJ, RADAR-CNS Consortium Relationship between major depression symptom severity and sleep collected using a wristband wearable device: multicenter longitudinal observational study. JMIR Mhealth Uhealth. 2021;9(4):e24604. doi: 10.2196/24604. https://mhealth.jmir.org/2021/4/e24604/ v9i4e24604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang Y, Folarin AA, Sun S, Cummins N, Ranjan Y, Rashid Z, Conde P, Stewart C, Laiou P, Matcham F, Oetzmann C, Lamers F, Siddi S, Simblett S, Rintala A, Mohr DC, Myin-Germeys I, Wykes T, Haro JM, Penninx BWJH, Narayan VA, Annas P, Hotopf M, Dobson RJB. Predicting depressive symptom severity through individuals' nearby Bluetooth device count data collected by mobile phones: preliminary longitudinal study. JMIR Mhealth Uhealth. 2021;9(7):e29840. doi: 10.2196/29840. https://mhealth.jmir.org/2021/7/e29840/ v9i7e29840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sun S, Folarin AA, Zhang Y, Cummins N, Garcia-Dias R, Stewart C, Ranjan Y, Rashid Z, Conde P, Laiou P, Sankesara H, Matcham F, Leightley D, White KM, Oetzmann C, Ivan A, Lamers F, Siddi S, Simblett S, Nica R, Rintala A, Mohr DC, Myin-Germeys I, Wykes T, Haro JM, Penninx BWJH, Vairavan S, Narayan VA, Annas P, Hotopf M, Dobson RJB, RADAR-CNS Consortium Challenges in using mHealth data from smartphones and wearable devices to predict depression symptom severity: retrospective analysis. J Med Internet Res. 2023;25:e45233. doi: 10.2196/45233. https://www.jmir.org/2023//e45233/ v25i1e45233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harrison Y. The impact of daylight saving time on sleep and related behaviours. Sleep Med Rev. 2013;17(4):285–292. doi: 10.1016/j.smrv.2012.10.001.S1087-0792(12)00114-1 [DOI] [PubMed] [Google Scholar]
- 55.de Zambotti M, Goldstone A, Claudatos S, Colrain IM, Baker FC. A validation study of Fitbit Charge 2™ compared with polysomnography in adults. Chronobiol Int. 2017;35(4):465–476. doi: 10.1080/07420528.2017.1413578. [DOI] [PubMed] [Google Scholar]
- 56.Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Accuracy of Wristband Fitbit Models in Assessing Sleep: Systematic Review and Meta-Analysis. J Med Internet Res. 2019;21(11):e16273. doi: 10.2196/16273. https://www.jmir.org/2019/11/e16273/ v21i11e16273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van Someren EJ, Hagebeuk EE, Lijzenga C, Scheltens P, de Rooij SE, Jonker C, Pot AM, Mirmiran M, Swaab DF. Circadian rest-activity rhythm disturbances in Alzheimer's disease. Biol Psychiatry. 1996;40(4):259–270. doi: 10.1016/0006-3223(95)00370-3.0006-3223(95)00370-3 [DOI] [PubMed] [Google Scholar]
- 58.Van Someren EJW, Swaab DF, Colenda CC, Cohen W, McCall WV, Rosenquist PB. Bright light therapy: improved sensitivity to its effects on rest-activity rhythms in Alzheimer patients by application of nonparametric methods. Chronobiol Int. 1999;16(4):505–518. doi: 10.3109/07420529908998724. [DOI] [PubMed] [Google Scholar]
- 59.Cornelissen G. Cosinor-based rhythmometry. Theor Biol Med Model. 2014;11:16. doi: 10.1186/1742-4682-11-16. https://tbiomed.biomedcentral.com/articles/10.1186/1742-4682-11-16 .1742-4682-11-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ali FZ, Parsey RV, Lin S, Schwartz J, DeLorenzo C. Circadian rhythm biomarker from wearable device data is related to concurrent antidepressant treatment response. NPJ Digit Med. 2023;6(1):81. doi: 10.1038/s41746-023-00827-6. doi: 10.1038/s41746-023-00827-6.10.1038/s41746-023-00827-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Esaki Y, Obayashi K, Saeki K, Fujita K, Iwata N, Kitajima T. Association between circadian activity rhythms and mood episode relapse in bipolar disorder: a 12-month prospective cohort study. Transl Psychiatry. 2021;11(1):525. doi: 10.1038/s41398-021-01652-9. doi: 10.1038/s41398-021-01652-9.10.1038/s41398-021-01652-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38(4):963–974. [PubMed] [Google Scholar]
- 63.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57(1):289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 64.Chen L, Ng E. Outdoor thermal comfort and outdoor activities: a review of research in the past decade. Cities. 2012;29(2):118–125. doi: 10.1016/j.cities.2011.08.006. [DOI] [Google Scholar]
- 65.Melo MCA, Daher EDF, Albuquerque SGC, de Bruin VMS. Exercise in bipolar patients: a systematic review. J Affect Disord. 2016 Jul 01;198:32–8. doi: 10.1016/j.jad.2016.03.004.S0165-0327(15)31406-3 [DOI] [PubMed] [Google Scholar]
- 66.Melo MCA, Garcia RF, de Araújo Carolina Freitas Cardeal, Rangel DM, de Bruin PFC, de Bruin VMS. Physical activity as prognostic factor for bipolar disorder: an 18-month prospective study. J Affect Disord. 2019 May 15;251:100–106. doi: 10.1016/j.jad.2019.03.061.S0165-0327(18)33062-3 [DOI] [PubMed] [Google Scholar]
- 67.Harvey SB, Øverland S, Hatch SL, Wessely S, Mykletun A, Hotopf M. Exercise and the prevention of depression: results of the HUNT Cohort Study. Am J Psychiatry. 2018;175(1):28–36. doi: 10.1176/appi.ajp.2017.16111223. [DOI] [PubMed] [Google Scholar]
- 68.Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE. Exercise for depression. Cochrane Database Syst Rev. 2013;2013(9):CD004366. doi: 10.1002/14651858.CD004366.pub6. https://europepmc.org/abstract/MED/24026850 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fang Y, Forger DB, Frank E, Sen S, Goldstein C. Day-to-day variability in sleep parameters and depression risk: a prospective cohort study of training physicians. NPJ Digit Med. 2021 Feb 18;4(1):28. doi: 10.1038/s41746-021-00400-z.10.1038/s41746-021-00400-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ghandeharioun A, Fedor S, Sangermano L, Ionescu D, Alpert J, Dale C, Sontag D, Picard R. Objective assessment of depressive symptoms with machine learning and wearable sensors data. International Conference on Affective Computing and Intelligent Interaction and Workshops, ACII; October 23-26, 2017; San Antonio, TX. 2017. [DOI] [Google Scholar]
- 71.Matcham F, Carr E, Meyer N, White KM. Wearable-derived sleep features predict relapse in major depressive disorder. ResearchGate. 2023. Mar, [2024-05-22]. https://www.researchgate.net/publication/369514383_Wearable-derived_sleep_features_predict_relapse_in_Major_Depressive_Disorder .
- 72.Luik AI, Zuurbier LA, Direk N, Hofman A, Van Someren EJ, Tiemeier H. 24-hour activity rhythm and sleep disturbances in depression and anxiety: a population-based study of middle-aged and older persons. Depress Anxiety. 2015;32(9):684–692. doi: 10.1002/da.22355. [DOI] [PubMed] [Google Scholar]
- 73.Zhang Y, Folarin AA, Sun S, Cummins N, Vairavan S, Bendayan R, Ranjan Y, Rashid Z, Conde P, Stewart C, Laiou P, Sankesara H, Matcham F, White KM, Oetzmann C, Ivan A, Lamers F, Siddi S, Vilella E, Simblett S, Rintala A, Bruce S, Mohr DC, Myin-Germeys I, Wykes T, Haro JM, Penninx BW, Narayan VA, Annas P, Hotopf M, Dobson RJ, RADAR-CNS consortium Longitudinal relationships between depressive symptom severity and phone-measured mobility: dynamic structural equation modeling study. JMIR Ment Health. 2022;9(3):e34898. doi: 10.2196/34898. https://mental.jmir.org/2022/3/e34898/ v9i3e34898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Otsuka K, Mitsutake G, Yano S. Depression, quality of life, and lifestyle: chronoecological health watch in a community. Biomed Pharmacother. 2002;56 Suppl 2:231s–242s. doi: 10.1016/s0753-3322(02)00297-4.S0753-3322(02)00297-4 [DOI] [PubMed] [Google Scholar]
- 75.Monsivais D, Ghosh A, Bhattacharya K, Dunbar RIM, Kaski K. Tracking urban human activity from mobile phone calling patterns. PLoS Comput Biol. 2017;13(11):e1005824. doi: 10.1371/journal.pcbi.1005824. https://dx.plos.org/10.1371/journal.pcbi.1005824 .PCOMPBIOL-D-17-00216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.de la Iglesia HO, Fernández-Duque E, Golombek DA, Lanza N, Duffy JF, Czeisler CA, Valeggia CR. Access to electric light is associated with shorter sleep duration in a Traditionally Hunter-Gatherer Community. J Biol Rhythms. 2015;30(4):342–350. doi: 10.1177/0748730415590702. https://europepmc.org/abstract/MED/26092820 .0748730415590702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yetish G, Kaplan H, Gurven M, Wood B, Pontzer H, Manger PR, Wilson C, McGregor R, Siegel JM. Natural sleep and its seasonal variations in three pre-industrial societies. Curr Biol. 2015;25(21):2862–2868. doi: 10.1016/j.cub.2015.09.046. https://linkinghub.elsevier.com/retrieve/pii/S0960-9822(15)01157-4 .S0960-9822(15)01157-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cepeda M, Koolhaas CM, van Rooij FJA, Tiemeier H, Guxens M, Franco OH, Schoufour JD. Seasonality of physical activity, sedentary behavior, and sleep in a middle-aged and elderly population: The Rotterdam study. Maturitas. 2018;110:41–50. doi: 10.1016/j.maturitas.2018.01.016.S0378-5122(17)31047-2 [DOI] [PubMed] [Google Scholar]
- 79.Kume Y, Makabe S, Singha-Dong N, Vajamun P, Apikomonkon H, Griffiths J. Seasonal effects on the sleep-wake cycle, the rest-activity rhythm and quality of life for Japanese and Thai older people. Chronobiol Int. 2017;34(10):1377–1387. doi: 10.1080/07420528.2017.1372468. [DOI] [PubMed] [Google Scholar]
- 80.Smagula SF, DuPont CM, Miller MA, Krafty RT, Hasler BP, Franzen PL, Roecklein KA. Rest-activity rhythms characteristics and seasonal changes in seasonal affective disorder. Chronobiol Int. 2018;35(11):1553–1559. doi: 10.1080/07420528.2018.1496094. https://europepmc.org/abstract/MED/30024782 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kanikowska D, Roszak M, Rutkowski R, Sato M, Sikorska D, Orzechowska Z, Bręborowicz A, Witowski J. Seasonal differences in rhythmicity of salivary cortisol in healthy adults. J Appl Physiol (1985) 2019;126(3):764–770. doi: 10.1152/japplphysiol.00972.2018. https://journals.physiology.org/doi/10.1152/japplphysiol.00972.2018?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PubMed] [Google Scholar]
- 82.Hadlow NC, Brown S, Wardrop R, Henley D. The effects of season, daylight saving and time of sunrise on serum cortisol in a large population. Chronobiol Int. 2013;31(2):243–251. doi: 10.3109/07420528.2013.844162. [DOI] [PubMed] [Google Scholar]
- 83.Zhang Y, Pratap A, Folarin AA, Sun S, Cummins N, Matcham F, Vairavan S, Dineley J, Ranjan Y, Rashid Z, Conde P, Stewart C, White KM, Oetzmann C, Ivan A, Lamers F, Siddi S, Rambla CH, Simblett S, Nica R, Mohr DC, Myin-Germeys I, Wykes T, Haro JM, Penninx BWJH, Annas P, Narayan VA, Hotopf M, Dobson RJB, RADAR-CNS consortium Long-term participant retention and engagement patterns in an app and wearable-based multinational remote digital depression study. NPJ Digit Med. 2023;6(1):25. doi: 10.1038/s41746-023-00749-3. doi: 10.1038/s41746-023-00749-3.10.1038/s41746-023-00749-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results of the subset analyses across 3 study sites.


