The health effects of climate change will affect vulnerable low income populations first, and this review provides convincing evidence of the public health importance of monitoring hotspots of climate change and health
Is climate change a serious threat to health? According to the most recent international assessments it unquestionably is, although its impact depends on where you live, your age, access to health care, and your public health infrastructure.1–4 Arguably, climate change is one of the largest environmental and health equity challenges of our times; wealthy energy consuming nations are most responsible for the emissions that cause global warming, yet poor countries are most at risk. In a globalised world, however, the health of populations in rich countries is affected as a result of international travel, trade, and human migration. Mapping “hotspots” of ecological risk has proved to be a useful construct for prioritising and focusing resources to stem the threat of losing biodiversity. Similarly, identifying hotspots in climate change and human health may help public health practitioners in anticipating and preventing any additional burden of disease.
Summary box
Health effects from climate change will stem from altered temperatures, extremes of precipitation (floods and droughts), air pollution, and infectious diseases
Although risk may be low compared with current acute health crises, the attributable burden of such a widespread global phenomenon may be quite high
Any region or population with concurrent environmental or socioeconomic stresses will be at risk
Long term disease surveillance must be maintained or established in suspected hotspots of climate change and health risks to enhance detection and prevention of disease
Climate change represents one of the greatest environmental and health equity challenges of our times; wealthy energy consuming nations are most responsible for global warming, yet poor countries are at most risk
Clinicians should recognise these changing risks and can serve as role models for responsible citizens living in societies consuming natural resources at an unsustainable level
Methods
We reviewed major findings from reports published by the United Nations Intergovernmental Panel on Climate Change (IPCC), the National Research Council, the World Health Organization, and the UN Environment Programme.1–4
Identifying vulnerable regions
The UN Intergovernmental Panel on Climate Change in its assessment considered which areas or populations are vulnerable to the health impacts of climate change:
Areas or populations in or bordering on regions with high endemicity of diseases that are sensitive to climate (for example, malaria)
Areas with an observed association between epidemic disease and extremes of weather (for example, epidemics linked to the El Niño weather pattern)
Areas at risk from several climate impacts relevant to health (for example, stress on food and water supplies, risk of coastal flooding)
Areas at risk from concurrent environmental or socioeconomic stresses and with little capacity to adapt (for example, local stresses from practices in the use of land or impoverished or undeveloped health infrastructure)
According to the UN Intergovernmental Panel on Climate Change, the vulnerability of human populations and natural systems to climate change will vary greatly across regions. Changes in seasonal river flows, increases in floods and droughts, decreased food security, and loss of biodiversity especially are of concern for parts of Africa, Latin America, and Asia. Particularly vulnerable regions include delta regions, low lying small island states, and many arid regions where drought and availability of water are problematic even without climate change.1
We performed a qualitative comparison of the conditions resulting from climate change and its environmental impacts across the above four reports. For each of these reports and extensive review of the literature had been conducted, and conclusions arose from an expert judgment process and peer review. Having participated in three of four of these assessments, we identified categories of risk conditions and geographical hotspots to guide monitoring for potential change in diseases related to climate.
Recent and projected climate change
According to the UN Intergovernmental Panel on Climate Change, evidence of recent warming is building. Since the late 1950s, the global average surface temperature has increased by 0.6oC, snow cover and ice extent have diminished; during the past century, the sea level has risen on average by 10-20 cm and the temperature of the oceans has increased.5 Mid-range estimates for future climate change are 3°C global mean warming and a rise in the sea level of 45 cm by 2100. Increased variability in the hydrological cycle (more floods and droughts) is expected to accompany global warming. The rate of change in climate is faster now than in any other period in the past thousand years.5
Although climate warming and changes in precipitation are expected to affect higher latitudes disproportionately, hotspots in health and climate change will occur where human populations are already at risk from climate extremes (such as drought induced famine or flooding) and lack adequate health infrastructure. Such vulnerable hotspots may therefore not necessarily coincide with areas that are experiencing the greatest change in climate. For any given vulnerable region, adverse health effects will generally occur in poor populations that have little capacity to adapt, predominantly in the tropics and subtropics.
Impacts of climate change will occur in the context of other environmental and socioeconomic pressures. For example, heavy precipitation can more readily cause dangerous flooding in areas denuded of forests. Localised warming can be intensified in sprawling cities through the “urban heat island” effect. The impact of increases in extreme rainfalls will be exacerbated by impervious road surfaces and inadequate drainage, making cities more prone to flooding. Impacts on food resources will compound current overharvesting of fisheries and intensive animal production.
Mapping hotspots of climate change and health
The strategy of mapping hotspots has been used by conservationists to choose locations to which to apply limited resources so that the world's biodiversity is best preserved.6 Impacts do, however, occur at the local level, and identifying vulnerable regions or countries does not account for diverse regional texture.
Hotspot 1—heat waves or air pollution
This kind of hotspot consists of geographically expanding or sprawling cities, replacing vegetation with surfaces retaining heat. Also cities with poor quality housing that currently experience an urban heat island effect, and cities that have topography that gives rise to stagnant air masses and summer pollution are at risk (for example, Santiago and Mexico City).
Mortality generally increases at both high and low temperatures above and below an optimum temperature value.7 Populations in warmer regions tend to be sensitive to low temperatures, and populations in colder climates are sensitive to heat.8,9 Vulnerability to heatwaves is driven by socioeconomic factors such as poor housing. Cities in developing countries may therefore be more vulnerable to heatwaves, although little research has been done in these countries. Elderly people and people with pre-existing illnesses are disproportionately affected. Mortality is primarily due to cardiovascular, cerebrovascular, and respiratory disease.10 A heatwave in Chicago in 1995 caused 514 heat related deaths (12 per 100 000 population).11 The urban heat island effect, whereby urban areas experience higher and nocturnally sustained temperatures owing to the concentration of heat retaining surfaces (for example, asphalt and tar roofs), can amplify general warming trends.
Increased ambient temperature and altered patterns of wind and air mass can affect chemistry in the atmosphere. Temperature and the formation of ozone at ground level (photochemical urban smog) are related: a strong positive relation with temperatures above 32°C has been observed in some US cities. Ozone can heighten the sensitivity of people with asthma to allergens and contribute to the development of asthma in children.12–14 The impact of climate change on the future frequency of episodes of air pollution during the summer in a given city remain highly uncertain.
Hotspot 2—sea level rise
This type of hotspot consists of settlements on low lying deltas or coral atolls and coastal megacities (such as Cairo, Egypt). After a rise in sea level, widespread flooding, intrusion of salt water, and coastal erosion are expected in low lying coastal settlements. The number of people at risk from flooding by coastal storm surges is projected to increase from the current 75 million to 200 million in a scenario of mid-range climate changes, in which a rise in the sea level of 40 cm is envisaged by the 2080s.1 Countries such as Vietnam, Egypt, Bangladesh, and small island nations would be especially vulnerable.
Coastal communities may experience forced migration of populations.15 Thirteen of the world's 20 current megacities are situated at sea level. Rising seas could result in salination of coastal freshwater aquifers and disrupt stormwater drainage and sewage disposal.16 Nicholls and Leatherman showed that the extreme case of a rise of one metre in the sea level could inundate low lying areas, affecting 18.6 million people in China, 13 million in Bangladesh, 3.5 million in Egypt, and 3.3 million in Indonesia.17 Considering the health burden experienced by refugees and populations subjected to overcrowding, lack of shelter, and competition for resources, the problems presented by displaced populations may turn out to be the largest public health challenge regarding the global health effects of climate change. Conflict may be one of the worst results emerging from such forced migration.
Hotspot 3—flooding
This type of hotspot consists of regions prone to river flooding, such as Central America, Europe, South Asia, and China. Specific watersheds in many countries throughout the world would be affected. Climate change may increase the risk of flooding of rivers. Immediate effects are largely death from drowning and injuries caused by being swept against hard objects.18 Medium term effects include increases in communicable diseases caused by ingestion of contaminated water (for example, cholera or hepatitis A) and contact with flood waters (for example, leptospirosis). Outbreaks of leptospirosis, a bacterial zoonosis, occurred after floods in Nicaragua and Brazil.19–21 In Bangladesh in 1988, watery diarrhoea in a population displaced by floods was the most common cause of death for all age groups under 45, followed by respiratory infection.22 In Bangladesh, settlement of populations in high risk areas such as floodplains and river deltas increases vulnerability.
Heavy rainfall and runoff influences the transport of other microbial and toxic agents from agricultural fields, human septic systems, and toxic dumps. Rainfall can alter the transport and dissemination of microbial pathogens (such as cryptosporidia and giardia), and temperature may affect their survival and growth.23,24
Hotspot 4—drought and malnutrition
This kind of hotspot consists of areas currently experiencing food insecurity and risk of drought, together with a lack of resources to import food (for example southern and eastern Africa, parts of Latin America, and central Asia). The UN Intergovernmental Panel on Climate Change projects a reduction in crop yields in most tropical and subtropical regions caused by mid-continental droughts. Some crops in tropical locations would be decimated because many are already grown in climate conditions near their maximum temperature tolerance. Africa and parts of Latin America are considered to be the most vulnerable regions.
Decreased availability of water as a result of climate change could affect populations in the subtropics where water is already scarce. Currently about a third of the world's population (1.7 billion people) live in water stressed countries, and that number is projected to increase to 5 billion people by 2025.1–4 Decreases in annual average streamflow are anticipated in central Asia and southern Africa, and the food supply may be affected. Politically inflexible regimes can exacerbate climate crises, as may have occurred during the recent severe drought in North Korea.25
Despite technological advances such as improved crop varieties and irrigation systems, agricultural productivity depends largely on weather conditions.26 According to the UN Food and Agriculture Organization (FAO), 790 million people in developing countries are malnourished.27 Nearly half the populations of countries in central, southern, and eastern Africa are already undernourished, and these regions are highly vulnerable. In addition, diarrhoea and diseases such as scabies, conjunctivitis, and trachoma are associated with poor hygiene and result from a breakdown in sanitation if water resources become depleted.16
Hotspot 5—El Niño effects
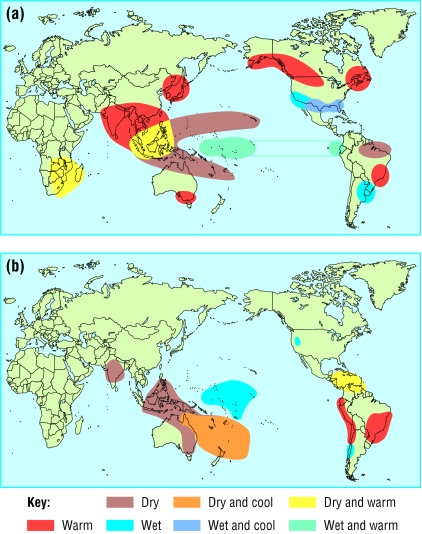
This hotspot consists of regions that experience weather extremes associated with the El Niño weather pattern (for example, Peru and Ecuador for floods; southern Africa, Indonesia, and Malaysia for drought; and some areas for epidemics of infectious disease, such as malaria in Punjab or cholera in Bangladesh). Some evidence shows that stronger or more frequent El Niño events may accompany global warming (fig 1).
Figure 1.
El Niño and warm episodes in December-February (a) and in June-August (b)
Climate change is likely to lead to greater extremes of drying and heavy rainfall and increases the risk of droughts and floods that occur with El Niño in many regions.5 Studies have shown that the El Niño cycle in certain areas is associated with changes in the risk of diseases transmitted by mosquitoes, such as malaria and dengue fever, and diseases caused by arboviruses other than dengue virus.1–4 The risk of malaria in areas in South America, Central Asia, and Africa has been shown to be sensitive to variability in climate driven by El Niño.28 In Peru, more children develop diarrhoeal disease when temperatures are high, and admissions during the El Niño of 1997-8 increased appreciably.29 In Southeast Asia, episodes of hazardous air pollution from fires in Indonesia were related to drought conditions connected with El Niño.30
Hotspot 6—highland malaria
This kind of hotspot consists of areas situated at the fringe of regions where malaria is endemic (for example, East Africa). Vectorborne diseases, such as malaria and dengue fever, are generally more influenced by ambient conditions than are diseases passed directly from human to human. Arthropods—such as mosquitoes, ticks, and fleas—are cold blooded and therefore sensitive to subtle changes in temperature and humidity. Populations of non-human mammalian hosts, such as rodents, are affected by conditions of their habitat and the weather. But temperature is only one of the many factors that determine the dynamics of transmission (see table A on bmj.com).31
International environmental policy and ethical implications
The UN Framework Convention on Climate Change (UNFCCC) is the international legal mechanism under which national governments are responsible for reducing greenhouse gas emissions, with the aim of avoiding, postponing, or reducing the environmental, economic, and social impacts of climate change. The convention was adopted at the earth summit in Rio de Janeiro in 1992, and at its third session in Kyoto in December 1997 governments from developed countries committed themselves to legally binding restrictions on their emissions under the newly established Kyoto protocol. Governments must now resolve many highly contentious political issues, including “supplementarity” (the extent to which rich countries must control domestic emissions rather than paying for controls abroad) and penalties for non-compliance. This year, all 15 member states of the European Union ratified the Kyoto protocol, and it is hoped that other developed countries will follow this lead. Meanwhile, in the United States, California became the first state to link car emissions directly to global warming, under pioneering legislation that could eventually lead to far reaching change across the country.
The way in which climate factors influence the transmission of malaria is more likely to become obvious in environmental fringe areas such as highlands or desert borders. Many of the highland regions in Africa that are surrounded by lowland areas where malaria is endemic are densely populated. Small changes in the distribution of malaria may therefore expose large numbers of people to infection. Some malaria epidemics in the African highlands have been associated with abnormally warm or wet weather conditions.32 The areas of the highlands of Africa that are currently free of malaria therefore represent an ecological zone of special concern, where the distribution of malaria may potentially be affected by climate warming (fig 2).32,33
Figure 2.
Areas vulnerable to malaria in the African highlands33 Reprinted from Patz J, Lindsay S, in: Curr Opin Microbiol 1999;2:445-51, with permission from Elsevier
The way forward
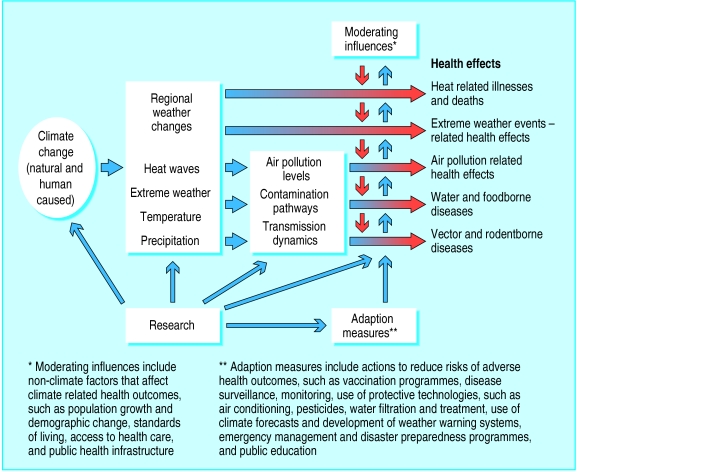
Medical practitioners can consider these hotspots of climate change and health as a guidepost for understanding populations and people at most risk from climate change (fig 3). Doctors' awareness of current health needs in their region is the key to identifying potential health problems that can be exacerbated by more extreme climate variability and long term climate change. Disease monitoring in such hotspots is a priority in order to prevent further health problems.
Additional educational resources
Websites
Program on Health Effects of Global Environmental Change at the Johns Hopkins Bloomberg School of Public Health (www.jhsph.edu/globalchange) links to other recent articles on climate change and health, the full text of the health sector report of the US National Assessment on Climate Variability and Change. In November 2002, a website on this subject will be launched for children (aged 10-14) and their teachers.
United Nations Intergovernmental Panel on Climate Change (www.ipcc.ch). Executive summaries of climate change science, impacts, and adaptation, or mitigation for downloading, complete with excellent key colour figures and tables. Researchers can download data from the general circulation models of global climate.
US Environmental Protection Agency (www.epa.gov/globalresearch/globalhome.html)—general information, assessment, and research tools pertaining to global environmental change.
US Global Change Research Information Office (www.gcrio.org). A guide to an extensive list of sites addressing global change education and research and a good reference site for various uses.
Tiempo Climate Cyperlibrary, The DIY guide to combating global warming (www.cru.uea.ac.uk/tiempo/floor2/educ/diy/diy.htm) shows ways for you and your family to combat global warming.
Textbooks
Aron JL, Patz JA, eds. Ecosystem change and public health: a global perspective. Baltimore: Johns Hopkins University Press, 2001.
McMichael AJ. Human frontiers, environments and disease: past patterns, uncertain futures. New York: Cambridge University Press, 2001.
Journal
Ecology and health. www.ecosystemhealth.com/journal.htm
Figure 3.
Potential health effects of climate variability and change34
Many options for limiting greenhouse gas emissions are available in the short and medium term. Policy makers can encourage energy efficiency and other climate friendly trends in the supply and consumption of energy. Key consumers of energy include industries, homes, offices, vehicles, and farms. Efficiency can be improved in large part by providing an appropriate economic and regulatory framework for consumers and investors. This framework should promote cost effective actions, the best current and future technologies, and “no regrets” solutions (such as reducing urban air pollution while meeting greenhouse gas reduction targets) that make economic and environmental sense irrespective of climate change. As advisers and role models, doctors can change their practices and lifestyles—for example, by commuting by bike rather than car or by installing energy efficient lights in their offices.
Efficiency and equity
The United States contains 5% of the total population of the world yet produces 25% of total annual emissions of greenhouse gas. This discrepancy exemplifies the ethical implications posed by climate change. A country's ability to cope with the impacts of climate change depends on its wealth, technology, and general infrastructure.1 Impoverished populations in the developing world do not have the industry, transportation, or intensive agriculture that cause global warming, yet they have limited capacity to protect themselves against the adverse consequences. In this way, climate change is one of the largest challenges of our times for environmental and health equity. If developing nations do not choose development pathways using more efficient energy technology, the imbalance of “equity” may be lessened—but the global warming problem will be exacerbated greatly.
Supplementary Material
Acknowledgments
We thank Mahmooda Khaliq, Johns Hopkins Bloomberg School of Public Health, for literature review and manuscript preparation.
Footnotes
Funding: JP is part funded by the US Environmental Protection Agency, cooperative agreement CR 827040.
Competing interests: None declared.
An extra table appears on bmj.com
References
- 1.McCarthy J, Canziani O, Leary N, Kokken D, White K. Climate change 2001: impacts, adaptation, and vulnerability. New York: Cambridge University Press; 2001. . (UN Intergovernmental Panel for Climate Change. Third assessment report.) [Google Scholar]
- 2.National Research Council. Under the weather: climate, ecosystems, and infectious disease. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 3.Task Force on Climate and Health. El Niño and health. Geneva: World Health Organization; 1999. [Google Scholar]
- 4.Kovats RS, Campbell-Lendrum D, Reid C, Martens P. Climate and vector-borne disease: An assessment of the role of climate in changing disease patterns. Maastricht: International Centre for Integrative Studies, Maastricht University; 2000. [Google Scholar]
- 5.United Nations Intergovernmental Panel on Climate Change. Contribution of working group I to the third assessment report of the intergovernmental panel on climate change. In: Houghton J, Ding Y, Griggs M, Noguer M, van der Linden P, Dai X, et al., editors. Climate change 2001: the scientific basis. Cambridge and New York: Cambridge University Press; 2001. p. 881. [Google Scholar]
- 6.Myers N, Mittermeier RA, Mittermeier CG, da Fonseca GA, Kent J. Biodiversity hotspots for conservation priorities. Nature. 2000;403:853–858. doi: 10.1038/35002501. [DOI] [PubMed] [Google Scholar]
- 7.Curriero F, Heiner K, Samet J, Zeger S, Strug L, Patz J. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 8.Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet. 1997;349:1341–1346. [PubMed] [Google Scholar]
- 9.Kalkstein LS, Greene JS. An evaluation of climate/mortality relationships in large US cities and possible impacts of a climate change. Environ Health Perspect. 1997;105:2–11. doi: 10.1289/ehp.9710584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kilbourne E. Heatwaves. In: Noji E, editor. The public health consequences of disasters. Oxford and New York: Oxford University Press; 1997. pp. 51–61. [Google Scholar]
- 11.Whitman S, Good G, Donoghue E, Benbow N, Shou W, Mou S. Mortality in Chicago attributed to the July 1995 heat wave. Am J Public Health. 1997;87:1515–1518. doi: 10.2105/ajph.87.9.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koren HS, Bromberg PA. Respiratory responses of asthmatics to ozone. Int Arch Allergy Immunol. 1995;107:236–238. doi: 10.1159/000236989. [DOI] [PubMed] [Google Scholar]
- 13.Koren HS, Utell MJ. Asthma and the environment. Environ Health Perspect. 1997;105:534–537. doi: 10.1289/ehp.97105534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McConnell R, Berhane K, Gilliland F, London S, Islam T, Gauderman W, et al. Asthma in exercising children exposed to ozone: a cohort study. Lancet. 2002;359:386–391. doi: 10.1016/S0140-6736(02)07597-9. [DOI] [PubMed] [Google Scholar]
- 15.Myers N, Kent J. Environmental exodus: an emergent crisis in the global arena. Washington, DC: Climate Institute; 1995. [Google Scholar]
- 16.Patz J. Public health risk assessment linked to climatic and ecological change. Hum Ecolog Risk Assess. 2001;7:1317–1327. [Google Scholar]
- 17.Nicholls R, Leatherman S. Global sea-level rise. In: Strzepek K, Smith J, editors. As climate changes: international impacts and implications. New York: Cambridge University Press; 1995. pp. 92–123. [Google Scholar]
- 18.Malilay J. Floods. In: Noji E, editor. The public health consequences of disasters. New York: Oxford University Press; 1997. [Google Scholar]
- 19.Trevejo RT, Rigau-Perez JG, Ashford DA, McClure EM, Jarquin-Gonzalez C, Amador JJ, et al. Epidemic leptospirosis associated with pulmonary hemorrhage—Nicaragua, 1995. J Infect Dis. 1998;178:1457–1463. doi: 10.1086/314424. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Outbreak of acute febrile illness and pulmonary hemorrhage—Nicaragua, 1995. Morb Mortal Wkly Rep MMWR. 1995;44:841–843. [Google Scholar]
- 21.Ko AI, Galvao Reis M, Ribeiro Dourado CM, Johnson WD, Jr, Riley LW. Urban epidemic of severe leptospirosis in Brazil. Salvador Leptospirosis Study Group. Lancet. 1999;354:820–825. doi: 10.1016/s0140-6736(99)80012-9. [DOI] [PubMed] [Google Scholar]
- 22.Siddique A, Baqui A, Eusof A, Zaman K. 1988 floods in Bangladesh: pattern of illness and cause of death. J Diarrhoeal Dis Res. 1991;9:310–314. [PubMed] [Google Scholar]
- 23.Rose J, Epstein P, Lipp E, Sherman B, Bernard S, Patz J. Climate variability and change in the united states: potential impacts on water and foodborne diseases caused by microbiologic agents. Environ Health Perspect. 2001;109(suppl 2):211–221. doi: 10.1289/ehp.01109s2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Curriero F, Patz J, Rose J, Lele S. The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948-1994. Am J Public Health. 2001;91:1194–1199. doi: 10.2105/ajph.91.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woodward A, Hales S, Litidamu N, Phillips D, Martin J. Protecting human health in a changing world: the role of social and economic development. Bull World Health Organ. 2000;78:1148–1155. [PMC free article] [PubMed] [Google Scholar]
- 26.McMichael A, Githeko A, Akhtar R, Carcavallo R, Gubler D, Haines A, et al. Human Health. In: McCarthy J, Canziani O, Leary N, Dokken D, White K, editors. Climate change 2001: impacts, adaptation, and vulnerability. New York: Cambridge University Press; 2001. [Google Scholar]
- 27.United Nations Food and Agriculture Organization. The state of food insecurity in the world 1999. Rome: FAO; 1999. [Google Scholar]
- 28.Bouma MJ, Poveda G, Rojas W, Chavasse D, Quinones M, Cox J, et al. Predicting high-risk years for malaria in Colombia using parameters of El Niño southern oscillation. Trop Med Int Health. 1997;2:1122–1127. doi: 10.1046/j.1365-3156.1997.d01-210.x. [DOI] [PubMed] [Google Scholar]
- 29.Checkley W, Epstein LD, Gilman RH, Figueroa D, Cama RI, Patz JA, et al. Effect of El Nino and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355:442–450. doi: 10.1016/s0140-6736(00)82010-3. [DOI] [PubMed] [Google Scholar]
- 30.Patz J, Engelberg D, Last J. The effects of changing weather on public health. Ann Rev Public Health. 2000;21:271–307. doi: 10.1146/annurev.publhealth.21.1.271. [DOI] [PubMed] [Google Scholar]
- 31.Gubler D, Reiter P, Ebi K, Yap W, Nasci R, Patz J. Climate variability and change in the United States: potential impacts on vector and rodent-borne diseases. Environ Health Perspect. 2001;109(suppl 2):223–243. doi: 10.1289/ehp.109-1240669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cox J, Craig MH, Le Seuer D, Sharp B. Mapping malaria risk in the highlands of Africa. Durban, South Africa/London: MARA/London School of Hygiene and Tropical Medicine; 1999. . (MARA/HIMAL Technical Report.) [Google Scholar]
- 33.Patz J, Lindsay S. New challenges, new tools: the impact of climate change on infectious diseases commentary. Curr Opin Microbiol. 1999;2:445–451. doi: 10.1016/s1369-5274(99)80078-2. [DOI] [PubMed] [Google Scholar]
- 34.Patz JA, McGeehin MA, Bernard SM, Ebi KL, Epstein PR, Grambsch A, et al. The potential health impacts of climate variability and change for the United States: executive summary of the report of the health sector of the US national assessment. Environ Health Perspect. 2000;108:367–376. doi: 10.1289/ehp.00108367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.