In the United Kingdom, infection with Haemophilus influenzae type b has considerably declined since the introduction of the conjugated H influenza type b vaccine in 1992, although isolated vaccine failures do occur. In countries without routine immunisation against the disease, it continues to be a major cause of morbidity and mortality. We report on three children who presented over a three month period with epiglottitis due to H influenzae type b infection. Each child had been fully immunised.
Case reports
Case 1—A 4 year old boy presented to the emergency department with a 12 hour history of fever and drowsiness, and later drooling and soft stridor. Three days previously he had visited his doctor for red inflamed ears. No antibiotics were prescribed. He had a history of glue ear and campylobacter gastroenteritis. On examination he was feverish (39.3°C) and had stridor and tachycardia. An x ray film of the neck showed swelling of the epiglottis; subsequent difficult intubation in theatre revealed a large cherry red epiglottis. He remained intubated for 36 hours and required a 20 ml/kg bolus of fluid. Blood cultures and a throat swab grew H influenzae type b. Intravenous cefotaxime was continued for 10 days, and he made an uneventful recovery. The table shows the results of blood tests performed during the acute and convalescent stages of the illness.
Case 2—A 2 year old girl was referred by her doctor with a short history of dyspnoea, tachypnoea, and stridor. On examination she was distressed, feverish (38.6°C), and pale. Her heart rate was 160/min and oxygen saturation 88% in air. Nebulised adrenaline was given, with no relief, and lateral radiography of the neck showed swelling of the epiglottis. She required intubation for 48 hours and was treated with cefotaxime for 7 days. Her recovery was uneventful. Blood cultures grew H influenzae type b. The table shows the results of blood tests performed 24 hours and 5 weeks after presentation.
Case 3—A 3 year old girl was referred by her doctor with fever and cough for four hours, stridor, and drooling for two hours. Her temperature was 40.5°C, pulse rate 160/min, respiratory rate 40/min, and oxygen saturation 95% in air. Her neck was extended, and she had dyspnoea. Nebulised budesonide and adrenaline had no effect, and she required intubation for 72 hours. Blood cultures and a throat swab grew H influenzae type b. She received intravenous cefotaxime for seven days. The table shows the results of other blood tests.
Discussion
Haemophilus influenzae type b is a cause of meningitis, epiglottitis, pneumonia, and septic arthritis. Before the introduction of the conjugate vaccine, it was a major cause of disease in early childhood.1 Epiglottitis is life threatening but is rare because of immunisation.
A prospective study over 6.5 years of invasive H influenzae type b in the United Kingdom was carried out to assess the efficacy of the vaccine and to monitor failures.2 Immunisation coverage exceeded 90%, and the incidence of disease declined by more than 95%. Of those 4 368 200 children immunised against H influenzae type b over the study period, 112 developed H influenzae type b, 96 of whom had been fully immunised. Overall vaccine effectiveness was 98%, giving an annual incidence of 0.7 for every 100 000 children immunised (95% confidence interval 0.6 to 0.9). Vaccine protection remained high in the children until 6 years of age. Nevertheless, cases of epiglottitis due to H influenzae continue to be reported.3,4
Epiglottitis is mainly seen in children aged 2-5 years. Typically there is a short history of fever, stridor, and dyspnoea.5 In contrast with children with acute laryngotracheobronchitis (croup), children with epiglottitis are often systemically unwell and may drool and extend their neck but have minimal cough.
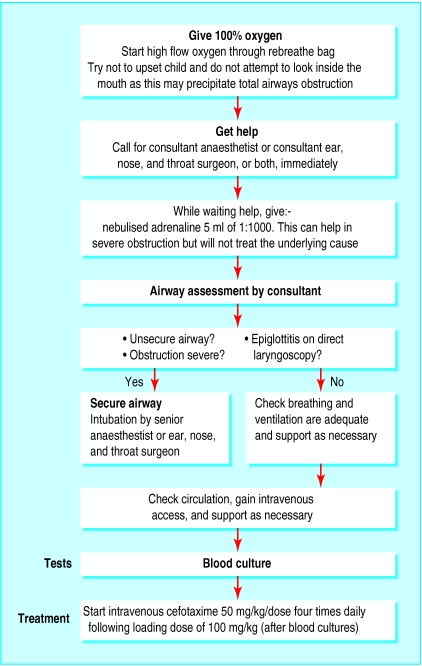
Radiography of the neck is justified only if the diagnosis is in doubt, providing the child is stable and in a safe environment.6 Performing radiography in the lateral position might precipitate a respiratory arrest from complete airway obstruction, especially if the child's neck is repositioned for optimum results. If epiglottitis is suspected, emergency intubation should be performed (figure).7
The ability to mount an immune response to a vaccine is vital for protection against the disease. The negligible antibody response in case 3 represented failure of the vaccine (table). Cases 1 and 2 were more difficult to explain because the antibody titre to H influenzae type b was in the protective range. However, a study of children in whom the H influenzae type b vaccine had failed showed that a subpopulation of children may have had vaccine induced or naturally induced serum anticapsular antibody, which is suboptimally protective against H influenzae type b.8
These three cases represented true failures of the vaccine—the vaccine should have protected them against the strain of bacterium that was identified. This cluster of H influenzae type b epiglottitis within a three month period is unusual, especially as our centre has had no cases since 1993. The children were unrelated and from widely different areas. None had identified risk factors for vaccine failure such as prematurity, malignancy, or neutropenia.9
The success of the H influenzae type b vaccine is attributed to protection from T cell memory and high vaccine uptake, which increases herd immunity. Herd immunity is the generation of a sufficiently large pool of immune people, thereby reducing the transmission of wild disease. With high herd immunity, colonisation and transmission of disease should decrease, benefiting the unvaccinated, partially vaccinated, and those in whom the vaccine is not immunogenic. It could be that herd immunity has declined with an increase in carriage rates, but there is currently no evidence for this. The protective effect of reduced carriage provided by the catch-up campaign in 3-4 year olds (now aged 11-12 years) would by now have waned. The question that arises is whether herd immunity has decreased, rendering people increasingly susceptible at a time when antibody levels are declining.
The British Paediatric Surveillance Unit has evidence of an increased incidence of true vaccine failures in 1999 and 2000, in all age groups. The year of presentation was the only consistent feature, suggesting increased exposure.10 A fourth vaccine against H influenzae type b is routine in the United States, Canada, and Iceland. A study evaluating long term vaccine protection found a minimal decline in clinical protection, suggesting that a booster dose was not essential.2 However, if true vaccine failures and carriage rates increase over the next few years, then a booster dose may be necessary. There is ongoing case ascertainment by the Oxford Vaccine Group.
Table.
Blood test results in three fully immunised children with epiglottitis due to Haemophilus influenzae type b
| Component
|
Normal range
|
Case 1
|
Case 2
|
Case 3
|
|
|---|---|---|---|---|---|
| Immunoglobulins during acute phase of illness (g/l): | |||||
| IgG | 3-15.2 | 8.6 | 7.33 | 7.05 | |
| IgA | 0.3-1.29 | 0.71 | 0.44 | 1.27 | |
| IgM | 0.43-1.9 | 0.63 | 0.57 | 0.59 | |
| IgG1 | 2.3-6.4 | 7.25 | 4.92 | 5.7 | |
| IgG2 | 0.7-4.5 | 1.06 | 2.17 | 1.09 | |
| IgG3 | 0.1-1.1 | 0.5 | 0.39 | 0.53 | |
| IgG4 | 0.0-0.8 | 0.54 | 0.18 | 0.19 | |
| Complement: | |||||
| CH100 | Normal | Normal | Normal | ||
| AP100 | Normal | Normal | Normal | ||
| Specific antibody 24-48 hours after presentation: | |||||
| H influenzae type b (mg/l) | 1.0-20 | 1.6 | >9.0 | <0.1 | |
| Tetanus (IU/ml) | 0.1-10 | 0.05 | Not done* | 0.07 | |
| Pneumococcus (IU/ml) | 20-200 | 9.9 | Not done* | 7.0 | |
| Specific antibody taken 5-6 weeks after presentation: | |||||
| H influenzae | Not applicable | >9 | >9 | <0.1 | |
| Tetanus | 0.05 | 0.85 | 0.07 | ||
| Pneumococcus | 15.2 | Not done* | 7.0 | ||
Full vaccination included meningococcal conjugate vaccine during catch up campaign.
Test not performed or insufficient blood to perform test.
Figure.
Emergency management of suspected acute epiglottitis
Haemophilus influenzae type b epiglottitis still occurs despite immunisation, and requires emergency intubation
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Rosenstein NE, Perkins BA. Update on Haemophilus influenzae serotype b and meningococcal vaccines. Pediatr Clin North Am. 2000;47:337–352. doi: 10.1016/s0031-3955(05)70210-8. [DOI] [PubMed] [Google Scholar]
- 2.Heath PT, Booy R, Azzopardi HJ, Slack MP, Bowen-Morris J, Griffiths H, et al. Antibody concentration and clinical protection after Hib conjugate vaccination in the United Kingdom. JAMA. 2000;284:2334–2340. doi: 10.1001/jama.284.18.2334. [DOI] [PubMed] [Google Scholar]
- 3.Selvadurai H, McIntyre P, Mellis C. Lest we forget acute epiglottitis. J Paediatr Child Health. 1998;34:306–307. [PubMed] [Google Scholar]
- 4.Wagle A, Jones RM. Acute epiglottitis despite vaccination with haemophilus influenzae type B vaccine. Paediatr Anaesth. 1999;9:549–550. doi: 10.1046/j.1460-9592.1999.00428.x. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez Valdepena H, Wald ER, Rose E, Ungkanont K, Casselbrant ML. Epiglottitis and Haemophilus influenzae immunization: the Pittsburgh experience—a five-year review. Pediatrics. 1995;96:424–427. [PubMed] [Google Scholar]
- 6.Butt W, Shann F, Walker C, Williams J, Duncan A, Phelan P. Acute epiglottitis: a different approach to management. Crit Care Med. 1988;16:43–47. [PubMed] [Google Scholar]
- 7.Advanced Life Support Group. Advanced paediatric life support. 3rd ed. London: BMJ Publishing Group; 2000. [Google Scholar]
- 8.Holmes SJ, Granoff DM. The biology of Haemophilus influenzae type b vaccination failure. J Infect Dis. 1992;165:S121–S128. doi: 10.1093/infdis/165-supplement_1-s121. [DOI] [PubMed] [Google Scholar]
- 9.Heath PT, Booy R, Griffiths H, Clutterbuck E, Azzopardi HJ, Slack MP, et al. Clinical and immunological risk factors associated with Haemophilus influenzae type b conjugate vaccine failure in childhood. Clin Infect Dis. 2000;31:973–980. doi: 10.1086/318132. [DOI] [PubMed] [Google Scholar]
- 10. McVernon J, Heath PT, Slack MPE, Ramsay M, Moxon ER. Hib vaccine efficacy—the United Kingdom (UK) ‘no boost’ experience [Abstract]. Proceedings of the 19th annual meeting of the European Society for Paediatric Infectious Diseases, Istanbul, Turkey, 2001:26.