Abstract
Osler-Weber-Rendu disease (OWRD), also known as hereditary haemorrhagic telangiectasia (HHT), is an autosomal dominant genetic disorder characterised by arteriovenous malformations in several organs. Ischemic cholangitis is a rare life-threatening complication of OWRD, with only a few documented cases in the literature. A liver transplant is the main curative treatment. In this paper, we report a case of a 33-year-old woman with a history of recurrent epistaxis, admitted with abdominal pain and fever, physical examination found multiple cutaneous and mucosal telangiectasias and the biological workup showed cholestasis, abdominal imaging identified arterio-venous shunts and multiple cystic hepatic lesions, one of them seemed to communicate with an intrahepatic biliary duct, finally the diagnosis of ischemic cholangitis due to OWRD was retained and antibiotic treatment has been initiated. We review the various therapeutic options available to improve the management of this fatal complication.
Keywords: Epistaxis, Rendu Osler Weber disease, Ischemic cholangitis, Bilomas, Bevacizumab, Liver transplantation
Introduction
Osler-Weber-Rendu disease (OWRD) is an autosomal dominant disorder characterised by mucocutaneous telangiectasias and arteriovenous malformations. The Curaçao criteria, published in 1999, were used to establish the diagnosis [1]. Liver involvement includes ischemic cholangitis, a rare complication of the disease due to a blood flow steal through arteriovenous shunting [2], the diagnosis must be suggested clinically, in the presence of abdominal pain, a family or personal history of recurrent epistaxis or confirmed OWRD, and/or the presence of cutaneous-mucosal telangiectasias. Here, we report the outcome of a patient with ischemic cholangitis due to OWRD managed with intravenous antibiotics.
Case report
A 33-year-old woman with a history of recurrent epistaxis presented with right upper quadrant pain and fever chronically ongoing for 6 months. The patient had a history of postpartum hemorrhage. Her family history was significant for recurrent epistaxis (the father and 2 nephews). Upon physical examination, the patient was found to have multiple cutaneous and mucosal telangiectasias. Laboratory tests revealed inflammatory syndrome and cholestasis.
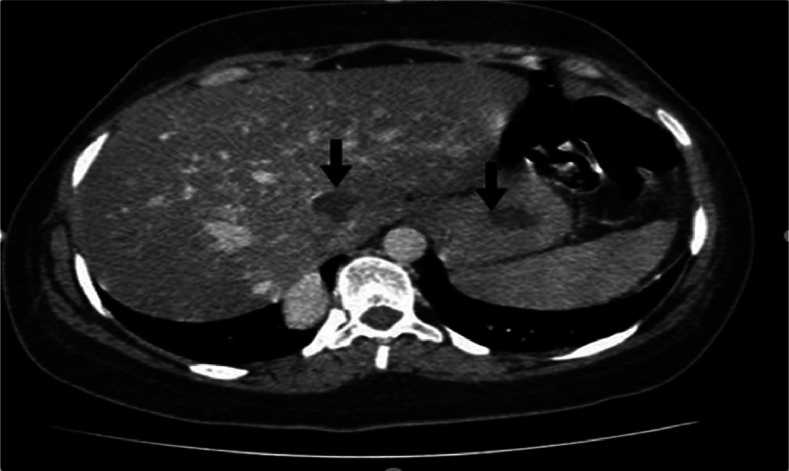
A Doppler ultrasound showed multiple cystic hepatic lesions realizing fluid-fluid levels, without dilatation of bile ducts, and arterio-venous shunts. An echocardiographic evaluation was normal. A brain magnetic resonance imaging was also normal. A computerized tomography (CT) scan found the previously described lesions, with a lesion in segment III containing air bubbles. The largest lesion was in segment VI, measuring 4 cm, and seemed to communicate with an intrahepatic biliary duct (Fig. 1).
Fig. 1.
CT scan showing arterialization of hepatic parenchyma and cystic lesions unenhanced (bilomas).
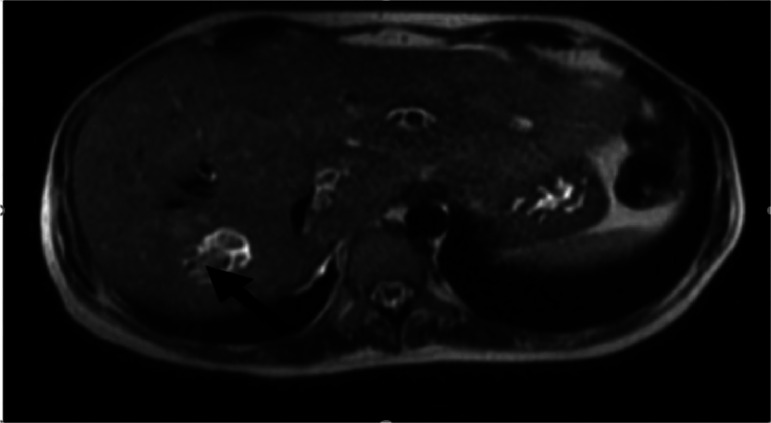
MRCP showed communication between cystic lesions and adjacent intrahepatic bile ducts suggesting infected bilomas (Fig. 2).
Fig. 2.
The largest biloma in segment VI with fluid level.
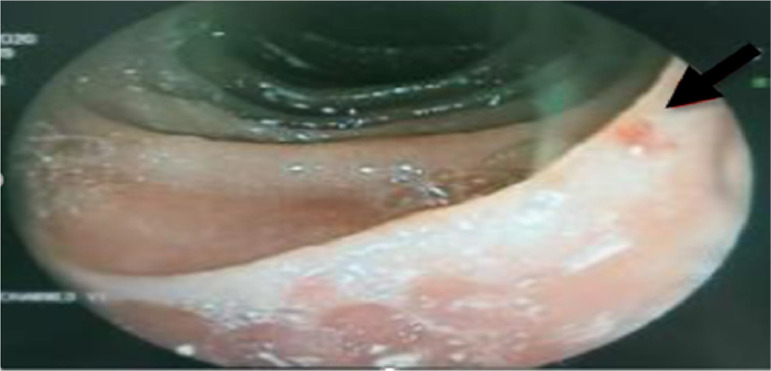
Nasopharyngoscopy showed multiple telangiectasias in the nasal septum bilaterally that was cauterized. Upper endoscopy showed mucosal gastric and duodenal telangiectasia without bleeding stigmata (Fig. 3), ileocolonoscopy was normal.
Fig. 3.
Gastric telagiectasia.
The Patient was managed with intravenous antibiotics Metronidazole (500 mg/8 h) and Ceftriaxone (2 g). Unfortunately, Bevacizumab was not readily available, and a liver transplantation was not obvious considering systemic sepsis.
A short-term evolution on antibiotics was favorable, with improvement of the inflammatory syndrome (Table 1), but the patient then declined rapidly and died after uncontrollable sepsis.
Table 1.
Laboratory findings before and after therapy.
| Pre | Post | ||
|---|---|---|---|
| total bilirubin (mg/L) | 7 | 8 | PRE: Pre-treatment values; POST: Post-treatment values ALP, alkaline phosphatase; GGT, gamma-glutamyl transferase; ALT, alanine transaminase; AST, aspartate transaminase; CRP, C-reactive protein. |
| ALT (UI/l) | 19 | 21 | |
| AST (UI/l) | 20 | 13 | |
| GGT (UI/l) | 140 | 122 | |
| ALP (UI/l) | 479 | 337 | |
| CRP (UI/l) | 276 | 58 |
Discussion
OWRD, or hereditary haemorrhagic telangiectasia (HHT), is a rare autosomal dominant disorder characterised by arteriovenous malformations and telangiectases. OWRD was first described in 1865 as hereditary epistaxis by B.G. Babington in The Lancet medical journal [3]. Osler, Weber and Rendu are the 3 scientists who revealed the other disorders of this syndrome, which bears their names [4]. Otherwise known as hereditary haemorrhagic telangiectasia (HHT), OWRD occurs due to a genetic disorder, and 2 main mutations are implicated in transformation growth factor-β signalling that contribute to the development of blood vessels: Endoglin (ENG) in HHT type 1 in chromosome 9 and anaplastic lymphoma kinase-1 (ALK-1) ACVLR1 in HHT type 2 in chromosome 12. Some HHT patients have SMAD4 mutation MADH4 with juvenile polyposis syndrome [5,6]. Other less frequently affected genes have been described, such as GDF2 and RASA1 [7].
The most common symptom of OWRD is recurrent epistaxis. Consensus clinical diagnostic criteria were published in 1999. The four Curaçao criteria (epistaxis, telangiectasia, visceral lesions, and appropriate family history) are carefully defined. The diagnosis of HHT is certain if three criteria are present [1]. Several organs may be affected: liver involvement due to arteriovenous malformations is variable, and many disorders have been described, including high-output cardiac failure, portal hypertension, encephalopathy, biliary ischemia and mesenteric ischemia [2].
Cholangitis due to biliary ischemia is a rare complication of the disease due to a blood flow steal through arteriovenous shunting. Only a few cases of cholangitis are described in the literature (Table 2). In a large Italian cohort of 154 patients diagnosed with HHT with liver involvement and followed for 44 months, none of the patients developed cholangitis [8].
Table 2.
Main literature cases of ischemic cholangitis in ROWD.
| Clinical symptoms | Laboratory testing | Imaging examination | treatment | Outcome after 12months | ||
|---|---|---|---|---|---|---|
| O Kharmach et al | Right upper quadrant pain | Cholestasis Enterobacter cloacae bacteremia | short stenoses with dilations of the Intrahepatic bile ducts intrahepatic bilomas 27 × 11 mm and 16 × 16 mm | monitoring | good clinical and biological outcome | [9] |
| A. Vlachou et al | Right upper quadrant pain Weight loss fever | Cholestasis leukocytosis positive blood cultures for Enterococcus | biliary stenosis and dilatation large bilomas | Antibiotics ursodeoxycholic acid Bevacizumab | good clinical, biological and morphological outcome | [10] |
| Right upper quadrant pain Weight loss fever | normal liver biochemistry | segmental intrahepatic biliary dilatation, intraductal filling defects and multiple bilomas | Antibiotics Bevacizumab | Good clinical, biological and morphological outcome | ||
| Right upper quadrant pain Weight loss fever | cholestasis | irregular intrahepatic biliary dilatation with areas of focal structuring multiple bilomas ischemic stricture in the gallbladder body | Antibiotics Bevacizumab | Bacterial cholangitis after 6months of treatment improved after 8months | ||
| C.Pavel et al | Right upper quadrant pain | cholestasis | AVMs with peribiliary ischemia Right lobe 6/5 cm biloma | Enlisted for liver transplantation | Death several days after admission | [13] |
The management of cholangitis with superimposed infection is based on prolonged antibiotic therapy adapted to the antibiogram, which may be effective in the short and medium term [9]. Given the high mortality risk of ischemic cholangitis [10] and in accordance with guidance from the European Association for the Study of the Liver, liver transplantation should be discussed when appropriate medical treatment fails in emergency cases of ischemic bile duct necrosis [2].
Bevacizumab, an anti-vascular endothelial growth factor, has been proven effective in treating patients with severe HHT and ischemic cholangitis but should not delay surgical intervention [11], [12], [13]. This treatment can induce complications that may delay transplantation. Q. Maestraggi reported the case of a patient with ischemic cholangitis treated with bevacizumab who developed pulmonary embolisms and thromboses of hepatic and portal veins after 6 courses of bevacizumab [14].
In our case, the patient could not benefit from a liver transplantation; antibiotic therapy was prescribed with a good short-term response, but subsequent deterioration led to death.
Given the limited number of cases of ischemic cholangitis due to OWRD published in the literature, the management of this liver complication is not straightforward. While liver transplantation is the main curative treatment, it is not always readily applicable, and the emergence of studies supporting the safety and efficacy of bevacizumab would therefore recommend it as a standby treatment in these conditions before the disease progresses. A multidisciplinary meeting should be convened for each patient in order to propose the most appropriate approach.
Conclusions
Ischemic cholangitis due to OWRD is rare but should be considered when a patient reports recurrent epistaxis and abdominal pain. It is a fatal complication and must be managed early and appropriately; further studies are needed to analyse morbi-mortality and to optimise the timing of liver transplantation.
Patient consent
I declare that the patient provided informed written consent for collection of personal and medical data for reporting in an anonymized manner in this case report.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Shovlin C L, Guttmacher A E. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome) Am J Med Genet. 2000;6:66–67. doi: 10.1002/(sici)1096-8628(20000306)91:1<66::aid-ajmg12>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 2.European Association for the Study of the Liver: EASL clinical practice guidelines: vascular diseases of the liver. J Hepatol. 2016;64:179–202. doi: 10.1016/j.jhep.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 3.Babington BG, Reynolds JR. Hereditary epistaxis. Lancet. 1865;86:362–363. doi: 10.1016/S0140-6736(02)55197-7. [DOI] [Google Scholar]
- 4.Fuchizaki U, Miyamori H, Kitagawa S. Hereditary haemorrhagic telangiectasia (Rendu-Osler-Weber disease) Lancet. 2003;362:1490–1494. doi: 10.1016/S0140-6736(03)14696-X. [DOI] [PubMed] [Google Scholar]
- 5.Cole S G, Begbie M E, Wallace G M F. A new locus for hereditary haemorrhagic telangiectasia (HHT3) maps to chromosome 5. J Med Genet. 2005;42:577–582. doi: 10.1136/jmg.2004.028712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prigoda N L, Savas S, Abdalla S A. Hereditary haemorrhagic telangiectasia: mutation detection, test sensitivity and novel mutations. J Med Genet. 2006;43:722–728. doi: 10.1136/jmg.2006.042606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viteri-Noël A, González-García A, Patier JL. Hereditary hemorrhagic telangiectasia: genetics, pathophysiology, diagnosis, and management. J Clin Med. 2022;11:5245. doi: 10.3390/jcm11175245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buscarini E, Leandro G, Conte D. Natural history and outcome of hepatic vascular malformations in a large cohort of patients with hereditary hemorrhagic teleangiectasia. Dig Dis Sci. 2011;56:2166–2178. doi: 10.1007/s10620-011-1585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O Kharmach, M Borahma, N Lagdali: O Kharmach, M Borahma. Ischemic cholangitis during Osler-Weber-Rendu disease: a case report. Egyptian Liver J. 12:10. 10.1186/s43066-021-00163-y
- 10.Pavel C, Cabel T. Dragoș Dinuță: hereditary hemorrhagic telangiectasia—a case series experience from a liver transplant center in Romania. Diagnostics (Basel) 2022;12:2959. doi: 10.3390/diagnostics12122959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vlachou PA, Colak E, Koculym A. Improvement of ischemic cholangiopathy in three patients with hereditary hemorrhagic telangiectasia following treatment with bevacizumab. J Hepatol. 2013;59:186–189. doi: 10.1016/j.jhep.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Guilhem A, Fargeton AE, Simon AC. Intra-venous bevacizumab in hereditary hemorrhagic telangiectasia (HHT): a retrospective study of 46 patients. PLoS One. 2017;30 doi: 10.1371/journal.pone.0188943. eCollection 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silvain C, Thévenot T, Colle I. Hereditary hemorrhagic telangiectasia and liver involvement Vascular liver diseases: position papers from the francophone network for vascular liver diseases, the French Association for the Study of the Liver (AFEF), and ERN-rare liver. Clin Res Hepatol Gastroenterol. 2020;44:426–432. doi: 10.1016/j.clinre.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Silvain C, Théveno T, Colle I, Maestraggi Q, Bouattour M. Bevacizumab to treat cholangiopathy in hereditary hemorrhagic telangiectasia: be cautious. Medicine (Baltimore. 2015;94:1966. doi: 10.1097/MD.0000000000001966. [DOI] [PMC free article] [PubMed] [Google Scholar]