Dear editor,
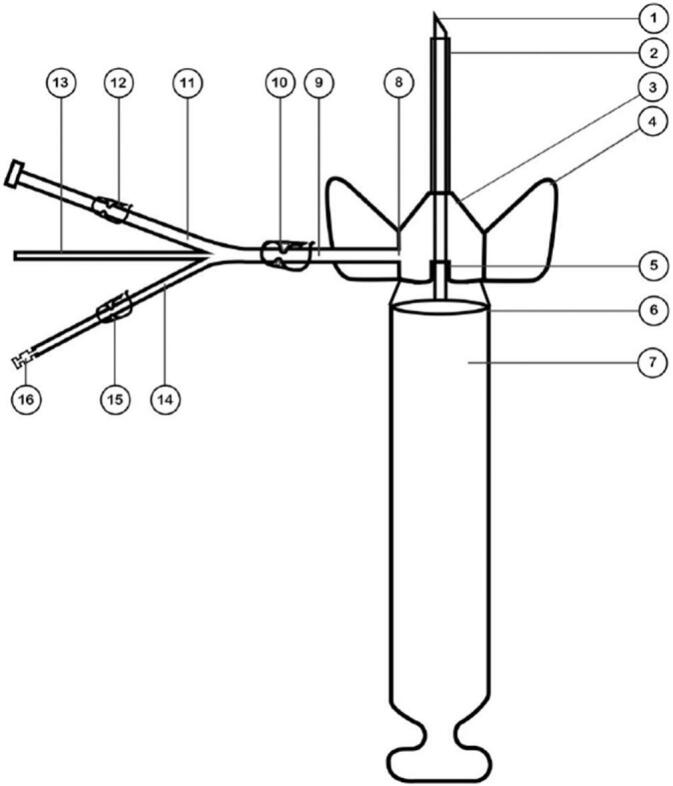
Peripheral vascular catheterization is one of the most common invasive procedures. Approximately 200 million catheters are used in America annually, and over 70 % of hospitalized patients require intravenous catheter insertion [1]. The use of an intravenous catheter can lead to various complications, including thrombosis, thrombophlebitis, infection, and injuries from contact with a contaminated needle [2]. Needlestick injury is one of the most serious occupational hazards among healthcare workers [3], which can lead to the transmission of various pathogens through blood. These include Hepatitis B, Hepatitis C, and AIDS [4]. The risk of AIDS transmission is 0.3 % to 0.5 %, while the risk of hepatitis B transmission is 10 % to 35 %, and hepatitis C transmission is 1.8 % to 10 % [5]. Needlestick injuries are more likely to occur among nurses than other medical staff [6]. This can be attributed to heavy workload, environmental stressors, job dissatisfaction [7], and working in specific departments [8]. One of the main situations in which needlestick injuries occur in nurses is during venipuncture and catheter insertion [9]. The engineering and design of medical tools, such as IV cannulas, are crucial in medicine [8]. Researchers have developed a cannula with a syringe-like cylinder to address this critical issue (Fig. 1). This design allows for safe disposal of the contaminated needle by retracting the cylinder's piston, which remains trapped inside the chamber after use (Fig. 2). Once the venipuncture process is complete, the needle, which is locked in the syringe-like chamber, can be removed from the one-way anti-leak silicone valve of the cannula and safely disposed of (Fig. 3). In this scenario, not only does a drop of blood leak out, but there is also zero probability of a needle sticking in nurses. Furthermore, the changes in the cannula mean there is no need to apply pressure to the blood vessels to stop the blood flow. This cannula has three separate ports for serum therapy, packed cell transfusion, and blood sampling, each equipped with a clamp to control the flow of liquids to the vein. The blood sampling port also has a one-way silicone valve to prevent leakage. A triple port eliminates the need for a three-way IV cannula when administering multiple serum therapies, which saves on using such tools. This type of cannula is unique because it features a safe chamber for disposing of the cannula needle, a triple port for simultaneous injections and blood sampling, and a blood filter at the beginning of the blood transfusion port. This eliminates the need for patients to use a separate filter set. The invention has been officially registered at the patent office under the title of ‘Cannula equipped with a triple port and a secure anti-needle stick housing (Registration no.: 111023)’ (Fig. 4).
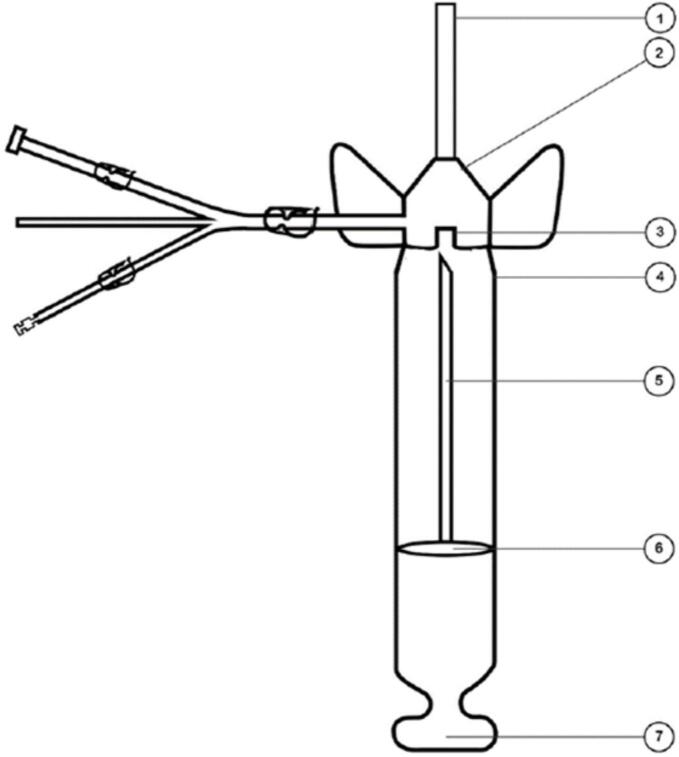
Fig. 1.
1. Needle.
2. Plastic catheter.
3. Catheter needle sheath*.
4. Catheter wing.
5. Silicone valve.
6. Safe chamber.
7. Safe chamber piston.
8. The area where the main branch of the triple port connects to the catheter needle sheath.
9. The main branch of the triple port.
10. Main port path clamp.
11. Serum therapy port.
12. Serum therapy port clamp.
13. Blood sampling port equipped with anti-leak silicone valve.
14. Blood transfusion port.
15. Blood transfusion port clamp.
16. 60-micron filter for blood transfusion.
*The catheter needle sheath includes a one-way anti-leakage valve, which allows the needle and syringe head to be safely separated from it.
In this figure, Part number 1 is the catheter metal needle. This 2.5 cm long needle passes through the silicone valve of the catheter needle sheath in part number 5 and is connected to the piston of the safe chamber (part no.7). The length of the safe chamber (part no. 6) is 3 cm, and the length of the piston of the safe chamber is 2.5 cm (and the length of the needle is 2.5 cm). By pulling back the piston of the safe chamber, the needle first passes through the silicone valve, then it is completely locked inside the safe chamber. After removing the needle, the narrow syringe tip detaches from the needle sheath's silicone one-way valve (part no. 5). The safe chamber, which now contains the contaminated needle, is safely disposed of. After inserting the plastic catheter (part no. 2) into the vein, catheter wings (part no. 4) are used to secure the catheter needle sheath (part no. 3) to the patient's skin.
Fig. 2.
Illustrates the post-IV catheter insertion. Part number 1 is a plastic catheter positioned within the vein. The catheter needle sheath (part no. 2) is completely fixed. The narrow head of the safe chamber syringe (part no. 4) is separated from the needle sheath by twisting. The used needle (part no. 5), which is connected to the cylinder of the safe chamber (part no. 6), is trapped by the piston of the safe chamber (part no. 7) in the body of the safe chamber (part no. 4). Considering the metal needle is shorter than the safety chamber, its sharp head is completely locked inside, like a syringe.
Fig. 3.
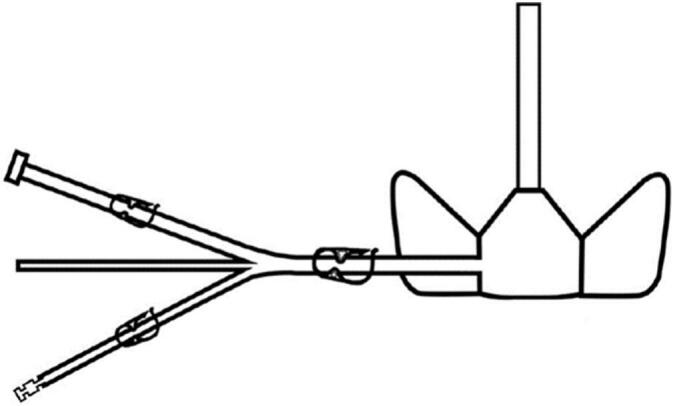
Illustrates the catheter after removing and disposing of the safe chamber. The needle, locked inside the safe chamber, has been separated from the catheter and discarded.
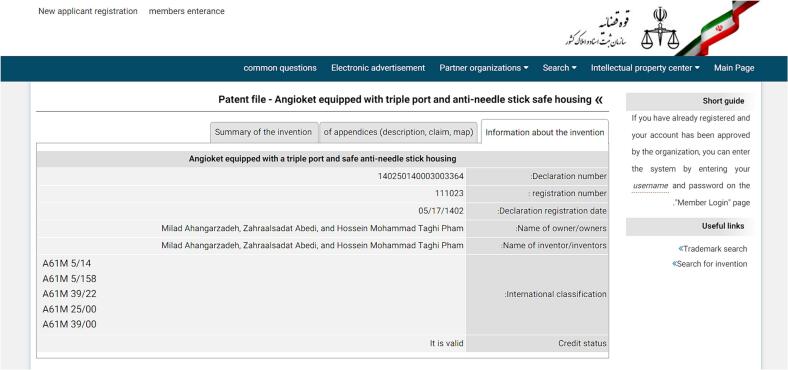
Fig. 4.
Illustrates the proof of patent registration.
Ethical approval
None. Our paper is in the format of a letter to the editor.
Funding
This letter to the editor received no specific funding from public, commercial, or not-for-profit sectors.
Author contribution
Milad Ahangarzadeh: Reviewed the literature and wrote the manuscript. Zahrasadat Abedi & Naser Parizad: Supervised the writing process and revised the manuscript.
Guarantor
Naser Parizad.
Research registration number
Not applicable.
Conflict of interest statement
None.
Acknowledgements
The authors would like to extend their sincere gratitude to the members of the patent registration office for their invaluable and unwavering cooperation. They also wish to express their appreciation to Mariam Angelica Parizad for her review and editing of the letter.
References
- 1.Alicdan J., Feldheim A., Fong C., Myers F., Torriani F. Peripheral venous catheter associated bloodstream infections (PVC-BSI) risk compared to central line associated bloodstream infections (CLABSI) Am. J. Infect. Control. 2023;51(7):S34–S35. doi: 10.1016/j.ajic.2023.04.061. [DOI] [Google Scholar]
- 2.Heng S.Y., Yap R.T.-J., Tie J., McGrouther D.A. Peripheral vein thrombophlebitis in the upper extremity: a systematic review of a frequent and important problem. Am. J. Med. 2020;133(4):473–484. e473. doi: 10.1016/j.amjmed.2019.08.054. [DOI] [PubMed] [Google Scholar]
- 3.Mengistu D.A., Tolera S.T. Prevalence of occupational exposure to needle-stick injury and associated factors among healthcare workers of developing countries: systematic review. J. Occup. Health. 2020;62(1) doi: 10.1002/1348-9585.12179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma R., Gupta P., Jelly P. Pattern and serological profile of healthcare workers with needle-stick and sharp injuries: a retrospective analysis. J. Family Med. Prim. Care. 2020;9(3):1391–1396. doi: 10.4103/jfmpc.jfmpc_1078_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bi P., Tully P., Pearce S., Hiller J. Occupational blood and body fluid exposure in an Australian teaching hospital. Epidemiol. Infect. 2006;134(3):465–471. doi: 10.1017/S0950268805005212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghanei Gheshlagh R., Aslani M., Shabani F., Dalvand S., Parizad N. Prevalence of needlestick and sharps injuries in the healthcare workers of Iranian hospitals: an updated meta-analysis. Environ. Health Prev. Med. 2018;23:1–11. doi: 10.1186/s12199-018-0734-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C., Huang L., Li J., Dai J. Relationship between psychosocial working conditions, stress perception, and needle-stick injury among healthcare workers in Shanghai. BMC Public Health. 2019;19:1–11. doi: 10.1186/s12889-019-7181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho E., Lee H., Choi M., Park S.H., Yoo I.Y., Aiken L.H. Factors associated with needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire survey. Int. J. Nurs. Stud. 2013;50(8):1025–1032. doi: 10.1016/j.ijnurstu.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson A.P., Almerol L.A., Campbell J., Hamilton L. Needlestick injuries: the role of safety-engineered devices in prevention. Br. J. Nurs. 2020;29(14):S22–S30. doi: 10.12968/bjon.2020.29.14.S22. [DOI] [PubMed] [Google Scholar]