Abstract
Purpose
Primary Sjögren’s syndrome (PSS) has many effects such as fatigue, pain, physical activity limitation and sleep disturbance, which limit patient’s daily and social lives. The aim of our study was to assess fatigue, depression, physical activity status and quality of life in patients with PSS, and to determine the relationship between these data and disease-related parameters.
Patients and Methods
This study was conducted with 117 primary Sjögren’s syndrome patients. Demographic and anthropometric characteristics, disease activity (ESSDAI), quality of life scale (SF36), depression (Beck Depression Scale), physical activity status (International Physical Activity Questionnaire Short Form (IPAQ) score) and sleep status (Pittsburgh Sleep Quality Scale) of PSS patients were evaluated and relationships have been examined.
Results
According to the results of our study, we found that sleep disorders are common in PSS patients (74.4%). Overweight patients, particularly higher lean mass sleep better (r:-0.201, p:0.043). Poor sleep causes fatigue (p=0.062) and depression (p=0.030). Sleep disturbance could not be explained by depressive state alone. However, after controlling for depression, the effect of sleep on fatigue seriously decreases (p=0.311). Exercise did not improve sleep quality (p=0.35) and the rate of poor sleep was higher among who exercised (p=0.192).
Conclusion
Based on the results of our study, we believe that, treating depression in PSS patients is crucial for reducing fatigue. Patients need education on performing the correct exercises and weight gain should done in a professional manner. Gaining a deeper understanding of the multisystem involvement of the disease and the impact of exercise on the disease, will have positive effects on patient care and treatment decisions.
Keywords: Sjogren’s syndrome, sleep disorders, quality of life, exercise
Introduction
Primary Sjögren’s syndrome (PSS) is a chronic, multisystem autoimmune disease. Dry mouth and eyes are most commonly observed as a result of the lymphocyte infiltrates in the tubular epithelium of the lacrimal and salivary glands.1 In addition, extraglandular involvement may be observed with various organ involvement. The disease also has many effects, including fatigue, reduced physical performance, pain and sleep disturbance which limit patient’s daily and social standards of living.1,2
As with other rheumatic diseases, fatigue is present in 70% of patients with PSS (2–4). Fatigue, which is an important finding, has a negative impact on patient’s daily and social lives. This may lead to a decrease in their quality of life.2–8 Anxiety and depression are also more common in PSS patients, and this may lead to a decrease in quality of life.2–7 Sleep problems are also common in patients with PSS. PSS patients have reduced sleep efficiency, increased number of awakenings and they have excessive daytime sleepiness. In addition, obstructive sleep apnea syndrome may be seen more frequently in pSS patients.9 Sleep problems may be caused by eye irritation and the need to use eye drops at night. Waking up to drink water to relieve dry mouth can be another reason. Pain, fatigue and depression also affect sleep problems.2,3,8,9 Physical fitness and aerobic capacity are reduced in women with PSS syndrome and may be related to the fatigue seen in the disease. Sedentary lifestyle and reduced physical activity are other causes of fatigue. A good exercise programme may help improve fatigue by increasing physical capacity.2,7,8 It has been observed that obesity causes an increase in proinflammatory cytokines and enhances inflammatory processes in patients with systemic lupus erythematosus.10 In this study, demographic and anthropometric characteristics, disease activity (ESSDAI), quality of life scale (SF36), depression (Beck Depression Scale), physical activity status (International Physical Activity Questionnaire Short Form (IPAQ) score) and sleep status (Pittsburgh Sleep Quality Scale) of PSS patients were assessed and relationships were investigated.
Materials and Methods
This study was conducted between August 2020 and August 2023 at Ege University, Department of Internal Medicine, Department of Rheumatology with volunteer female patients over 19 years of age who were diagnosed with primary Sjögren’s syndrome. Patients were selected consecutively. All were diagnosed with pSS and fulfilled the 2016 ACR-EULAR Classification Criteria.11 Written informed consent form was obtained from the patients who agreed to participate in the study. The exclusion criteria are: (a) Being under 18 years of age; (b) any other systemic autoimmune diseases; (c) malignant tumor, severe kidney or liver dysfunction; (d) having an eating disorder (such as Anorexia, Bulimia); (e) being pregnant or a nursing mother; (f) having any mental illness (such as schizophrenia, dementia); (g) inability to cooperate in the study, and incapability to understand and answer the questions. The study adhered to the principles of the Declaration of Helsinki. Ethical committee approval was obtained from the Ethics Committee of Ege University, dated and numbered 01/10/2020, 20–10T/32.
Patient information was obtained from the patient registration system, anthropometric measurements were taken, the disease activity index (ESSDAI)11 was calculated, blood biochemical tests were analysed, the Short Form 36 (SF36)12 was used to assess quality of life, the Pittsburgh Sleep Scale13 was used to assess sleep quality, and the Physical Activity Questionnaire Short Form (IPAQ)14 was used to assess physical activity levels.
The body composition of the individuals was evaluated with the TANITA BC-418 MA device based on the bioelectrical impedance analysis (BIA) method. BIA analyzed body fat mass, body fat percentage and lean body mass based on the difference in electrical conductivity of adipose tissue and lean tissue mass (Kyle et al, 2004).15
The Quality-of-Life Scale Short Form SF-36 is a multi-title scale that assesses 2 main dimensions (physical dimension and mental dimension) and 8 concepts (physical functioning, role limitations due to physical problems, bodily pain, general health perception, energy/vitality (fatigue), social functioning, role limitations due to emotional problems, mental health and general health perception).12
The Pittsburgh Sleep Scale is an overall score ranging from 0 to 21, with a higher total PSQI score indicating poorer sleep quality. A score of six or more is considered to indicate poor sleep quality.13
The International Physical Activity Questionnaire (IPAQ) has four sections (vigorous physical activity, moderate physical activity, walking and sitting). The assessment analyses the data by converting them into metabolic equivalent (MET) values. The level of physical activity is classified as physically inactive (<600 MET-min/week), minimally active (600–3000 MET-min/week) and vigorously active (> 3000 MET-min/week).14
Statistical Analysis
Data obtained from the study were analysed using IBM SPSS Statistics Standard Campus Edition package programme v.23.0. Descriptive statistics were expressed as mean ± standard deviation for normally distributed variables and median (lower-upper) for non-normally distributed variables. The Student’s T-test was used to evaluate the means between two groups with normal distribution. The Mann–Whitney U-test was used to evaluate means between two groups with non-normal distribution. The Pearson and Spearman correlation tests were used to obtain information on about the strength and direction of the linear relationship between two continuous variables. In all statistical tests, 95% confidence intervals were accepted and p<0.05 was considered significant.
Results
The sociodemographic and clinical characteristics of the 117 female patients with PSS who participated in the study are shown in Table 1. The mean age of the participants was 55.2±11.7 years and the mean duration of PSS was 11.8±7.0 years. The disease score (ESSDAI) of the patients was calculated to be 4.4±5.0. Sociodemographic and clinical characteristics were shown in Table 1.
Table 1.
Sociodemographic and Clinical Characteristics of Patients
| Sociodemographic Characteristics | Values Mean ±Std. Deviation (Min-Max) |
|---|---|
| Age | 55.2±11.77 (23–82) |
| Sjögren’s disease duration | 11.85±7.05 (1–35) |
| Disease Score (ESSDAI) | 4.43±5.07 (0–27) |
| Education status | N (%) |
| Primary School | 47 (40.2) |
| Middle School | 13 (11.1) |
| High School | 19 (16.2) |
| University | 38 (32.5) |
| Employment Status | N (%) |
| Full day | 23 (19.7) |
| Half day | 9 (7.7) |
| Not working | 85 (72.6) |
| Cigarette Use | N (%) |
| Current | 10 (8.5) |
| Never | 98 (83.8) |
| Ex-smoker | 9 (7.7) |
| Height (m) | 1.57 ± 0.07 |
| Weight (kg) | 71.1 ± 12.1 |
| BMI (kg/m2) | 28.7 ± 5.7 |
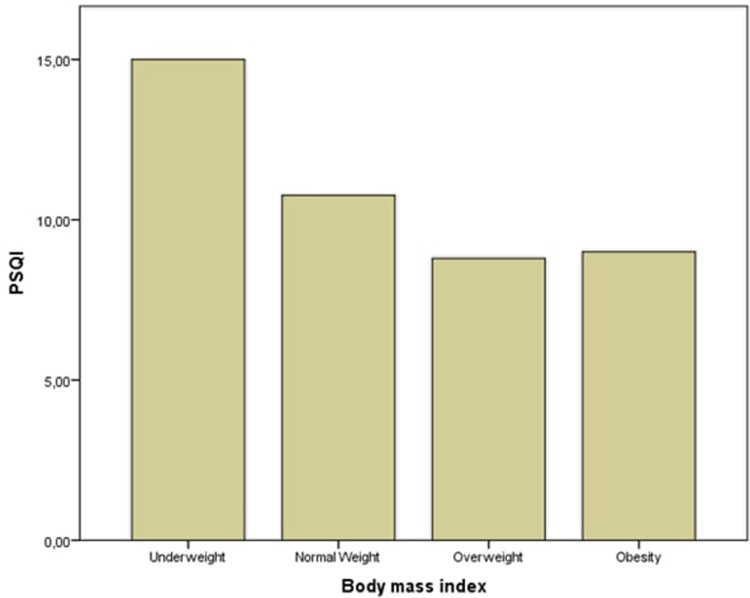
There was a significant relationship between educational level and BMI. As the level of education increased, the prevalence of obesity and patient weight decreased significantly (p<0.001). Although not significant, there was an association between BMI and sleep quality (p=0.186) (Figure 1). The sleep quality of overweight people seems to be relatively better. In particular, patients with more lean mass than fat mass had better sleep. Regression analysis showed a significant relationship between lean mass and PSQI sleep scores (r:-0.201, p:0.043).
Figure 1.
Body mass index and sleep quality relations.
Sleep quality worsened with increasing educational status (p=0.065), and those with a university degree were more likely to have poor sleep than those without a university degree (p=0.024). Physical function (p=0.048) and general health perception (p=0.043) were lower among those without a university degree. Those with a university degree were more likely to be depressed (p=0.035).
While 55.6% of the patients were inactive, 44.5% performed minimal or vigorous exercise. There were no significant associations between exercise and disease activity score, educational status, body mass index, quality of life scales, fatigue, biochemical values and depression status. Physical functioning in the SF-36 quality of life scale was found to be lower in patients with vigorous physical activity compared with the minimal and low physical activity groups, although not significantly (p=0.061). The ESSDAI scores of the very active patients were higher than those of the minimally active or inactive patients, although not significantly (p=0.153), whereas the fatigue scores of the vigorous exercises were better (0.360). Mean depression scores were lower for those who exercised (p=0.156). In addition, the mental health of those who did vigorous exercise was better (p=0.169). Exercise did not improve sleep quality (p=0.35). On the contrary, the rate of poor sleep was higher in those who exercised (p=0.192). The rate of patients with poor sleep quality was 74.4% in all patients, and the rate of sleep disturbance was 80.8% in those who exercised. The relationships between exercise status (inactive - minimal or vigorous exercise) and clinical, sleep quality, depression and quality of life scales are shown in Table 2.
Table 2.
Relationships Between Exercise Status (Inactive - Minimal or Vigorous Exercise) and Clinical, Sleep Quality, Depression, and Quality of Life Scales
| Inactives Mean 95% CI | Actives Mean 95% CI | Mean Difference (95% CI of Difference) | P | |
|---|---|---|---|---|
| Disease activity score | 4.15 (3.01–5.30) | 4.60 (3.01–6.19) | −0.56 (−2.44–1.30) | 0.552 |
| Depression score | 17.45 (15.27–19.63) | 15.03 (13.08–16.99) | 2.14 (−0.83–5.12) | 0.156 |
| Physical functioning | 55.15 (48.34–61.97) | 54.60 (46.43–62.78) | 0.54 (−9.89–10.99) | 0.917 |
| Physical role difficulties | 43.22 (32.06–54.39) | 38.23 (26.43–50.03) | −3.86 (−19.59–11.87) | 0.628 |
| Emotional role difficulties | 43.22 (32.06–54.39) | 47.05 (33.91–60.20) | −3.82 (−20.79–13.13) | 0.656 |
| Fatigue | 37.96 (33.35–42.58) | 38.23 (32.98–43.48) | −0.26 (−7.16–6.63) | 0.939 |
| Mental health | 55.00 (51.14–58.85) | 53.01 (49.38–56.65) | 1.98 (−3.36–7.32) | 0.464 |
| Social functioning | 60.74 (54.65–66.83) | 61.76 (55.22–68.30) | −1.02 (−9.90–7.85) | 0.820 |
| Pain | 59.64 (53.19–66.09) | 56.86 (50.03–63.69) | 2.78 (−6.56–12.13) | 0.556 |
| General health perception | 47.10 (42.45–51.76) | 45.19 (39.74–50.64) | 1.91 (−5.13–8.96) | 0.592 |
| Sleep score | 8.89 (7.64–10.13) | 10.00 (8.62–11.37) | −1.10 (−2.94–0.72) | 0.234 |
Abbreviation: CI, Confidence Interval.
Depression was more common in patients with poor sleep quality (p=0.009). Patients with poor sleep quality had more impaired physical functions (p=0.037), emotional role difficulties (p=0.014), fatigue (p=0.062), and general health perception (p=0.002). Relationships between sleep quality and clinical, depression and quality of life scales were shown in Table 3.
Table 3.
Relationships Between Sleep Quality and Clinical, Depression and Quality of Life Scales
| Good Sleepers | Bad Sleepers | Mean Difference (95% CI of Difference) | P | |
|---|---|---|---|---|
| Mean 95% CI | Mean 95% CI | |||
| Social functioning | 66.96 (57.99–75.93) | 59.33 (54.26–64.41) | 7.62 (−2.55–17.81) | 0.141 |
| Mental health | 57.42 (52.46–62.39) | 53.05 (49.92–56.19) | 4.37 (−1.77–10.51) | 0.162 |
| Fatigue | 43.7 (35.54–51.95) | 36.26 (32.58–39.94) | 7.48 (−0.37–15.34) | 0.062 |
| General health perception | 55.71 (48.66–62.7) | 43.21 (39.33–47.09) | 12.49 (4.66–20.33) | 0.002 |
| Disease activity score | 3.17 (1.80–4.55) | 4.73 (3.57–5.89) | −1.25 (−3.41–0.90) | 0.253 |
| Depression score | 14.34 (11.00–17.68) | 17.20 (15.54–18.86) | −2.86 (−6.27–0.54) | 0.099 |
| Physical functioning | 64.46 (52.87–76.05) | 51.83 (46.13–57.54) | 12.62 (0.76–24.48) | 0.037 |
| Physical role difficulties | 48.21 (30.72–65.70) | 32.18 (23.51–40.85) | 16.03 (−1.95–34.01) | 0.080 |
| Emotional role difficulties | 63.09 (46.46–79.72) | 39.08 (29.49–48.66) | 24.01 (4.87–43.15) | 0.014 |
| Pain | 66.07 (54.86–77.27) | 55.94 (50.96–60.92) | 10.12 (−2.02–22.27) | 0.100 |
Abbreviation: CI, Confidence Interval.
The mean depression score of the PSS patients in the study was 16.4±8.09 and 78.6% of the patients were mildly or severely depressed (Beck Depression Score >10) Sleep quality was more impaired in depressed patients (p=0.008). There was no significant association between depressed patients and exercise status (p=0.912). Depressed patients had significantly worse fatigue (p=0.001).
In the study, 50% of PSS patients without depression slept poorly. When patients with moderate and severe depression scores were excluded, 70.8% of the patients slept poorly. When the depression was excluded, there was no significant association between sleep quality and fatigue (p=0.311), disease score (p=0.507), or the other quality of life scales.
In regression analyses, there were no significant relationships between physical activity scores and disease activity, depression scores, sleep quality scores and quality of life scales. There was no significant association between sleep and disease activity scores in regression analyses. However, there was a significant association between sleep and depression in regression analyses. There were also significant associations between sleep scores and physical role difficulties, emotional role difficulties, fatigue, social functioning, pain, and general health perception. There was no significant relationship between sleep quality and fatigue in patients without depression (F(70):-0.102 p:0.393). Correlations between the Pittsburgh Sleep Quality Index (PSQI) total score and other variables are shown in Table 4.
Table 4.
Correlation Between Total Score from Pittsburgh Sleep Quality Index (PSQI) and Other Variables
| rs* | P | |
|---|---|---|
| Physical functioning | −0.221 | 0.018 |
| Physical role difficulties | −0.301 | 0.001 |
| Emotional role difficulties | −0.289 | 0.002 |
| Fatigue | −0.205 | 0.028 |
| Mental health | −0.146 | 0.119 |
| Social functioning | 0.254 | 0.006 |
| Pain | 0.221 | 0.017 |
| General health perception | −0.281 | 0.002 |
| Depression score | 0.266 | 0.004 |
| Physical activity score | 0.104 | 0.267 |
| Disease activity score | 0.069 | 0.460 |
When the effects of all factors on sleep were examined by logistic regression analysis, it was seen that the effect of lean body mass (0.904 (0.848–0.964) p=0.002) and general health (0.953 (0.927–0.979) p=0.001) had the most significant effect.
There were no significant relationships between disease scores and sleep scores and physical activity scores. There were significant relationships between disease scores and physical functioning, social functioning, and general health perception in regression analyses. There is no significant relationship between disease scores and UFFA physical activity scores. Correlations between the ESSDAI total score and other variables are shown in Table 5.
Table 5.
Correlation Between Total Score from ESSDAI and Other Variables
| rs* | P | |
|---|---|---|
| Physical functioning | −0.356 | 0.0001 |
| Physical role difficulties | −0.169 | 0.071 |
| Emotional role difficulties | −0.077 | 0.412 |
| Fatigue | −0.091 | 0.333 |
| Mental health | −0.020 | 0.834 |
| Social functioning | −0.271 | 0.003 |
| Pain | −0.097 | 0.303 |
| General health perception | −0.291 | 0.002 |
| Physical activity score | 0.026 | 0.780 |
| Sleep quality score | 0.069 | 0.460 |
Discussion
The aim of our study was to determine demographic characteristics and anthropometric measurements, to assess fatigue, depression, physical activity status and quality of life in patients with PSS, and to determine the relationship between these data and disease-related parameters.
There is a significant relationship between BMI and the level of education, with a decrease in obesity rates as the level of education increases. Sleep quality deteriorated with increasing educational level (p=0.065). Those with a university degree were more likely to be depressed (p=0.035). It is thought that as the educational status increases, patients pay more attention to their diet and are likely to maintain a normal weight. It was thought that as the level of education increased, patient’s awareness of the disease and its complications increased depression and sleep disturbances.
The impact of physical activity levels on the disease in inflammatory rheumatic diseases has received increasing attention in recent years. Low levels of physical activity have been associated with reduced quality of life in patients with rheumatoid arthritis.16 Regular exercise is known to reduce death from all causes.17 Studies have also shown that exercise plays a role in inflammation.18–21 During exercise, the chemokine IL-6 is released from muscle fibres through a TNF-independent pathway. And this released IL-6 inhibits the production of the pro-inflammatory cytokine TNF-alpha and stimulates the release of other anti-inflammatory cytokines such as IL-1ra and IL-10. As a result, regular exercise is thought to reduce CRP levels and suppress inflammation.16,18–21 The acute effects and long-term benefits of exercise in inflammatory diseases are not fully understood.21
Research has demonstrated a reduction in physical capacity and function among PSS patients compared to healthy controls.7 In this study, 55.6% of PSS patients were inactive, while 44.4% engaged in minimal or vigorous exercise. This study found no significant correlation between exercise status and disease activity score, nor any significant impact of exercise on fatigue. Furthermore, the quality-of-life scales calculated with SF-36 showed lower physical function in patients with severe physical activity compared to those in the minimal and low physical activity groups, although this difference was not statistically significant (p=0.061). One study reported a transient increase in serum CRP and CK after intense exercise in patients with systemic lupus erythematosus, but chronic physical activity reduced resting CRP levels and muscle injury. Exercise did not exacerbate disease activity or cause serious side effects in patients with systemic lupus erythematosus.21 In patients with rheumatoid arthritis, exercise did not have a negative effect on disease activity and was found to have a positive effect in some studies.22 In Miyamoto et al’s study, there was no difference in disease activity according to ESSDAI between patients with Sjögren’s syndrome who exercised and those who did not.23
Some studies have found significant benefits particularly in reducing fatigue when the exercise rates are increased.18,23 In our study, the ESSDAI scores of highly active patients were slightly higher than those of minimally active or inactive patients, although this difference was not statistically significant (p=0.153). However, the fatigue scores of those who engaged in intense exercise were better, although this difference was also not statistically significant (p=0.360). Another study found that exercise conducted with an instructor was found to be more effective than self-administered exercise. The lack of significant relationships between exercise rate and disease activity and fatigue may be due to inadequate knowledge of correct exercise techniques. As it is unclear whether our patients worked with an instructor or not, further studies are needed to determine the optimal exercise intensity ratio for patients. It may be beneficial to encourage patients to exercise with an instructor.18,23–25
However, it is important to keep in mind that rheumatic disease and increased inflammation can/may increase the risk of cardiovascular disease. Therefore, increasing physical activity may help reduce cardiovascular risk by preventing conditions such as metabolic syndrome, diabetes, and hypertension, as well as through the benefits of exercise itself.23
It is believed that exercise may have anti-depressant effects by increasing serotonin and tryptophan levels. While some studies have shown positive effects of exercise on depression,26 our study did not find a significant improvement in depression with increased physical activity, which is consistent with the findings of Miyamoto et al.23 However, it is worth noting that the mental health of those who engaged in intense physical activity was slightly better (p=0.169).
In our study, we found that exercise did not improve sleep quality, contrary to previous beliefs. In fact, the rate of poor sleep was higher in those who exercised (p=0.192). Overall, 75.5% of all patients had poor sleep quality, and this number rose to 83% in those who performed any exercise. In a study, it was shown that vigorous and moderate physical exercise sessions lasting > 90 min had a significant positive correlation with poor sleep quality. However, it was found that morning light physical exercise of 10 minutes per day has a good effect on sleep.27,28 Also, Wendt et al found that night PA seems to have an inverse effect on sleep variables. The Results also show the effect of adequate and effective exercise on sleep and emphasizes the importance of planned exercise.29
Approximately 33–50% of the adult population may experience sleep disturbances.30 Increased sleep disturbance has been reported in patients with various rheumatic diseases including rheumatoid arthritis and systemic lupus erythematosus.31 In patients with PSS, the prevalence of sleep disturbance is more prevalent than in healthy population and other inflammatory rheumatologic diseases.31 In another study conducted in Turkey where our study was conducted, the frequency of obstructive sleep apnea in patients with PSS was 84% and a decrease in the percentage of REM was found.9 In a study of patients with PSS, mean PSQI score was 8.0 and 46.1% were classified as poor sleepers.31 Other studies have reported the prevalence of poor sleep in PSS patients to be between 57–82%.30,32,33 In our study, 74.4% of the patients experienced poor sleep (PITSS>5). The mean PSQI score was found to be 9.38 (SD 4.97).
Sleep disturbance may be caused by disease-related inflammatory status and depression. It may also affect the immune system and inflammatory response, potentially increasing the risk of exacerbation in autoimmune diseases. It is unclear whether sleep changes are the result of disease-related symptoms, such as sicca symptoms, pain, and depression, or disease-related immune changes.31
The study suggests that overweight individuals with higher lean mass experience better sleep quality than those with higher fat mass. Regression analysis demonstrated a significant correlation between lean mass and PSQI sleep scoring (F (70):-0.201 p:0.043), indicating that increase in muscle mass and healthy weight gain have a positive impact on sleep. Effective exercise under the guidance of a trainer may improve sleep quality in patients with PSS.
Lean body mass is positively associated with non-REM and slow-wave sleep and obesity. The combination of reduced skeletal muscle and increased fat mass was found to be strongly associated with reduced sleep duration in the literature. Leptin is secreted by fat cells and has an inhibitory effect on appetite. Leptin concentration correlates with body fat percentage and is associated with obesity. Leptin levels increase in the first half of the night and decrease in the second half, demonstrating a circadian shift. Furthermore, leptin has protective effect on deep sleep by opposing the function of orexin neurons in the hypothalamus. As another different perspective lack of sleep causes a decrease in leptin so poor sleep quality may be one of the factors of obesity.34–36
Studies have shown poor sleep quality in PSS is associated with disease scores, pain, fatigue, and depression.30–33 Chung et al found that the ESSDAI was significantly lower in poor sleepers than in good sleepers, but no significant relationship was established.31 In some other studies, PSQI scores have been found to have a significant positive correlation with the course of the disease and depression score.30,32,33 In our study, although not significant, individuals with poor disease scores were more likely to experience poor sleep quality (p=0.253).
Studies have shown that patients with PSS and poor sleep quality exhibit significantly higher levels of fatigue.30,31 In our study, we found that fatigue was higher in those with poor sleep (p=0.062). This situation could be explained by a possible disorder in the hypothalamic-pituitary-adrenal axis.
Research has shown that individuals with poor sleep quality have a higher prevalence of depression compared to those with good sleep quality.31–33 Our study also found a significant relationship between sleep quality and depression (F(114): 0.266, p=0.004), with depression being more common in individuals with poor sleep quality (p=0.009).
However, Chuck et al found that poor sleep quality in patients with primary Sjögren’s syndrome (PSS) was not solely attributed to depression, as one third of PSS patients without depression also experienced poor sleep.31 Our study similarly found that poor sleep quality was prevalent in 50% of PSS patients without depression. Additionally, sicca symptoms, pain, and fatigue were identified as potential contributors to poor sleep quality in PSS patients.31 When the confounding effect of depression was removed, the significant relationship between sleep quality and fatigue (p=0.311) in patients without depression disappeared. Furthermore, there was no significant correlation between sleep quality and fatigue in patients without depression (F(70):-0.102, p:0.393).
Therefore, better management of disease activity and reduction of fatigue may be achieved by developing strategies to improve patient’s’ sleep quality, as suggested by the observation that people who sleep well tend to have better fatigue scores.
The meta-analysis by Zhang et al showed that patients with PSS had lower scores on all items of the SF-36 scale compared with healthy controls with the greatest difference observed in the Physical Role.37 All scores in the SF36 scale found in our study were lower than the SF36 scores found in the healthy population in the Turkish population.38 There were also significant relationships between the disease activity score and physical functioning (p<0.001), social functioning (p=0.003) and general health perception (p=0.002) in the SF-36 scale. There were no significant relationships between disease activity score and physical role difficulties, emotional role difficulties, fatigue, and pain.
Conclusion
Our study found that sleep disturbance is prevalent among patients with PSS. Furthermore, we observed a significant correlation between sleep disturbance and fatigue. Although depression is associated with sleep disturbance, it alone cannot account for the observed sleep disturbance. However, after controlling for depression, the effect of sleep on fatigue decreases. Therefore, our study suggests that treating depression in PSS patients is crucial for reducing fatigue. Furthermore, it is worth noting that depression is prevalent among PSS patients and can significantly impact their quality of life. Additionally, fatigue is a major issue for PSS patients, affecting both their quality-of-life scores and pain levels. It is important to highlight that over half (55.6%) of PSS patients are inactive, which has a negative impact on their sleep status. It is also worth noting that there is no significant correlation between physical activity levels and disease activity in PSS patients. Although there was no significant difference, very active patients had slightly higher ESSDAI scores compared to minimally active or less active patients. Additionally, patients who engaged in intense exercise had better fatigue scores. The study also found that overweight patients had relatively better sleep quality, particularly those with more lean mass than fat mass. This suggests that increasing muscle mass and achieving a healthy weight may have a positive impact on sleep quality. In Conclusion, exercise training with appropriate intensity in the presence of an instructor could be more effective for PSS patients.
Previous studies have not adequately analysed the impact of weight on sleep or the effect of exercise on disease scores and fatigue in PSS patients.18,23–25 Working with a trainer may be particularly beneficial for PSS patients. We suggest that it is very important that patients receive proper education on the importance of performing the correct exercises and that weight gain is done in a professional manner. Furthermore, prioritising the treatment of the depressive state may greatly benefit patients. The limitations of the study are the lack of a control group and non-randomized patient selection. And also, physical activity and sleep status in the questionnaires were for a certain period of time and cannot fully reflect the general situation. The type of physical activity and whether it was accompanied by an instructor is unknown. Despite this, many different scales were used and this study was able to evaluate the effects of sleep, physical exercise and depression on disease and quality of life. It is believed that gaining a deeper understanding of the multisystem involvement of the disease, as well as the relationship between different findings and the impact of exercise on the disease, will have positive effects on patient care and treatment decisions.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Fox RI. Sjögren’s syndrome. Lancet. 2005;366(9482):321–331. doi: 10.1016/S0140-6736(05)66990-5 [DOI] [PubMed] [Google Scholar]
- 2.Venables PJ. Management of patients presenting with Sjogren’s syndrome. Best Pract Res Clin Rheumato. 2006;20(4):791e807. [DOI] [PubMed] [Google Scholar]
- 3.Stack RJ, Southworth S, Fisher BA, et al. A qualitative exploration of physical, mental and ocular fatigue in patients with primary Sjögren’s Syndrome. PLoS One. 2017;12(10):e0187272. doi: 10.1371/journal.pone.0187272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strömbeck B, Ekdahl C, Manthorpe R, Wikström I, Jacobsson L. Health-related quality of life in primary Sjögren’s syndrome, rheumatoid arthritis and fibromyalgia compared to normal population data using SF-36. Scand J Rheumatol. 2000;29(1):20–28. doi: 10.1080/030097400750001761 [DOI] [PubMed] [Google Scholar]
- 5.Liu Z, Dong Z, Liang X, et al. Health-related quality of life and psychological status of women with primary Sjögren’s syndrome: a cross-sectional study of 304 Chinese patients. Medicine. 2017;96(50):e9208. doi: 10.1097/MD.0000000000009208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Omma A, Tecer D, Kucuksahin O, Sandikci S, Yildiz F, Erten S. Do the European League Against Rheumatism (EULAR) Sjögren’s syndrome outcome measures correlate with impaired quality of life, fatigue, anxiety and depression in primary Sjögren’s syndrome? Arch Med Sci. 2018;14(4):830–837. doi: 10.5114/aoms.2017.70300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strömbeck B, Ekdahl C, Manthorpe R, Jacobsson LT. Physical capacity in women with primary Sjögren’s syndrome: a controlled study. Arthritis Rheum. 2003;49(5):681–688. doi: 10.1002/art.11384 [DOI] [PubMed] [Google Scholar]
- 8.Hackett KL, Newton JL, Frith J, et al. Impaired functional status in primary Sjögren’s syndrome. Arthritis Care Res. 2012;64(11):1760–1764. doi: 10.1002/acr.21738 [DOI] [PubMed] [Google Scholar]
- 9.Karabul E, Borekci S, Ugurlu S, Musellim B. The frequency of obstructive sleep apnea in patients with primary Sjogren’s syndrome. Sleep Breath. 2022;26(4):1583–1591.PMID: 34773202; PMCID: PMC8589227. doi: 10.1007/s11325-021-02491-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aparicio-Soto M, Sánchez-Hidalgo M, Alarcón-de-la-lastra C. An update on diet and nutritional factors in systemic lupus erythematosus management. Nutr Res Rev. 2017;30(1):118–137. doi: 10.1017/S0954422417000026 [DOI] [PubMed] [Google Scholar]
- 11.Shiboski CH, Shiboski SC, Seror R, et al. 2016 American college of rheumatology/European league against rheumatism classification criteria for primary Sjogren's syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 2017;69(1):35–45. doi: 10.1002/art.39859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. doi: 10.1177/2050312116671725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 14.Saglam M, Arikan H, Savci S, et al. International physical activity questionnaire: reliability and validity of the Turkish version. Percept Mot Skills. 2010;111(1):278–284. doi: 10.2466/06.08.PMS.111.4.278-284 [DOI] [PubMed] [Google Scholar]
- 15.Kyle UG, Bosaeusb I, Lorenzoc ADD, et al. Bioelectrical impedance analysis—part I: review of principles and methods. Clin Nutr. 2004;23(5):1226–1243. doi: 10.1016/j.clnu.2004.06.004 [DOI] [PubMed] [Google Scholar]
- 16.Dassouki T, Benatti FB, Pinto AJ, et al. Objectively measured physical activity and its influence on physical capacity and clinical parameters in patients with primary Sjögren’s syndrome. Lupus. 2017;26(7):690–697. doi: 10.1177/0961203316674819 [DOI] [PubMed] [Google Scholar]
- 17.Kim MH, Sung JH, Jin MN, et al. Impact of physical activity on all-cause mortality according to specific cardiovascular disease. Front Cardiovasc Med. 2022;9:811058. doi: 10.3389/fcvm.2022.811058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dardin LP, Garcia ABA, Minali PA, Pinto ACPN, Trevisani VFM. The effects of resistance training in patients with primary Sjogren’s syndrome. Clin Rheumatol. 2022;41(4):1145–1152. doi: 10.1007/s10067-021-05977-0 [DOI] [PubMed] [Google Scholar]
- 19.Fallon KE, Fallon SK, Boston T. The acute phase response and exercise: court and field sports. Br J Sports Med. 2001;35(3):170–173. doi: 10.1136/bjsm.35.3.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mattusch F, Dufaux B, Heine O, Mertens I, Rost R. Reduction of the plasma concentration of C-reactive protein following nine months of endurance training. Int J Sports Med. 2000;21(1):21–24. doi: 10.1055/s-2000-8852 [DOI] [PubMed] [Google Scholar]
- 21.Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol (1985). 2005;98(4):1154–1162. doi: 10.1152/japplphysiol.00164.2004 [DOI] [PubMed] [Google Scholar]
- 22.Hu H, Xu A, Gao C, Wang Z, Wu X. The effect of physical exercise on rheumatoid arthritis: an overview of systematic reviews and meta-analysis. J Adv Nurs. 2021;77(2):506–522. doi: 10.1111/jan.14574 [DOI] [PubMed] [Google Scholar]
- 23.Miyamoto ST, Valim V, Carletti L, et al. Supervised walking improves cardiorespiratory fitness, exercise tolerance, and fatigue in women with primary Sjögren’s syndrome: a randomized-controlled trial. Rheumatol Int. 2019;39(2):227–238. doi: 10.1007/s00296-018-4213-z [DOI] [PubMed] [Google Scholar]
- 24.Tench CM, McCarthy J, McCurdie I, White PD, D’Cruz DP. Fatigue in systemic lupus erythematosus: a randomized controlled trial of exercise. Rheumatology. 2003;42(9):1050–1054. doi: 10.1093/rheumatology/keg289 [DOI] [PubMed] [Google Scholar]
- 25.Sveaas SH, Smedslund G, Hagen KB, Dagfinrud H. Effect of cardiorespiratory and strength exercises on disease activity in patients with inflammatory rheumatic diseases: a systematic review and meta-analysis. Br J Sports Med. 2017;51(14):1065–1072. doi: 10.1136/bjsports-2016-097149 [DOI] [PubMed] [Google Scholar]
- 26.Strömbeck BE, Theander E, Jacobsson LT. Effects of exercise on aerobic capacity and fatigue in women with primary Sjogren’s syndrome. Rheumatology. 2007;46(5):868–871. doi: 10.1093/rheumatology/kem004 [DOI] [PubMed] [Google Scholar]
- 27.Alkhaldi EH, Battar S, Alsuwailem SI, Almutairi KS, Alshamari WK, Alkhaldi AH. Effect of nighttime exercise on sleep quality among the general population in Riyadh, Saudi Arabia: a cross-sectional study. Cureus. 2023;15(7):e41638.PMID: 37565115; PMCID: PMC10411382. doi: 10.7759/cureus.41638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alnawwar MA, Alraddadi MI, Algethmi RA, Salem GA, Salem MA, Alharbi AA. The effect of physical activity on sleep quality and sleep disorder: a systematic review. Cureus. 2023;15(8):e43595.PMID: 37719583; PMCID: PMC10503965. doi: 10.7759/cureus.43595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wendt A, da Silva ICM, Gonçalves H, Menezes A, Barros F, Wehrmeister FC. Short-term effect of physical activity on sleep health: a population-based study using accelerometry. J Sport Health Sci. 2022;11(5):630–638.PMID: 32422346; PMCID: PMC9532894. doi: 10.1016/j.jshs.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dardin LP, Garcia ABA, Gazoni FM, Santos FCD, Mello MT, Trevisani VFM. Correlation of sleep quality with fatigue and disease activity among patients with primary Sjögren’s syndrome: a cross-sectional study. Sao Paulo Med J. 2020;138(2):146–151. doi: 10.1590/1516-3180.2019.0251.R1.1912019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung SW, Hur J, Ha YJ, et al. Impact of sleep quality on clinical features of primary Sjögren’s syndrome. Korean J Intern Med. 2019;34(5):1154–1164. doi: 10.3904/kjim.2017.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cui Y, Li J, Li L, et al. Prevalence, correlates, and impact of sleep disturbance in Chinese patients with primary Sjögren’s syndrome. Int J Rheum Dis. 2020;23(3):367–373. doi: 10.1111/1756-185X.13678 [DOI] [PubMed] [Google Scholar]
- 33.Wang YF, Fan Z, Cheng YB, Jin YB, Huo Y, He J. 原发性干燥综合征患者睡眠障碍的相关影响因素 [Investigation of sleep disturbance and related factors in patients with primary Sjögren’s syndrome]. Beijing Da Xue Xue Bao Yi Xue Ban. 2020. 52(6):1063–1068. Chinese. Chinese. doi: 10.19723/j.issn.1671-167X.2020.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muscogiuri G, Barrea L, Annunziata G, et al. Obesity and sleep disturbance: the chicken or the egg? Crit Rev Food Sci Nutr. 2019;59(13):2158–2165. doi: 10.1080/10408398.2018.1506979 [DOI] [PubMed] [Google Scholar]
- 35.Vgontzas AN, Bixler EO, Basta M. Obesity and sleep: a bidirectional association? Sleep. 2010;33(5):573–574. doi: 10.1093/sleep/33.5.573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kawasaki Y, Kitamura E, Kasai T. Impact of body composition on sleep and its relationship with sleep disorders: current insights. Nat Sci Sleep. 2023;15:375–388. PMID: 37220427; PMCID: PMC10200107. doi: 10.2147/NSS.S340946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang Q, Wang X, Chen H, Shen B. Sjögren’s syndrome is associated with negatively variable impacts on domains of health-related quality of life: evidence from short form 36 questionnaire and a meta-analysis. Patient Prefer Adherence. 2017;11:905–911. doi: 10.2147/PPA.S132751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Demiral Y, Ergor G, Unal B, et al. Normative data and discriminative properties of short form 36 (SF-36) in Turkish urban population. BMC Public Health. 2006;6(1):247. doi: 10.1186/1471-2458-6-247 [DOI] [PMC free article] [PubMed] [Google Scholar]