Summary
Background
Health systems have a dual imperative to take action on climate change. First, they must develop climate resilient health services in response to the direct and indirect impacts of climate change on health. Second, they must reduce their own carbon footprint since health systems are a significant contributor to global greenhouse gas emissions.
Methods
An environmentally-extended multi-region input–output analysis was carried out, incorporating National Accounts data for Australia and annual expenditure data from WA Health for financial year 2019–20. Expenditure data were categorised to one of 344 economic sectors and by location of the provider of goods or services purchased.
Findings
WA Health contributes 8% of WA's total carbon footprint, driven by expenditure on chemicals (23.8% of total), transport (20.2% of total), and electricity supply (19.7% of total). These 3 sectors represent 63.7% of WA Health's carbon footprint, but only 10.8% of its total expenditure.
Interpretation
Reducing emissions related to health service provision in WA will require a holistic approach that leverages carbon footprinting insights and integrates them into organisational decision-making across all health programs. The high carbon-intensity of the transport and chemicals sectors supports previous research calling for a reduction in unnecessary pathology testing and the transition to delivery of non-urgent health care via sustainable models of telehealth. The impact of WA's size and location presents challenges, with a predominantly non-renewable energy supply and reliance on transport and supply chains from other states adding significantly to emissions.
Funding
The study received funding from the Australian Research Council, The University of Sydney, and the WA Department of Health. The full list of funding information can be found in Acknowledgements.
Keywords: Carbon footprint, Input–output analysis, Environmental impacts, Western Australia, GHG emissions
Research in context.
Evidence before this study
Environmental impacts such as greenhouse gas emissions, water scarcity, and air pollution arise from the delivery of health services. Previous studies have analysed the carbon footprint of health care at a global and national level, and for some sub-national regions. As the public health care provider in Australia's largest state, WA Health manages one of the largest geographical health jurisdictions in the world, covering an area of 2.5 million km2 and servicing a population of 2.7 million people.
Added value of this study
WA Health contributes 8% of Western Australia's carbon footprint, driven by its expenditure on chemicals, transport, and electricity supply. This study is the first of its kind assessment of an Australian state-based health sector organisation, as it utilises high resolution expenditure data to analyse the health system's greenhouse gas emissions. The use of high-resolution expenditure data in a state-level health care carbon footprint assessment reveals the significance of procurement decisions in reducing greenhouse gas emissions implicated in the supply chains that support the delivery of health services.
Implications of all the available evidence
Embedding carbon emission data into management at all levels of WA Health, increasing the delivery of non-urgent health care via sustainable models of telehealth, reducing unnecessary pathology testing, and sourcing products from locations with a low-carbon electricity grid can support the reduction of WA Health's carbon footprint.
Introduction
Climate change is affecting human health in increasingly severe, unpredictable, and visible ways.1 Human activity has increased the Earth's temperature by 1.1 °C since the start of the last century and the United Nations Intergovernmental Panel on Climate Change (IPCC) expects that warming will exceed 1.5 °C during this century, regardless of mitigation activities.2 Human health gains are severely threatened by climate change as access to safe, clean, secure environments is undermined. Direct health impacts include injuries and death from extreme events such as bushfires, floods, and heatwaves, while indirect impacts are mediated by air pollution, waterborne diseases, changing vector distribution, and food safety and insecurity.3,4 Climate change also exacerbates health inequities by disproportionatley affecting already vulnerable populations.4
Health systems have a dual imperative in relation to climate change. First, they must adapt and respond to the increased human health impacts due to climate-related events which will increase demand on services. Second, the far-reaching operational and social footprint of the health sector means that it is a significant contributor to greenhouse gas (GHG) emissions. Therefore, health systems must mitigate their own contribution to climate change to reduce the flow-on effects to the health of patients and populations that they serve.5
Previous research into the carbon footprint associated with delivery of health care across 36 countries has shown that, on average, it contributes 5.5% of the total national carbon footprint.6 A study of the carbon footprint of the English National Health Service (NHS) found that the majority of its GHG emissions (62%) were attributable to the supply chains which support clinical care, 24% were attributable to the direct delivery of care, 10% to staff commute and patient and visitor travel, and 4% to private health care services commissioned by the NHS.7 In Australia, expenditure on the health sector produces 7% of the national carbon footprint,8 while the health sector in New South Wales (NSW) contributes 6.6% of the state's GHG emissions.9
Western Australia (WA) is the largest state in Australia, spanning 2.5 million km2 with a population of 2.7 million people,10 and it is among the largest geographical areas in the world covered by a single health authority. Health care provision in WA is the responsibility of WA Health, comprised of the Department of Health and seven Health Service Providers.11 Accounting for 31% of WA Government expenditure in financial year 2019–20, the health sector has been identified as a key pillar in the WA Government's commitment to transition to a low-carbon economy, and an essential contributor in protecting the health of the community from the effects of climate change.11
To determine the most effective actions to deliver this commitment, it is important to understand the scale and characteristics of WA Health's GHG emissions—its carbon footprint. Previous studies of the health sector's carbon footprint have employed input–output analysis, which connects environmental impacts such as GHG emissions12 and material use13 to the economic activity that ultimately creates those impacts. These previous studies have faced data limitations, relying on publicly available information regarding expenditure directed to the health sector, rather than using a health organisation's own expenditure data as the key input to these calculations. For example, Pichler et al.6 used health sector expenditure data from the Organisation for Economic Co-operation and Development for the 36 countries studied. Similarly, the carbon footprint assessments of the Australian health sector8 and the sub-national analysis of the NSW health sector9 relied on national health expenditure data from the Australian Institute of Health and Welfare.
In this study, we calculate WA Health's carbon footprint utilising input–output methodology and high-resolution expenditure data sourced directly from internal accounts for the 2019–20 financial year. This provides the most detailed assessment to date of any Australian health care system at a state level, and minimises the limitations associated with estimating expenditure values directed to each of the 344 economic sectors included in the input–output tables. The carbon footprint presented here is calculated based on the point at which WA Health spends money on the goods and services that support its operations, rather than at the point at which the patient spends money on the health care system, as has been the case in previous studies.
Methods
The carbon footprint for WA Health was calculated using environmentally-extended input–output methodology which connects an environmental impact (in this case, GHG emissions) to the monetary transactions within a given economic system for a given year. To do this, we built a custom multi-region input–output (MRIO) table using the Australian Industrial Ecology Laboratory (AusIELab),14 featuring information on monetary transactions taking place between the eight states and territories in Australia and 344 industry and commodity sectors across the Australian economy.
Data
The custom-built MRIO table for financial year 2019–20 included three matrices. The first, the intermediate demand matrix (T), provided information on the value of economic transactions between each of the 5504 (344 industries + 344 commodities x 8 regions) region–sector combinations included in the MRIO table for that year. The 344 sectors that form the basis for this MRIO include all goods and services available for purchase by individuals, businesses, or government agencies within Australia. Next, the final demand matrix (Y) provided information on the total final demand for each of these region–sector combinations. Finally, the satellite matrix (Q) provided information on the 2020 GHG emissions associated with each of the 5504 region–sector combinations, measured in tonnes of CO2 equivalent (CO2-e).
Expenditure data for the 2019–20 financial year were obtained from the internal accounting records of WA Health. Initially, these were categorised according to WA Health's internal account codes and the state or territory where the expenditure was directed. In order to connect this expenditure to the MRIO table built within the AusIELab, a concordance matrix was created to allocate each of the WA Health account codes to one or more of the 344 economic sectors which form the basis of the MRIO table. This concordance matrix was used to generate a customised expenditure vector yWAH (where WAH represents WA Health) for use in the input–output assessment described below.
This customised expenditure vector, yWAH, captured all money spent by WA Health within Australia during the 2019–20 financial year in order to run its operations. This included expenditure on a wide range of goods such as prostheses, pharmaceuticals, food, chemicals, medical consumables, and equipment. Expenditure on services such as patient transport, facilities management, waste removal, linen supply and laundering, and other outsourced services was also included. This expenditure data was a key input to the input–output analysis described in the following section, which calculated results for each of the 344 economic sectors included in the MRIO table. These results were aggregated to higher level sectors for ease of presentation, with information on the sectors included in these aggregations available in the Supplementary Material.
Data analysis
These data were used as inputs to mathematical calculations using input–output methodology, widely used in carbon footprint assessments.6,8,12,15,16 This mathematical technique connects the greenhouse gases emitted at the point of production of a product, or delivery of a service, to the economic activity that creates the demand for that product or service. It takes advantage of the rigorous financial accounts kept by countries under the System of National Accounts framework17 to generate the required MRIO tables, and the reporting of Nationally Determined Contributions required under the Paris Agreement18 to provide GHG emissions data. When coupled with an entity's operating accounts, such as those provided by WA Health, this technique calculates the GHG emissions attributable to that entity's expenditure on products and services, emissions that accumulate along the supply chain transactions that support the delivery of those products and services to WA Health.
Input-output methodology is built around the Leontief Inverse (L), a matrix which provides information on the interdependencies within the economic system quantified by a given MRIO table. Once the custom-built MRIO table was generated, the Leontief Inverse (L) was calculated in a number of steps. First, the total output vector x for the economic system represented in the MRIO table was calculated from the summation of the intermediate demand matrix T and the final demand matrix Y. This output vector x was then diagonalised and inverted to provide −1 which, when multiplied by the intermediate demand matrix T, provided the direct requirements matrix A. Finally, the Leontief Inverse L was calculated according to Equation (1), where I is an identity matrix with dimensions equal to those of A.
| Equation (1) |
Once the Leontief Inverse (L) was calculated, it was used to connect the GHG emissions data represented in the satellite matrix (Q) with the expenditure data provided in the customised expenditure vector yWAH, according to Equation (2).
| Equation (2) |
where fWAH represents the carbon footprint associated with WA Health's expenditure and q represents the direct intensities matrix, calculated by multiplying the satellite matrix Q with −1.
Data limitations
The need to allocate expenditure by an entity to the economic sectors included in the MRIO table introduces limitations to any input–output analysis, since the sector taxonomies used by entities and those used by the statistical agencies that provide national accounts data are designed for different purposes. In this research, the sector taxonomy used in WA Health's internal reporting framework included 83 different account codes, which needed to be mapped to the 344 sectors included in the Australian MRIO. In many cases this mapping was straightforward with, for example, the WA Health account codes for accommodation mapped to the MRIO sector ‘Accommodation’, and the WA Health account code for bank fees mapped to the MRIO sector ‘Banking’.
In some cases, there was not a direct match available between sectors, such as the ‘Gas Power Water’ account code which needed to be pro-rated to three sectors within the MRIO: ‘Electricity supply’; ‘Gas supply’; and ‘Water supply: sewerage and drainage services’. In other cases, multiple WA Health account codes were mapped to just one of the MRIO sectors, reducing the ability to isolate the carbon footprint associated specifically with these account codes. The most notable example of this was the MRIO's ‘Business services’ sector, which includes the account codes related to all outsourced services such as facilities management, security management, administration, and waste management.
Other limitations may be introduced through the internal accounting procedures used by WA Health to allocate each expense to the appropriate internal account code. If there are errors in the allocation of expenses, these will be propagated through the input–output analysis since this expenditure is the key driver of the footprint results. Given the rigorous accounting procedures and guidelines in place for public health care in Australia as part of the Australian Hospital Patient Costing Standards,19 this limitation is not expected to be material.
Limitations associated with the creation of MRIO tables using national input–output tables, such as those used in this research, have been discussed in detail previously,20,21 and are not explored further here.
Ethics approval
No ethics approval was required for this study as it utilised routinely collected financial data. The purpose of this data is for the management of WA Health operations. No patient data or personally identifiable information was accessed or used in this study.
Role of the funding source
This work was partly funded by the WA Department of Health to enable development of a concordance of financial data with the AusIELab sectoral structure. WA Department of Health staff provided advice on the correct interpretation of financial data codes; however, the researchers remained independent of the funder. No authors received payment from a pharmaceutical company or other agency. All authors had access to the data used in the study and accept responsibility for the decision to submit the manuscript for publication.
Results
Our analysis quantified the total GHG emissions, or carbon footprint, for WA Health at 6578 kilotonnes (kt) of carbon dioxide equivalent (CO2-e) for the 2019–20 financial year. In the same year, total GHG emissions for the state of WA were 82,116 kt CO2-e,22 which puts WA Health's carbon footprint at an estimated 8% of the state's total, and an estimated 1.3% of Australia's total emissions. This is consistent with previous research demonstrating that the health sector contributes 6.6% of the total emissions of NSW,9 7% of the total emissions of Australia,8 and between 1.5% and 10% of emissions worldwide.6,23
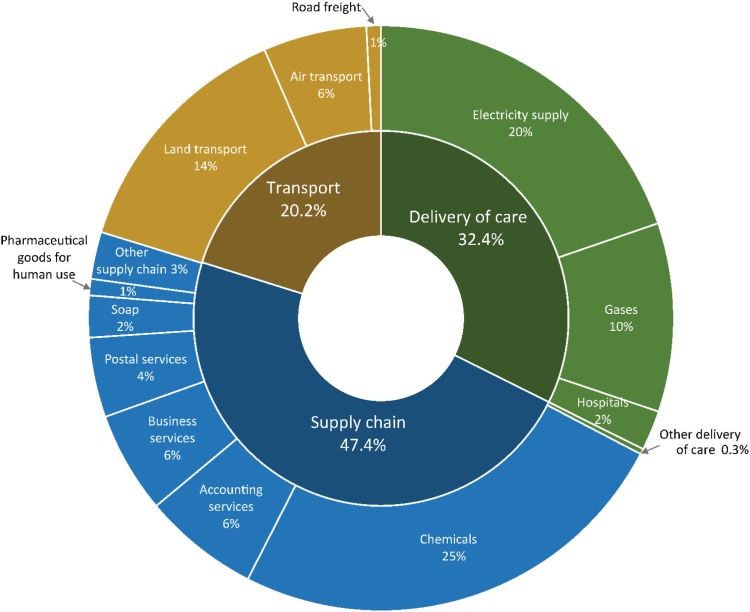
Examination of these emissions in more detail provides information on the contribution that expenditure on each economic sector makes to WA Health's total carbon footprint. These sectors can be grouped into three overarching categories based on the degree of direct control the organisation has over the emissions and the location of the emissions7: Delivery of care, which contributes 32.4% of the total footprint and includes all emissions directly associated with the treatment of patients; Supply chain, which contributes 47.4% of the total footprint and incudes all emissions generated by the manufacture and delivery of products and services of suppliers upstream of the point at which care is delivered; and Transport, which contributes 20.2% and includes the intra- and inter-state movements of patients, staff, and goods. At an economic sector level, the top 12 sectors contributed 96.7% of WA Health's carbon footprint, with the highest contribution coming from expenditure on chemicals, at 24.8%. Fig. 1 illustrates the breakdown of WA Health's total carbon footprint by economic sector, and by category. The footprint generated by the top 12 sectors is also presented in Table 1, which includes a comparison of each sector's contribution to WA Health's carbon footprint alongside the share it represents of WA Health's expenditure. Information on the sub-sectors included in each of the aggregated sectors presented in Fig. 1 is available in the Supplementary Material.
Fig. 1.
Breakdown of WA Health's carbon footprint by sector and by category. Sectors have been categorised into: delivery of care, which includes all emissions directly associated with the treatment of patients; supply chain, which includes all the upstream activity required to enable delivery of care; and transport.
Table 1.
Comparison of contribution to carbon footprint and share of total expenditure for the top 12 economic sectors contributing to WA Health's carbon footprint.
| Rank | Sector | Footprint (kt CO2-e) | % emissions | % expenditure |
|---|---|---|---|---|
| 1 | Chemicals | 1629 | 24.8% | 0.7% |
| 2 | Electricity supply | 1298 | 19.7% | 1.3% |
| 3 | Land transport | 902 | 13.7% | 8.2% |
| 4 | Gases | 682 | 10.4% | 0.3% |
| 5 | Accounting services | 420 | 6.4% | 1.8% |
| 6 | Air transport | 374 | 5.7% | 0.2% |
| 7 | Business services | 369 | 5.6% | 14.7% |
| 8 | Postal services | 287 | 4.4% | 0.1% |
| 9 | Soap and other detergents | 151 | 2.3% | 0.3% |
| 10 | Hospitals and nursing homes | 142 | 2.2% | 47.4% |
| 11 | Pharmaceutical goods for human use | 59 | 0.9% | 0.3% |
| 12 | Road freight | 51 | 0.8% | 0.4% |
These 12 sectors contribute 96.7% of WA Health's total carbon footprint and represent 75.8% of expenditure.
Some activities undertaken to support WA Health's operations occur in locations outside WA. Table 2 provides a comparison of the proportion of expenditure directed at each state and territory compared to its share of WA Health's carbon footprint. An interesting finding here is that regions where the ratio of emissions to expenditure is higher (such as Queensland and Victoria) are also states where the electricity grid is more dependent on fossil fuels.24 These states have higher carbon intensity in their supply chains, and therefore more carbon is embodied in the goods and services sourced from suppliers based there. On the other hand, there are lower emissions despite higher expenditure in regions such as South Australia and the Australian Capital Territory, where renewable energy is a greater component of the electricity grid.18
Table 2.
Comparison of contribution to carbon footprint and total expenditure for each state and territory.
| State or territory | Footprint (kt CO2-e) | % emissions | % expenditure |
|---|---|---|---|
| Western Australia (WA) | 5138 | 78.1% | 72.0% |
| New South Wales (NSW) | 712 | 10.8% | 17.4% |
| Victoria (VIC) | 497 | 7.6% | 7.3% |
| Queensland (QLD) | 186 | 2.8% | 1.4% |
| South Australia (SA) | 26 | 0.4% | 0.9% |
| Australian Capital Territory (ACT) | 16 | 0.2% | 1.1% |
| Tasmania (TAS) | 3 | 0.0% | 0.1% |
| Northern Territory (NT) | 0 | 0.0% | 0.0% |
| Total | 6578 | 100% | 100% |
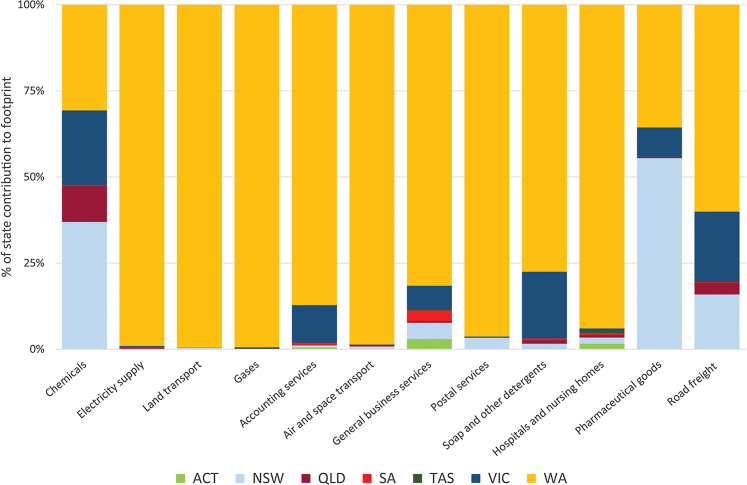
Considering WA Health's carbon footprint by region provides insights into the contribution of different states and territories to the carbon footprint associated with each economic sector, as illustrated in Fig. 2. Two of the top 12 sector contributors to WA Health's carbon footprint were the Chemicals and Pharmaceutical goods sectors, both of which have strong supply chain links to NSW and Victoria. The Road freight sector also has a high attribution to NSW and Victoria; however, it is worth noting that intra-state road freight within WA still accounts for the majority (58.8%) of emissions attributable to this sector.
Fig. 2.
Breakdown by region of expenditure for the top 12 economic sectors contributing to WA Health's carbon footprint.
Discussion
Health systems have substantial carbon footprints due to the broad scope of their operations. This includes: managing large campuses at multiple sites across wide geographical areas; operating continuously and consuming environmental resources for heating, cooling, water supply, and waste disposal; transporting patients and goods; and purchasing supplies and commissioning services from other organisations. The sources of GHG emissions for the WA Health system reflect common patterns seen in other health systems6, 7, 8, 9 with some additional findings due to the unique operating environment for delivering health services in Western Australia.
The transport sector makes a substantial contribution to WA Health's GHG emissions, at 20.2% of the total. This is not unexpected given WA's geographic size, with health services being delivered across an area of more than 2.5 million km2. WA Health also relies on supply chains based in eastern states, which further increases the contribution of transport to its carbon footprint. Importantly, this analysis was based on expenditure by WA Health, and therefore it does not include GHG emissions generated by staff commuting to work or people visiting patients in hospital. Some transport services such as road freight may represent an unavoidable expenditure due to the vast geographic area and dispersed populations served by WA Health. However, the underlying need creating the demand for other transport services, such as movement of patients for non-urgent care, could be met through other means such as sustainable models of telehealth, which have been shown to reduce emissions with minimal adverse outcomes for some conditions.25,26 Virtual or digitally enabled patient care pathways, such as Royal Perth Hospital's Hospital in Virtual Environments (HIVE) program27 also have the potential to reduce emissions, although such programs must be designed carefully to avoid inadvertently introducing inequities and additional emissions.
The Chemicals sector also presents an opportunity for emissions reductions, as it generates 24.8% of the total carbon footprint but only comprises 0.7% of total expenditure. Products within this sector include diagnostic supplies, reagents, and culture media used in the pathology laboratory setting. The over-use of pathology testing in a clinical setting has been linked to low value care,28 and a reduction in the number of unnecessary pathology tests has been identified as a potential avenue for reducing the carbon footprint of clinical care.28,29 The results presented here would support this focus area and indicate that, over time, a reduction in expenditure on the chemical products that support pathology testing would facilitate a reduction in WA Health's carbon footprint. This approach can assist in bringing the carbon footprint into clinical decision-making, and assist health managers to achieve sustainable value in healthcare, defined by Mortimer and colleagues as creating positive outcomes for patients and populations while considering the ‘triple bottom line’ of environmental, social, and financial impacts.30
Electricity supply to WA Health also generates a significant share of the total carbon footprint, at 19.7%. This presents a short-term challenge in achieving reductions, since the energy system in WA remains fossil fuel dependent, with only 15% of electricity generated from renewable energy sources.24 However, WA Health's facilities can invest in energy efficiency measures to reduce their emissions from electricity expenditure, as well as identify opportunities for electrification of sites in anticipation of the WA government's commitment to lower-emissions electricity and a decarbonised, renewable energy supply.31 The difference in carbon intensity of the electricity grid in other states and territories presents another potential avenue for reducing the carbon footprint associated with WA Health's supply chains. As seen in Fig. 2 and 69% of the carbon footprint attributable to the supply of chemicals is generated in NSW, VIC, and QLD, all of which have high carbon intensity electricity grids.24 Procuring from suppliers based in less carbon intensive regions, such as SA, TAS and the ACT, may reduce the carbon footprint associated with WA Health's supply chains.
Conclusion
This study of an Australian state-based health sector organisation utilises high resolution expenditure data to analyse the health system's greenhouse gas emissions. Our assessment has identified “carbon hotspots”—the economic sectors and locations of expenditure that make the greatest contribution to the GHG emissions generated by the provision of health services by WA Health.
These findings present an opportunity for WA Health to take a holistic approach to carbon emissions reduction by implementing specific initiatives to target the transport, energy, and chemicals sectors and to review its supply chain. These insights may be useful in developing a long-term program which allows WA Health to realise its potential to lead the state of Western Australia in its transition to a low carbon economy, while simultaneously protecting the health of the community from the effects of climate change.
Contributors
AM, AV, CB, and SJ conceptualised the study; AI, AM, and AV developed the data concordance; AI carried out data manipulation and analysis; CB and AI drafted the original manuscript, and all authors contributed to the final manuscript.
Data sharing statement
The input–output table used to carry out the study is based on Australia's national input output tables, which are available from the Australian Bureau of Statistics at this link: https://www.abs.gov.au/statistics/economy/national-accounts/australian-national-accounts-input-output-tables/2019-20.
Expenditure data from WA Health is proprietary and not available for sharing.
Declaration of interests
The authors declare no conflicts of interest. The author's views are their own and not necessarily those of the Western Australian State Government or WA Department of Health.
Acknowledgements
The authors would like to thank the staff at the WA Department of Health who provided their advice on the correct interpretation of financial data codes. This work was supported by the Australian Research Council through its Discovery Project DP200103005, Discovery Early Career Researcher Award DE230101652, Linkage Project LP200100311 and ARC Research Hub IH190100009, and a University of Sydney SOAR Prize. This work was partly funded by the WA Department of Health to enable development of a concordance of financial data with the AusIELab sectoral structure. WA Department of Health staff provided advice on the correct interpretation of financial data codes; however, the researchers remained independent of the funder.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2024.101115.
Appendix A. Supplementary data
References
- 1.Haines A., Ebi K. The imperative for climate action to protect health. N Engl J Med. 2019;380(3):263–273. doi: 10.1056/NEJMra1807873. [DOI] [PubMed] [Google Scholar]
- 2.IPCC . 2023. Synthesis report of the IPCC sixth assessment report (AR6): summary for policymakers. [Google Scholar]
- 3.Patel L., Conlon K.C., Sorensen C., et al. Climate change and extreme heat events: how health systems should prepare. NEJM Catalyst. 2022;3(7) CAT.21.0454. [Google Scholar]
- 4.Watts N.M.A., Adger W.N.P., Agnolucci P.P., et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386(10006):1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 5.Charlesworth K., Stewart G., Sainsbury P. Addressing the carbon footprint of health organisations: eight lessons for implementation. Public Health Res Pract. 2018;28(4):2841830. doi: 10.17061/phrp2841830. [DOI] [PubMed] [Google Scholar]
- 6.Pichler P.-P., Jaccard I.S., Weisz U., Weisz H. International comparison of health care carbon footprints. Environ Res Lett. 2019;14(6) [Google Scholar]
- 7.Tennison I., Roschnik S., Ashby B., et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):e84–e92. doi: 10.1016/S2542-5196(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik A., Lenzen M., McAlister S., McGain F. The carbon footprint of Australian health care. Lancet Planet Health. 2018;2(1):e27–e35. doi: 10.1016/S2542-5196(17)30180-8. [DOI] [PubMed] [Google Scholar]
- 9.Malik A., Padget M., Carter S., et al. Environmental impacts of Australia's largest health system. Resour Conserv Recycl. 2021;169 [Google Scholar]
- 10.Australian Bureau of Statistics Snapshot of Western Australia. 2022. https://www.abs.gov.au/articles/snapshot-wa-2021
- 11.Weeramanthri T.S.J.S., Bowman F., Bangor-Jones R., Law C. Final Report; Perth: 2020. Climate health WA inquiry. [Google Scholar]
- 12.Hertwich E., Peters G. Carbon footprint of nations: a global, trade-linked analysis. Environ Sci Technol. 2009;43(16):6414. doi: 10.1021/es803496a. [DOI] [PubMed] [Google Scholar]
- 13.Wiedmann T.O., Schandl H., Lenzen M., et al. The material footprint of nations. Proc Natl Acad Sci U S A. 2015;112(20):6271. doi: 10.1073/pnas.1220362110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenzen M., Geschke A., Malik A., et al. New multi-regional input-output databases for Australia - enabling timely and flexible regional analysis. Econ Syst Res. 2017;29(2):275–295. [Google Scholar]
- 15.Leontief W. Quantitative input and output relations in the economic systems of the United States. Rev Econ Stat. 1936;18(3):105–125. [Google Scholar]
- 16.Lenzen M., Malik A., Li M., et al. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020;4(7):e271–e279. doi: 10.1016/S2542-5196(20)30121-2. [DOI] [PubMed] [Google Scholar]
- 17.United Nations Statistics Division . 2008. System of national accounts. New York. [Google Scholar]
- 18.UNFCCC . United Nations; Paris: 2015. Paris agreement. [Google Scholar]
- 19.IHACPA Australian hospital patient costing standards version 4.2. 2023. https://www.ihacpa.gov.au/resources/australian-hospital-patient-costing-standards-version-42
- 20.Geschke A., Hadjikakou M. Virtual laboratories and MRIO analysis – an introduction. Econ Syst Res. 2017;29(2):143–157. [Google Scholar]
- 21.Wood R., Hawkins T.R., Hertwich E.G., Tukker A. Harmonising national input-output tables for consumption-based accounting - experiences from EXIOPOL. Econ Syst Res. 2014;26(4):387–409. [Google Scholar]
- 22.Department of Climate Change Energy the Environment and Water Australia's national greenhouse accounts. 2020. https://greenhouseaccounts.climatechange.gov.au/
- 23.Health Care Without Harm . 2019. Health care's climate footprint. [Google Scholar]
- 24.Department of Climate Change Energy the Environment and Water Australian energy statistics by state and territory. 2023. https://www.energy.gov.au/publications/australian-energy-statistics-state-and-territory
- 25.Blenkinsop S., Foley A., Schneider N., Willis J., Fowler H.J., Sisodiya S.M. Carbon emission savings and short-term health care impacts from telemedicine: an evaluation in epilepsy. Epilepsia. 2021;62(11):2732–2740. doi: 10.1111/epi.17046. [DOI] [PubMed] [Google Scholar]
- 26.Donald N., Irukulla S. Greenhouse gas emission savings in relation to telemedicine and associated patient benefits: a systematic review. Telemed J E Health. 2022;28(11):1555–1563. doi: 10.1089/tmj.2022.0047. [DOI] [PubMed] [Google Scholar]
- 27.East Metropolitan Health Service Hive – health in a virtual environment. 2023. https://emhs.health.wa.gov.au/Hospitals-and-Services/Services/HIVE
- 28.Barratt A.L., Bell K.J.L., Charlesworth K., McGain F. High value health care is low carbon health care. Med J Aust. 2022;216(2):67–68. doi: 10.5694/mja2.51331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McAlister S., Barratt A.L., Bell K.J.L., McGain F. The carbon footprint of pathology testing. Med J Aust. 2020;212(8):377–382. doi: 10.5694/mja2.50583. [DOI] [PubMed] [Google Scholar]
- 30.Mortimer F., Isherwood J., Wilkinson A., Vaux E. Sustainability in quality improvement: redefining value. Future Healthc J. 2018;5(2):88–93. doi: 10.7861/futurehosp.5-2-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Government of Western Australia Leading Western Australia's brighter energy future. Energy Transformation Strategy State. 2021;2:2021–2025. https://www.wa.gov.au/system/files/2021-07/Energy-Transformation-Strategy-Stage2-July2021.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.