Abstract
Bleeding is a very rare complication of Fasciola species (F. hepatica or F. gigantica) infection. We present here three cases of subcapsular liver bleeding caused by the hepatic phase of Fasciola spp. infection in patients, two of whom were women, aged 22, 66, and 84 years in Diyarbakir Province, southeastern Turkey. They had symptoms of right upper quadrant pain (n = 3), nausea (n = 1), and vomiting (n = 2) for periods ranging from 6 hours to 15 days. All patients with clinical presentations ranging from moderate abdominal pain to hypovolemic shock and ischemic hepatitis were improved with supportive treatment without the need for surgery. They showed complete clinical and laboratory recovery after triclabendazole administration in their follow-up. In conclusion, Fasciola spp. infection should be considered in the etiology of bleeding from liver disease.
Keywords: Fasciola hepatica, Hemorrhage, Liver disease, Shock
Introduction
Fascioliasis is an infection caused by liver flukes, Fasciol hepatica, or F. gigantica. Fascioliasis has a broad geographic distribution and the majority of cases have been reported from a few discrete regions of the world (1). Human fascioliasis is a rare disease and infection most commonly involves the liver. The liver infection has an acute hepatic phase and a chronic biliary phase. Initially, signs and symptoms of the acute hepatic phase are abdominal pain located in the upper quadrant, fever, mild hepatomegaly, eosinophilia, and mildly elevated liver enzymes. Intermittent right upper quadrant pain with or without cholestasis is a prominent feature of chronic biliary phase (1–3).
Atypical clinical manifestations, such as acute pancreatitis (2), extrahepatic fascioliasis with peritoneal malignancy tumor feature, subcapsular hepatic hematoma (1,4,5) and multiple brain hemorrhages and hematomas associated with ectopic fascioliasis in brain and eye, have been reported previously (6).
We present three cases with severe bleeding complicated from the acute hepatic phase of Fasciola spp. infection.
Case reports
The clinical, laboratory, and radiological features of the patients were evaluated according to the 2008 Helsinki Declaration principles. Written informed consent was obtained from all patients.
Case 1
A 68-year-old woman was admitted to the Dicle University Faculty of Medicine Hospitals Emergency Department (Diyarbakır – Turkey) with sudden onset right upper abdominal pain radiating to the right shoulder, deterioration in general condition, nausea, and vomiting for 6 hours,. The pain was sharp and continuous. She had no remarkable medical history. On admission, a physical examination showed a patient in acute distress with a tired appearance. Her axial temperature was 36.9 0C, her blood pressure was 70/40 mmHg, her pulse rate was 110 beats/minute, and her respiration rate was 24 times per minute. The chest was clear and cardiac examination was unremarkable. Abdominal examination revealed moderate right upper quadrant tenderness and 5 cm hepatomegaly below the right costal margin.
Initial laboratory tests were significant for anemia (hemoglobin: 7.5 g/dL), elevated liver enzymes [alanine aminotransferase 852 U/L, (normal range: 10–35 U/L), aspartate aminotransferase 1104 U/L, (normal range:10–40 U/L), alkaline phosphatase 600 U/L (normal range:40–150 U/L), gamma-glutamyl transferase 350 U/L, (normal range 9–64 U/L)] and elevated lactate dehydrogenase (LDH) 1140 U/L (normal range:125–234 U/L). Micro ELISA test was positive for Fasciola spp. antibody.
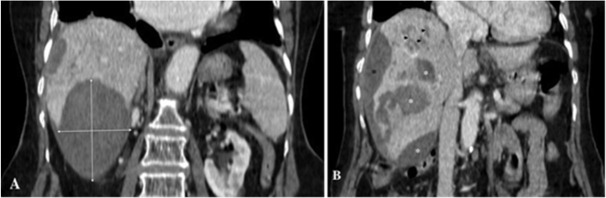
Abdominal ultrasonography revealed a large sub-capsular liver hematoma causing compression of the underlying liver parenchyma. No source for the hemorrhage was evident. Contrast enhancement computerized tomography scan of the abdomen showed a subcapsular (19x5 cm) hematoma on the right lobe (Fig.1 A, black line), multiloculated irregular lesions through both the left lobe and right lobe (Fig. 1 A, black arrows), and subcapsular tubular branching lesions (Fig. 1 B, black arrow) in the left lobe of the liver.
Fig. 1:
A–B. Axial section of contrast-enhanced abdominal CT showing large sub-capsular liver hematoma in the right lobe (A, black line) and multiloculated irregular lesions through both left lobe and right lobe (A, black arrows) and subcapsular tubular branching lesions (Fig. 1 B, black arrows) in the left lobe of the liver.
Initially ultrasound-guided fine needle aspiration was performed to exclude abscess or hematoma complicated by secondary infection. Aspiration material consisted of pure partially defibrinized blood and the culture of aspirate was negative. We considered the diagnosis of fasciolosis infection based on tomographic findings and the positivity of antibody against Fasciola (DRG IgG ELISA, DRG International, Inc., New Jersey, USA). Initially patient was treated conservatively by intravenous fluid and blood replacement (2 packed red cells). ). Triclabendazole (Egaten, Novartis Pharma, Switzerland) 10 mg/kg for two days was given (7). Complete recovery of hypovolemic shock was observed three days after the initiation of fluid and blood replacement therapy. Serum aminotransferase and LDH levels were returned to normal levels one week after admission to the hospital.
The patient was discharged without any symptoms or complications. Contrast enhancement abdominal CT examination showed significant regression in sub-capsular hematoma and liver lesions two months later.
The diagnosis of hypovolemic shock and ischemic hepatitis caused by sub-capsular hematomas complicated from the hepatic phase of Fasciola spp. infection was confirmed by clinical features, laboratory, and radiological findings.
Case 2
An 84-year-old woman was admitted to the Dicle University Faculty of Medicine Hospitals Gastroenterology Department (Diyarbakır – Turkey) with sudden onset and constant right upper abdominal pain radiating to the epigastrium and right shoulder, deterioration in general condition, and nausea for 48 hours. She had a history of recurrent urticarial eruption for two weeks. The physical examination at admission revealed a severe anemic appearance. Her axial temperature was 37 °C, her blood pressure was 100/60 mmHg, her pulse rate was 96 beats/minute, and her respiration rate was 22 times per minute. The chest was clear and cardiac examination was unremarkable. Abdominal examination revealed moderate right upper quadrant tenderness and 7 cm hepatomegaly below the right costal margin.
Initial laboratory tests were significant for anemia (hemoglobin: 8.5 g/dL), elevated white blood cell (20.000/mm3), eosinophilia (8.026/mm3), elevated erythrocyte sedimentation rate (46 mm/h), elevated liver enzymes (alanine aminotransferase 84 U/L, aspartate aminotransferase 70 U/L, alkaline phosphatase 470 U/L, gamma-glutamyl transferase 246 U/L, and elevated LDH 425 U/L). Micro ELISA test was positive for Fasciola antibody.
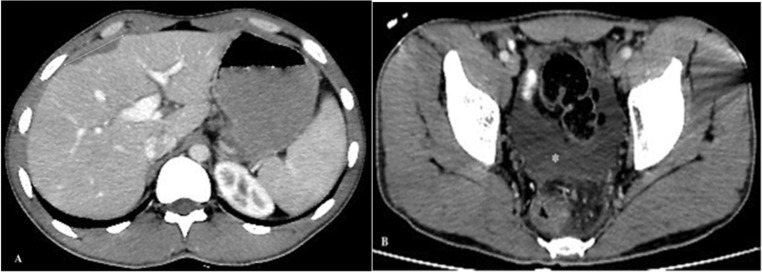
Abdominal ultrasonography revealed a large sub-capsular liver hematoma causing compression of the underlying liver parenchyma. No source for the hemorrhage was evident. Three phasic contrast enhancement computerized tomography scan of the abdomen showed large sub-capsular 9 cm in large diameter (Fig. 2A) and intraparenchymal hematoma on the right lobe (Fig. 2B, black asterisk), multiloculated irregular lesions through both left lobe and right lobe (Fig. 2B, white asterisk), and sub-capsular tubular branching lesions (Fig. 2B, black arrowheads) in the left lobe and right lobe of the liver.
Fig. 2:
A–B. The coronary section of three phasic contrast enhancement computerized tomography scan of the abdomen showed large sub-capsular 9 cm in large diameter (fig. 2A) and intraparenchymal hematoma on the right lobe (fig. 2B, black asterisk), multiloculated irregular lesions through both left lobe and right lobe (fig. 2B, white asterisk), and subcapsular tubular branching lesions (figure 2B, black arrows) in the left lobe and right lobe of the liver
We considered the diagnosis of Fasciola spp. infection based on clinical, laboratory, and tomographic findings. Initially patient was treated conservatively by intravenous fluid and blood replacement (2 packed red cells). Triclabendazole 10 mg/kg for two days was given. Complete recovery clinical findings were observed 15 days after admission to our clinic. Laboratory findings were returned to normal levels one week after admission to the hospital. Three months after triclabendazole administration, abdominal ultrasonographic examination showed prominent regression in subcapsular hematoma.
Case 3
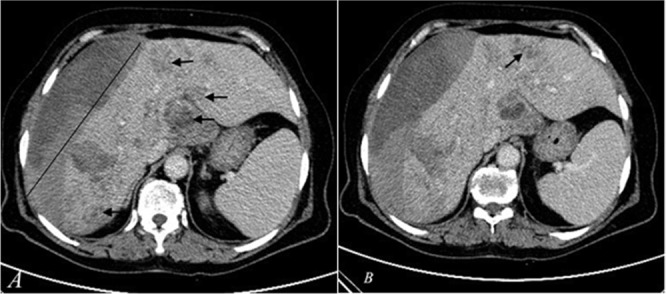
A 22-year-old male was admitted to the Dicle University Faculty of Medicine Hospitals Gastroenterology Department (Diyarbakır – Turkey) with right upper abdominal pain sometimes radiating to all abdomen for 15 days. He had a history of recurrent urticarial eruption for two weeks. He had no remarkable medical history. The physical examination at admission did not reveal any abnormality except mild tenderness on the right upper abdomen. Initial laboratory tests were significant for elevated WBC (12.680/mm3) and eosinophilia (4.448/mm3). Hemoglobin and hematocrit were within normal limits. Liver function tests were normal. Micro ELISA test was positive for F. hepatica antibody. Abdominal ultrasonography revealed a small fluid collection in the subcapsular space of the liver and a small intraperitoneal fluid collection. Three phasic contrast enhancement computerized tomography scans of the abdomen showed a small sub-capsular fluid collection (Fig. 3A, white arrow) at the right lobe of the liver and intraperitoneal fluid collection (Fig. 3B, white asterisk). We confirmed the presence of intraperitoneal and sub-capsular hemorrhage by ultrasound guidance fine needle aspiration. Triclabendazole 10 mg/kg for two days was given. Complete recovery of symptoms, and clinical and laboratory abnormalities were observed one month after admission to our clinic. Two months after triclabendazole administration, abdominal ultrasonography showed complete resolution of intraperitoneal hemorrhage and subcapsular hematoma.
Fig. 3:
A–B. The axial section of three phasic contrast enhancement computerized tomography scan of the abdomen showed a small sub-capsular fluid collection (fig. 3A, white arrow) at the right lobe of the liver and intraperitoneal fluid collection (fig. 3B, white asterisk)
Discussion
Fascioliasis is common in our region Southeast of Anatolia, Turkey (8). We presented two cases with isolated subcapsular liver hematomas and one case with subcapsular hematomas associated with intraperitoneal bleeding caused by the hepatic phase of Fasciola spp. infection.
Fascioliasis has a hepatic phase and a biliary phase, each phase has different clinical signs and symptoms. The hepatic phase begins with the slow migration of Fasciola hepatica through the liver parenchyma; the mature flukes digest and consume hepatocytes, dig tunnels and caves, and reside in the liver for months. The hepatic phase is characterized by fever with chills, upper abdominal pain, hepatomegaly, mild hepatitis, weight loss, and prominent eosinophilia (1–3). Sub-capsular hematomas and hemobilia have been reported in very rare cases (4,5). Diagnosis is confirmed by demonstrating live parasites or eggs in the bile or feces, specific radiological findings in CT, and the presence of anti-Fasciola antibody. Characteristic abdominal CT findings are multiple nodular lesions like micro-abscesses, tubular branching lesions, sub-capsular low-density areas surrounded by rim of parenchyma, solitary nodular lesions with hazy margins, and lymph node enlargement in the portal area. Triclabendazole at a dose of 10 mg/kg body weight is effective in about 80%–90% of patients (2,9). We confirmed fascioliasis infection by elevated eosinophilia, classical radiological findings, positivity of antibody against Fasciola spp., and complete response to triclabendazole.
Ischemic hepatitis is the result of any clinical condition in which hepatic blood-flow is not sufficient for the delivery of oxygen and nutrients for hepatocyte survival. It is characterized by a sudden and excessive elevation in liver transaminases and LDH associated with hypotension, hypoxia, and impaired tissue perfusion. Aminotransferases are usually higher than ten times the upper limit of normal (10–12). Tapper et al. have reported that the proportion of patients with documented hypotensive events of any duration is 52.9%. It is a common cause of severe acute liver injury and is associated with a significant risk of in-hospital death. In-hospital mortality associated with ischemic hepatitis is nearly 50% (13). There is no specific treatment for ischemic hepatitis. Early recognition and correction of underlying hemodynamic instability is the most important therapeutic modality. Normalization of transaminases and LDH usually occurs in a few days after recovery from underlying shock (13). One of our patients had classical clinical symptoms, physical examination findings, and laboratory abnormality compatible with ischemic hepatitis. We excluded all causes of acute hepatitis in our case. Abrupt and extreme elevation and normalization of liver enzymes and LDH associated with hypovolemic shock confirmed the diagnosis of ischemic hepatitis in our patients. To the best of our knowledge, this is the first case in the literature that presented with severe hemorrhage, hypovolemic shock, and ischemic hepatitis caused by Fasciola spp. infection.
Conclusion
Bleeding is an important complication of Fasciola spp. infection. In case of intra-abdominal bleeding caused by liver parenchymal lesions, the hepatic phase of Fasciola spp. infection should be considered.
Footnotes
Funding
This study received no funding.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- 1.Infantes LRR, Yataco GAP, Ortiz-Martínez Y, et al. The global prevalence of human fascioliasis: a systematic review and meta-analysis. Ther Adv Infect Dis. 2023; 10:20499361231185413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaya M, Beştaş R, Çetin S. Clinical presentation and management of Fasciola hepatica infection: single-center experience. World J Gastroenterol. 2011; 17:4899–4904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mas-Coma S, Valero MA, Bargues MD. Fascioliasis. Adv Exp Med Biol. 2019:1154:71–103. [DOI] [PubMed] [Google Scholar]
- 4.Leon M, Alave J, Alvarado R, Gotuzzo E, Terashima A, Seas C. A 52-year-old woman with a subcapsular liver hematoma. Clin Infect Dis. 2011; 52:1137, 1195–6. [DOI] [PubMed] [Google Scholar]
- 5.Kim SB, Kim TN, Kim KH. Fascioliasis: A rare cause of hepatic pseudoaneurysmal rupture. J Gastroenterol Hepatol. 2015;30:4. [DOI] [PubMed] [Google Scholar]
- 6.Zhou L, Luo L, You C, Wang B, Xu J, Liao L, Hui X, Cai B. Multiple brain hemorrhages and hematomas associated with ectopic fascioliasis in brain and eye. Surg Neurol. 2008;69: 516–521. [DOI] [PubMed] [Google Scholar]
- 7.El-Morshedy H, Farghaly A, Sharaf S, Abou-Basha L, Barakat R. Triclabendazole in the treatment of human fascioliasis: a community-based study. East Mediterr Health J. 1999;5(5):888–94. [PubMed] [Google Scholar]
- 8.Çiçek M, Yalçın K, Bilden A, Çakır F, Akpolat N. Evaluation of the seroprevalence and the demographic and clinical findings of fascioliasis patients in the Dicle River Basin in Turkey: a nine-year experience at a university hospital. Eur Rev Med Pharmacol Sci. 2023;27(22):10831–10838. [DOI] [PubMed] [Google Scholar]
- 9.Mohammed-Ghalehbin B, Chinifroush-Asl MM, Ramzi F. Extra-hepatic fascioliasis with peritoneal malignancy tumor feature. J Parasit Dis. 2012; 36:78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henrion J. Hypoxic hepatitis. Liver Int. 2012; 32:1039–1052. [DOI] [PubMed] [Google Scholar]
- 11.Fuhrmann V, Jager B, Zubkova A, Drolz A. Hypoxic hepatitis-epidemiology, pathophysiology and clinical management. Wien Klin Wochenschr. 2010; 122:129–139. [DOI] [PubMed] [Google Scholar]
- 12.Drolz A, Horvatists T, Roedl K, Fuhrmann V. Shock liver and cholestatic liver in critically ill patients. Med Klin Intensivmed Notfmed. 2014; 109:228–234. [DOI] [PubMed] [Google Scholar]
- 13.Tapper EB, Sengupta N, Bonder A. The incidence and outcomes of ischemic hepatitis: A systematic review with meta-analysis. Am J Med. 2015; 128:1314–1321. [DOI] [PubMed] [Google Scholar]