Abstract
Introduction
Dichoptic training has emerged as a promising rehabilitation approach for improving binocular visual function in patients with strabismus. A prospective observational study design was employed to assess the effectiveness of online video game-based dichoptic training in rehabilitating binocular visual function in patients who had undergone an operation for intermittent exotropia.
Methods
A total of 64 patients who had undergone an operation for intermittent exotropia were recruited and divided into the training group and the control group based on whether they would receive the dichoptic training. The dichoptic training was conducted for 3 months in the training group and the control group would not accept any form of orthoptic therapy. Assessments of binocular visual functions and deviation were conducted at baseline, 3-month and 6-month follow-up.
Results
Twenty-nine participants in the training group (mean 9.69 ± 2.66 years old) and 26 participants in the control group (mean 8.41 ± 2.64 years old) completed follow-up. At both 3- and 6-month follow-ups, the training group showed superior distance stereopsis compared to the control group, with near stereopsis only showing significant difference at the 6-month follow-up. Additionally, the training group exhibited significantly less distance exo-deviation drift than the control group at these times, and no significant difference was observed in near exo-deviation drift between the groups. The control group had a significantly higher rate of suboptimal surgical outcomes at both the 3- and 6-month follow-up. However, no significant differences were observed in simultaneous perception and fusion functions between the two groups.
Conclusions
Online video game-based dichoptic training has the potential to become a novel postoperative rehabilitation strategy for patients with intermittent exotropia.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40123-024-00978-z.
Keywords: Intermittent exotropia, Dichoptic visual training, Binocular vision, Video game
Key Summary Points
| Why carry out this study? |
| Dichoptic training presents a promising avenue for the restoration of binocular vision in the patients with intermittent exotropia after surgery, opening the door to novel rehabilitation techniques. However, the long-term efficacy of these methods is still unclear. |
| What was learned from the study? |
| Online video game-based dichoptic training, with good compliance, aids in the rehabilitation of stereopsis after surgery, while also limiting postoperative exo-deviation drift, and reducing the incidence rate of suboptimal surgical outcomes. |
| It may offer a non-invasive and supplementary method for enhancing outcomes in the patients with intermittent exotropia after surgery. |
Introduction
Intermittent exotropia (IXT), the most prevalent form of exotropia, had an incidence rate of approximately 1.93% in the population [1]. It is described as a form of strabismus that is not always present [2]. The deviation of the eye can be managed through the mechanisms of fusion, yet it often becomes noticeable during times of fatigue or when attention wavers. The threshold for surgical intervention in intermittent exotropia remains uncertain, but it is typically considered when there is a decline in the patient's ability to control eye alignment or stereopsis is compromised [3]. Some studies had revealed that although surgery corrected the eye position, a subset of patients did not experience restoration of binocular functions such as fusion and stereopsis [3–6], highlighting the need for postoperative visual function rehabilitation. Traditional vision training methods, which typically utilized devices such as synoptophore, vectorgrams, and stereoscopes, were criticized for being repetitive and dull, leading to low adherence among patients [7].
In recent years, visual training based on the video game and dichoptic paradigm has emerged as a promising approach for enhancing the visual functions of patients with strabismus and amblyopia [8–12]. This paradigm, in which each eye receives different images, helps stimulate binocular vision and restored binocular functions [13]. Tan et al. demonstrated that virtual reality-based binocular dichoptic training could ameliorate the perceptual eye position in children who had accepted strabismus surgery for correcting intermittent exotropia, indicating the potential of this intervention for improving binocular visual functions [6]. Similarly, Yang et al. found that short-term visual training using virtual reality or augmented reality could effectively improve stereopsis in patients with strabismus postoperatively, though the longevity of these improvements has yet to be determined [7]. Moreover, integrating video games into the training paradigms in these studies has rendered the process more captivating and engaging, offering an interactive and motivational platform for treatment.
In summary, dichoptic training holds a positive prospect for the rehabilitation of binocular visual functions in postoperative patients, potentially leading to the development of innovative rehabilitation strategies. Nevertheless, the long-term effects of these approaches remained uncertain. Consequently, this research utilized a prospective observational study framework to investigate the efficacy of an online video game-based binocular dichoptic training program in patients that underwent surgical correction for intermittent exotropia. All patients were recruited at the Zhongshan Ophthalmic Center from August 2017 to September 2019. They were divided into a control group (CG) and a training group (TG) based on whether they would receive the training and the differences in binocular visual functions between the two groups were assessed during the follow-up period.
Methods
Participants
A total of 64 patients who had undergone an operation for intermittent exotropia were recruited at the Zhongshan Ophthalmic Center from August 2017 to September 2019. The inclusion criteria were as follows: male or female patients aged 5 to 17 years with intermittent exotropia who had undergone corrective surgery and were successfully corrected 2 months prior (exotropia < 10 prism diopter (PD) of or esotropia ≤ 5 PD when fixating on distant and near targets using the prism-alternate cover test (PACT)). Exclusion criteria included patients with more than five PD vertical deviations or anisometropia (spherical equivalent refraction > 2.50 diopters), or nystagmus. More detailed eligibility criteria are presented in Table 1. In this study, researchers did not actively assign participants to groups or administer interventions; instead, participants self-selected into groups based on whether they chose to accept dichoptic training. The training group would undergo an online video game-based binocular dichoptic training with fully corrected glasses and the control group would not accept any form of orthoptic therapy. Written informed consent was obtained from each participant. This study adhered to the tenets of the Declaration of Helsinki, and the study protocol was reviewed and approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (Approved ID: 2017-38). Participants gave informed consent to participate in the study before taking part. This study was not registered, primarily because it began before such registration was commonly required. We acknowledge that the absence of registration may affect the study's perceived transparency and credibility. Consequently, we made sure to disclose all details of the study’s design, methods, and data processing fully and transparently during the publication process to enhance its integrity, and the study results were presented in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Table 1.
The inclusion and exclusion criteria
| Inclusion criteria |
|---|
| Male or female aged 5 to 17 years |
| The spherical equivalent of refraction for each eye should range from − 6.00 D to + 6.00 D* |
| Clinical diagnosis of intermittent exotropia |
| After ocular surgery for intermittent exotropia within 2 months |
| Baseline deviation range: esotropia ≤ 5△ or exotropia < 10△ at near and distance after surgery# |
| Best corrected visual acuity ≥ 20/25 |
| Exclusion criteria |
|---|
| Vertical deviation ≥ 5Δ at primary position# |
| Abnormal oblique or rectus |
| Nystagmus |
| Anisometropia > 2.5 diopters (spherical equivalent of refraction)* |
| With other ocular surgery history |
| With vision therapy history within 8 weeks |
| Epilepsy and other brain disorders |
*The spherical equivalent of refraction was calculated based on the results of the cycloplegic refraction examination
#The deviation was tested by the prism-alternate cover test
Study Design
The study consisted of pre-training assessment, online video game-based dichoptic training only for TG, and post-training assessment at 3- and 6-month follow-up. The dichoptic training was conducted on about 180 times for three months in the TG, with each session comprising 60 to 90 trials, lasting about 15 min. The CG would not accept any form of orthoptic therapy. Assessments of simultaneous perception, fusion, stereopsis, and deviation were conducted at baseline, 3-month, and 6-month follow-up. All patients had accepted refractive correction and wore appropriate glasses for a minimum of 3 months before undergoing surgery. The goal for myopia correction was full correction, while for hyperopia, the spherical component could be reduced at the investigator's discretion, adhering to the principle of maximizing plus power for optimal visual acuity. Regarding astigmatism, the cylinder needed to be within 0.25 diopters of full correction, with the axis within 5 degrees of full correction. Postoperatively, both the training and control groups continued to wear corrective glasses. Patients must have accepted refractive correction before conducting any visual function assessments.
Online Video Game-Based Dichoptic Visual Training
In our study, we utilized the SJ-RS-WL2015, an online video game-based dichoptic visual training software developed by Guangzhou Shijing Medical Software Co., Ltd., China. This software has received medical approval from the China Food and Drug Administration (CFDA). Initially, professional instructors would assist participants at the hospital, teaching them the installation and operation of this software. Each participant would receive a personal account after completing the instructional phase. Prior to commencing the training, they needed to input their test results encompassing simultaneous perception, fusion range, stereopsis, and deviation into the software. The software's adaptive algorithm would utilize this data to create a customized training regimen tailored to the specific needs of each participant. Participants were required to wear red-blue dichoptic glasses throughout the training. The training program includes elements of simultaneous vision, fusion function, and stereoscopic perception. It was presented in a fun, game-based format, with each aspect featuring dozens of different games, which ensures that participants remained interested throughout the training period. A selection of these games is already showcased in Figure S1. The system could automatically evaluate each session based on compliance and accuracy of their performance, grading on a scale from 1 to 5. Significant rating fluctuations (more than two levels) would prompt an ophthalmologist to conduct a follow-up with the patient to consider potential adjustments to their training plan [14]. For the best training experience, the recommended display settings are a monitor size of 14 inches or more, a refresh rate of 60 Hz, a resolution of 1920 × 1080, and 24-bit true color. The software could smartly acquire and adapt to these display settings and suggest an ideal training distance, which varies based on screen size—approximately 70 cm for a 23-inch screen, 60 cm for a 19-inch screen, and 45 cm for a 14-inch screen. Participants engaged in two training sessions daily, each lasting about 15 min. Finally, each individual in the training groups would complete around 180 sessions in total.
Measurements of Visual Function
Simultaneous Perception
The Worth 4-dot test in a dark room assessed simultaneous perception. Correcting refractive errors, participants wore red-green glasses and reported colors and numbers of lights (one red, two green, one white) shown by the apparatus at 33 cm and 5 m. These responses were carefully recorded. Seeing only green or red dots indicates suppression of the right or left eye, respectively, reflecting the absence of simultaneous perception.
Fusion
Fusion range was evaluated using a synoptophore. It presented two separate yet similar visual images individually to each eye. The subject was required to gradually adjust the relative position of these targets, and report whether they could merge the two separate images into a single image. When the subject successfully merged the images, the value displayed at this point was recorded as the fusion point. The examiner subsequently altered the relative positions of the two images from the fusion point in both converging and diverging directions. When the subject reported that the images had separated again, the value on the synoptophore at that moment was noted as the break point. The distance between the two break points represented the fusion range.
Stereopsis
Near stereoacuity was measured with the TNO test (Laméris Ootech B.V., Nieuwegein, The Netherlands) at a distance of 33 cm. The distance stereoacuity was measured using the Randot Stereoacuity Tests (Stereo Optical Co., Inc., Chicago, IL, USA) at a distance of 4 m, including disparities ranging from 60 to 400 arc-seconds with no monocular cues. All observers wore polarizing glasses, and the refractive error was corrected during the test. Nil stereopsis was recorded as 800″ for the distance and 960″ for the near [15].
Each measurement was repeated twice. A logarithmic transformation with a base of 10 was applied to the stereopsis measurement results.
Deviation
The prism alternate cover test measured participants' deviation at 33 cm and 6 m by observing initial eye alignment and movements towards a fixation target when alternatingly covering each eye. A prism corrected the deviation, and its strength, indicating the deviation angle, was recorded when no movement occurred upon switching covers. The exo-deviation drift is defined as the amount by which the current deviation decreases from the baseline deviation.
Data Analysis
The sample size was calculated based on the primary outcome (stereopsis at distance), the mean difference of stereoacuity at distance was expected to be 0.3 log arcsec between two groups with a common standard deviation of 0.2 log arcsec from previous studies [7, 16, 17]. After allowing for a maximum dropout rate of 20% during the 6 months follow-up, a sample size of 12 per group calculated using PASS 2021 (NCSS, LLC, Kaysville, UT, USA) was required to achieve 80% power at a two-sided significance level of 0.05 based on a two-sample t test.
Statistical analysis was conducted using Stata 15.1 (StataCorp LLC, College Station, TX, USA). Continuous variable data were reported as mean ± standard deviation. Categorical data were described as frequencies and percentages. For categorical variables, the Chi-square test was used to assess the significance of differences between the groups. For continuous variables, mixed effects models were used in the analysis and all analyses incorporated age as covariates for adjustment. Additionally, in the analysis of exo-deviation drift, the deviation at baseline was also included as a covariate to mitigate any potential impact of these factors on the statistical outcomes.
A suboptimal surgical outcome is defined as a postoperative deviation > 5 PD for esotropia, ≥ 10 PD for exotropia at any distance, or a stereoacuity decline > 0.6 log arcsec [1, 18]. A two-sided P value of less than 0.05 was considered statistically significant.
Results
Participants and Follow-Up
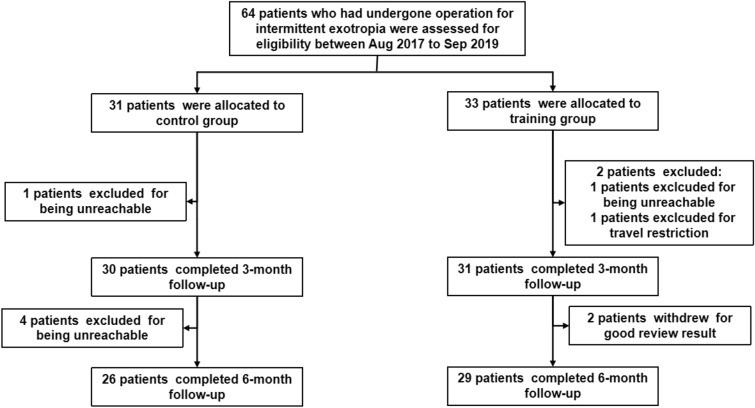
In total, 64 participants were recruited at the Zhongshan Ophthalmic Center between August 2017 and September 2019. These individuals were divided based on their participation in dichoptic training, with 33 assigned to the training group and the remaining 31 forming the control group, which would not receive any orthoptic treatment throughout the study. By the 3-month follow-up, there was a dropout of six participants (9.4%), and by the 6-month follow-up, an additional three participants (4.7%) had left the study. The flowchart provides detailed reasons for these participant losses (Fig. 1). In the end, the analysis incorporated results from 55 participants, comprising 29 in the training group (average age 9.69 ± 2.66 years) and 26 in the control group (average age 8.41 ± 2.64 years). There were no significant differences between the baseline data for participants who completed and did not complete the study (all P > 0.05; Table S2). No significant differences were found between the two groups in terms of gender, age, and other measured indicators at baseline (Table 2) and the outcomes were exhibited in Table 3.
Fig. 1.
Flowchart showing study completion for each group
Table 2.
Demographic and baseline clinical characteristics of two groups
| Characteristic | Control group | Training group | P value |
|---|---|---|---|
| Gender (M: F) | 16:10 | 13:16 | 0.215 |
| Age (years) | 9.69 ± 2.66 | 8.41 ± 2.64 | 0.080 |
| SER (D) | |||
| OD | − 0.03 ± 2.34 | 0.23 ± 1.72 | 0.457 |
| OS | 0.19 ± 2.19 | 0.26 ± 1.82 | 0.624 |
| BCVA (logMAR) | |||
| OD | 0.01 ± 0.03 | 0.01 ± 0.02 | 0.642 |
| OS | 0.01 ± 0.03 | 0.01 ± 0.03 | 0.468 |
| Simultaneous perception (present: absent) | |||
| Near | 21:5 | 21:8 | 0.467 |
| Distance | 18:8 | 21:8 | 0.795 |
| Fusion range (degree) | 11.38 ± 7.41 | 8.21 ± 7.32 | 0.241 |
| Stereopsis (log arcsec) | |||
| Near | 1.80 ± 0.32 | 1.79 ± 0.40 | 0.945 |
| Distance | 2.73 ± 0.29 | 2.78 ± 0.25 | 0.224 |
| Deviation (PD) | |||
| Near | − 2.50 ± 3.68 | − 0.90 ± 3.15 | 0.151 |
| Distance | − 2.12 ± 3.72 | − 1.03 ± 3.44 | 0.261 |
Means ± standard deviations for age, SER, fusion range, deviation, stereoacuity
OD oculus dexter (right eye), OS oculus sinister (left eye), SER spherical equivalent of refraction, F Female, M Male, D diopter, PD prism diopter
P represented the level of statistical significance for the comparison between the two groups at baseline
Table 3.
Outcome by 6 months in the training group and control group
| Characteristic | 3 months | 6 months | P1 value | P2 value | ||
|---|---|---|---|---|---|---|
| Control group | Training group | Control group | Training group | |||
| Simultaneous perception (present: absent) | ||||||
| Near | 22:4 | 21:8 | 22:4 | 22:7 | 0.418 | 0.418 |
| Distance | 18:8 | 20:9 | 21:5 | 19:10 | 0.983 | 0.205 |
| Fusion range (degree) | 11.85 ± 7.55 | 14.07 ± 8.00 | 11.42 ± 7.31 | 12.66 ± 9.10 | 0.150 | 0.337 |
| Stereopsis (log arcsec) | ||||||
| Near | 1.68 ± 0.35 | 1.49 ± 0.36 | 1.69 ± 0.37 | 1.44 ± 0.32 | 0.052 | 0.013* |
| Distance | 2.61 ± 0.35 | 2.34 ± 0.38 | 2.66 ± 0.27 | 2.40 ± 0.39 | 0.011* | 0.012* |
| Exo-deviation drift (PD) | ||||||
| Near | − 2.42 ± 3.71 | − 0.72 ± 2.97 | − 3.50 ± 4.48 | − 1.93 ± 4.85 | 0.109 | 0.058 |
| Distance | − 2.88 ± 3.66 | − 0.38 ± 3.70 | − 3.62 ± 3.57 | − 1.52 ± 4.42 | 0.010* | 0.028* |
| Suboptimal surgical outcomes | 12 (46.15%) | 3 (10.34%) | 13 (50.00%) | 5 (17.24%) | 0.003* | 0.010* |
Means ± standard deviations for fusion range, exo-deviation drift, stereoacuity
PD prism diopter
P1 represented the level of statistical significance for the comparison between the two groups at 3 months, P2 represented the level of statistical significance for the comparison between the two groups at 6 months
*Significance at 0.05
Simultaneous Vision and Fusion Range
At baseline, as well as at the 3-month and 6-month follow-up periods, there were no significant differences in simultaneous vision function at near and distance between the two groups (all P > 0.05, Table 3). Similarly, no significant differences were observed in the range of fusion function among the participants of both groups at baseline (11.38 ± 7.41 degree vs. 8.21 ± 7.32 degree, P > 0.05, 95% CI − 6.48 to 1.63), and at the 3-month (11.85 ± 7.55 degree vs. 14.07 ± 8.00 degree, P > 0.05, 95% CI − 1.08 to 7.03) and 6-month follow-up periods (11.42 ± 7.31 degree vs. 12.66 ± 9.10 degree, P > 0.05, 95% CI − 2.07 to 6.04) (Table 3).
Stereopsis
At baseline, there were no significant differences in both near and distance stereopsis between the control group and the training group (near: 1.80 ± 0.32 log arcsec vs. 1.79 ± 0.40 log arcsec, P > 0.05, 95% CI − 0.20 to 0.18; distance: 2.73 ± 0.29 log arcsec vs. 2.78 ± 0.25 log arcsec, P > 0.05, 95% CI − 0.06 to 0.26). However, at 3 months, a significant difference was observed in distance stereopsis between the two groups (2.61 ± 0.35 log arcsec vs. 2.34 ± 0.38 log arcsec, P < 0.05, 95% CI − 0.37 to − 0.05), but not in near stereopsis (1.68 ± 0.35 log arcsec vs. 1.49 ± 0.36 log arcsec, P > 0.05, 95% CI − 0.38 to 0.00). At 6 months, significant differences were found in both distance stereopsis (2.66 ± 0.27 log arcsec vs. 2.40 ± 0.39 log arcsec, P < 0.05, 95% CI − 0.37 to − 0.04) and near stereopsis (1.69 ± 0.37 log arcsec vs. 1.44 ± 0.32 log arcsec, P < 0.05, 95% CI − 0.43 to − 0.05) between the two groups (Table 3). After the 6-month follow-up period, the cumulative proportion of participants in the control group who received improvements in stereopsis was significantly lower than in the training group (near: 53.4 vs. 89.7%, χ2 = 8.86, P < 0.05; distance: 26.9 vs. 75.9%, χ2 = 13.17, P < 0.05).
Exo-Deviation Drift
At 3 months, a significant difference was observed in the exo-deviation drift at distance between the control group and training group (− 2.88 ± 3.66 PD vs. − 0.38 ± 3.70 PD, P < 0.05, 95% CI 0.65 to 4.69). However, there was no significant difference in the exo-deviation drift at near (− 2.42 ± 3.71 PD vs. − 0.72 ± 2.97 PD, P > 0.05, 95% CI − 0.04 to 4.32). At 6 months, the significant difference in exo-deviation drift at distance remained (− 3.62 ± 3.57 PD vs. − 1.52 ± 4.42 PD, P < 0.05, 95% CI 0.24 to 4.28), while the difference at near was not significant (− 3.50 ± 4.48 PD vs. − 1.93 ± 4.85 PD, P > 0.05, 95% CI − 0.17 to 4.19) (Table 3).
Suboptimal Surgical Outcomes
During the 3-month follow-up, suboptimal surgical outcomes were observed in 10.3% (3/29) participants from the training group and 46.2% (12/26) from the control group, showing a significant difference (χ2 = 4.05, P < 0.05). During the 6-month follow-up, 17.2% (5/29) of the training group and 50.0% (13/26) of the control group experienced suboptimal surgical outcomes and the significant difference remained (χ2 = 3.68, P < 0.05) (Table 3). The details are shown in Table S1.
Compliance of the Dichoptic Training Group
Participants in the training group needed to complete a total of 180 training sessions in 90 days. According to the training records in online-based training software, 96.6% (28/ 29) subjects in the training group completed all trainings.
Discussion
Our study suggests that the online video game-based dichoptic training significantly improved distance stereopsis in patients post-IXT surgery and effectively lowered the chance of suboptimal surgical outcomes. Although a tendency towards postoperative exo-deviation drift was observed in both groups, the extent of this drift was less pronounced in the TG.
IXT could compromise binocular visual functions of the patients, most commonly affecting their distance stereopsis. Previous studies had clarified that simply correcting the position of the eyes did not completely address impairments in binocular visual functions [4–6]. In the study conducted by Feng et al. [19], it was noted that approximately 77% of patients suffering from IXT experienced an enhancement in stereopsis six weeks following their surgical correction. Similarly, Yildirim et al. reported a lower percentage, with 58% of patients observing an improvement in distance stereopsis after corrective surgery [20]. Our study revealed that at the 6-month follow-up period, only 53.4% of participants in the control group experienced improvement in near stereopsis, and a mere 26.9% gained enhancement in distance stereopsis, significantly lower than those in the TG. Therefore, the rehabilitation of binocular visual functions after operation was crucial. In our research, both the CG and TG started with similar baseline levels of stereopsis. Follow-up assessments at 3 and 6 months revealed that the TG's distance stereopsis was superior to that of the CG. However, their near stereopsis only showed better than CG at the 6-month follow-up, aligning with the results reported in Xu et al.’s study [21]. Nonetheless, there were no significant differences in simultaneous perception and fusion range between the two groups, which indicated that there seemed to be a short-term bottleneck and further observation is needed.
Patients with IXT may experience a progressive enlargement of exotropia months or even years following their surgical correction, a condition referred to as postoperative exo-deviation drift [22]. Clinically, a more substantial exo-deviation drift tends to raise the likelihood of the condition recurring [3, 23–26]. In analyzing the exo-deviation drift between both groups, we prudently adjusted for age and baseline strabismus deviation as covariates to mitigate their possible effects on the statistical results. During the 3- and 6-month follow-ups, the extent of distance exo-deviation drift in the TG was significantly smaller compared to the CG. However, there were no significant differences in the near distance exo-deviation drift observed between the groups. This outcome suggested that the improved distance stereopsis observed in the training group might help in restraining the progression of exo-deviation drift [20].
Previous studies had shown the success rate of IXT surgical correction to be around 50–70%, possibly due to differing definitions of success [1, 18, 27–30]. In our study, we define Suboptimal Surgical Outcomes as a postoperative deviation of esotropia greater than 5 PD, or exotropia equal to or greater than 10 PD at distance or near, or a decline in stereoacuity greater than 0.6 log arcsec, which is different from the study of the Pediatric Eye Disease and Investigator Group [1]. It is noteworthy that we utilized the PACT rather than the Simultaneous Prism and Cover Test (SPCT) for assessing strabismus. PACT encompasses both latent and manifest deviations, whereas SPCT primarily focuses on manifest deviations. Consequently, our criteria are comparatively stringent. At the 3- and 6-month follow-up evaluations, the likelihood of suboptimal surgical outcomes was notably higher in the CG compared to the TG. This difference was likely attributable to the rehabilitation of stereopsis and the containment of exo-deviation drift progression observed in the TG. Thus, accepting the binocular dichoptic training after corrective operation could potentially enhance the success rate of the corrective procedure.
Traditional intervenes to rehabilitating binocular visual functions frequently employ devices such as the synoptophore, vectorgrams, and stereoscope [31]. However, the repetitive and monotonous nature of these training processes typically result in low patient compliance, often necessitating physician oversight [21, 32]. In contrast, our study found that 96.6% of patients in the TG successfully completed 180 sessions of home-based training. This suggests that incorporating video games into dichoptic training could make the rehabilitation process more interactive and enjoyable, resulting in higher patient adherence.
There are also some limitations in our study. Firstly, it was non-randomized that might raise the potential for selection bias, despite we tried to eliminate these effects through statistical methods. Secondly, the follow-up duration was brief, extending only over six months, affected by the COVID-19 pandemic [33]. Xu et al. carried out their study with a follow-up period lasting 12 months [21]. Lastly, the loss of participants during follow-up might have potential influence on the results. Consequently, it is essential to undertake multicentric, randomized-controlled studies with longer follow-up durations in future investigations.
Conclusions
In summary, our research indicated that online video game-based dichoptic training may offer a non-invasive and supplementary method for enhancing outcomes in the patients with IXT after surgery. Nonetheless, further studies would be required to validate and expand upon these initial findings. This study marked a significant advancement in recognizing the possible advantages of this novel approach to vision therapy.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Special thanks are due to Dr. Li and Dr. Yan for their invaluable support throughout this study. Dr. Li's guidance in research design and data analysis, along with Dr. Yan's encouragement and provision of resources, were crucial to the success of this work.
Author Contributions
Jinrong Li and Jianhua Yan contributed to the project design, data analysis, and the revision of the manuscript. Xuan Qiu and Yusong Zhou contributed to the project design, data analysis, and drafted the manuscript. Xinping Yu, Heping Wu, Tao Shen, Daming Den, Jingchang Chen, Xiaoming Lin, Heping Wu, Ying Kang, Qingqing Ye, and Qiwen Chen contributed to data collection and manuscript discussion. All authors contributed to the article, read, and approved the submitted version.
Funding
Dr. Li is supported by National Natural Science Foundation of China (82371088) and National Key Research & Development Project (2020YFC2003905), and is responsible for paying the journal’s Rapid Service Fee.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
All named authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No other disclosures were reported.
Ethical Approval
This study adhered to the tenets of the Declaration of Helsinki, and the study protocol was reviewed and approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (Approved ID: 2017-38). Participants gave informed consent to participate in the study before taking part. This study was not registered, primarily because it began before such registration was commonly required.
Footnotes
Xuan Qiu and Yusong Zhou contributed equally to this work and share first authorship.
Jianhua Yan and Jinrong Li contributed equally as co-corresponding authors.
Contributor Information
Jianhua Yan, Email: yanjh2011@126.com.
Jinrong Li, Email: lijingr3@mail.sysu.edu.cn.
References
- 1.Donahue SP, Chandler DL, Holmes JM, Arthur BW, Paysse EA, Wallace DK, et al. A randomized trial comparing bilateral lateral rectus recession versus unilateral recess and resect for basic-type intermittent exotropia. Ophthalmology. 2019;126(2):305–317. doi: 10.1016/j.ophtha.2018.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burian HM. Exodeviations: their classification, diagnosis and treatment. Am J Ophthalmol. 1966;62(6):1161–1166. doi: 10.1016/0002-9394(66)92570-0. [DOI] [PubMed] [Google Scholar]
- 3.Pang Y, Gnanaraj L, Gayleard J, Han G, Hatt SR. Interventions for intermittent exotropia. Cochrane Database Syst Rev. 2021;9(9):CD003737. doi: 10.1002/14651858.CD003737.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahn YJ, Park YY, Chung YW, Park SH, Shin SY. Surgical and sensory outcomes in patients with intermittent exotropia according to preoperative refractive error. Eye (Lond) 2019;33(8):1314–1320. doi: 10.1038/s41433-019-0419-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Y, Xu M, Zhang J, Zhou J, Wan M, Dai Z, et al. Can clinical measures of postoperative binocular function predict the long-term stability of postoperative alignment in intermittent exotropia? J Ophthalmol. 2020;2020:7392165. doi: 10.1155/2020/7392165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tan F, Yang X, Chu H, Yan L, Wiederhold BK, Wiederhold M, et al. The study of perceptual eye position examination and visual perceptual training in postoperative intermittent exotropes. Cyberpsychol Behav Soc Netw. 2020;23(12):871–875. doi: 10.1089/cyber.2020.0837. [DOI] [PubMed] [Google Scholar]
- 7.Yang X, Fan Y, Chu H, Yan L, Wiederhold BK, Wiederhold M, et al. Preliminary study of short-term visual perceptual training based on virtual reality and augmented reality in postoperative strabismic patients. Cyberpsychol Behav Soc Netw. 2022;25(7):465–470. doi: 10.1089/cyber.2022.0113. [DOI] [PubMed] [Google Scholar]
- 8.Caoli A, Sabatini SP, Gibaldi A, Maiello G, Kosovicheva A, Bex P. A dichoptic feedback-based oculomotor training method to manipulate interocular alignment. Sci Rep. 2020;10(1):15634. doi: 10.1038/s41598-020-72561-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, Thompson B, Deng D, Chan LYL, Yu M, Hess RF. Dichoptic training enables the adult amblyopic brain to learn. Curr Biol. 2013;23(8):R308–R309. doi: 10.1016/j.cub.2013.01.059. [DOI] [PubMed] [Google Scholar]
- 10.Li X, Yang C, Zhang G, Zhang Y, Lan J, Chu H, et al. Intermittent exotropia treatment with dichoptic visual training using a unique virtual reality platform. Cyberpsychol Behav Soc Netw. 2019;22(1):22–30. doi: 10.1089/cyber.2018.0259. [DOI] [PubMed] [Google Scholar]
- 11.Liu X-Y, Zhang Y-W, Gao F, Chen F, Zhang J-Y. Dichoptic perceptual training in children with amblyopia with or without patching history. Invest Ophthalmol Vis Sci. 2021;62(6):4. doi: 10.1167/iovs.62.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li J, Spiegel DP, Hess RF, Chen Z, Chan LYL, Deng D, et al. Dichoptic training improves contrast sensitivity in adults with amblyopia. Vision Res. 2015;114:161–172. doi: 10.1016/j.visres.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 13.Hess RF, Mansouri B, Thompson B. A binocular approach to treating amblyopia: antisuppression therapy. Optom Vis Sci. 2010;87(9):697–704. doi: 10.1097/OPX.0b013e3181ea18e9. [DOI] [PubMed] [Google Scholar]
- 14.Zheng C-Y, Xu W, Wu S-Q, Han D-X. A randomized study of network-based perception learning in the treatment of amblyopia children. Int J Ophthalmol. 2022;15(5):800–806. doi: 10.18240/ijo.2022.05.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatt SR, Mohney BG, Leske DA, Holmes JM. Variability of stereoacuity in intermittent exotropia. Am J Ophthalmol. 2008;145(3):556–561. doi: 10.1016/j.ajo.2007.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xi J, Jia W-L, Feng L-X, Lu Z-L, Huang C-B. Perceptual learning improves stereoacuity in amblyopia. Invest Ophthalmol Vis Sci. 2014;55(4):2384–2391. doi: 10.1167/iovs.13-12627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Žiak P, Holm A, Halička J, Mojžiš P, Piñero DP. Amblyopia treatment of adults with dichoptic training using the virtual reality oculus rift head mounted display: preliminary results. BMC Ophthalmol. 2017;17(1):105. doi: 10.1186/s12886-017-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kushner BJ. Selective surgery for intermittent exotropia based on distance/near differences. Arch Ophthalmol. 1998;116(3):324–328. doi: 10.1001/archopht.116.3.324. [DOI] [PubMed] [Google Scholar]
- 19.Feng X, Zhang X, Jia Y. Improvement in fusion and stereopsis following surgery for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2015;52(1):52–57. doi: 10.3928/01913913-20141230-08. [DOI] [PubMed] [Google Scholar]
- 20.Yildirim C, Mutlu FM, Chen Y, Altinsoy HI. Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol. 1999;128(2):222–230. doi: 10.1016/S0002-9394(99)00079-3. [DOI] [PubMed] [Google Scholar]
- 21.Xu M, Peng Y, Zheng F, Yu H, Zhou J, Zheng J, et al. The effects of orthoptic therapy on the surgical outcome in children with intermittent exotropia: randomised controlled clinical trial. J Clin Med. 2023;12(4):1283. doi: 10.3390/jcm12041283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J AAPOS. 2009;13(1):4–7. doi: 10.1016/j.jaapos.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee H-J, Kim S-J. Long-term outcomes following resection-recession versus plication-recession in children with intermittent exotropia. Br J Ophthalmol. 2020;104(3):350–356. doi: 10.1136/bjophthalmol-2018-313711. [DOI] [PubMed] [Google Scholar]
- 24.Mohan K, Sharma SK. Long-term motor and sensory outcomes after unilateral lateral rectus recession-medial rectus resection for basic intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2020;57(5):326–332. doi: 10.3928/01913913-20200731-01. [DOI] [PubMed] [Google Scholar]
- 25.Park H, Kim WJ, Kim MM. The stabilization of postoperative exo-drift in intermittent exotropia after surgical treatment. Korean J Ophthalmol. 2016;30(1):60–65. doi: 10.3341/kjo.2016.30.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morisawa S, Hamasaki I, Shibata K, Shimizu T, Kono R, Miyata M, et al. Risk factors for excessive postoperative exo-drift after unilateral lateral rectus muscle recession and medial rectus muscle resection for intermittent exotropia. BMC Ophthalmol. 2020;20(1):216. doi: 10.1186/s12886-020-01484-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang X, Man T-T, Tian Q-X, Zhao G-Q, Kong Q-L, Meng Y, et al. Long-term postoperative outcomes of bilateral lateral rectus recession vs. unilateral recession-resection for intermittent exotropia. Int J Ophthalmol. 2014;7(6):1043–1047. doi: 10.3980/j.issn.2222-3959.2014.06.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L, Wu Q, Kong X, Li Z. Comparison of bilateral lateral rectus recession and unilateral recession resection for basic type intermittent exotropia in children. Br J Ophthalmol. 2013;97(7):870–873. doi: 10.1136/bjophthalmol-2013-303167. [DOI] [PubMed] [Google Scholar]
- 29.Procianoy E, Procianoy L. Bilateral lateral rectus recession vs. unilateral recess-resect procedure for exotropia with a dominant eye. Am J Ophthalmol. 2006;142(4):708. doi: 10.1016/j.ajo.2006.06.043. [DOI] [PubMed] [Google Scholar]
- 30.Wu H, Sun J, Xia X, Xu L, Xu X. Binocular status after surgery for constant and intermittent exotropia. Am J Ophthalmol. 2006;142(5):822–826. doi: 10.1016/j.ajo.2006.06.045. [DOI] [PubMed] [Google Scholar]
- 31.Ma MM-L, Kang Y, Chen C, Su C, Tian Z, Le M. Vision therapy for intermittent exotropia: a case series. J Optom. 2021;14(3):247–253. doi: 10.1016/j.optom.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jang JU, Jang JY, Tai-Hyung K, Moon HW. Effectiveness of vision therapy in school children with symptomatic convergence insufficiency. J Ophthalmic Vis Res. 2017;12(2):187–192. doi: 10.4103/jovr.jovr_249_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu J, Ye Q, Xiao C, Zhuang Y, Feng L, He Y, et al. Impact of COVID-19 pandemic control measures on amblyopia treatment: a retrospective study of records from a tertiary eye hospital in China. BMJ Open. 2023;13(7):e071839. doi: 10.1136/bmjopen-2023-071839. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.