Abstract
Background:
HITEC 2 (Health Improvement through Employee Control 2) is the follow-up to HITEC, a participatory action research (PAR) program that integrates health and work conditions interventions designed by the workforce. HITEC 2 compares intervention programs between two correctional sites, one using a pure workforce level design team and the other using a more structured and time delineated labor-management kaizen effectiveness team.
Methods:
HITEC 2 utilizes a seven step participatory Intervention Design and Analysis Scorecard (IDEAS) for planning interventions. Consistent with PAR, process and intervention efficacy measures are developed and administered through workforce representation.
Results:
Participation levels, robustness of participatory structures and sophistication of interventions have increased at each measured interval. Health comparisons between 2008 and 2013 showed increased hypertension, static weight maintenance, and increased ‘readiness to change’.
Conclusions:
The PAR approaches are robust and sustained. Their long-term effectiveness in this population is not yet clear.
Keywords: participatory action research, IDEAS, worksite health promotion
1. Introduction
There are more than half a million COs1 in the United States. Although there is a general paucity of occupational safety and health literature on this population, the prevailing evidence is that corrections is associated with high rates of psychological distress and musculoskeletal and cardiovascular disease risk (Tiesman et al., 2010). Associated contextual risk factors include physical danger, low autonomy, and work-family conflict (Bourbonnais et al., 2007; Schaufeli and Peeters, 2000). HITEC2 1 (2006–2011) and HITEC2 2 (2012-present) is an intervention research program initiated with the Connecticut Department of Correction. It features an integration of preventive occupational health, directed to the physical and organizational work environment, with workplace health promotion (WHP) (Punnett et al., 2009).
Because the methods employed in HITEC2 2 are an evolution within an ongoing study, its design can be appreciated through an overview. The HITEC2 1 approach entailed comparison of an administratively conceived ergonomics and WHP/best practices or professional program at one corrections facility with an intervention program entirely directed by a CO1 dominated DT3 at a second corrections facility. The DT3 was internally generated from the workforce, and adhered to principles of participatory action research (PAR) (Henning et al., 2009; Punnett et al., 2013). In HITEC2 1, health outcomes were measured by survey, focus groups and interviews, by physiologic function and performance testing, and by a standardized Health Risk Appraisal (HRA). The WHP/best practices prison facility (Site A) and the DT3 represented prison facility (Site B) were selected from 19 candidate prisons on the basis of comparable size, security level, staffing, physical plant, and from a preliminary survey of supervisors. The supervisor survey aided site selection by identifying inter-site congruence, particularly around measures of openness to interventions and ‘readiness to change’.
In HITEC2 1, the WHP/best practices prison facility (Site A) had limited success: attendance was modest at individual health coaching, weight loss, and chronic disease prevention classes, and participation in a labor-management advisory committee was sparse. At Site B, the DT3 met regularly 1–2 times per month on protected work time, and conducted its own surveys and recruitments. Innovative DT3 programs included improved inter-officer conduct (civility program), footwear revision, and DT3-directed weight loss configured to work schedules. A clear differential in health outcomes between the two sites for participants engaged continuously from 2008–2013 was not readily obvious.
There were other important findings from HITEC2 1 that informed HITEC2 2. Serious emotional health problems among COs1 were widespread with ominous indicators appearing in the first years of employment (Obidoa et al., 2011). Approximately one third (31%) had scores of 10 or more on the Center for Epidemiologic Studies Depression Scale (CES-D) an indication of the presence of significant depressive symptoms (Radloff, 1977), and work family conflict was identified in the majority of respondents. A high prevalence of obesity also appeared to emerge early in work tenure (Figure 1). Figure 1 also suggests that the obese pattern is persistent, changing little over the 20–25 year career of a CO1. Perhaps more striking are the findings on hypertension which are presented in Figure 2. In the US male population, hypertension is an age related disorder with prevalence accumulating progressively between the 3rd and 4th decades. Contrarily, in COs1, hypertension follows the pattern of early presentation in work life, being elevated between the ages of 20–34, compared with national rates, and remaining high in subsequent working years.
Figure 1.
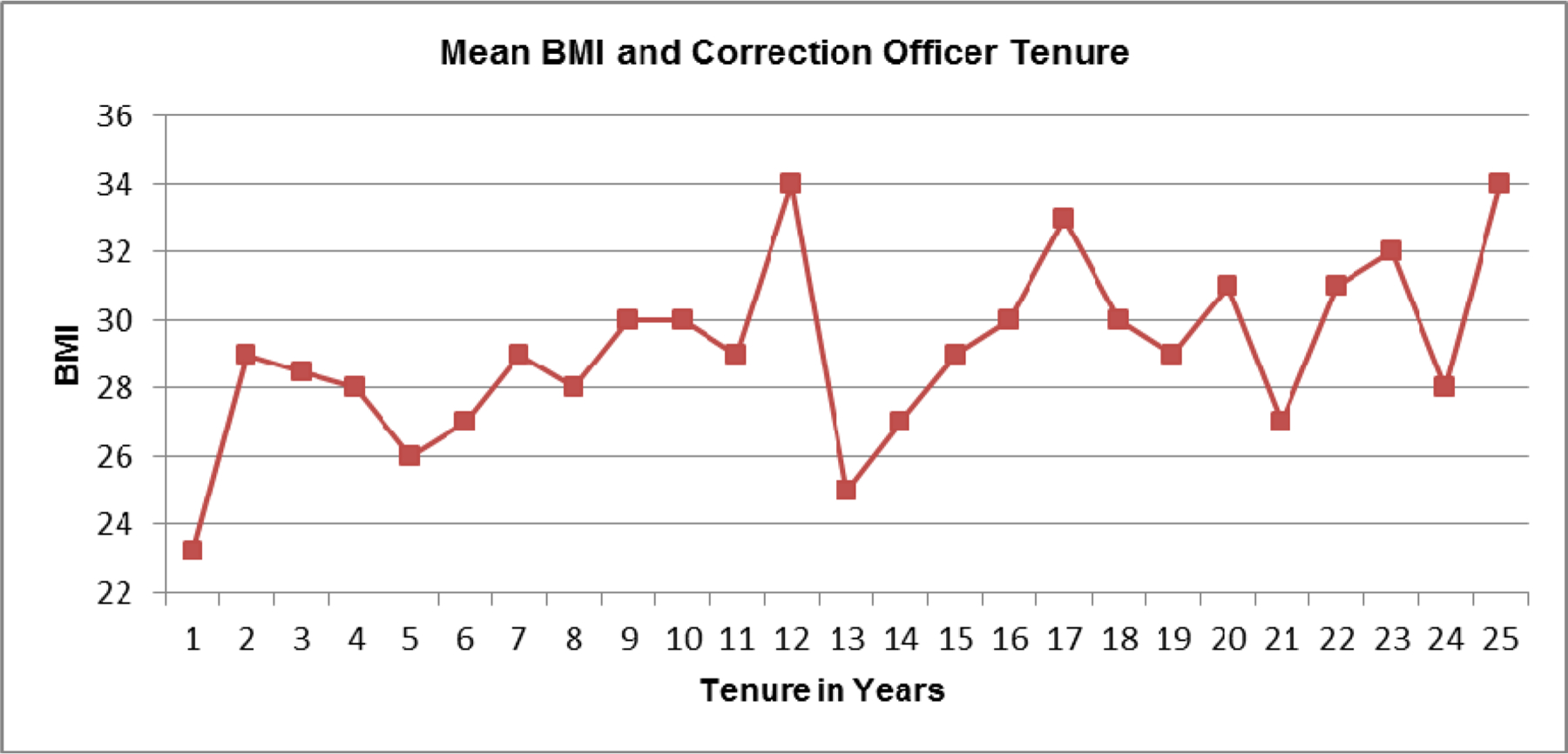
BMI status and years of employment in correction officers
Figure 2.
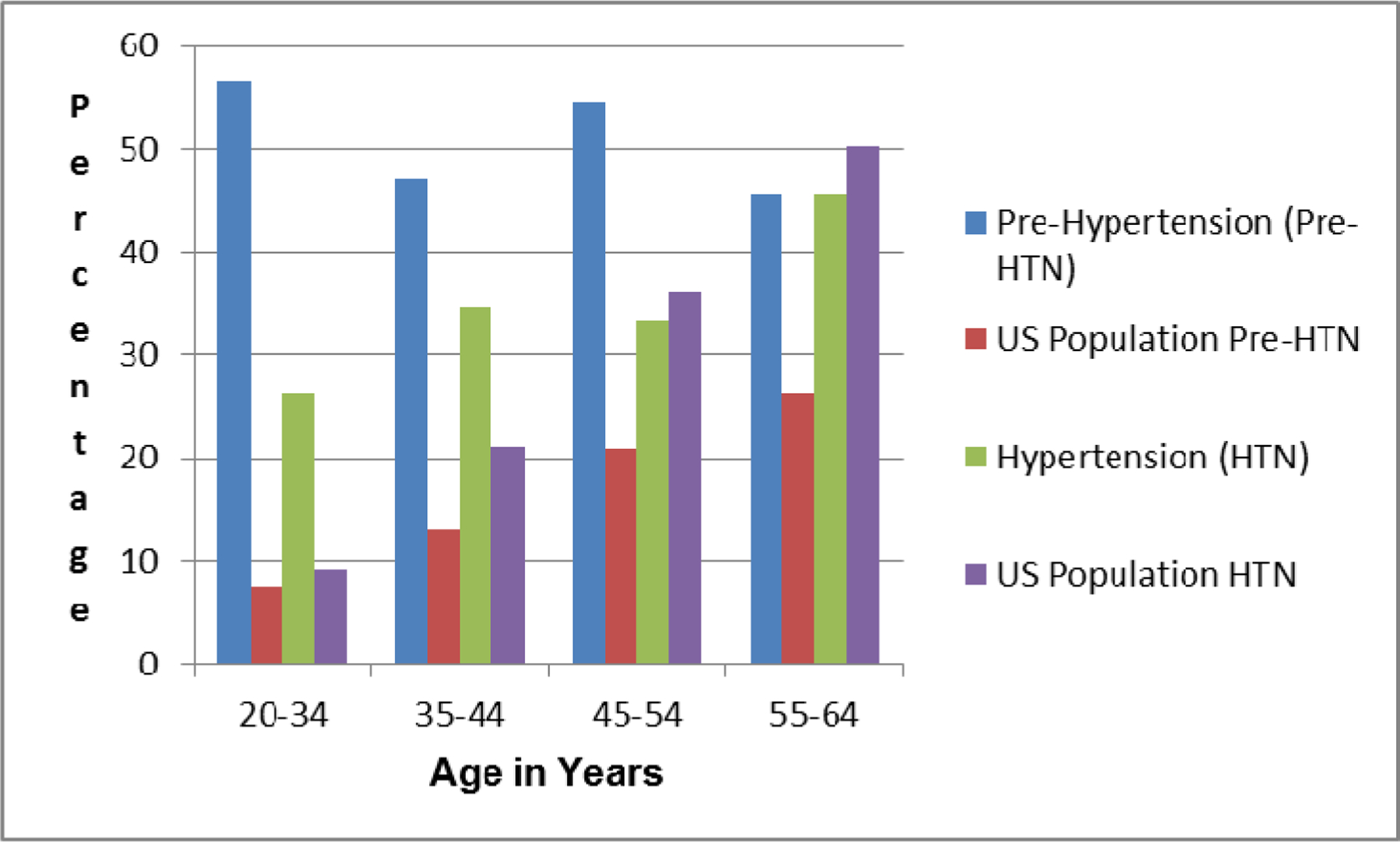
Hypertension in male correction officers: age specific comparison with US norms
The participatory interventions at Site B proved feasible and were superior to the WHP/best practices approach at Site A in terms of efficacy and workforce engagement and participation levels. HITEC2 2 incorporated these outcomes by replacing the more top-down professional interventions at Site A with a task driven successor based on joint labor-management KET4. The KET4 construction was borrowed from industrial experience (Glover et al., 2011; Farris et al., 2009). To better understand the KET4 composition, its internal process and its differentiation from the pure workforce directed DT3 at Site B, it is useful to review the HITEC2 governance and action process. In PAR, study structure and outcomes are developed within the study process, and the study population is a party to design and execution (Reason and Bradbury, 2001; Small, 1995). Recognized strengths of PAR include incorporation of worker knowledge of hazards and feasibility of interventions, and a high potential for workforce participation, effectiveness and sustainability (Small, 1995). Major obstacles include maintaining consistency of scientific design and endpoints. HITEC’s2 operational governance has followed PAR principles, involving the DT3 at Site B, Facility Specific Steering Committee at both sites, and a Study Wide Steering Committee consisting of Department of Correction administrators, site managers (wardens and deputies) and labor union representatives. The Facility Specific Steering Committee provides oversight and feasibility assessment at the facility level. The Study Wide Steering Committee has decision making authority over most study programmatics, but with critical exceptions. These exclusions, which remain within the authority of the research team, involve human subjects and data protection, the conduct of testing and evaluation, and adherence to specific ‘study metrics’ which are essential to scientific design and evaluation of effectiveness. The role of the Study Wide Steering Committee was critical in the evolution of HITEC2 1 into HITEC2 2. The Study Wide Steering Committee requested that the research team replace the top-down WHP/best practices approach at Site A with a more participatory format. The result was the restructuring of intervention planning at Site A. The top-down or administrative best practices approach was replaced with a multi-level participatory form, translated from manufacturing, called a kaizen effectiveness team. The organizational structure of HITEC2 2 is presented in the following Methods section and is introduced here for orientation as Figure 3.
Figure 3.
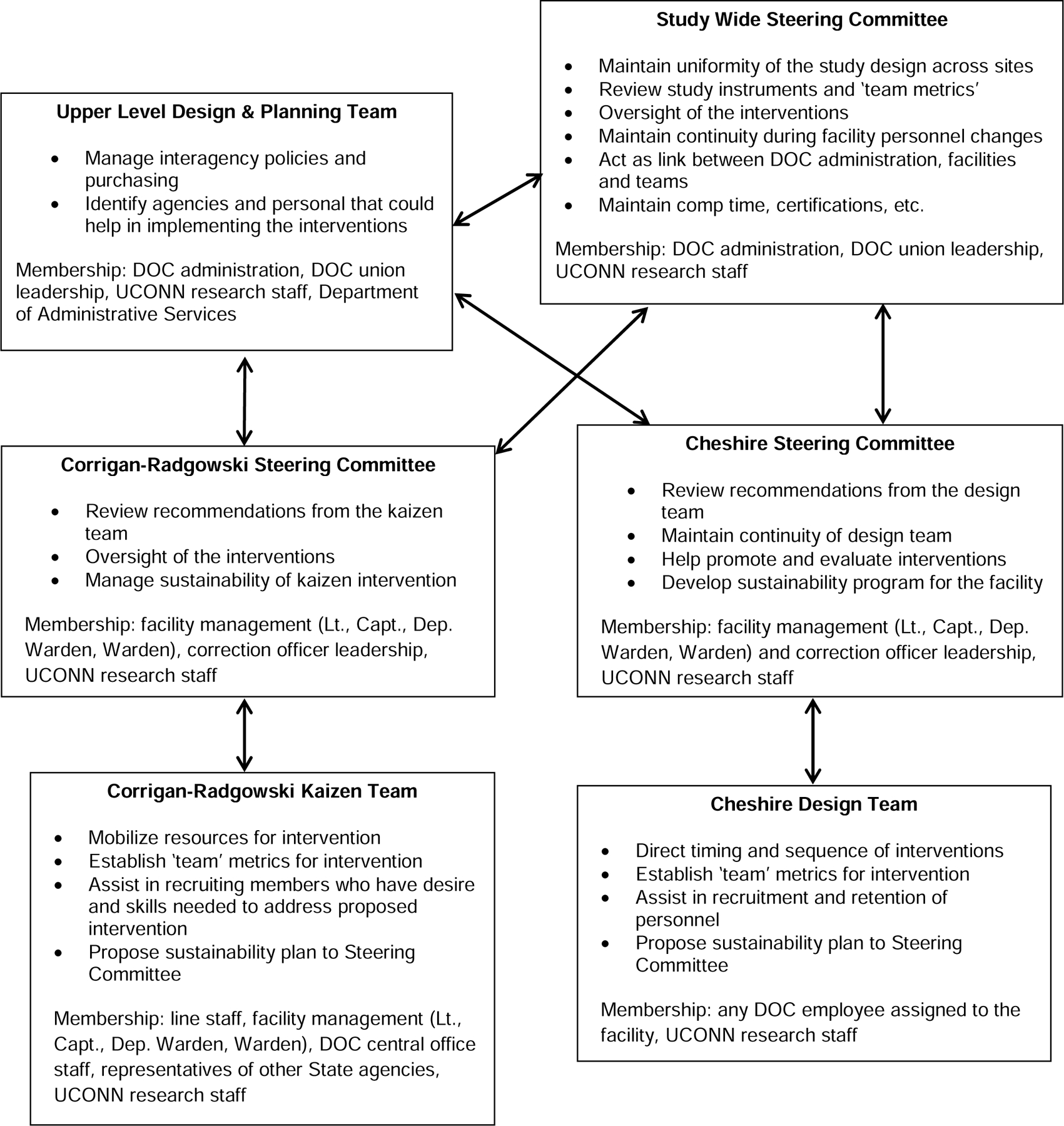
Organizational structure and responsibilities
The lack of applicability of several commonly used survey instruments covering job strain, stress, and work-family conflict was another important finding from HITEC2 1 (Obidoa et al., 2011). Mental health was evaluated both by the Mental Component Score of the Short Form 12 (SF-12) (Ware et al., 2002; Obidoa et al., 2010) and the Center for Epidemiological Studies Depression (CES-D) scale (Radloff, 1977). Focus groups substantiated high levels of depression and bi-directional influences of work family conflict (WFC). Focus groups and physical testing identified deficits in health, but physical and emotional scores on the SF-12 equaled or exceeded national averages and were correlated only weakly with elevated depression (r<0.20). Neither the Job Content Questionnaire subscales nor the HRA were associated with the depression scores. The limitations of the SF-12 for longitudinal tracking of employed populations has been noted (Obidoa et al., 2010), but the discordance between reduced physical performance and self-assessed capacity was unanticipated. Similar problems with the bluntness of conventional survey instruments when translated into corrections was noted by Schaufeli and Peeters (2000) in their review of CO1 health. The HITEC2 2 survey was modified, accordingly, by introducing more ‘concrete’ questions on health status.
2. Methods
2.1. Kaizen Effectiveness Team and Design Team
The involvement of study population representatives in selection of outcome measures introduces two potential problems. First, differences in the content of interventions can weaken inter-group comparisons of effectiveness. Second, participant-selected outcome measures may differ from parameters that are either more effectively measured or preferred by the study team. In HITEC2 2, the problem is approached through a mixed methods approach.
In order to remain consistent with the PAR approach while maintaining approximate comparability of the interventions, the KET4 and the DT3 were each assigned four basic task areas, determined by the Study Wide Steering Committee. These are described with their pertinent acronyms in Table 1. BILD5 is essentially an ergonomics and work environment program. W-2 BFIT6 was intended to introduce participatory problem solving to fitness for duty, an area that has reflexively provoked labor-management discord in hazardous duty work, where the assurance of long-term fitness and job security are potentially in conflict. BFED7 was first proposed by the DT3 in HITEC2 1 and is meant to address the problems of excessive calorie intake that in this population appears to be affected by stress, overtime and shiftwork, and the general requirement for sedentary vigilance (Ferraro et al., 2013). SWIPE8 was intended to encourage the exploration and solution to a pattern of greater injury severity and lost work time in inmate provoked codes or assaults.
Table 1.
HITEC 2 Interventions
| Name of Intervention | Description |
|---|---|
| Building Improvement Linked to Design | An ergonomic intervention focused on procurement policies and building design to support exercise and relaxation |
| Work to be Fit | A correction officer-developed intervention to improve fitness |
| Better Food through Education and Design | A weight management intervention aimed at improved nutrition and altering the environment to affect eating patterns at work |
| Structured Work-related Injury Prevention through Ergonomics | A safety intervention addressing correction officer injury related to inmate incidents |
By design, it falls to the Study Wide Steering Committee to determine the sequence of the interventions at Site A. Each KET4 was provided a 120 day time window to complete the project. The study team and Study Wide Steering Committee were responsible for inviting outside experts, conducting technical investigations, and bringing State budgetary officers and other key personnel to the KET4 sessions. Otherwise, internal representation was determined by the Facility Specific Steering Committee. The intention was to arrange all KET4 sessions during formal work hours. Because non-CO1 personnel generally work and meet during daytime hours, this practically meant first shift assignment.
The DT3 at Site B had a different and more fluid work plan. The order and duration of the four interventions were left to be determined by the DT3. Based on HITEC2 1 experience where the joint attendance of supervisors and line officers was thought to be inhibiting, the DT3 consisted of line officers only. Because senior officers prefer and select first shift assignments, but are also nearer to their retirement, the Study Wide Steering Committee chose to hold all DT3 sessions at the start of the 2nd shift in order to insure inclusion of younger officers and promote sustainability. Meetings were to be scheduled with release time, at least monthly. Coincident with the ethos for joint labor management cooperation, both the bargaining unit and Connecticut Department of Correction administration agreed that DT3 members would contribute 50% of their time in the format of pre or post- shift attendance with the remaining 50% of time being covered by Connecticut Department of Correction. By consensus, these arrangements were kept outside of the collective bargaining agreement. In the history of HTEC2, there has never been a formal tenure limit for the DT3. Retirements and transfers require natural replacement. Because rotating work shifts vitiate non-interrupted attendance by the same personnel, the DT3 maintains a membership of 12 COs1 with the understanding that at least 3–4 will be available for every meeting. A designated facilitator, an essential element for the DT3, was provided by the academic study team.
Figure 3 depicts reporting and decision making processes. The DT3 work is iterative, whereby proposals for activities are reviewed between the Facility Specific Steering Committee Committee, the Study Wide Steering Committee, and the KET4 or DT3. An Upper Level Design and Planning Team is also introduced in Figure 3. Upper level design process is recognition of contingency: some executive decision making, technical expertise within State government, and fiscal authority for non-budgeted activities exceed Connecticut Department of Correction purview or authority. Accordingly, a non-Department of Correction group of senior administrators convenes to vet and fund (or provide matching funds for) project proposals that are recommended and budgeted by the KET4 or DT3 and the Study Wide Steering Committee.
For point of clarification, this was not a randomized trial within a single population. The sites were geographically and programmatically distinct. Randomization within a single site was not feasible for two reasons: 1) the close quarters of COs makes blinding unfeasible and 2) exclusivity within a site is not compatible with PAR methods, which allow for variable levels of involvement.
2.2. Assessment Tools
There are 5 assessment tools designated for HITEC2 2: 1) the HITEC2 core survey; 2) scripts and tools for qualitative assessment; 3) short pre- and post- tracking instruments to evaluate participation and intervention effectiveness; 4) a physical assessment examination protocol; and 5) workplace exposure assessment protocols.
The physical assessment was unchanged from HITEC2 1. It consists of measurement of height, weight, waist circumference, blood pressure, hand grip strength, body fat content and exercise capacity assessed by bicycle ergometry. Tests were re-administered in 2013 and will be administered in 2016. The core survey is a multi-dimensional questionnaire whose key domains address mental health and depression, workplace conditions, work and family relationships, and general health and wellbeing. It has been described elsewhere (Obidoa et al., 2011; Faghri et al., 2010). It was amended in HITEC2 2 to include more ‘concrete’ items on symptoms, types and frequency of medical treatments, reactions to noise and the physical environment, and sleep and alcohol use patterns. In addition, there were new question batteries that included pre-intervention and outcomes measures the four interventions: BILD5, W-2 BFIT6, BFED7, and SWIPE8. These included greater detail on physical injury, on speech communications, and on diet. The survey was vetted by a designated sub-group of the Study Wide Steering Committee, with each Facility Specific Steering Committee acting as a focus group.
The use of short surveys and related instruments reflects an effort to enable participatory teams and committees to assess the process changes and intervention effects. Accordingly responses are measured over short intervals without requiring the longer duration and more multiply influenced outcomes that are essential to a longitudinal research study. Completion time of short surveys varies from 5–10 minutes compared to more than 30 minutes for the longer HITEC2 core survey. Short surveys and KET4 or DT3 generated interviews fall into a category termed ‘team metrics’. Their development provides working results and requires active administration and supervision by the KET4 or DT3. ‘Team metrics’ are usually customized for within-site assessment. They also addressed an intrinsic problem with PAR, since it poses barriers to more traditional controlled study design. Two such transgressions to conventional research design are privacy and the need to delineate a firm threshold between participatory activity and research design integrity (Israel et al., 2001; Koelen et al., 2001). The short-survey mechanism followed in HITEC2 2 involves the development of modular blinded surveys with the modules developed with the study team and the KET4 or DT3. Respondents identify themselves by an idiosyncratic code (phone digits + PIN). These ‘team metrics’ rest on the supposition that sampling and ascertainment for follow-up will be incomplete, that results are only semi-quantitative, and process indicators, such as willingness to participate and to follow-up are at least as important as traditional outcomes. Generally, ‘team metrics’ are intervention-specific in order to document the effectiveness of each project, apart from more general and longer-term study metrics, defined as study Aims.
For HITEC2 2, iteratively developed ‘team metrics’ have been developed for IAQ9 assessment, noise and barriers and communications, job stress, work organization and inter-staff civility, and tracking of weight loss and its institutional obstacles. Short surveys developed for HITEC2 1 and available to HITEC2 2 also include the IAS10, the NPAQ11, and the Food and Physical Activity Liking Survey. IAS10 is an <10 question health and workplace change instrument; NPAQ11 is a food knowledge questionnaire; and NPALS15 is a psychometric ‘food-liking’ instrument developed to assist in participatory weight loss programs (Duffy et al., 2009). These instruments are further detailed in manuscripts produced from HITEC2 1; their inclusion introduces the general format applicable to all short surveys (Faghri et al., 2012). “Team metric” surveys are refined and piloted by either the KET4 or DT3 with study team input. To date, all instruments have been developed in a pre- and post- intervention format. To further distinguish, the core survey and the physical testing contribute to what are termed ‘study metrics’. These are the standardized cohort assessment instruments, first used in HITEC2 1. ‘Study metrics’ also include study-driven qualitative assessments, such as periodic scripted focus groups and key interviews that will inform interpretation of quantitative results. In Table 2, ‘study metrics’ and ‘team metrics’ are presented for the four interventions. The priori ‘team metrics’, and by default, the associated ‘study metrics’, are necessarily incomplete due to the PAR nature of the project. Accordingly, the ‘team metrics’ are deliberately unspecified. The more exacting ‘study metrics’ are not answerable until full re-evaluation of the workforce in 2016.
Table 2.
Evaluation: Team and Study Metrics for HITEC 2
| Intervention | Team Metric | Kaizen Site | Design Team Site | Study Metric |
|---|---|---|---|---|
| BILDa | 10% ↓ HMSb,c | Revised | NA | >3 dB reduction |
| Ergonomic reassessments | In place | In place | NA | |
| BFEDd | FPALSe and NPAQf completion rate | NA | On-going | BIAg ∆ |
| Weight loss goals | NA | On-going | -- | |
| W-2 BFITh | To be Determined | -- | -- | ↓ 5% BIA ↓ 15% MSD ↑ 10 kcal ergometry |
| SWIPEi | Program adoption | -- | -- | ↓ 20% critical events |
BILD = Building Improvement Linked to Design
HMS = Hearing Measurement Scale
BFED = Better Food through Education and Design
FPALS = Food and Physical Activity Liking Survey
NPAQ = Nutrition and Physical Activity Questionnaire
BIA = Bio-impedance Analysis
W-2 BFIT = Work to be Fit
SWIPE = Structured Work-related Injury Prevention through Ergonomics
2.3. Intervention Design and Analysis Scorecard
The PAR approach poses essential challenges for inter-site comparison due to the inherent potential of divergent priorities and operational approaches that potentially divide Site A from Site B. The four thematic intervention areas were one solution to achieving comparability. A second was the provision of using the same structured intervention planning approach at both sites. The IDEAS12 Tool is part of a larger suite of Research-to-Practice tools developed by the Center for the Promotion of Health in the New England Workplace (CPH-NEW) to support healthy workplace participatory programs (Robertson et al., 2013). CPH-NEW is a NIOSH funded Total Worker Health (TWH) center of excellence and is the parent organization for HITEC2. A seven-step intervention planning process was developed through multi-site beta testing, including introduction in HITEC2. This stepwise scorecard approach to develop, evaluate, rank, and select the most effective and affordable intervention ideas and solutions is available to the public domain and can be referenced on the CPH-NEW website (http://www.uml.edu/Research/Centers/CPH-NEW/Healthy-Work-Participatory-Program/default.aspx). A simplified illustration documenting the process and interaction with upper level design is presented in Figure 3. The process which involves a DT3 (or KET4 in HITEC2 2) that interacts with an organizational steering committee carries interventions from an open problem identification phase through intervention implementation and evaluation is multi-component and generates intervention alternatives that can be systematically reviewed and selected by the Facility Specific Steering Committee. The IDEAS12 was used at both Site A and Site B. The Facility Specific Steering Committee, Study Wide Steering Committee, and Upper Level Design and Planning Team are not presented in Figure 4 but their incorporation is implicit in what are termed activities of the Steering Committee. Fidelity to the delineated steps of the Ideas Tool is further maintained KET4 reports to the Study Wide Steering Committee at the onset and conclusion of the intervention (coherence with the 3 priority areas). Having no specified timeline, the DT3 had a different reporting expectation. The Study Team met on a weekly basis to insure that the facilitator prevented divergence from the main project theme.
Figure 4.
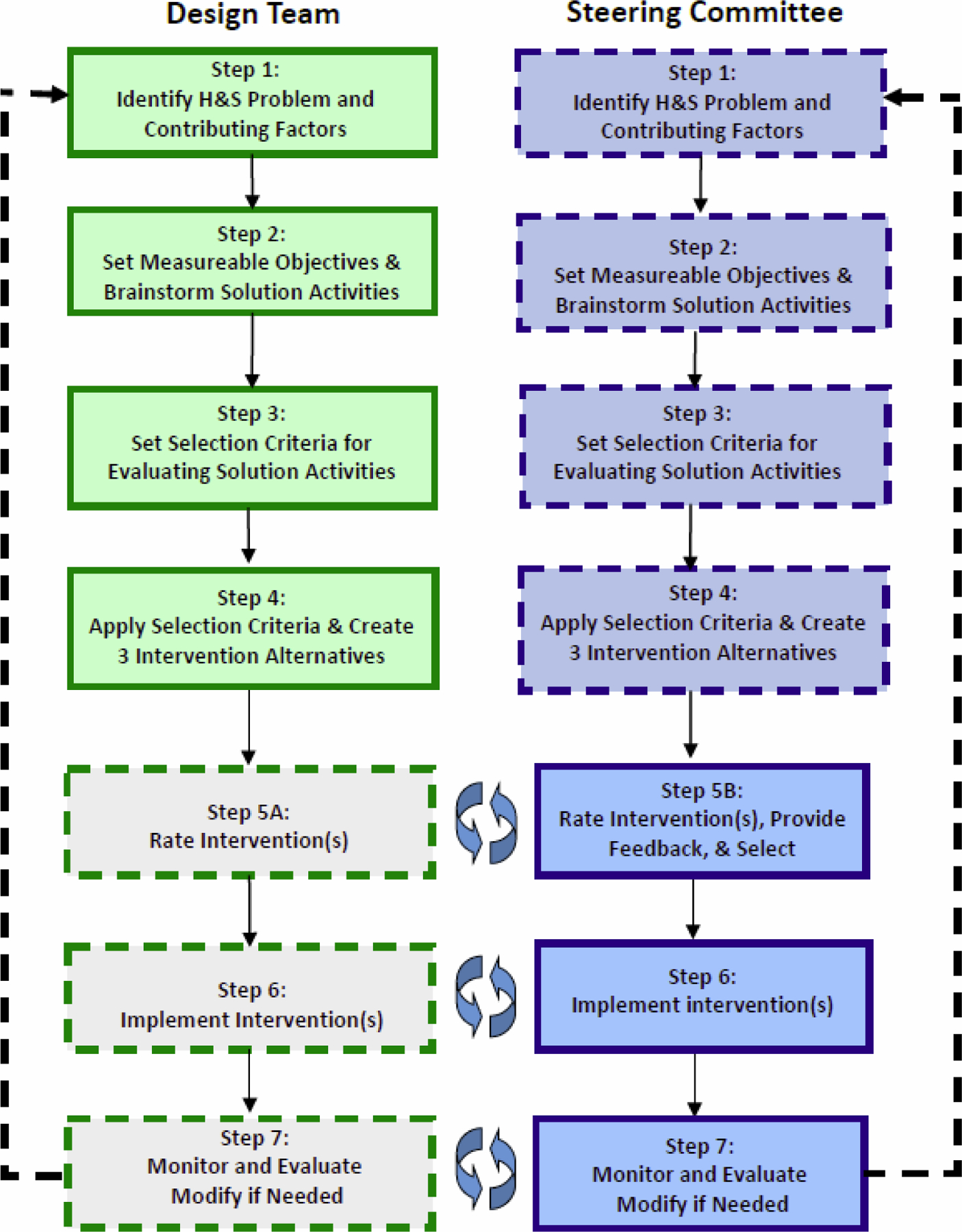
Intervention, Design and Analysis Scorecard
3. Results
Results to date fall into two categories: 1) the activity of both the KET4 or DT3 determined by their own and external evaluation criteria, and 2) health outcomes provided at baseline of HITEC2 2 (Year 7 of HITEC2). This is a practical division. While the baseline health data can be compared to HITEC2 1, either as a repeated cross-section or as a prospectively followed inception cohort, the follow-up ‘study metric’ data is not yet available. Accordingly, HITEC2 2 efficacy can be evaluated at this point only in terms of its participatory metrics. Nevertheless, critical baseline health data, and comparisons with early evaluations were provided to the Study Wide Steering Committee, the KET4 and the DT3. A summary of longitudinal health outcomes follow.
3.1. Health Outcomes
Although the general outline of program interventions was established by the study team and the Study Wide Steering Committee prior to HITEC2 2 interventions, the baseline health survey and testing had ramifications that were absorbed into participatory study approaches and metrics. In Table 3, blood pressure, BMI and BIA (body fat) are compared for 2008 and 2013 (HITEC2 2 baseline). The larger population in 2013 (n=326), compared with 2008 (n=198) reflects the open enrollment and replacement nature of the study, allowing new participants to join at each testing interval. Accordingly, these results are best understood as a comparison of two cross sections, although continuous data is available at all testing periods for participants who have continued from project inception. Although BMI and BIA were not significantly different at the two test periods, the prevalence of COs1 with hypertension increased from 27.3% to 54.6% for the combined participant population when 2013 is compared to 2008. In 2013, between site differences were small. Overall CVD risk calculations, based on BIA were elevated in 53.1% of COs1 at Site A and 50.8% at Site B. Table 3 also includes information on the members of the workforce who have participated continuously from Year 2 → Year 7 (2008–13).
Table 3.
Health Parameters 2008–2013
| 2008 | 2013 | 2008–2013 | |||
|---|---|---|---|---|---|
| Blood Pressure | Normal | % (N) | 23.2% (46) | 10.7% (35) | 21.4% (9) |
| Mean systolic/diastolic | 111.59/73.52 | 112.11/69.03 | 112.0/66.0 | ||
| SD | 7.416/6.069 | 5.092/5.399 | 7.55/3.464 | ||
| Prehypertension | % (N) | 52% (103) | 34.7% (113)* | 61.9% (26) | |
| Mean systolic/diastolic | 125.77/81.27 | 129.93/78.76 | 129.15/76.92 | ||
| SD | 6.82/4.705 | 5.373/6.87 | 6.581/6.576 | ||
| Hypertension | % (N) | 24.7% (49) | 54.6% (178)* | 16.7% (7) | |
| Mean systolic/diastolic | 133.84/92.92 | 151.21/88.01 | 149.13/88.71 | ||
| SD | 8.973/5.431 | 12.272/11.461 | 7.964/10.183 | ||
| BMI | Underweight | % (N) | 0 | 0.3% (1) | 0 |
| Mean BMI | |||||
| SD | |||||
| Normal Weight | % (N) | 9.6% (19) | 15.2% (49)* | 9.5% (4) | |
| Mean BMI | 23.12 | 23.22 | 24.55 | ||
| SD | 1.53 | 1.55 | 1.02 | ||
| Overweight | % (N) | 35.4% (70) | 36.2% (117) | 47.6(20) | |
| Mean BMI | 27.79 | 27.93 | 28.19 | ||
| SD | 1.38 | 1.38 | 2.54 | ||
| Obese | % (N) | 54.5% (108) | 48.3% (156) | 42.9% (18) | |
| Mean BMI | 34.99 | 32.55 | 33.53 | ||
| SD | 4.57 | 5.24 | 6.57 | ||
| Body Fat % | Well Below Average Risk | % (N) | 13.1% (26) | 10.9% (28) | 11.1% (3) |
| Below Average Risk | % (N) | 15.2% (30) | 10.5% (27) | 25.9% (7) | |
| Average Risk | % (N) | 23.2% (46) | 23.6% (61) | 18.5% (5) | |
| Above Average Risk | % (N) | 24.2% (48) | 28.7% (74) | 22.2% (6) | |
| Well Above Average Risk | % (N) | 16.7% (33) | 26.4% (68) | 22.2% (6) |
2013 Participants taking part in all testing procedures from 2008–2013. Comparison is with 2008 baseline.
p<0.05
Body Fat percentage category values vary by age and gender Means and Standard Deviation not reported because of wide variance in age and gender appropriate values.
Table 4 (Readiness to Change) combines participants at Site A and B. It reflects the continuing interest of the workforce in making health and work related-changes, and the cognitive awareness of obstacles. As Figure 5 demonstrates, the mental health of COs1 remains a significant barrier to change. The prevalence of major depression, determined by the CES-D, was elevated in 2013 (16.3%) compared to 12.1% in the concluding survey for HITEC2 1 in 2011. Figures 6a and 6b provide additional evidence of a stressed workforce. As depicted in figure 6a, 68.2% of the CO1 workforce report 6 or less hours of sleep per night or day during the work week. This reflects a 15% increase in this fewest hours of sleep category compared with 2011. Contrarily, 71.3% of COs1 indicated that they required 7 or more hours of sleep per night. In Figure 6b, drinking patterns are presented. The reliability and validity of alcohol reporting is sometimes problematically regarded, although the volume equivalents used here appear preferable (DelBaco and Darkes, 2003; Stockwell et al., 2004).
Table 4.
Readiness to Change on Key Health and Lifestyle Parameters 2013
| No present interest in change | Plan to change in 6 months | Plan to change this month | Recently started doing this | Already do this regularly | |
|---|---|---|---|---|---|
| Be physically active | 7.4% | 18.8% | 17.3% | 20.2% | 36.4% |
| Practice good eating habits | 7.4% | 12.7% | 13.9% | 24.1% | 41.9% |
| Lose weight, or maintain healthy weight | 6.2% | 15.0% | 16.1% | 25.8% | 36.8% |
| Handle stress well | 6.3% | 12.1% | 9.8% | 18.4% | 53.4% |
Figure 5.
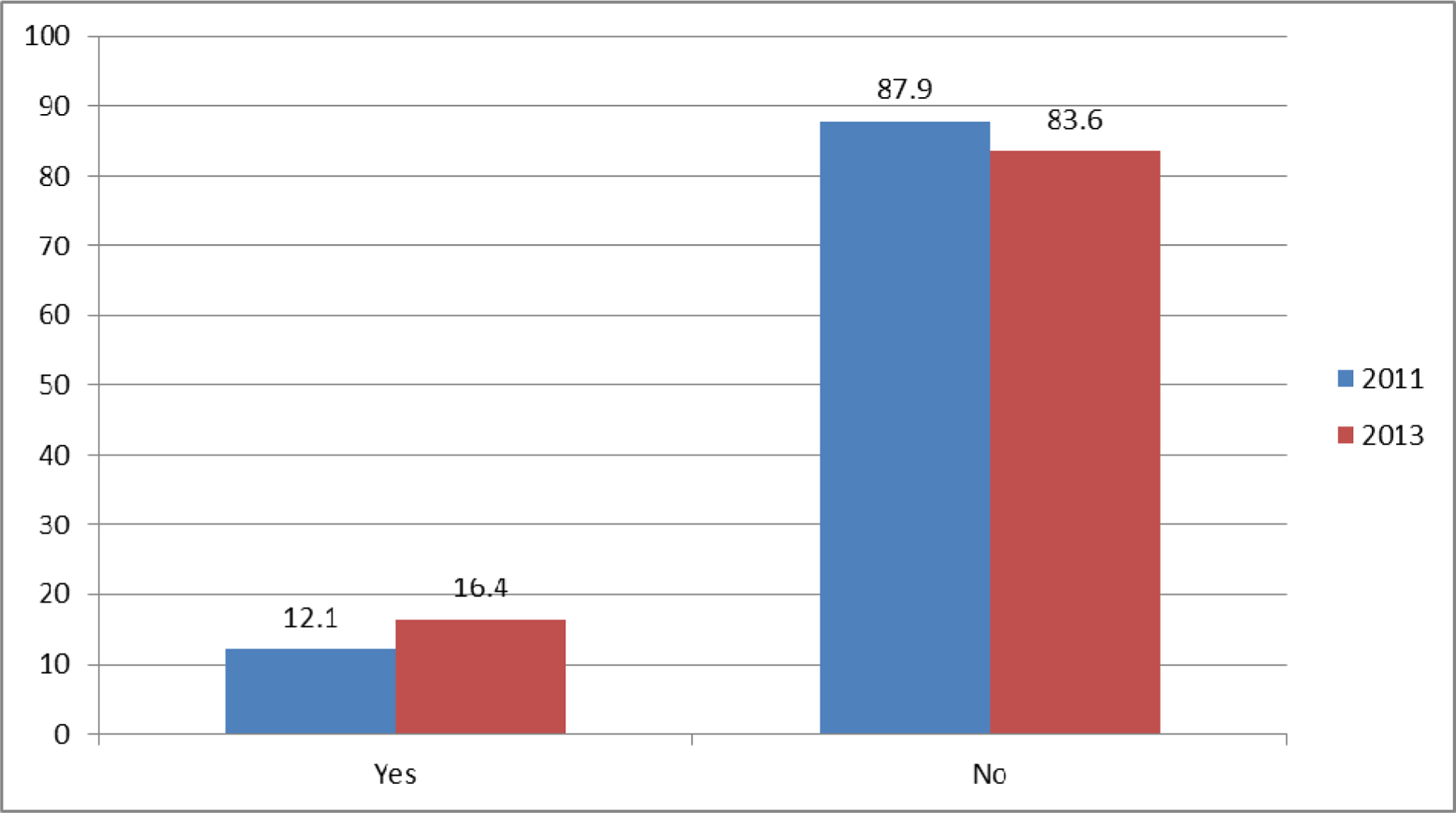
Major depression in correction officers (CES-D) 2013
Figure 6a.
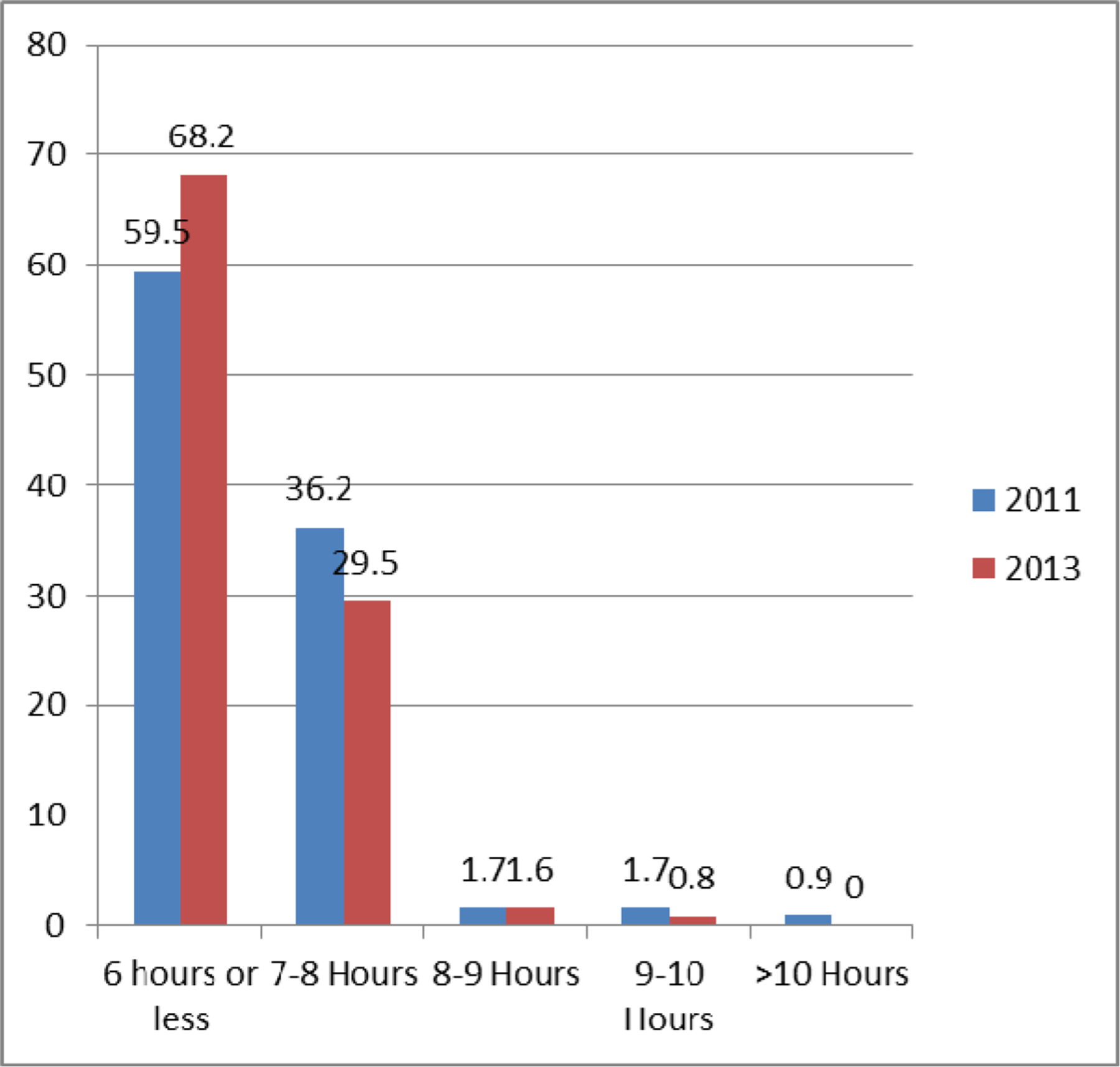
Hours of sleep typical work week
Figure 6b.
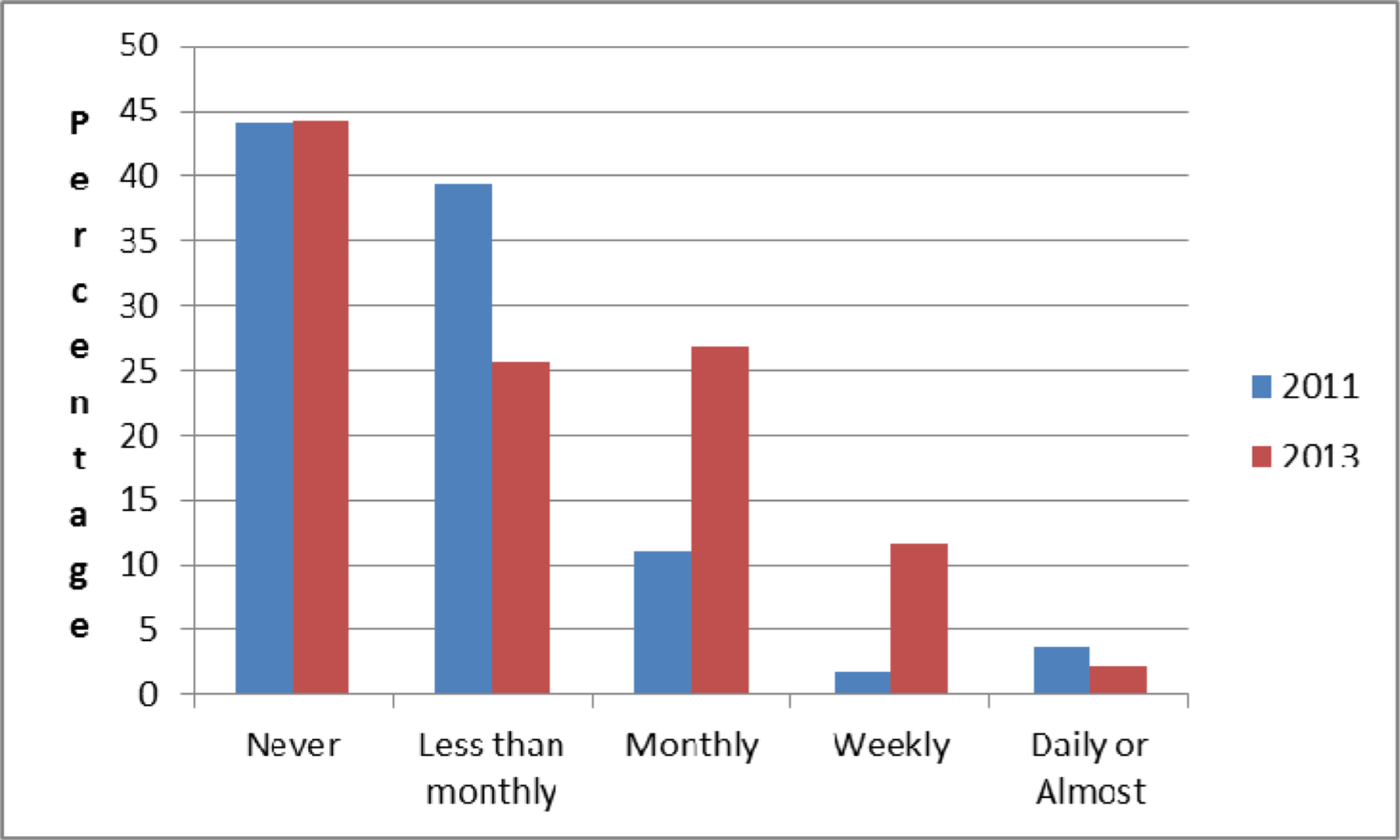
% 6 or more drinks at a time
There was no change over the 2 year interval from 2010 (Year 5) to 2013 (Year 7) in the frequency of participants denying heavy drinking (6 or more drinks at a session), the level being 44% in both years. However, among the 56% who reported episodic heavy drinking, the frequency distribution changed substantially. There was an almost doubling in reported episodes of heavy drinking at least once per month --30.2% in 2013 compared with 16.5% in 2011. This between-year difference was entirely attributable to the decline in reports of heavy drinking occurring less than once per month --25.6% in 2013 compared with 39.4% in 2011.
Increased levels of hypertension, a greater prevalence of heavy drinking, relatively increased levels of depression and few hours of sleep were not, however, conclusive evidence of an indifference to lifestyle risk factors or diffidence towards workplace health promotion. The frequency of current smoking was unchanged, 17.3% in 2011 and 17.1% in 2013. There are various explanations of underlying reasons for these more ominous health indicators. These include greater candor towards repeated surveys and budgetary and staffing constraints. There is no single identifiable association at this time.
3.2. Process Change and Evaluation Outcomes
DT3 and KET4 process goals are represented in Table 5. The different intervention content and ordering of priority mitigates against exact comparison of evaluation metrics between sites.
Table 5.
Status of Process Milestones
| Kaizen Site A | Design Team Site B | ||||
|---|---|---|---|---|---|
| BILDa | BFEDb | ||||
| Participatory Engagement | Labor-management participation | √ | √ | Stable attendance rates | √ |
| Completion of kaizen effectiveness team in 90 days | ↓ | NA | Meeting at least monthly | √√ * | |
| Involvement in upper level design | √ | √ | Use of technical consultation | √ | |
| Complete BILD and BFED in 1 year | ↓ | NA | Schedule conflict resolution | √ | |
| Use of short surveys | √ | NA | Inclusion of 4 interventions | √ | |
| Meeting attendance | ↓ | √ | Design team engaged in dissemination | √ | |
| Meeting frequency | ↓ | √ | |||
| Program Policy | Release team for staff | √ | √ | Correction officers released or cross-covered | √ |
| Use of IDEASc | ↓ | √ | Use of IDEAS | √ | |
| Completion of all IDEAS steps | ↓ | NA | Completion of all IDEAS steps | ↓ | |
| Full use of media and roll call | ↓↓ | NA | Full use of media and roll call | √ | |
| Compliance with Intervention | √ | NA | Compliance with BILD intervention | √ | |
Design team meets 2x per month and has petitioned the Facility Specific Steering Committee for weekly meeting.
BILD = Building Improvement Linked to Design
BFED = Better Food through Education and Design
IDEAS = Intervention Design and Analysis Scorecard
Legend
not applicable
fulfilled
surpassed
not met
major deficiency
Site A.
the BILD5 ‘team metric’ evolved considerably as walk-through and interviews established that principal problems were less related to hearing acuity, the original focus group complaint, than to elevated background noise from inmate activities and often deliberate efforts to override CO1 radio communications. The same approach lead to the creation of an IAQ9 survey and air quality evaluation by study team industrial hygienists. Thirty-two officers participated in identifying noise and IAQ9 problem areas. There were two IAQ9 process goals: purchasing and scheduled utilization of HVAC cleaners, and modification of the air duct and cleaning schedules. The KET4 identified two problems affecting noise and communications: poor design of the CO1 radio shoulder-worn speakers and poor sound damping in critical areas. Three areas and appropriate damping and noise cancelling panels were identified as pilot locations. A final decision on location and follow-up evaluation rests on current budgetary allocation. Substitute radio headsets and earbuds were reviewed by the KET4. Five combinations, including contoured devices were selected for pre- and post- evaluation. The entire process has transpired over more than a year is still not yet complete.
BFED7 was selected as the second project. The new KET4 no overlapping members with the BILD5 KET4. There have been 6 active members, including a deputy warden and 2 supervisors. The KET4 met every two weeks and strictly adheres to planning steps in the IDEAS12. While it is too early to consider outcomes, as Table 5 demonstrates, there are already significantly improvements in engagement compared with the BILD5 predecessor. Adopted measures have included, changes in vending choices, contracting with area restaurants to construct healthier menus, and an extensive information campaign with workforce designed posters and materials. These are elaborated on in the Discussion section. The W-2 BFIT6 and SWIPE8 interventions are pending.
Overall, KET4 representation has followed HITEC2 2 projections. The KET4 that was assigned the BILD5 project included the warden, maintenance engineers, COs1, supervisors, and senior administrative personnel. A key evaluation metric, completion of the task within 120 days, has not been met. A principal obstacle has been the problem of aligning schedules, which has reduced the frequency of KET4 session to <1/month. Use of the State vendor system further delayed actions despite expectations that the KET4 approach could overcome procurement obstacles. Another key evaluation metric, team membership continuity and consistency, has not been realized due to staff changes and meeting infrequency. Three of four COs1 and the responsible deputy warden retired or transferred during the KET4 project timeline.
Site B.
The DT3 met its initial evaluation criteria by meeting regularly at least once per month with 3 or more COs1 in attendance. The general BILD5 approach was addressed in two proposed projects: 1) IAQ9 assessment leading to changes in the cleaning schedule and improvement in temperature variability, 2) stress reduction by alterations in the physical environment. The IAQ9 initiative was readily adopted by the Facility Specific Steering Committee. A proposal to improve officer safety and awareness through strategic placement of mirrors was rejected by the FSC5, after exploration, due to concern with security from mirrors being weaponized. A program to construct stress reduction area(s) was initially rejected by the Facility Specific Steering Committee because of concerns over abandoned posts and limited available space. However, the iterative IDEAS12 process is functioning with engagement of the Study Wide Steering Committee.
One critical outcome of the DT3 process has been reinforcement of the necessarily structured participatory approach to intervention planning. The assiduous application of the IDEAS12 is a prolonged, even permanent process, as each intervention focus requires the development of three alternative approaches to increase the likelihood of Facility Specific Steering Committee support, including development by the DT3 of evaluation and selection criteria (Step 3) which are applied to each intervention alternative. For point of illustration, in Figure 7, the specific content for Step 2 and Step 4 that were generated by the DT3 are posted for the IAQ9 project. To appreciate the sophistication of the DT’s3 approach, it should be noted that DT3 members requested and received specific training in IAQ9 assessment by the State of Connecticut. The DT3 also worked with the study team to design and administer a short survey identifying both problematic work areas and respiratory complaints in the active workforce. The DT3 was also able to avail itself of data on respiratory symptoms reported in the baseline survey. Within the CO1 population, 15% reported either a diagnosis of asthma or met criteria for a diagnosis of asthma (DeMarco et al., 2000; European Survey 2002). Among non-CO1 staff, the level was higher – 27%.
Figure 7.
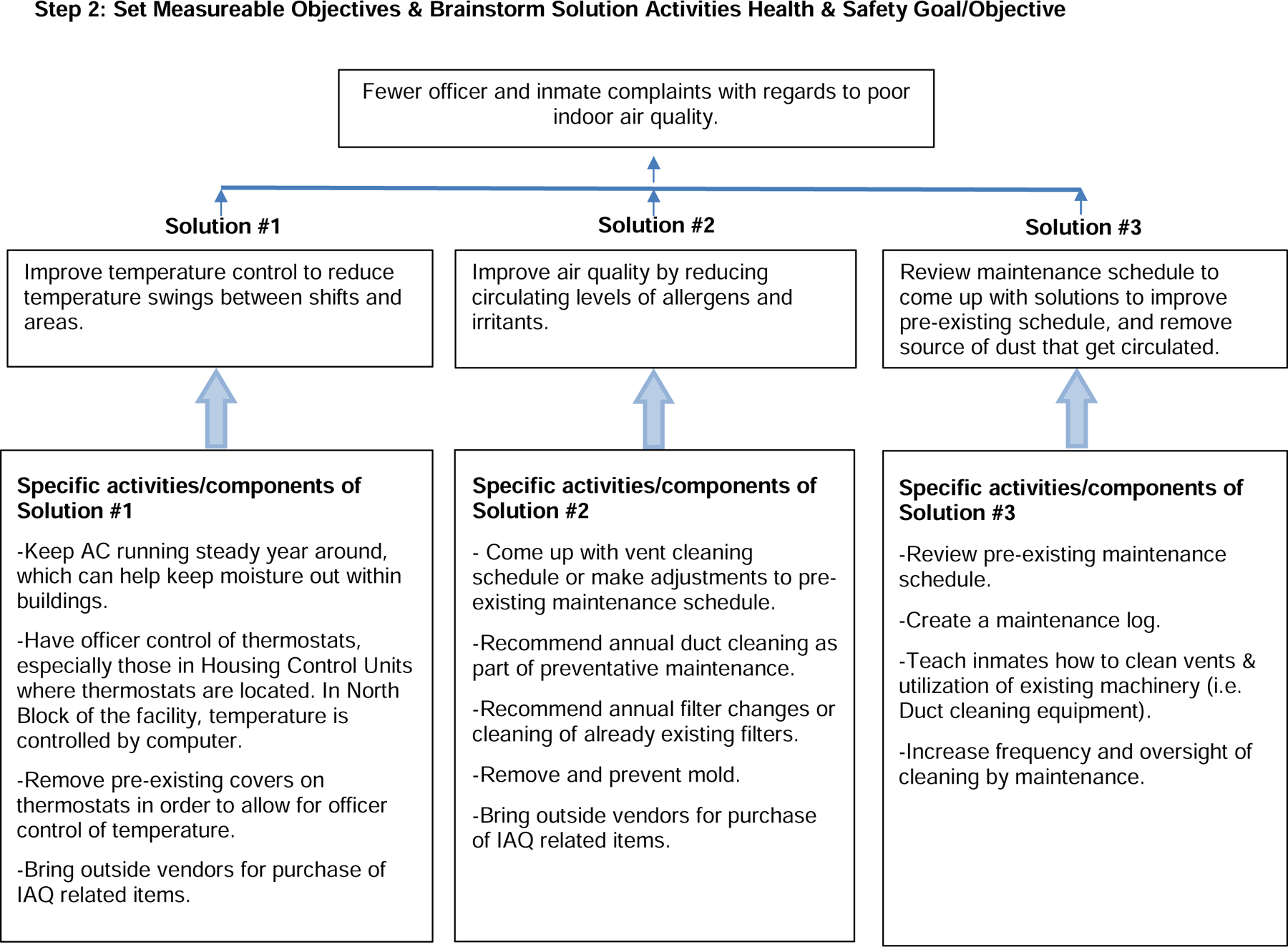
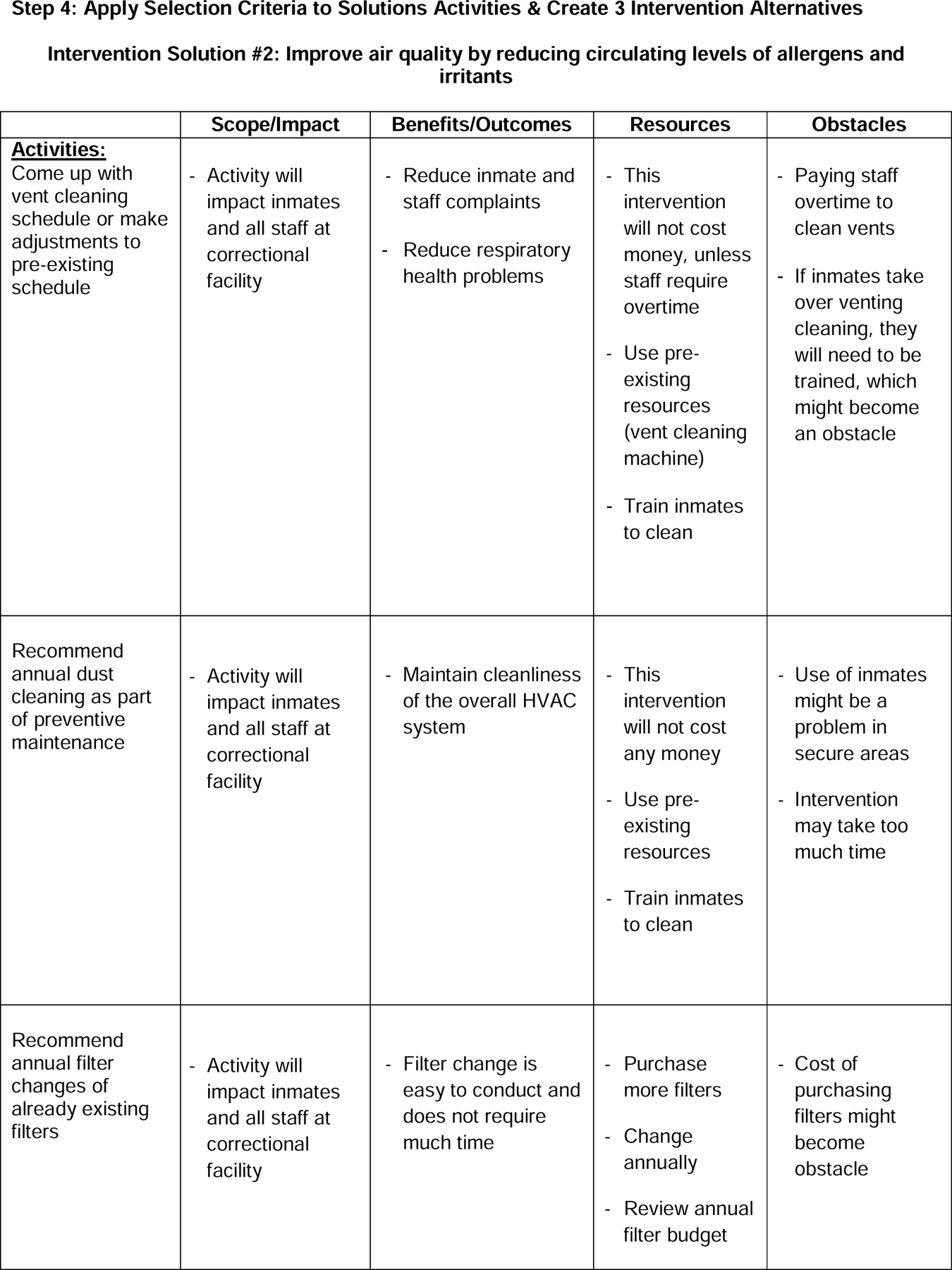
IDEAS Graphics: Steps 2 & 4.
The DT3 has also been running its own weight loss and nutrition program, entitled Weight no More. It administered its own survey based on HITEC2 materials. A potential flaw of participatory interventions is the loss of morale on the part of the engaged members of the workforce because of the long duration and often partial successes of interventions. In this context, the weight loss program is presented as a result for contextual reasons. The program had been previously developed and did not require the IDEAS12. The DT3 introduced it to get a quick to investment by the workforce while the longer-term and more complex intervention planning efforts were underway. Interestingly, weight loss programs are usually considered the most easily introduced and reliably successful WHP activities (Benedict and Arterbum, 2008; Heaney and Goetzel, 1997). In this case, the DT3 approached weight loss as a process, and part of a longer term strategy, rather than an outcome. At the current time, the DT3 has had a sustainable process for reaching program goals (see Table 5). This is particularly illustrated by the stability of the team meeting process, use of direct CO1 participatory communications, such as roll calls, and more effective use of problem solving instruments.
4. Discussion
This current and second phase of intervention research in corrections began with uncertainties. A primary concern was that the KET4 and DT3 approaches were insufficiently dissimilar and would decant into a convergent intervention program. Another concern was that the KET4, with its emphasis on shorter-term measurable outcomes, would too naturally align with the Connecticut Department of Correction culture of problem-directed initiatives, such as lock downs for weapon and drug searches. This professional cultural bias, along with the greater and more immediate access to upper level design and decision making seemed to give the KET4 structural advantages over the DT3. To date, however, events have not supported the superiority of the KET4 approach.
The IDEAS12 has proven to be effective at Site B because of its detailed staging which obliges local and central administration to respond to the DT3 at each completed step. While the detailed, security-driven, and procedural nature of work in corrections naturally invites structured and contingent planning by officers and administrators, the translation of the IDEAS12 to the KET4 was not automatic for the BILD5 intervention. At Site A, the IDEAS12 was used sporadically and none of the selected BILD5 interventions progressed beyond Step 2. Completing the design steps in order had become an imposition, rather than an intuitively applicable planning aid.
The greater intervention planning effectiveness to date at Site B has several apparent explanations. First, the responsibility for each intervention plan along with the solicitation of external technical consultants rested entirely with COs1. While realization depended and still depends on responsiveness to recommendations at more senior levels, there is no reflexive deference to managers for decision making; furthermore failed execution cannot be attributed to a supervisor. Second, the attendance by experts and senior administrators at KET4 meetings favored a process of executive or administrative decision making. While specific solutions could be realized or rejected over a shortened process, line officer engagement took a more customary form of censoring and deference to information provided by higher authority. Third, the frequency and intensity of planning sessions and continuity of attendance came more easily to the DT3 site. Redundant membership and substitution by team members was more practical for a DT3 composed of CO1 peers, rather than a multi-organizational KET4, where critical absences by non-facility based key personnel compromised team function.
Nevertheless, it is too early to conclude that a DT3 will continue to be superior to a KET4 in corrections, particularly since, consistent with PAR, KET4 shortcomings are continuously corrected. Some of the difficulties at the KET4 site may have been related to the choices for the initial intervention program. The sequence of BILD5, followed by BFED7, was determined by the Study Wide Steering Committee. The assumption was that an ergonomic program directed principally to the external environment would be a more acceptable starting point than a lifestyle oriented intervention. A second assumption was that key State personnel in facilities and engineering who were essential to BILD5 should be represented at all KET4 sessions. The physical environment may have been too diffuse a target. IAQ9, noise and communications, and physical work conditions are each complex and necessitate discrete intervention efforts. Qualitative follow-up suggests that a committed participatory action team can accept the 7-step IDEAS12 intervention planning approach but the approach remains cumbersome whenever there are too many complex issues, infrequent meetings, and limited team continuity. The BFED7 intervention, which is currently underway, may prove to be a more accessible platform for the KET4 because of tighter, single theme focus. Other factors include the reduced expectations on attendance of senior offsite personnel and the inclusion of supervisory personnel who were more distant from expected retirement.
Some of the barriers for all participatory work in corrections stem from the complexities of scheduling and the difficulty of aligning CO1 schedules with those of managers, supervisors and extra Department of Correction resources. Currently 76% of COs1 who are study participants are working > 9 hours per week of voluntary overtime and for 48%, the weekly commitment is in excess of 17 hours. The term ‘voluntary’ must be prefaced by appreciation that overtime is treated as a futures market with forced holdovers being an undesired option, but with withdrawal from schedule hours being penalized. Issues around overtime are complex, being the product of both highly structured and participatory negotiation and the ongoing public sector budgetary crises’ that discourage the creation of new positions or even full replacement of retirees. Because of the complexity of overtime and scheduling and limited back-up personnel, there are major impediments to scheduling labor-management cooperative engagement. Overtime and shift work are process issue that are endemic to corrections and complicate participatory activity; they also introduce potential health issue because of effect on sleep, stress, fatigue, and work-family conflict. These issues are currently under study in HITEC2 2. Connecticut Department of Correction and its bargaining unit have been very flexible in accommodating a mutually valued program. However, the perpetual short staffing and overtime demands pose a structural problem whose resolution will require a significant change in both the culture of corrections and in the ability of the State to liberalize employment policies.
Connecticut Department of Correction and its bargaining unit have been very flexible in accommodating the mutually valued health promotion program. However, the perpetual short staffing and overtime demands pose a structural problem whose resolution will require a significant change in the culture of corrections by requiring balancing of personal and family perspective with income and in the culture of public sector allocations by monetizing the quality of work life.
The factors that most motivate the DT3, KET4, Facility Specific Steering Committee and Study Wide Steering Committee are the severity of the health risk profiles, and the young age at their expression. As Table 3 presented, the CO1 population is at risk for cardiovascular and mental health disorders, and the risk profile has not improved over the lifespan of HITEC2. While all of this evidence contributes to a perception of overall awareness and concern, problems remain intractable, structural or implicit in the corrections culture. Budget cuts have been continuous for the past 5 years. Structural problems are not, however, impermeable barriers. Focus groups and key interviews demonstrate a growing recognition that cultural change is a long-term investment and these types of health and work life related interventions are new to corrections. Such investments have a longer history in other hazardous duty services, such as police (Parks and Steelman, 2008) and fire (Dishman et al., 1998; Cowen, 2010), where it has taken several decades to build the appropriate research and intervention base, and familiarity and fluency within the profession.
To date, the entire HITEC2 study can be summarized as successful, when measured by participatory engagement, but, at best, equivocal in its documentable effect on key adverse health parameters in COs1. A longer-term view that placed particular value on quality of work or recognized the extended timeframe that may underlie change in work and professional culture, particularly in a constrained work environment, may be a legitimate explanation for the uncertainty with health outcomes. But, explanation is not a result. At many organizational levels, personnel in the Connecticut Department of Correction recognize the problems of stress, premature mortality, and suicide in COs1, and have invested time and resources in a variety of efforts to improve the physical and mental health of corrections staff. These include, health and safety committees, work stress committees, quality of life committees, an extensive Employee Assistance Program, crisis management committees, administratively initiated mentoring of new cadets, and a crisis management team. Therefore, it may not be altogether obvious why HITEC2 2 should continue to generate support and engagement given existing and abandoned parallel efforts. There are multiple signs of organizational commitment and change that appear to be evolving independently of measured health parameters. The BFED7 intervention, which the KET4 renamed Eating for Action’ has been adopted throughout the Department of Correction system. The supervisors have begun their own health improvement program that involves the study staff, but is internally managed, while reporting to the Study Wide Steering Committee and the still evolving interventions around fitness and injury are both complex and thorough. There are at least four likely explanations for growing adherence and commitment.
First, the long tenure (25 years to full retirement benefits) of COs1 and common experiences of COs1, supervisors, and administrators, personalizes and localizes the health and disease of the workforce. Funerals of co-workers are widely attended; home visits to personnel deployed abroad in the National Guard or Reserves are performed and valued; and rank and status tend to dissolve around non-work personal hardship. The work is recognized both for its stresses and by its perceived societal disdain. The actual levels of morbidity were not known to the workforce before HITEC2, but the results have reinforced the notion that solutions are both difficult and long-term. Second, determining a beginning point has been elusive. As Table 3, demonstrates, over 5 years the number of engaged personnel has increased by 65%. At Site B, there was an original prohibition of lieutenants and captains from the staff DT3 because of the concern with supervisory censoring and confidentiality. A separate supervisor DT3 was formed and functioned until staffing reductions made attendance at regular meetings impossible Acceptance of the intervention program has been gradual. It can be argued that until the program proves its sustainability, there is not yet a true point of origination. This may be a somewhat contrarian formulation to the usual dictum that first there is a demonstration of overwhelming effectiveness before issues of sustainability arise. Third, HITEC2 has offered a pathway that is deferential to but also outside of labor-management negotiations. The difficulties of the Department of Correction work climate are implicitly understood. Overcrowding is beyond the authority of inmates or officers. Similarly, restricted budgets have limited new hiring and expansion of personnel in corrections in many states, including Connecticut. Issues involving the fitness of COs1, work avoidance, and endemic overeating and obesity are recognized and agreement on underlying factors commonly articulated. Collective bargaining is limited when the solutions are complex and experimentation is necessary. And, fourth, the commitment of a university based study team has been magnetic in ways that customary vendor-supplied or administratively directed programs cannot duplicate. With 7 years of engagement, and extensive involvement in the organizational structure of the intervention, the research team has become part of an institutional culture and replaced the usual expectation that prisons are studied and then left behind. There is also a curious feature of a university research group. Graduate students and research assistants are inevitably replaced with their successors. While this introduces new thinking and energy around PAR engagement, it is also replicates key aspects of Department of Correction work culture, where officers and supervisors are continuously replaced by trainees due to retirement and transfer. Of course, the intensity and experimentation that can reside within an academic research program are limited resources. They require a no less sophisticated process of dissemination.
5. Conclusions
The PAR approaches for workplace intervention planning and implementation within corrections are robust and sustained. Innovative personal health and work organization programs have been introduced in key areas. Their long-term effectiveness in an increasingly stressed population is not yet clear.
Highlights.
A participatory action research project implemented with correctional officers is described
We examine 2 different participatory approaches that use the IDEAS tool
Outcomes are varied based on intervention theme and implementation
Acknowledgements
This publication was supported by grant Number 1U19OH008857 from the National Institute for Occupational Safety and Health (NIOSH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CO = Correction Officer(s)
HITEC = Health Improvement through Employee Control
DT = Design Team
KET = Kaizen Effectiveness Team
BILD = Building Improvement Linked to Design
W-2 BFIT = Work to be Fit
BFED = Better Food through Education and Design
SWIPE = Structured Work-related Injury Prevention through Ergonomics
IAQ = Indoor Air Quality
IAS = Intervention Assessment Survey
NPAQ = Nutrition and Physical Activity Questionnaire
IDEAS = Intervention Design and Analysis Scorecard
References
- Benedict MA, Arterburn D, 2008. Worksite-based weight loss programs: a systematic review of recent literature. Am. J. Health Promot, 22(6), 408–416. doi: 10.4278/ajhp.22.6.408. [DOI] [PubMed] [Google Scholar]
- Bourbonnais R, Jauvin N, Dussault J, Vezina M, 2007. Psychosocial work environment, interpersonal violence at work and mental health among correctional officers. Int. J. Law Psychiatry, 30(4–5), 355–368. [DOI] [PubMed] [Google Scholar]
- Cowen VS, 2010. Functional fitness improvements after a worksite-based yoga initiative. J. Bodyw. Mov. Ther 14(1), 50–54. doi: 10.1016/j.jbmt.2009.02.006. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J 2003. The validity of self‐reports of alcohol consumption: state of the science and challenges for research. Addiction, 98(s2), 1–12. [DOI] [PubMed] [Google Scholar]
- de Marco R, Locatelli F, Sunyer J, Burney P, 2000. Differences in incidence of reported asthma related to age in men and women: a retrospective analysis of the data of the European Respiratory Health Survey. Am. J. Respir. Crit. Care Med, 162(1), 68–74. [DOI] [PubMed] [Google Scholar]
- Dishman RK, Oldenburg B, O’Neal H, Shephard RJ 1998. Worksite physical activity interventions. Am. J. Prev. Med, 15(4), 344–361. [DOI] [PubMed] [Google Scholar]
- Duffy VB, Hayes JE, Sullivan BS, Faghri P, 2009. Surveying food and beverage liking: a tool for epidemiological studies to connect chemosensation with health outcomes. Ann. N Y Acad. Sci 1170(01), 558–568. [DOI] [PubMed] [Google Scholar]
- European Community Respiratory Health Survey II Steering Committee, 2002. The European Community Respiratory Health Survey II. European Respiratory Journal, 20(5), 1071–1079. [DOI] [PubMed] [Google Scholar]
- Faghri PD, Duffy VB, Benson NR, Cherniack MG, 2012. Worksite weight loss intervention for employees in stressful workplaces: a pilot study and baseline survey indicators of success. J. Obes. Weight Loss Ther, 2(2), 100021. doi: 10.4172/2165-7904.1000121. [DOI] [Google Scholar]
- Faghri PD, Kotejoshyer R, Cherniack M, Reeves D, Punnett L, 2010. Assessment of a worklife health promotion readiness checklist. J. Occup. Environ. Med, 52(9), 893–899. doi: 10.1097/JOM.0b013e3181efb84d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris JA, Van Aken EM, Doolen TL, Worley J, 2009. Critical success factors for human resource outcomes in Kaizen events: an empirical study. Int. J. Prod. Econ, 117(1), 42–65. doi: 10.1016/j.ijpe.2008.08.051. [DOI] [Google Scholar]
- Ferraro L, Faghri PD, Henning R, Cherniack M, 2013. Workplace-based participatory approach to weight loss for correctional employees. J. Occup. Environ. Med, 55(2), 147–155. doi: 10.1097/JOM.0b013e3182717cd4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover WJ, Farris JA, Van Aken E, Doolen T, 2011. Critical success factors for the sustainability of Kaizen event human resource outcomes: an empirical study. Int. J. Prod. Econ, 132, 197–213. doi: 10.1016/j.ijpe.2011.04.005. [DOI] [Google Scholar]
- Heaney CA, Goetzel RZ, 1997. A review of health-related outcomes of multi-component worksite health promotion programs. Am. J. Health Promot, 11(4), 290–307. [DOI] [PubMed] [Google Scholar]
- Henning R, Warren N, Robertson M, Faghri P, Cherniack M; CPH-NEW Research Team, 2009. Workplace health promotion through participatory ergonomics: an integrated approach for greater effectiveness and sustainability. Public Health Rep, 124(S1), 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB, 2001. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ. Health, 14(2), 182–197. [DOI] [PubMed] [Google Scholar]
- Koelen MA, Vaandrager L, Colomér C, 2001. Health promotion research: dilemmas and challenges. J. Epidemiol. Community Health, 55(4), 257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obidoa C, Reeves D, Warren N, Reisine S, Cherniack M, 2011. Depression and work family conflict among correction officers. J. Occup. Environ. Med, 53(11), 1294–1301. doi: 10.1097/JOM.0b013e3182307888. [DOI] [PubMed] [Google Scholar]
- Obidoa CA, Reisine SL, Cherniack M, 2010. How does the SF-36 perform in healthy populations? A structured review of longitudinal studies. J. Social Behav. Health Sci, 4(1), 30–48. doi: 10.5590/JSBHS.2010.04.1.02. [DOI] [Google Scholar]
- Parks KM, Steelman LA, 2008. Organizational wellness programs: a meta-analysis. J. Occup. Health Psychol, 13(1), 58. doi: 10.1037/1076-8998.13.1.58. [DOI] [PubMed] [Google Scholar]
- Punnett L, Cherniack M, Henning R, Morse T, Faghri P; CPH-NEW Research Team, 2009. A conceptual framework for the integration of workplace health promotion. Public Health Rep, 124(S1),16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punnett L, Warren N, Henning R, Nobrega S, Cherniack M; CPH-NEW Research Team, 2013. Participatory ergonomics as a model for integrated programs to prevent chronic disease. J. Occup. Environ. Med, 55(12S), 19–24. doi: 10.1097/JOM.0000000000000040. [DOI] [PubMed] [Google Scholar]
- Radloff LS, 1977. The CES-D scale: a self-report depression scale for research in the general population. App. Psychol. Meas, 1, 385–401. [Google Scholar]
- Reason P, Bradbury H, 2001. Handbook of Action Research Thousand Oaks, CA: Sage. [Google Scholar]
- Robertson M, Henning R, Warren N, Nobrega S, Dove-Steinkamp M, Tibirica L, Bizarro A; CPH-NEW Research Team, 2013. The Intervention Design and Analysis Scorecard: a planning tool for participatory design of integrated health and safety interventions in the workplace. J. Occup. Environ. Med, 55(12S), S86–88. doi: 10.1097/JOM.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaufeli WB, Peeters MCW, 2000. Job stress and burnout among correctional officers: a literature review study. Int. J. Stress Manage, 7(1), 19–48. doi: 10.1023/A:1009514731657. [DOI] [Google Scholar]
- Small SA, 1995. Action-oriented research: models and methods. Journal of Marriage and the Family, 57, 941–955. doi: 10.2307/353414. [DOI] [Google Scholar]
- Stockwell T, Donath S, Cooper‐Stanbury M, Chikritzhs T, Catalano P, Mateo C, 2004. Under‐reporting of alcohol consumption in household surveys: a comparison of quantity–frequency, graduated–frequency and recent recall. Addiction, 99(8), 1024–1033. [DOI] [PubMed] [Google Scholar]
- Tiesman HM, Hendricks SA, Bell JL, Amandus HA, 2010. Eleven years of occupational mortality in law enforcement: The Census of Fatal Occupational Injuries, 1992–2002. Am. J. Ind. Med, 53(9), 940–949. doi: 10.1002/ajim.20863. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Turner-Bowker DM, Gandek B SF-12v2™: How to Score Version 2 of the SF-12® Health Survey Lincoln, RI: QualityMetric Incorporation. [Google Scholar]
- Weinstein BE, Ventry IM, 1982. Hearing impairment and social isolation in the elderly. J. Speech Hear. Res, 25(4), 593–599. [DOI] [PubMed] [Google Scholar]


