Abstract
Introduction
Chronic myelomonocytic leukemia (CMML) and myelodysplastic syndromes (MDS) with ring sideroblasts (RS) or SF3B1 mutation (MDS-RS/SF3B1) differ in many clinical features, but share others, such as anemia. RS and SF3B1 mutation can also be found in CMML.
Methods
We compared CMML with and without RS/SF3B1 and MDS-RS/SF3B1 considering the criteria established by the 2022 World Health Organization classification.
Results
A total of 815 patients were included (CMML, n=319, CMML-RS/SF3B1, n=172 and MDS-RS/SF3B1, n=324). The percentage of RS was ≥15% in almost all CMML-RS/SF3B1 patients (169, 98.3%) and most (125, 72.7%) showed peripheral blood monocyte counts between 0.5 and 0.9 x109/L and low risk prognostic categories. CMML-RS/SF3B1 differed significantly from classical CMML in the main clinical characteristics, whereas it resembled MDS-RS/SF3B1. At a molecular level, CMML and CMML-RS/SF3B1 had a significantly higher frequency of mutations in TET2 (mostly multi-hit) and ASXL1 (p=0.013) and CMML had a significantly lower frequency of DNMT3A and SF3B1 mutations compared to CMML/MDS-RS/SF3B1. Differences in the median overall survival among the three groups were statistically significant: 6.75 years (95% confidence interval [CI] 5.41-8.09) for CMML-RS/SF3B1 vs. 3.17 years (95% CI 2.56-3.79) for CMML vs. 16.47 years (NA) for MDS-RS/SF3B1, p<0.001. Regarding patients with CMML and MDS, both with SF3B1 mutation, survival did not significantly differ. CMML had a higher risk of transformation to acute myeloid leukemia (24% at 8 years, 95%CI 19%-30%).
Discussion
CMML-RS/SF3B1 mutation resembles MDS-RS/SF3B1 in terms of phenotype and clearly differs from CMML. The presence of ≥15% RS and/or SF3B1 in CMML is associated with a low monocyte count. SF3B1 mutation clearly improves the prognosis of CMML.
Keywords: CMML-RS/SF3B1 , CMML, MDS-RS/SF3B1 , phenotype, mutational profile, prognosis
Introduction
Monocytosis (≥0.5 x109/L and ≥10%) in peripheral blood is the hallmark of chronic myelomonocytic leukemia (CMML). A subset of myelodysplastic syndromes (MDS) presents with ring sideroblasts (RS) mostly associated with SF3B1 (splicing factor 3B, subunit 1) mutation and are recognized as a subgroup of MDS by the 2022 World Health Organization (WHO) classification (called MDS with low blasts and mutated SF3B1 or MDS with RS) and the International Consensus Classification of Myeloid Neoplasms and Acute Leukemias (ICC) of 2022 (called MDS with mutated SF3B1) (1–3).
CMML and MDS with RS/SF3B1 mutation differ in many clinical features but share others, such as anemia. In MDS, defective erythropoiesis includes impaired early and terminal erythroid maturation, which involves the development of RS, mostly associated with the presence of SF3B1 mutation. The clinical presentation of CMML is more heterogeneous, while anemia is often present and more frequent and severe in the myelodysplastic subtype.
Treatment with erythropoietic stimulating agents is the standard of care of symptomatic anemia in low-risk MDS and CMML (4, 5). Beyond this first line, there are limited options for the treatment of anemia in lower-risk MDS/CMML. Luspatercept is a novel activin receptor type IIB fusion ligand trap agent that has shown activity for treating anemia in patients with MDS-RS/SF3B1 and has been approved for this indication (6–8).
RS and SF3B1 mutation can also be found in CMML. In a study of 226 patients with CMML, 6% harbored the SF3B1 mutation (mostly the K700E variant), with this mutation being strongly associated with the presence of ≥15% RS and mutually exclusive with mutations in other splicing genes, such as SRSF2 and U2AF1. Interestingly, these other splicing mutations were also associated with the presence of RS, suggesting that this feature in CMML is not restricted to the presence of a mutant SF3B1 clone (9). It has been suggested that SF3B1 mutation defines a unique entity within all myeloid neoplasms, but distinctive clinical and biological features and prognosis have been observed between MDS and MDS/MPN harboring this mutation, which would argue against the idea of classifying SF3B1-mutant myeloid neoplasms as a single entity (10–13). On the other hand, ASXL1 and SRSF2 mutations are infrequent in SF3B1 mutant CMML, which may suggest that SF3B1 mutant CMML differs clearly from CMML without SF3B1 mutations and this specific biological profile translates into a distinct phenotype and survival rate (12, 13).
On the other hand, monocytosis (monocyte count >0.6 x109) is not uncommon in patients with MDS with low blast count (< 5%). Within the RS phenotype, 20% of patients show monocytosis and there seems to be a positive correlation between the percentage of RS and absolute monocyte count, with the overall survival (OS) being significantly shorter (14). Moreover, the absolute monocyte count at diagnosis may affect the prognosis in MDS independently of the Revised International Prognostic Score System (IPSS-R) risk score, and monocytopenia (<0.2 x109/L) may be associated with a higher risk of acute myeloid leukemia (AML) transformation (15).
We aimed to describe the clinical characteristics and prognosis of CMML patients with SF3B1 and/or ≥15% RS (CMML-RS/SF3B1) and compare them with CMML without this feature and with MDS-RS/SF3B1. We hypothesize that a proportion of RS ≥15% (or less but with the presence of SF3B1 mutation) in the bone marrow of patients with CMML might define a subset of patients with biological characteristics that clearly differ from CMML without such features, and might have a clinical course closer to that of MDS-RS/SF3B1 and better than classical CMML. This is currently of special interest given that a lower monocyte count cut-off has been established for the diagnosis of CMML in the new 2022 WHO and ICC classifications, and thus, more patients who would have previously been diagnosed with MDS or MDS/MPN-Unclassifiable (MDS/MPN-U) are currently considered CMML.
Materials and methods
For this purpose, we included patients with CMML and MDS-RS/SF3B1 from the Spanish Registry of MDS, the Düsseldorf Registry and the Humanitas Research Hospital in Milan. We considered the 2022 WHO classification criteria for the diagnosis of CMML and MDS-RS/SF3B1. Among the CMML patients, we checked for the presence of RS (and SF3B1, if applicable, following the same criteria applied for the diagnosis of MDS-RS/SF3B1). Accordingly, CMML cases were divided into CMML and CMML-RS/SF3B1. Molecular data were collected when available. First, the presence of SF3B1 mutations, analyzed by either Sanger sequencing (exons 13-15) or next generation sequencing (NGS) (all coding exons), was recorded. In addition, the mutational profile across myeloid-related genes was collected in cases with available NGS data. The clinical characteristics as well as risk stratification considering the CMML-Prognostic Score System (CPSS) in both CMML and CMML-RS/SF3B1 and the IPSS-R in all three groups were recorded and compared. The OS and cumulative incidence of progression (CIP) to AML were also assessed. OS was calculated from the date of diagnosis to the date of death or last follow-up. The CIP to AML was measured from the date of diagnosis to the date of progression to AML, considering any death not due to progression as a competing event. Similarly, the two groups (CMML and MDS) harboring SF3B1 mutation regardless of the percentage of RS were also compared.
Statistical analysis
Baseline characteristics were described as median and range for quantitative variables and frequency and percentage for categorical variables. Comparisons of proportions, medians of variables between the groups were performed with the chi-square test, or Fisher’s exact and median test, as appropriate. OS was calculated with the Kaplan-Meier method, with the log-rank test for comparisons, and CIP to AML was estimated using cumulative incidence functions by competing risks analysis. Groups were compared by Gray’s test. Statistical analyses were performed with SPSS v.24 and R v.4.2.0 software.
Results
A total of 815 patients were included in the study (CMML, n=319, CMML-RS/SF3B1, n=172 and MDS-RS/SF3B1, n=324). The main clinical characteristics of the three groups are summarized in Table 1 .
Table 1.
Main clinical characteristic of the three groups of patients.
| CMML-RS/SF3B1
(n=172) |
CMML (n=319) |
MDS-RS/SF3B1
(n=324) |
CMML-RS/SF3B1
Vs CMML p |
CMML-RS/SF3B1 vs. MDS-RS/SF3B1 P |
|||
|---|---|---|---|---|---|---|---|
| Male, n (%) | 118 (68.6) | 232 (72.7) | 192 (59.3) | 0.335 | 0.041 | ||
| Age, median (range) | 76 (32–94) | 75 (28—95) | 73 (24-96) | 0.318 | 0.011 | ||
| Hemoglobin, median (range) | 9.8 (6.2-15.3) | 12 (6.6-17.1) | 9.750 (3.9-13.4) | <0.001 | 0.844 | ||
| Platelets, median (range) | 225 (15-853) | 120 (7-1067) | 225 (13-443) | <0.001 | 0.896 | ||
| Leukocyte count, median (range) | 5.6 (1.7-48) | 8.5 (2.5-111.7) | 5.04 (0.5-12.69) | <0.001 | 0.024 | ||
| Monocyte count, median (range) | 0.791 (0.5-22.419) | 1.9 (0.5-43.8) | 0.32444 (0-0.984) | <0.001 | <0.001 | ||
| Monocyte %, median (range) | 14.2929 (10-51.08) | 23.1729 (10-66.97) | 6.6051 (0-23) | <0.001 | <0.001 | ||
|
Monocyte count
x109/L |
<0.5 | 0 | 0 | 256 (79) | <0.001 | <0.001 | |
| 0.5-0.9 | 125 (72.7) | 14 (4.4) | 68 (21) | ||||
| ≥1 | 47 (27.3) | 305 (95.6) | 0 | ||||
| Neutrophils, median (range) | 2.6 (0.003-12.593) | 4.17935 (0.1-70.4) | 2.95 (0.036-9.720) | <0.001 | 0.025 | ||
| Peripheral blood blasts, median (range) | 0 (0-4) | 0 (0-10) | 0 (0-1) | 0.007 | 0.068 | ||
| Bone marrow blasts, median (range) | 2 (0-18) | 3 (0-19.4) | 1 (0-4) | <0.001 | 0.038 | ||
| FAB CMML n (%) | MD | 165 (95.9) | 232 (72.7) | – | <0.001 | – | |
| MP | 7 (4.1) | 87 (27.3) | |||||
| WHO 2022, CMML n (%) | CMML-1 | 166 (97) | 278 (87.1) | – | 0.001 | – | |
| CMML-2 | 6 (3) | 41 (12.9) | |||||
|
Bone marrow cellularity
n (%) |
Hypocellular | 1/156 (0.6) | 5/278 (1.8) | 8/294 (2.7) | 0.296 | 0.324 | |
| Normal | 39/156 (25) | 55/278 (19.8) | 73/294 (24.8) | ||||
| Hypercellular | 116/156 (74.4) | 218/278 (78.4) | 213/294 (72.4) | ||||
| 1 | 46/163 (28.2) | 88/305 (28.9) | 83/278 (29.9) | ||||
| 2 | 55/163 (33.7) | 124/305 (40.7) | 87/278 (31.3) | ||||
| 3 | 62/163 (38) | 80/305 (26.2) | 108/278 (38.8) | ||||
| RS, n (%) | Median, range | 42 (6-99) | 0 (0-13) | 42 (5-98) | <0.001 | 0.838 | |
| <5% | 0 | 311 (97.5) | 0 | <0.001 | 0.133 | ||
| 5%-14% | 3 (1.7) | 8 (2.5) | 14 (4.3) | ||||
| ≥15% | 169 (98.3) | 0 | 310 (95.7) | ||||
| SF3B1 mutation, n (%) | 61/87 (70.1) | 0/93 | 98/124 (79) | <0.001 | 0.139 | ||
| Dyserythropoiesis., n (%) | 145/149 (97.3) | 172/280 (61.4) | 255/259 (98.5) | <0.001 | 0.471 | ||
| Dysgranulopoiesis, n (%) | 96/141 (68.1) | 204/241 (84.6) | 167/233 (71.7) | <0.001 | 0.462 | ||
| Dysmegakaryopoiesis, n (%) | 79/142 (55.6) | 152/260 (58.5) | 144/240 (60) | 0.584 | 0.403 | ||
|
CPSS
n (%) |
Low | 66 (38.4) | 180 (56.4) | – | 0.001 | – | |
| Int-1 | 74 (43) | 87 (27.3) | |||||
| Int-2 | 28 (16.3) | 41 (12.9) | |||||
| High | 4 (2.3) | 11 (3.4) | |||||
|
IPSS-R
n (%) |
Very Low | 57/170 (33.5) | 84/292 (28.8) | 116 (35.8) | 0.189 | 0.016 | |
| Low | 75/170 (44.1) | 131/292 (44.9) | 164 (50.6) | ||||
| Intermediate | 29/170 (17.1) | 43/292 (14.7) | 36 (11.1) | ||||
| High | 8/170 (4.7) | 27/292 (9.2) | 3 (0.9) | ||||
| Very high | 1/170 (0.6) | 7/292 (2.4) | 5 (1.5) | ||||
|
Risk (IPSS-R)
n (%) |
Low | 149/172 (86.6) | 231/292 (79.1) | 292 (90.1) | 0.042 | 0.238 | |
| High | 23/172 (13.4) | 61/292 (20.9) | 32 (9.9) | ||||
CMML, chronic myelomonocytic leukemia; RS, ring sideroblasts; MDS, myelodysplastic syndrome; FAB, French-American-British; MD, myelodysplastic; MP, myeloproliferative; WHO, World Health organization; CPSS, Chronic myelomonocytic leukemia Prognostic Score System; IPSS-R, Revised International Prognostic Score System.Significant differences are highlighted in bold.
Within the group of CMML-RS/SF3B1, 165 (95.9%) had the myelodysplastic phenotype according to the French-American-British (FAB) classification and 166 (96.5%) had a low percentage of blasts (CMML1 according to WHO 2022). It is of note that the percentage of RS was ≥15% in most patients (169, 98.3%) with a median of 42 (6-99%), and SF3B1 mutation was present in 61 out of 87 evaluable patients (70.1%). The median hemoglobin level was 9.8 (range 6.2-15.3). In most CMML-RS/SF3B1 (125, 72.7%) the monocyte count in peripheral blood was between 0.5 and 0.9 x109/L (previously referred to as oligomonocytic CMML) and low risk categories by CPSS were predominant (low/intermediate-1 140, 81.4%), also after stratifying patients as low and high risk by IPSS-R considering the cut-off of 3.5 (n=149, 86.6%) ( Table 1 ). Around 70% of CMML cases had MD subtype and almost 90% CMML-1 in this series.
CMML-RS/SF3B1 significantly differed from classical CMML in the main clinical characteristics of the patients except for age, gender, bone marrow cellularity, dysmegakaryopoiesis and risk by IPSS-R, whereas it shared most of the clinical features with MDS-RS/SF3B1, excluding total and subsets of white blood cell counts. As expected, the median total monocyte count was higher in CMML-RS-SF3B1 compared to MDS-RS/SF3B1, but this value was still less than 1 x109/L (125, 72.7%) in most patients.
SF3B1 mutation was present in 61 patients with CMML and 98 patients with MDS. Considering this molecular feature, CMML-SF3B1 and MDS-SF3B1 were phenotypically very close, barely differing in absolute and relative monocyte count. Again, the absolute monocyte count was lower than 0.5 x109/L in most MDS-SF3B1 patients, whereas in the group of CMML-SF3B1 a range between 0.5 and 1 x109/L was predominant ( Table 2 ).
Table 2.
Main clinical characteristic of the two groups of patients with SF3B1 mutation.
| CMML-SF3B1
(n=61) |
MDS-SF3B1
(n=98) |
P | ||
|---|---|---|---|---|
| Male, n (%) | 36 (59) | 63 (64.3) | 0.505 | |
| Age, median (range) | 77 (48-94) | 74 (41-96) | 0.146 | |
| Hemoglobin, median (range) | 10 (6.8-15.3) | 9.850 (6.6-13.2) | 0.581 | |
| Platelets, median (range) | 246 (23-853) | 241 (26-437) | 0.821 | |
| Leukocyte count, median (range) | 5.6 (3.3-22.8) | 5.6 (1.73-11.94) | 0.980 | |
| Monocyte count, median (range) | 0.8 (0.5-5.470) | 0.4 (0.035-0.984) | <0.001 | |
| Monocyte %, median (range) | 14.4578 (10-37.22) | 7.6655 (1-17) | <0.001 | |
|
Monocyte count
x109/L |
<0.5 | 0 | 72 (73.5) | <0.001 |
| 0.5-1 | 48 (78.7) | 26 (26.5) | ||
| ≥1 | 13 (21.3) | 0 | ||
| Neutrophils, median (range) | 2.6895 (0.003-9.58) | 3.30400 (0.265-8.177) | 0.075 | |
| Bone marrow blasts, median (range) | 1 (0-10) | 1 (0-4) | 0.070 | |
|
Bone marrow cellularity
n (%) |
Hypocellular | 0 | 2/82 (2.4) | 0.441 |
| Normal | 14/51 (27.5) | 26/82 (31.7) | ||
| Hypercellular | 37/51 (72.5) | 54/82 (65.9) | ||
| Dysplastic lines | 1 | 24 (39.3) | 29/91 (31.9) | 0.632 |
| 2 | 15 (24.6) | 26/91 (28.6) | ||
| 3 | 22 (36.1) | 36/91 (39.6) | ||
| RS, n (%) | Median, range | 45 (6-91) | 41 (5-94) | 0.498 |
| 5%-14% | 3 (4.9) | 14 (14.3) | 0.063 | |
| ≥15% | 58 (95.1) | 84 (85.7) | ||
| Dyserythropoiesis., n (%) | 57/58 (98.3) | 85/87 (97.7) | 1.000 | |
| Dysgranulopoiesis, n (%) | 32/58 (55.2) | 55/83 (66.3) | 0.182 | |
| Dysmegakaryopoiesis, n (%) | 23/58 (39.7) | 44/85 (51.8) | 0.154 | |
|
CPSS
n (%) |
Low | 29 (47.5) | – | – |
| Intermediate-1 | 26 (42.6) | |||
| Intermediate-2 | 6 (9.8) | |||
| High | 0 | |||
|
IPSS-R
n (%) |
Very Low | 28 (45.9) | 40 (40.8) | 0.347 |
| Low | 24 (39.3) | 49 (50) | ||
| Intermediate | 8 (13.1) | 9 (9.2) | ||
| High | 1 (1.6) | 0 | ||
| Very high | 0 | 0 | ||
|
Risk (IPSS-R)
n (%) |
Low | 58 (95.1) | 92 (93.9) | 1.000 |
| High | 3 (4.9) | 6 (6.1) | ||
CMML, chronic myelomonocytic leukemia; RS, ring sideroblasts; MDS, myelodysplastic syndrome; CPSS, CMML-Prognostic Score System; IPSS-R, Revised International Prognostic Score System.Significant differences are highlighted in bold.
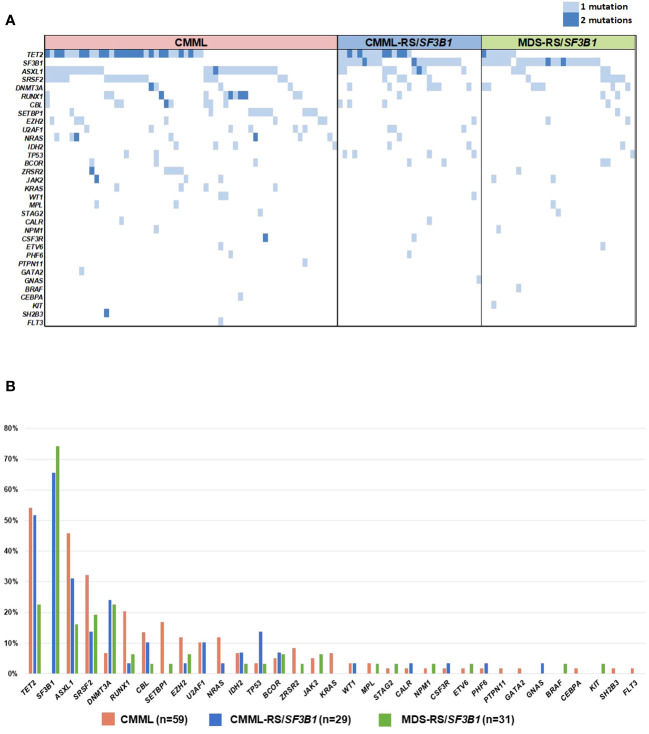
Data from NGS was available in 29, 61 and 32 patients with CMML-RS/SF3B1, CMML and MDS-RS/SF3B1, respectively. The molecular profiles of the three groups (CMML, CMML-RS/SF3B1 and MDS-RS/SF3B1), as well as the percentage of mutations, can be seen in Figures 1A, B . Briefly, the most frequent mutations were TET2 (mostly multi-hit), ASXL1 and SRSF2 in CMML, TET2 (mostly multi-hit), SF3B1 and ASXL1 in CMML-RS/SF3B1, and SF3B1, DNMT3A and TET2 in MDS-RS/SF3B1. As expected, other splicing mutations (SRSF2, U2AF1, ZRSR2) were exceptionally found ( Figures 1A, B ) in SF3B1 mutated patients.
Figure 1.
(A) Molecular profile of the three groups of patients. (B) Frequency of gene mutations in the three groups of patients.
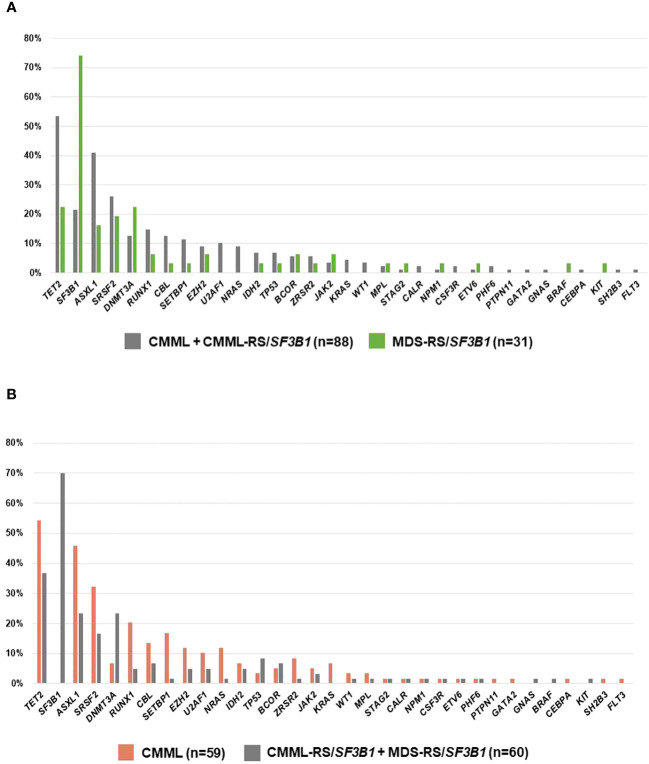
Then, we compared the molecular landscape across groups defined by phenotype. On one hand, when we compared MDS-RS/SF3B1 vs. CMML (CMML+CMML-RS/SF3B1), the latter showed a significantly higher frequency of mutations in TET2 (p=0.003), mostly multi-hit, and in ASXL1 (p=0.013), and fewer in SF3B1 (p<0.001) ( Figure 2A ). On the other hand, when we compared CMML vs. RS/SF3B1 patients (CMML-RS/SF3B1 + MDS-RS/SF3B1), CMML was enriched in mutations in TET2 (p=0, 054), ASXL1 (p=0.010), SRSF2 (p=0.048), RUNX1 (p=0.011), SETBP1 (p=0.004) and NRAS (p=0.026) but lacked mutations in DNMT3A (p=0.012) and, obviously (by definition), SF3B1 ( Figure 2B ). In addition, the CMML-RS/SF3B1 group was also compared individually with CMML and MDS-RS/SF3B1 ( Table 3 ).
Figure 2.
(A) Frequency of gene mutations in CMML (with and without ring sideroblasts (RS)/SF3B1) vs. MDS-RS/SF3B1. (B) Frequency of mutations in CMML vs. the two groups with ring sideroblasts (RS)/SF3B1.
Table 3.
Comparison of similar studies performed in patients with MDS or MDS/MPN and the present series.
| MANGAONKAR13 | WUDHIKARN12 | XICOY/Present series | ||||
|---|---|---|---|---|---|---|
| n=778 | n=859 | n=815 | ||||
| SF3B1 MUTMDS/MPNvs | CMMLSF3B1MUTvs | CMML with RS/SF3B1 vs | ||||
| SF3B1 WTMDS/MPN | SF3B1 mut MDS | CMML SF3B1 WT | SF3B1 MUT MDS-RS | CMML without RS/SF3B1 | MDS with RS/SF3B1 | |
| CLINICAL DIFFERENCES | Hemoglobin | |||||
| Platelet | ||||||
| Sex | WBC | |||||
| Hemoglobin | Hemoglobin | AMC and % | ||||
| WBC | Sex | WBC | Leukocyte | ANC | Age | |
| ANC | WBC ANO | ANC | Monocyte count Platelet count | PB blasts | Gender | |
| AMC | AMC | AMC | IMCs | BM blasts | WBC | |
| Platelet | Platelet | Platelet count | PB blasts | FAB subtype | AMC and% | |
| BM RS | PE blats | RS | BM blasts | Dysplastic lines | IPSS-R | |
| PB blats | BM blasts | FAB subtype | RS (median, %) | |||
| BM blasts | Cytogenetic risk | Dyserythropoieseis | ||||
| Abnormal karyotype | Dysgranulopiesis | |||||
| CPSS | ||||||
| IPSS-R (low/High) | ||||||
| MOLECULAR DIFFERENCES | - |
JAK2 V617F
(enriched in SF3B1 MUT MDS/MPN) |
ASXL1 and SRSF2
(enriched in CMML SF3B1 WT |
RUNX1
(enriched in CMML SF3B1WT) |
DNMT3A, SF3B1
(enriched in CMML-RS/SF3B1 RUNX1, SETBP1 (enriched in CMML without RS/SF3B1 |
TET2 (enriched in CMML-RS/SF3B1) |
| AML-T | Lower | NS | Lower | Higher | Lower | NS |
| os | Higher | NS | NS (trend) | NS (trend) | Higher | NS |
MDS/MPN, myelodysplastic syndrome/myeloproliferative neoplasm; CMML, chronic myelomonocytic leukemia; MDS, Myelodysplastic syndrome; RS, ring sideroblasts; WBC, leukocyte count; ANC, absolute neutrophil count; AMC, absolute monocyte count; BM, bone marrow; RS, ring sideroblasts; PB, peripheral blood; FAB, French-American-British; IMC, immature myeloid cells; CPSS, CMML-Prognostic Score System; IPSS-R, Revised International Prognostic Score; AML-T, acute myeloid leukemia transformation; OS, overall survival.
The median follow-up for alive patients in the whole series was 3.25 (0.26-33.66) years: 2.96 (0.35-17.9) for CMML-RS/SF3B1, 2.51 (0.33-25.1) for CMML and 3.96 (0.26-33.66) for MDS-RS/SF3B1. The median OS was 6.38 years (95%CI 5.2-7.49). Differences in OS among the three groups were statistically significant: 6.75 years (95% CI 5.41-8.09) for CMML-RS/SF3B1 vs. 3.17 years (95% CI 2.56-3.79) for CMML vs. 16.47 years (NA) for MDS-RS/SF3B1, p<0.001 ( Figure 3A ). When comparing OS between CMML-RS/SF3B1 and both CMML and MDS-RS/SF3B1, the differences remained significant (p<0.001 and p=0.008). Regarding patients with SF3B1 mutation, the survival was not significantly different. At 8 years, the OS was 57% (95%CI 30%-84%) in CMML with SF3B1 mutation and 71% (95%CI 56%-86%) in MDS with SF3B1 mutation ( Figure 3B ).
Figure 3.
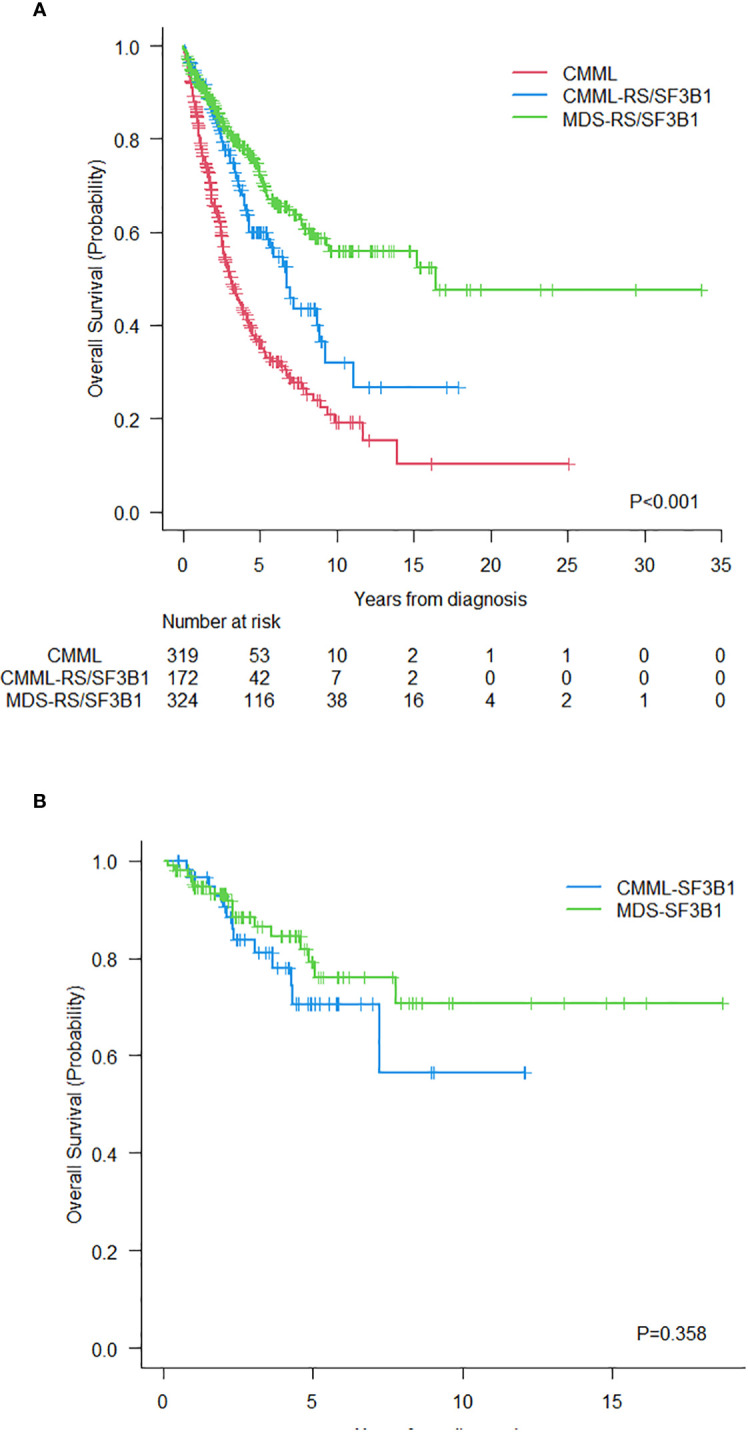
(A) Overall survival of the three groups of patients. (B) Overall survival of patients with CMML and MDS with SF3B1 mutation.
The 8-year CIP to AML transformation (95%CI) in the 3 groups (CMML-RS/SF3B1, CMML and MDS-RS/SF3B1) was: 12% (6%-19%), 24% (19%-30%) and 10% (7%-15%), respectively. This outcome did not significantly differ between the groups with SF3B1 mutation: for CMML-SF3B1 14% (1%-43%) and for MDS-SF3B1 9% (2%-24%) (p=0.929) ( Figures 4A, B ).
Figure 4.
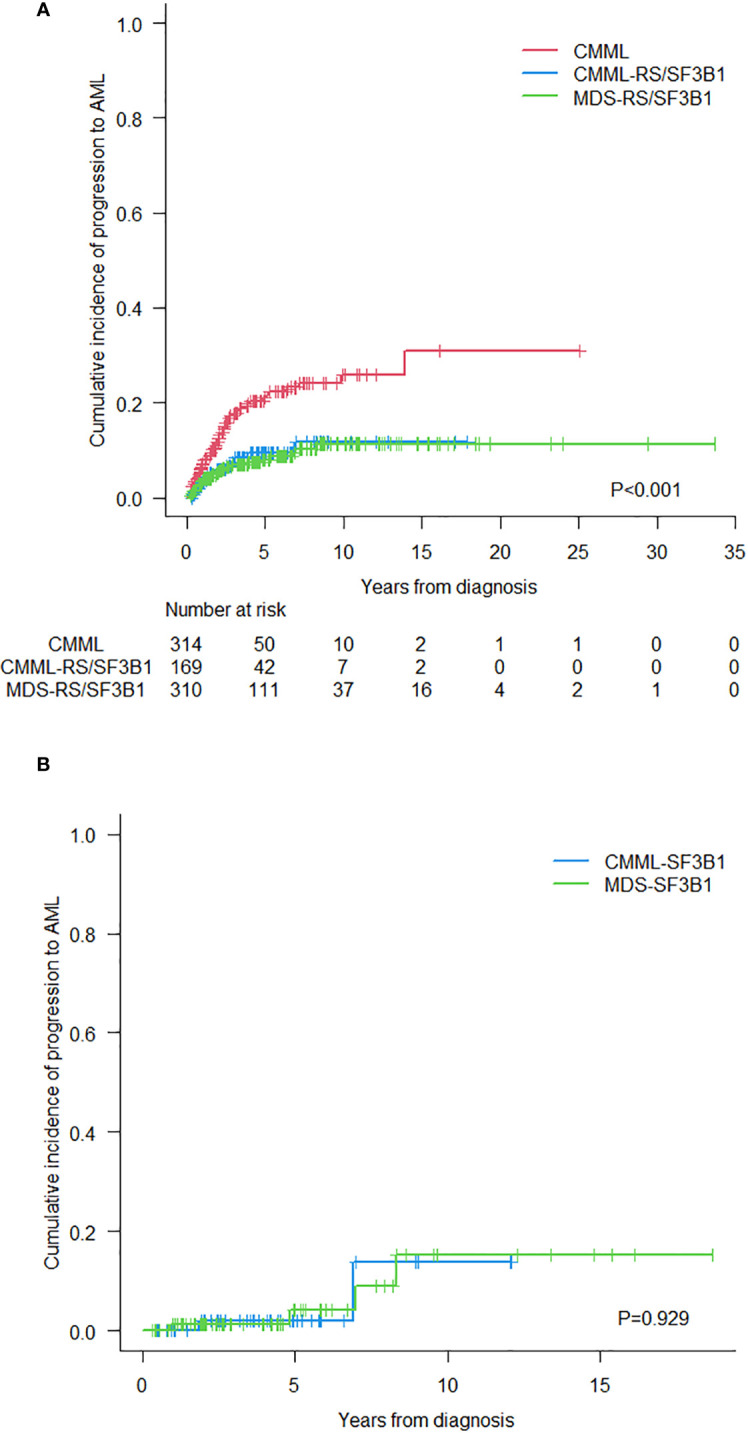
(A) Cumulative incidence of progression to acute myeloid leukemia in the three groups of patients. (B) Cumulative incidence of progression to acute myeloid leukemia in CMML and MDS with SF3B1 mutation.
Finally, we focused on the group of MDS-RS/SF3B1 looking for a possible influence of absolute monocyte count in peripheral blood on outcomes. There was no correlation between the percentage of RS and monocyte count (p=0.120 but we observed that the greater the number of monocytes (<0.2, 0.3-0.4 and ≥0.5), the worse the survival (8-year OS, 95% CI: 78% (63%-87%) vs. 60% (50%-69%), vs. 41% (22%-58%), p=0.010) ( Supplementary Figure 1A ). Within the group with SF3B1 mutation, a better OS was observed in the presence of a very low monocyte count (<0.2 vs. ≥0.2) (8-yr OS 89% (43%-98%) vs. 69% (50%-82%), p=0.088) ( Supplementary Figure 1B ).
Discussion
CMML was first described by the FAB group in 1976 as a chronic disease in which the monocyte count was higher than 1 x109/L and the monocytes often showed atypical morphological features (16). The presence of RS was initially reported as a frequent feature of MDS (at that time called sideroblastic anemia) in the 1982 FAB classification (17). Approximately 30%-35% of MDS patients present with RS, erythroblasts in the bone marrow with at least five iron granules that cover one-third or more of the perinuclear region, corresponding to mitochondrial ferritin (18, 19). In FAB and previous WHO classification systems for myeloid neoplasms, cases presenting with both an absolute and relative monocyte count in peripheral blood > 1×109/L and ≥10% of the leukocyte count were considered as CMML regardless of other morphological findings, such as the presence of RS in the bone marrow. However, the greater preeminence given to the monocyte count in peripheral blood over the proportion of RS in the bone marrow was not evidence-based.
Molecular techniques, and especially NGS, have improved the knowledge of the biology of most myeloid neoplasms. It is well known that more than 90% of patients with CMML have somatic mutations, with splicing factor mutations such as SRSF2, U2AF1, ZRSR2 and SF3B1 being highly prevalent, especially SRSF2 (20–24). Because SRSF2 has not been detected in the healthy elderly population (unlike TET2 and ASXL1) and although this mutation is not specific of this disease, it is useful as a clonal marker in the differential diagnosis of other causes of monocytosis (25). Moreover, co-occurrence of mutations in SRSF2 and TET2, and the presence of multiple TET2 mutations, are considered hallmarks of CMML (21, 22, 26). In MDS, SF3B1 mutations are present in 80% of patients with MDS with RS (90% of MDS-RS-UD and in 70% MDS-RS-MD based on the 2017 WHO classification)10. According to the 2017 WHO classification, its presence allows the diagnosis of MDS with RS when the percentage of RS ranges between 5%-14%, whereas its detection can be ignored when this proportion is greater than or equal to 15%. This subtype of MDS is characterized by a good prognosis in terms of OS and CIP to AML and by responses to Luspatercept (6–8). More recently, SF3B1 mutation was incorporated as a defining genetic feature, named MDS with low blasts and SF3B1 mutation by the 2022 WHO classification, and MDS with mutated SF3B1 by the ICC of the same year (2, 3). In patients with CMML, mutations in SF3B1 have also been associated with lower hemoglobin levels with no impact in prognosis (9, 21).
The Spanish Group of MDS suggested that the proportion of RS in bone marrow could be a much more powerful prognostic indicator than the absolute monocyte count in peripheral blood in CMML (27). Two recent studies have addressed this issue focusing on the role of SF3B1 mutation in the phenotype and clinical course of MDS/MPN neoplasms. The study by Wudhikam et al. compared CMML-SF3B1MUT to CMML-SF3B1 WT and MDS-SF3B1 MUT, while Mangaonkar et al. focused on the distinction between MDS/MPN-SF3B1MUT , its wild-type counterparts, and the group of MDS-SF3B1MUT (12, 13). In both studies, the CMML phenotype was closer to that of MDS as long as they shared the SF3B1 mutation. Moreover, no significant differences were found in terms of OS and the transformation to AML between MDS/MPN-SF3B1 MUT and MDS-SF3B1MUT in the study by Mangaonkar et al., whereas only leukemia-free survival of CMML-SF3B1MUT was poorer than that of MDS-SF3B1 MUT in the series of Wudhikarn et al. ( Table 3 ) (12, 13).
Unlike the study of Wudhikarn et al., we adopted the 2022 WHO classification in our series and, accordingly, patients with a monocyte count between 0.5 and 0.9 x109/L and ≥10% were considered as CMML (with or without RS/SF3B1) (12). Indeed, the majority of CMML-RS/SF3B1 patients in our series fulfilled this criterion (the so-called oligomonocytic CMML) and in the past, these patients would have been classified as MDS or MDS/MPN-U following the criteria of previous WHO classifications (28). In other words, the presence of RS or SF3B1 mutation in CMML is associated with a low absolute monocyte count in peripheral blood and, based on our findings, only the relative monocyte count allocates a patient into the CMML category. Several studies have suggested that oligomonocytic CMML shares many characteristics with classical CMML and may be considered as an early stage with better prognosis (28–32).
Regarding other clinical features, we observed that when RS are predominant and regardless of the presence of SF3B1 mutation, CMML and MDS patients share the main clinical characteristics, supporting the hypothesis that RS play a greater role than the monocyte count in determining the phenotype, which is closer to MDS than CMML. In line with these findings, the molecular landscape of CMML-RS/SF3B1 was closer to that of MDS-RS/SF3B1 than to CMML (without RS/SF3B1), being enriched in DNMT3A mutations, and with a lower frequency of mutations in SRSF2, RUNX1 and SETBP1 ( Table 3 ). Furthermore, when we grouped together and compared patients according to their main defining morphological findings (monocytosis or RS/SF3B1, Figures 2A, B ), the most notable differences were observed between CMML and patients with RS/SF3B1 (both MDS and CMML). Even though numbers of patients with available NGS in the three series are small, it is of some interest the observation that TP53 mutation- – which is generally reported in <5% of CMML patients-, is in the 13%-14% range in CMML-RS/SF3B1 (possibly due to some cases of CMML-RS with unknown SF3B1 status) ( Figures 1A, B ).
Nevertheless, the OS of CMML-RS/SF3B1 was not as good as MDS-RS/SF3B1 and this finding cannot be attributed to a higher CIP to AML. Patients with CMML-RS/SF3B1 were older, and this is usually associated with the presence of more comorbidities, but the causes of death different from AML transformation did not apparently differ (data not shown). Based on our results and published data, a prospective study is required to better clarify the impact of RS/SF3B1 on OS and AML transformation (12, 13). The frequency of poor prognosis mutations, as defined in CPSS molecular scoring system, such as ASXL1, SETBP1, RUNX1 and NRAS, was higher in CMML than in CMML-RS/SF3B1, which may explain the poorer prognosis of the former group. In contrast, the presence of multi-hit mutations in TET2 was similar in CMML cases (with and without RS/SF3B1) and more frequent than in the MDS-RS/SF3B1 group, which explains the higher monocyte count that characterizes CMML, while cases with RS/SF3B1 (CMML or MDS) frequently showed co-mutations in DNMT3A, as previously described (29, 33). Unfortunately, molecular data were insufficient to evaluate whether mutations defined in the IPSS-M as having poor prognosis in patients with MDS-SF3B1 have the same impact in cases with CMML-SF3B1 (34).
In our cohort of MDS-RS/SF3B1 mutation the absolute monocyte count in peripheral blood negatively influenced OS. These data are in line with those of Kasprzak et al. and Silzle et al., which, in a population of MDS with low blast count, have recently shown that monocytosis >0.6 x109/L is associated with a shorter OS, also in the subtype enriched with RS. This suggests that MDS with monocytosis and CMML with RS may be located in a “gray zone” that makes diagnosis challenging but, on the other hand, supports a therapeutically similar approach in these cases (14, 15). Altogether, this study supports the notion that classifications based on selected clinical characteristics, generally with arbitrarily chosen thresholds, have always inherent limitations. The results of this study raise the question whether patients with CMML-RS/SF3B1 and monocytosis <1.0 x109/L should be properly classified as CMML or should be rather classified as MDS with RS/SF3B1 mutation and relative monocytosis similar to what we observe in myelofibrosis when it presents with monocytosis (35). Furthermore, for patients with absolute monocyte count in the range 0.5-0.9 x 109/L to distinguish the entities MDS-RS/SF3B1 or CMML-RS/SF3B1 on the base of relative monocytosis (i.e. <10% vs ≥10%) is biologically irrational. Some studies have shown that oligomonocytic CMML patients resemble CMML mainly for their immunophenotypic and genomic features, and thus, absolute monocyte count has been lowered from 1 to 0.5 x109/L in the 2022 WHO/ICC classifications, provided that an acquired cytogenetic or molecular clonality is found. The results reported in this manuscript, however, indicate that in such subset of patients, the diagnostic criteria should at least include the exclusion of patients with RS/SF3B1.
This is a registry-based study and, therefore, includes retrospective data and has its inherent limitations; First, we cannot rule out a selection bias in the inclusion of patients, especially with the CMML-RS/SF3B1 phenotype and thus, we could not determine the real prevalence of this subtype of CMML; Second, a centralized diagnosis was missing and we were not able to exhaustively revise causes of death; third, the use of Sanger and NGS, with different sensitivity for analyzing SF3B1, may bias the results; Finally, the availability of a complete molecular profile was restricted to a few patients and also, the type of variants and variant allele frequency were missing in some patients, limiting the evaluation of the influence of existing mutations on the phenotype and evolution of the cases.
In conclusion, CMML harboring RS/SF3B1 mutation resembles MDS-RS/SF3B1 in terms of phenotype and prognosis and clearly differs from classical CMML. The presence of ≥15% RS and/or SF3B1 mutation in CMML is associated with a low monocyte count and SF3B1 mutation clearly improves the prognosis of CMML.
Data availability statement
This study has been carried out collecting data from different registries. Requests to access these datasets should be directed to BX, bxicoy@iconcologia.net.
Ethics statement
The studies involving humans were approved by Comitè d’etica d’Investigació de l’Hospital Universitari Germans Trias i Pujol. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BX: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. HP: Writing – review & editing, Data curation. MM: Writing – review & editing, Methodology, Formal analysis. UG: Writing – review & editing, Data curation. MA: Writing – review & editing, Data curation. MT: Writing – review & editing, Data curation. LP: Writing – review & editing, Data curation. EO: Writing – review & editing, Data curation. MD: Writing – review & editing, Data curation. FS: Writing – review & editing, Data curation. MD-B: Writing – review & editing, Data curation. AE: Writing – review & editing, Data curation. AM: Writing – review & editing, Data curation. LL: Writing – review & editing, Data curation. AA: Writing – review & editing, Data curation. MU: Writing – review & editing, Data curation. AP: Writing – review & editing, Data curation. VR: Writing – review & editing, Data curation. FH: Writing – review & editing, Data curation. MD-C: Writing – review & editing, Data curation. LZ: Writing – review & editing, Data curation.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1385987/full#supplementary-material
(A) Overall survival of patients with MDS-RS/SF3B1 mutation according to monocyte count. (B) Overall survival of patients with MDS-SF3B1 mutation according to monocyte count.
References
- 1. Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. (2016) 127:2391–405. doi: 10.1182/blood-2016-03-643544 [DOI] [PubMed] [Google Scholar]
- 2. Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data. Blood. (2022) 140:1200–28. doi: 10.1182/blood.2022015850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the world health organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. (2022) 36:1703–19. doi: 10.1038/s41375-022-01613-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fenaux P, Santini V, Aloe Spiriti MA, Giagounidis A, Schlag R, Radinoff A, et al. A phase 3 randomized, placebo-controlled study assessing the efficacy and safety of epoetin-α in anemic patients with low-risk MDS. Leukemia. (2018) 32:2648–58. doi: 10.1038/s41375-018-0118-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xicoy B, Germing U, Jimenez MJ, Garcia O, Garcia R, Schemenau J, et al. Response to erythropoietic-stimulating agents in patients with chronic myelomonocytic leukemia. Eur J Haematol. (2016) 97:33–8. doi: 10.1111/ejh.12679 [DOI] [PubMed] [Google Scholar]
- 6. Platzbecker U, Germing U, Gotze KS, Kiewe P, Mayer K, Chromik J, et al. Luspatercept for the treatment of anaemia in patients with lower-risk myelodysplastic syndromes ¨ (PACE-MDS): a multicentre, open-label phase 2 dose-finding study with long-term extension study. Lancet Oncol. (2017) 18:1338–47. doi: 10.1016/S1470-2045(17)30615-0 [DOI] [PubMed] [Google Scholar]
- 7. Fenaux P, Platzbecker U, Mufti GJ, Garcia-Manero G, Buckstein R, Santini V, et al. Luspatercept in patients with lower-risk myelodysplastic syndromes. N Engl J Med. (2020) 382:140–51. doi: 10.1056/NEJMoa1908892 [DOI] [PubMed] [Google Scholar]
- 8. Platzbecker U, Della Porta MG, Santini V, Zeidan AM, Komroji RS, Shortt J, et al. Efficacy and safety of luspatercept versus epoetin alfa in erythropoiesis-stimulating agent-naive, transfusion-dependent, lower-risk myelodysplastic syndromes (COMMANDS): interim analysis of a phase 3, open-label, randomised controlled trial. Lancet. (2023) 402:373–85. doi: 10.1016/S0140-6736(23)00874-7 [DOI] [PubMed] [Google Scholar]
- 9. Patnaik MM, Lasho TL, Finke CM, Hanson CA, Hodnefield JM, Knudson RA, et al. Spliceosome mutations involving SRSF2, SF3B1, and U2AF35 in chronic myelomonocytic leukemia: prevalence, clinical correlates, and prognostic relevance. Am J Hematol. (2013) 88:201–6. doi: 10.1002/ajh.23373 [DOI] [PubMed] [Google Scholar]
- 10. Malcovati L, Karimi M, Papaemmanuil E, Ambaglio I, Järdesten I, Jansson M, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. (2015) 126:233–41. doi: 10.1182/blood-2015-03-633537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Malcovati L, Stevenson K, Papaemmanuil E, Neuberg D, Bejar R, Boultwood J, et al. SF3B1-mutant MDS as a distinct disease subtype: a proposal from the International Working Group for the Prognosis of MDS. Blood. (2020) 136:157–70. doi: 10.1182/blood.2020004850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wudhikarn K, Loghavi S, Mangaonkar AA, Al-Kali A, Binder M, Carr R, et al. SF3B1-mutant CMML defines a predominantly dysplastic CMML subtype with a superior acute leukemia-free survival. Blood Adv. (2020) 4:5716–21. doi: 10.1182/bloodadvances.2020003345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mangaonkar AA, Lasho TL, Finke C, Al-Kali A, Binder M, Carr B, et al. SF3B1-mutant myelodysplastic syndrome/myeloproliferative neoplasms: a unique molecular and prognostic entity. Haematologica. (2022) 107:1189–92. doi: 10.3324/haematol.2021.280463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kasprzak A, Assadi C, Nachtkamp K, Rudelius M, Hass R, Giagunidis A, et al. Monocytosis at the time of diagnosis has a negative prognostic impact in myelodysplastic syndromes with less than 5% bone marrow blasts. Ann Hematol. (2023) 102:99–106. doi: 10.1007/s00277-022-05043-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Silzle T, Blum S, Kasprzak A, Nachtkamp K, Rudelius M, Hildebrandt B, et al. The absolute monocyte count at diagnosis affects prognosis in myelodysplastic syndromes independently of the IPSS-R risk score. Cancers (Basel). (2023) 15:3572. doi: 10.3390/cancers15143572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol. (1976) 33:451–8. doi: 10.1111/j.1365-2141.1976.tb03563.x [DOI] [PubMed] [Google Scholar]
- 17. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. (1982) 51:189–99. doi: 10.1111/j.1365-2141.1982.tb08475.x [DOI] [PubMed] [Google Scholar]
- 18. Mufti GJ, Bennett JM, Goasguen J, Bain BJ, Baumann I, Brunning R, et al. Diagnosis and classification of myelodysplastic syndrome: International Working Group on Morphology of Myelodysplastic Syndrome (IWG-MDS) consensus proposals for the definition and enumeration of myeloblasts and ring sideroblasts. Haematologica. (2008) 93:1712–7. doi: 10.3324/haematol.13405 [DOI] [PubMed] [Google Scholar]
- 19. Juneja SK, Imbert M, Sigaux F, Jouault H, Sultan C. Prevalence and distribution of ringed sideroblasts in primary myelodysplastic syndromes. J Clin Pathol. (1983) 36:566–9. doi: 10.1136/jcp.36.5.566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Meggendorfer M, Roller A, Haferlach T, Eder C, Dicker F, Grossmann V, et al. SRSF2 mutations in 275 cases with chronic myelomonocytic leukemia (CMML). Blood. (2012) 120:3080–8. doi: 10.1182/blood-2012-01-404863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M, et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oygncol. (2013) 31:2428–36. doi: 10.1200/JCO.2012.47.3314 [DOI] [PubMed] [Google Scholar]
- 22. Patnaik MM, Tefferi A. Chronic myelomonocytic leukemia: 2022 update on diagnosis, risk stratification, and management. Am J Hematol. (2022) 97:352–72. doi: 10.1002/ajh.2645 [DOI] [PubMed] [Google Scholar]
- 23. Bastie JN, Aucagne R, Droin N, Solary E, Delva L. Heterogeneity of molecular markers in chronic myelomonocytic leukemia: a disease associated with several gene alterations. Cell Mol Life Sci. (2012) 69:2853–61. doi: 10.1007/s00018-012-0956-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McCullough KB, Patnaik MM. Chronic myelomonocytic leukemia: a genetic and clinical update. Curr Hematol Malig Rep. (2015) 10:292–302. doi: 10.1007/s11899-015-0271-4 [DOI] [PubMed] [Google Scholar]
- 25. Steensma DP, Bejar R, Jaiswal S, Lindsley RC, Sekeres MA, Hasserjian RP, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. (2015) 126:9–16. doi: 10.1182/blood-2015-03-631747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Castaño-Díez S, Pomares H, Esteban D, Jimenez-Vicente C, Zugasti I, Álamo JR, et al. Characteristics and long-term outcome in a large series of chronic myelomonocytic leukaemia patients including 104 formerly referred to as oligomonocytic. Br J Haematol. (2014) 204:892–7. doi: 10.1111/bjh.19217 [DOI] [PubMed] [Google Scholar]
- 27. Such E, Senent L, Nomdedeu B, Bueno J, Bernal T, Carbonell F, et al. Chronic myelomonocytic leukemia (CMML) with more than 15% of ring sideroblasts in bone marrow: an overlapping disorder between CMML and refractory anemia with ring sideroblasts. Blood. (2009) 114:290. doi: 10.1182/blood.V114.22.290.290 19357397 [DOI] [Google Scholar]
- 28. Valent P. Oligo-monocytic CMML and other pre-CMML states: Clinical impact, prognostication and management. Best Pract Res Clin Haematol. (2020) 33:101137. doi: 10.1016/j.beha.2019.101137 [DOI] [PubMed] [Google Scholar]
- 29. Garcia-Gisbert N, Arenillas L, Roman-Bravo D, Rodriguez-seviulla JJ, Fernandez-Rodriguez C, Garcia-Avila S, Gibert J, et al. Multi-hit TET2 mutations as a differential molecular signature of oligomonocytic and overt chronic myelomonocytic leukemia. Leukemia. (2022) 36:2922–6. doi: 10.1038/s41375-022-01733-8 [DOI] [PubMed] [Google Scholar]
- 30. Calvo X, Roman-Bravo D, Garcia-Gisbert N, Rodriguez-Sevilla JJ, Garcia-Avila S, Florensa L, et al. Outcomes and molecular profile of oligomonocytic CMML support its consideration as the first stage in the CMML continuum. Blood Adv. (2022) 6:3921–31. doi: 10.1182/bloodadvances.2022007359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Montalban-Bravo G, Kanagal-Shamanna R, Guerra V, Ramos-Perez, Hammond D, Shilpa P, et al. Clinical outcomes and influence of mutation clonal dominance in oligomonocytic and classical chronic myelomonocytic leukemia. Am J Hematol. (2021) 96:E50–3. doi: 10.1002/ajh.26044 [DOI] [PubMed] [Google Scholar]
- 32. Schuler E, Frank F, Hildebrandt B, Betz B, Strupp C, Rudelius M, et al. Myelodysplastic syndromes without peripheral monocytosis but with evidence of marrow monocytosis share clinical and molecular characteristics with CMML. Leuk Res. (2018) 65:1–4. doi: 10.1016/j.leukres.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 33. Huber S, Haferlach T, Meggendorfer M, Hutter S, Hoermann G, Baer C, et al. SF3B1 mutated MDS: Blast count, genetic co-abnormalities and their impact on classification and prognosis. Leukemia. (2022) 36:2894–902. doi: 10.1038/s41375-022-01728-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bernard E, Tuechler H, Greenberg PL, Hasserjian RP, Arango Ossa JE, Nannya Y, et al. Molecular international prognostic scoring system for myelodysplastic syndromes. N Engl J Med. (2022) 1:EVIDoa2200008. doi: 10.1056/EVIDoa2200008 [DOI] [PubMed] [Google Scholar]
- 35. Chapman J, Geyer JT, Khanlari M, Moul A, Casas C, Connor ST, et al. Myeloid neoplasms with features intermediate between primary myelofibrosis and chronic myelomonocytic leukemia. Mod Patho. (2018) 31:429–41. doi: 10.1038/modpathol.2017.148 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Overall survival of patients with MDS-RS/SF3B1 mutation according to monocyte count. (B) Overall survival of patients with MDS-SF3B1 mutation according to monocyte count.
Data Availability Statement
This study has been carried out collecting data from different registries. Requests to access these datasets should be directed to BX, bxicoy@iconcologia.net.