Countries participating in the International Registry of Acute Aortic Dissection.
Central Message.
Thoracic aortic dissections are understudied in low- and lower-middle-income countries. Collaborative efforts such as the International Registry of Acute Aortic Dissection may change this reality.
The knowledge surrounding the global epidemiology of thoracic aortic disease is mostly confined to high-income countries, where thoracic aortic aneurysms (TAAs) have an incidence of at least 5.3 per 100,000 people per year and acute thoracic aortic dissections (ATADs) occur in approximately 3 to 4 cases per 100,000 person-years.1,2 The true prevalence of TAAs is likely underestimated because more than 90% of people who live with TAAs remain asymptomatic until dissection or rupture occurs, which may explain why epidemiological estimates of TAAs and ATADs are nearly comparable. Nevertheless, in high-income countries, thoracic aortic surgery already makes up a considerable share of total cardiac surgical volumes: in the United States, 8% of all cardiac surgery procedures involve the thoracic aorta.3 In low- and middle-income countries (LMICs), detailed epidemiological studies on TAAs and ATADs are lacking, although the overall cardiovascular and aortic disease burdens are increasing: The global morbidity and mortality due to any aortic pathology increased by 67.0% between 1990 and 2019, particularly among LMICs, which experienced an increase of up to 150.6%.4 These trends are driven by countries’ epidemiological transition away from communicable (infectious) diseases and toward noncommunicable diseases, with an overlapping transition period of a double burden. As life expectancy improves, rates of hypertension and resulting aortic pathology are expected to increase. Between 2000 and 2019, the healthy life expectancy in sub-Saharan Africa increased by 10 years, with overall life expectancy increasing even further, contributing to the rise in noncommunicable diseases and aortic pathology, especially in working-age adults.5 Unlike high-income countries, LMICs will continue to observe high rates of HIV/AIDS, syphilis, and tuberculosis for many years to come, each of which may contribute to aortic pathology in younger populations. Indeed, evidence suggests the age at ATAAD onset in LMICs is lower compared to high-income countries.6 Concurrently, traumatic injuries are an important cause of thoracic aortic injury, responsible for 2% to 3% of deaths from road traffic incidents.7 Despite possessing only 60% of the world’s vehicles, LMICs face more than 90% of deaths due to road traffic injuries worldwide.8 As a result of these unique challenges, an understanding of the thoracic aortic burden and management in LMICs is crucial to inform health care planning and reduce countries’ aortic morbidity and mortality.
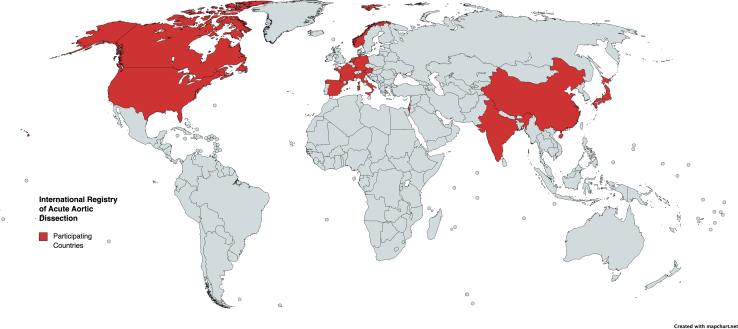
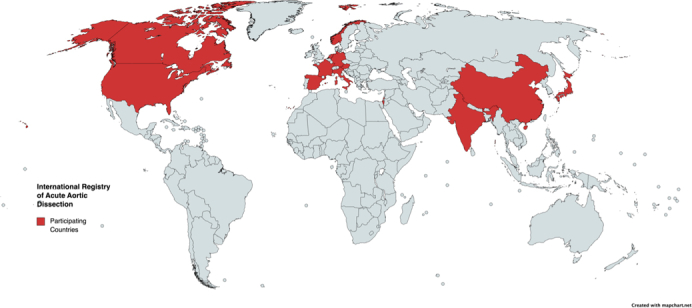
The International Registry of Acute Aortic Dissection (IRAD) is an international, multicenter effort focused on acute thoracic aortic dissections and recently celebrated its 25th anniversary. During these 25 years, 97 studies on acute aortic dissections were published.9 As such, IRAD has been foundational to informing the clinical and surgical management of ATADs, with findings informing guidelines and practice worldwide. IRAD’s growth and scientific contributions are commendable and provide an example for similar initiatives in other areas of cardiothoracic surgery; however, 1 crucial gap remains: IRAD represents 58 aortic surgery centers in 13 countries, of which 56 centers are based in high-income countries (Figure 1). Two centers are based in China and India, and are, respectively, among the world’s highest-volume centers and a private center, thereby not representing the realities of most centers and patients in LMICs.
Figure 1.
Countries participating in the International Registry of Acute Aortic Dissection.
In this article, we summarize access to cardiac surgery in LMICs with a focus on thoracic aortic surgery and briefly summarize the available evidence on scheduled and emergency surgical outcomes for thoracic aortic disease in variable-resource contexts. Herein, we define LMICs according to the World Bank’s Country and Lending Groups classification for the 2024 fiscal year as countries with a gross national income per capita ≤$13,845. We acknowledge that LMICs, home to 6.7 billion people, are heterogeneous in terms of their disease burdens, overall health care capacity, and sociocultural and political systems. Nevertheless, several key challenges, including insufficient cardiac surgical capacity, health coverage, and underrepresentation in cardiac surgical research, are shared, and illustrated through the example of thoracic aortic surgery delivery in Cameroon, an LMIC in sub-Saharan Africa. We conclude by highlighting opportunities to generate contextual evidence for management of thoracic aortic disease in LMICs through IRAD and beyond.
Access to Cardiac Surgery in LMICs
Access to safe, timely, and affordable cardiac surgical care in LMICs is poor because 6 billion people lack access when needed and more than 100 countries and territories do not have a single cardiac surgeon or cardiac surgical center.10,11 High-income countries rely on 7.15 cardiac surgeons and 2.18 cardiac surgery centers per million population; by contrast, low-income countries have only 0.04 cardiac surgeons and 0.04 centers per million people.11,12 Regionally, sub-Saharan Africa is disproportionately affected: the subcontinent has only 92 cardiac surgery centers to cater for more than 1 billion people. Whereas LMICs face a substantial mismatch between their cardiac surgical needs and capacity, various countries continue to show leadership in terms of surgical volumes (eg, the world’s largest centers are in China and India), procedural costs (eg, centers in India and Vietnam perform cardiac surgery at as little as $1500-$3000), training programs (eg, South Africa, Morocco, and Egypt train cardiac surgeons from across the sub-Saharan African subcontinent), and health coverage (eg, most Latin American countries have comprehensive health coverage, whereas Nepal has introduced a microinsurance scheme to enable children, elderly, and those in poverty to access cardiac surgery for free).13,14
The care provided by surgeons in LMICs is often focused on procedures that minimize resource utilization (eg, less complex congenital heart surgery) and length of stay (eg, need for postoperative intensive care), and are associated with favorable outcomes (eg, lower-risk procedures). This is the result of small overall health budgets and, especially, a lack of prioritization of and investment into cardiac surgical services.10 Indeed, communicable diseases make up more than half of all global health financing for less than one-third of deaths in LMICs; by contrast, noncommunicable diseases, which notably include cardiovascular disease, receive <2% of funds but account for 74% of all deaths.15,16 This discrepancy between disease burden and political and economic action is sustained by both a focus on smaller, population-level interventions providing potentially faster marginal health gains, despite not necessarily having greater cost-effectiveness, and prevailing myths surrounding care for complex conditions, such as cardiac surgical disease.17 As such, noncommunicable diseases are on the rise in LMICs without concurrent health systems strengthening efforts to manage this growing burden. Primordial, primary, and secondary preventive efforts are key to mitigate cardiovascular disease burdens, but cannot eradicate cardiovascular disease nor meet the needs of those already living with cardiac surgical disease. Scaling cardiac surgical services requires considerable time for training teams and setting up the necessary infrastructure; waiting to act will only cause greater health system gaps in the future.
Thoracic Aortic Surgery in LMICs
Reports from LMICs without local cardiac surgical capacity are rare but illustrate the dire situation with patients expiring or requiring costly and traumatizing travel abroad for a glimpse of hope of survival.18,19 In LMICs with local cardiac surgical capacity, thoracic aortic pathology is less frequently managed compared with high-income countries, whether as a result of no diagnosis (eg, death in the community or lack of imaging), no or delayed referral, limited emergency care and surgery capacity, and/or a lack of staffing or resources.20
Despite these challenges, select centers perform cardiac surgery for thoracic aortic pathology in both scheduled and emergency settings. Although outcomes differ, experienced but lower-volume centers are able to achieve favorable outcomes.20 For example, several publications from Cameroon illustrate the ability to perform scheduled and emergency thoracic aortic surgery in an LMIC influenced by political instability and conflict.20, 21, 22 There, the local cardiac-aortic surgeon (senior author of this manuscript: Dr Mvondo) was trained abroad and acquired further expertise through visiting team partnerships, now independently performing thoracic aortic procedures in Cameroon. Between 2010 and 2018, 28 patients were operated on for TAAs (N = 18 [64.3%]), ATADs (N = 9 [32.1%]), and a nonsyphilitc pseudoaneurysm (N = 1 [3.6%]).21 After surgery, the 30-day mortality was 10.7% (5.6% for TAAs; 22.2% for ATADs). More recent findings suggest that, despite delayed referrals and management of patients in the subacute or chronic phase, composite aortic root replacement for type A ATADs (n = 12) with 75% (n = 9) of patients undergoing concomitant aortic arch surgery had an operative mortality of 16.7%, thus comparing favorably to outcomes reported by IRAD.9,20 Lastly, aortic root enlargement with double (mitral and aortic) valve replacements (n = 25) have been successfully performed in young patients (mean age at surgery, 23.3 ± 12.9 years) with predominantly (96%) rheumatic heart disease; the 8% operative mortality rate was higher than that observed in nonrheumatic, high-income country series (<2%).22,23 Patients’ experiences and outcomes could be optimized even further if timely screening, diagnostics, and more experienced and trained professionals across the care continuum were available. Moreover, locoregional registries to track thoracic aortic surgical outcomes in the sub-Saharan subcontinent could provide further insight into the optimal management of local patients to inform quality improvement initiatives.
Data from centers in most LMICs, especially low- and lower-middle-income countries, are limited, resulting in the contemporary evidence and clinical guidelines being rooted in populations and high-resourced contexts from (mostly) high-income countries. By contrast, patients managed in LMICs are generally younger, have higher rates of uncontrolled hypertension, and poorer adherence to medical therapy compared with patients in high-income countries.23 Moreover, aortic consequences of endemic diseases, such as HIV/AIDS, syphilis, and tuberculosis, as well as genetic and biological differences require further study. As such, it is unclear whether existing guidelines may be directly applied in populations unrepresented in the evidence base.
It must also be acknowledged that the costs, risks, and needs of thoracic aortic surgery are considerable. In variable-resource contexts, where triage decisions have to be made amidst considerable cardiac surgical waiting lists, noncardiac surgical health agendas, and limited budgets, the decision to perform complex cardiac surgery is potentially contentious.24 From a purely utilitarian point of view, which seeks to maximize health benefits across the population for a given amount of a good (eg, health budget), thoracic aortic surgery may not be high on the list of priorities. Conversely, egalitarian and prioritarian views may suggest that those worst off should not be neglected and the rule of rescue comes at the forefront; indeed, conditions that are as life-threatening as thoracic aortic pathology would fall under such an umbrella. Regardless of the ethical lens taken, investments into thoracic aortic (and broader cardiac) surgical capacity do not need to come at the cost of other health priorities. LMICs’ spending on health care as part of their health budgets remains considerably below past commitments, whereas global health financing by foreign aid agencies and private organizations should be directed toward overall health systems instead of earmarked to individual disease silos that do not necessarily match local needs.12,15,24
The heterogeneous needs and models to establish cardiac centers fall outside the scope of this article but have been described elsewhere.10 Similarly, thoracic aortic programs in LMICs have different origins, ranging from their introduction through the aortic training of local cardiac surgeons (as observed in Cameroon) to twinning programs between centers.
Moving the Center of Thoracic Aortic Research Gravity
Evidence from and guidelines for managing populations in high-income countries cannot be assumed to translate directly to the distinct populations and contexts in LMICs, requiring a shift in thoracic aortic research paradigms. Beyond clinical challenges, underreporting of data from LMICs is partially the result of other time pressures and limited research capacity and funding on the ground, as well as the traditional barriers to academic collaborations and publishing.24 Addressing these hurdles will require proactive support and increased opportunities by existing initiatives to level the playing the field and more comprehensively inform our understanding of ATAD in different populations and regions of the world.
Participation in existing database efforts, such as IRAD, can shed light on the current thoracic aortic practices in LMICs. However, barriers to participation must be thoroughly assessed and addressed to avoid skewing of participation toward well-resourced centers that may not be representative of the realities of resources and patient presentations in most cardiac centers in LMICs. Barriers may include a lack of electronic health records, linguistic challenges for data entry, administrative and legal issues, and potential costs surrounding human resources, data infrastructure, or database participation. Addressing these barriers may involve efforts by overarching data infrastructures, organizations, or societies to waive or subsidize costs and provide logistical support to overcome any learning curve. In addition, translations of data input, information, and capacity-building should be provided to move away from an anglophone-dominated research field, which excludes a considerable part of LMICs where English is not frequently spoken (eg, Latin America and francophone African countries).
Research efforts may further be supported by clinical efforts to provide virtual continued medical education. In recent years, there has been a surge in online educational platforms and webinars in cardiac surgery, many of which are widely attended across the globe, including by health care professionals from LMICs.25 For congenital heart surgery, the International Quality Improvement Collaborative has provided a platform for participating congenital heart surgery centers and teams to not only contribute LMIC data to an international outcomes registry but also receive regular training for all team members through recurring webinars.26 Such an approach engages not merely surgeons but can also ensure research empowerment of all health care professionals engaged in thoracic aortic care and provides further opportunity for clinical team-based training. This may enable aortic team models to be more embedded across the globe and further optimize patient outcomes. In addition, in-person educational opportunities and scholarships, such as those supported by the Thoracic Surgery Foundation, as well as twinning programs between cardiac centers with a focus on thoracic aortic surgery should be further encouraged and supported to scale thoracic aortic surgical care in LMICs.
As thoracic aortic surgical efforts and research scale in LMICs, a focus on research equity will be paramount. Evidence from the global surgical literature suggests that authors from high-income countries are disproportionately in first and last authorship positions for research conducted in LMICs,27 suggesting potential power imbalances or a lack of sponsorship of local authors. Although this may be the result of limited research experience and training, LMIC authors should be supported in developing the research and writing skills necessary to lead their own research efforts.27 Such research capacity-building may be done in the context of international partnerships with support of high-income country experts, but should, akin to budding cardiac surgical centers, move toward south-south partnerships and, ultimately, full local ownership.
Additionally, professional societies play a leading role in raising awareness of the issue of thoracic aortic care in LMICs. For example, annual meetings are increasingly placing global cardiac surgery discussions on their agendas28; in the future, conference organizers may consider thoracic aortic disease as part of these sessions or at dedicated aortic meetings, where such topics remain undiscussed. Furthermore, existing societal efforts, such as the Cardiac Surgery Intersociety Alliance,29 can better recognize and integrate all aspects of the cardiac surgical care continuum to recognize the systems-wide issues influencing practice, including health policy, health care financing, supply chains, and lifelong care into the community.
Lastly, and perhaps most importantly, patients must remain at the center of any global cardiac surgical effort. Among patients with thoracic aortic disease, proper informed consent and shared decision-making practices are essential and must be tailored to patients’ and families’ level of health literacy. In addition, because follow-up after thoracic aortic care is challenging even in high-income countries, telemedicine modalities must be explored. In LMICs, there is a wide availability of smartphones in part due to their use for a variety of purposes, including education and mobile payments; as such, mobile health and telemedicine in LMICs have been successful for a range of cardiovascular prevention and care purposes.30
Conclusions
The efforts of IRAD in the past 25 years are remarkable and have contributed to many lives saved around the world. Geographically expanding IRAD’s efforts to underrepresented countries and populations in the next 25 years can help dissect the realities facing the majority of the world’s population and exponentially increase the influence of IRAD through both clinical evidence and academic and clinical capacity-building.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Dr Vervoort is supported by the Canadian Institutes of Health Research Vanier Canada Graduate Scholarship. Dr Ouzounian is partially supported by the Munk Chair in Advanced Therapeutics and the Antonio & Helga De Gasperis Chair in Clinical Trials and Outcomes Research.
References
- 1.LeMaire S.A., Russell L. Epidemiology of thoracic aortic dissection. Nat Rev Cardiol. 2011;8(2):103–113. doi: 10.1038/nrcardio.2010.187. [DOI] [PubMed] [Google Scholar]
- 2.Gouveia E Melo R., Silva Duarte G., Lopes A., et al. Incidence and prevalence of thoracic aortic aneurysms: a systematic review and meta-analysis of population-based studies. Semin Thorac Cardiovasc Surg. 2022;34(1):1–16. doi: 10.1053/j.semtcvs.2021.02.029. [DOI] [PubMed] [Google Scholar]
- 3.Kim K.M., Arghami A., Habib R., et al. The Society of Thoracic Surgeons Adult Cardiac Surgery database: 2022 update on outcomes and research. Ann Thorac Surg. 2023;115(3):566–574. doi: 10.1016/j.athoracsur.2022.12.033. [DOI] [PubMed] [Google Scholar]
- 4.Wang Z., You Y., Yin Z., et al. Burden of aortic aneurysm and its attributable risk factors from 1990 to 2019: an analysis of the Global Burden of Disease Study 2019. Front Cardiovasc Med. 2022;9 doi: 10.3389/fcvm.2022.901225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Healthy life expectancy in Africa rises by almost 10 years. WHO Regional Office for Africa. https://www.afro.who.int/news/healthy-life-expectancy-africa-rises-almost-ten-years
- 6.Krishna Moorthy P.S., Sakijan A.S., Permal D., Gaaffar I.F., Kepli A.S., Sahimi H.I. Current review of acute type A aortic dissection in Malaysia. Indian J Thorac Cardiovasc Surg. 2023;39(S2):297–307. doi: 10.1007/s12055-023-01608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sznol J.A., Koru-Sengul T., Graygo J., Murakhovsky D., Bahouth G., Schulman C.I. Etiology of fatal thoracic aortic injuries: secondary data analysis. Traffic Inj Prev. 2016;17(2):209–216. doi: 10.1080/15389588.2015.1067805. [DOI] [PubMed] [Google Scholar]
- 8.Tavakkoli M., Torkashvand-Khah Z., Fink G., et al. Evidence from the decade of action for road safety: a systematic review of the effectiveness of interventions in low and middle-income countries. Public Health Rev. 2022;43 doi: 10.3389/phrs.2022.1604499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trimarchi S., Mandigers T.J., Bissacco D., et al. Twenty-five years of observations from the International Registry of Acute Aortic Dissection (IRAD) and its impact on the cardiovascular scientific community. J Thorac Cardiovasc Surg. July 13, 2023 doi: 10.1016/j.jtcvs.2023.06.021. [DOI] [PubMed] [Google Scholar]
- 10.Vervoort D., Lee G., Lin Y., et al. 6 Billion people have no access to safe, timely, and affordable cardiac surgical care. JACC Adv. 2022;1(3):1–5. doi: 10.1016/j.jacadv.2022.100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vervoort D., Meuris B., Meyns B., Verbrugghe P. Global cardiac surgery: access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 2020;159(3):987–996.e6. doi: 10.1016/j.jtcvs.2019.04.039. [DOI] [PubMed] [Google Scholar]
- 12.Vervoort D., Babar M.S., Sabatino M.E., et al. Global access to cardiac surgery centers: distribution, disparities, and targets. World J Surg. 2023;47(1):2909–2916. doi: 10.1007/s00268-023-07130-1. [DOI] [PubMed] [Google Scholar]
- 13.Vervoort D., Swain J.D., Pezzella A.T., Kpodonu J. Cardiac surgery in low- and middle-income countries: a state-of-the-art review. Ann Thorac Surg. 2021;111(4):1394–1400. doi: 10.1016/j.athoracsur.2020.05.181. [DOI] [PubMed] [Google Scholar]
- 14.Vervoort D., Premkumar A., Ghandour H., Kpodonu J. Health system needs to establish cardiac surgery centers. Thorac Cardiovasc Surg. 2021;69(8):729–732. doi: 10.1055/s-0040-1721395. [DOI] [PubMed] [Google Scholar]
- 15.Chang A.Y., Cowling K., Micah A.E., et al. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet. 2019;393(10187):2233–2260. doi: 10.1016/S0140-6736(19)30841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization Noncommunicable diseases. 2022. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 17.Vervoort D. The neglected component of cardiovascular care: dispelling the myths. Glob Heart. 2019;14(3):281–283. doi: 10.1016/j.gheart.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Landa K., Ellenga Mbolla B.F., Mongo-Ngamami S.F., et al. Aortic dissection in sub Saharan Africa: difficulty of management in a country without cardiac surgery. Clinical case in Congo-Brazzaville. Rwanda Med J. 2017;74(3):14–16. [Google Scholar]
- 19.Swift C.P., Ekyinabah E., Graglia S., Adeiza M.A. “Never say never”: the first successful management of a type A aortic dissection in Liberia. BMJ Case Rep. 2019;12(1) doi: 10.1136/bcr-2018-227511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mvondo C.M., Yon L.C.N., Kengni H.N.T., Ngowe M.N. Composite aortic root replacement in African patients with type A aortic dissection: report of 12 cases. Pan Afr Med J. 2023;45:18. doi: 10.11604/pamj.2023.45.18.37147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mvondo C.M., Ngatchou W., Kengni H.N.T., Ngowe M.N. Surgical repair of thoracic aortic aneurysm and dissection in the Sub-Saharan Africa: 30-day outcomes from a Cameroonian Center. African Ann Thorac Cardiovasc Surg. 2021;13(1):1–6. [Google Scholar]
- 22.Mve Mvondo C., Djientcheu C., Ngo Yon L.C., et al. Aortic root enlargement in patients undergoing mitral and aortic replacement: early outcomes in a sub-Saharan population. Front Cardiovasc Med. 2023;10 doi: 10.3389/fcvm.2023.1239032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocha R.V., Manlhiot C., Feindel C.M., et al. Surgical enlargement of the aortic root does not increase the operative risk of aortic valve replacement. Circulation. 2018;137(15):1585–1594. doi: 10.1161/CIRCULATIONAHA.117.030525. [DOI] [PubMed] [Google Scholar]
- 24.Vervoort D., Fenton K.N. Cardiac surgery in variable-resource contexts: overly ambitious or long overdue? Ann Thorac Surg. 2023;116(3):445–449. doi: 10.1016/j.athoracsur.2023.03.019. [DOI] [PubMed] [Google Scholar]
- 25.Vervoort D., Dearani J.A., Starnes V.A., Thourani V.H., Nguyen T.C. Brave new world: virtual conferencing and surgical education in the COVID-19 era. J Thorac Cardiovasc Surg. 2021;161(3):748–752. doi: 10.1016/j.jtcvs.2020.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan A., Abdullah A., Ahmad H., et al. Impact of International Quality Improvement Collaborative on congenital heart surgery in Pakistan. Heart. 2017;103(21):1680–1686. doi: 10.1136/heartjnl-2016-310533. [DOI] [PubMed] [Google Scholar]
- 27.Ravi K., Bentounsi Z., Tariq A., et al. Systematic analysis of authorship demographics in global surgery. BMJ Glob Health. 2021;6(10) doi: 10.1136/bmjgh-2021-006672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vervoort D. Five years since defining global cardiac surgery: from afterthought to tipping point. Eur J Cardio Thorac Surg. 2023;64(2) doi: 10.1093/ejcts/ezad280. [DOI] [PubMed] [Google Scholar]
- 29.Enumah Z.O., Bolman R.M., Zilla P., et al. United in earnest: first pilot sites for increased surgical capacity for rheumatic heart disease announced by Cardiac Surgery Intersociety Alliance. J Thorac Cardiovasc Surg. 2021;161(6):2108–2113. doi: 10.1016/j.jtcvs.2020.11.183. [DOI] [PubMed] [Google Scholar]
- 30.Hoffer-Hawlik M., Moran A., Zerihun L., Usseglio J., Cohn J., Gupta R. Telemedicine interventions for hypertension management in low- and middle-income countries: a scoping review. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0254222. [DOI] [PMC free article] [PubMed] [Google Scholar]