Abstract
Background
The COVID‐19 pandemic, caused by the SARS‐CoV‐2 virus, has resulted in illness, deaths and societal disruption on a global scale. Societies have implemented various control measures to reduce transmission of the virus and mitigate its impact. Individual behavioural changes are crucial to the successful implementation of these measures. One commonly recommended measure to limit risk of infection is frequent handwashing. It is important to identify those factors that can predict the uptake and maintenance of handwashing.
Objectives
We aimed to identify and synthesise the evidence on malleable psychological and psychosocial factors that determine uptake and adherence to handwashing aimed at reducing the risk of infection or transmission of COVID‐19.
Search Methods
We searched various literature sources including electronic databases (Medline ALL, Child Development & Adolescent Studies, ERIC, PsycInfo, CINAHL and Web of Science), web searches, conference proceedings, government reports, other repositories of literature and grey literature. The search strategy was built around three concepts of interest including (1) context (terms relating to COVID‐19), (2) behaviour of interest and (3) terms related to psychological and psychosocial determinants of COVID Health‐Related Behaviours and adherence or compliance with handwashing, to capture malleable determines. Searches capture studies up until October 2021.
Selection Criteria
Eligibility criteria included observational studies (both retrospective and prospective) and experimental studies that measure and report malleable psychological and psychosocial determinants and handwashing at an individual level, amongst the general public. Screening was supported by the Cochrane Crowd. Titles and abstracts were screened against the eligibility criteria by three independent screeners. Following this, all potentially relevant studies were screened at full‐text level by the research team. All conflicts between screeners were resolved by discussion between the core research team.
Data Collection and Analysis
All data extraction was managed in EPPI‐Reviewer software. All eligible studies, identified through full‐text screening were extracted by one author. We extracted data on study information, population, determinant, behaviour and effects. A second author checked data extraction on 20% of all included papers. All conflicts were discussed by the two authors until consensus was reached.
We assessed methodological quality of all included studies using an adapted version of the Joanna Briggs Institute Quality appraisal tool for cross‐sectional studies.
Main Results
Our initial searches yielded 23,587 results, of which 56 studies were included in this review. The included studies were cross sectional in design, came from 22 countries and had a combined sample of 199,376 participants. The vast majority of studies had samples from the general public, with eight of the studies focusing on specific samples. All included studies considered people over the age of 18. The quality of the majority of the studies was good (n = 30 rated low risk of bias), with 8 rated high risk of bias, predominately due to lack of reporting of recruitment, sample characteristics and methodology. Thirty‐four studies were included in the narrative synthesis and 28 in the meta‐analysis.
Findings indicated that emotions about COVID‐19 (worry [0.381, confidence interval [CI] = 0.270–0.482, I 2 = 92%) and anxiety (0.308, CI = 0.154–0.448, I 2 = 91%]), knowledge of COVID‐19 (0.323, CI = 0.223–0.417, I 2 = 94%), and perceived social norms (0.303, CI = 0.184–0.413, I 2 = 92%) were among the malleable determinants most associated with handwashing. Perceived severity (0.006, CI = ‐0.011–0.023) and susceptibility of COVID‐19 (0.041, CI = −0.034 to 0.115) had little to no effect on handwashing behaviour.
Authors' Conclusions
Understanding the effects of various malleable determinants on COVID‐related handwashing can aid in the development and implementation of interventions and public health campaigns to promote handwashing behaviour in potential new waves of COVID‐19 or other respiratory infections. Emotions about COVID, knowledge of COVID and perceived social norms warrant further consideration in future research and policy.
Keywords: anxiety, COVID‐19, handwashing, social norms
1. PLAIN LANGUAGE SUMMARY
Knowledge, anixety, worry and social norms related to COVID affect handwashing.
1.1. What is this review about?
Health‐protective behaviours, such as handwashing, will be vital to reducing risk of infection and transmission in potential new waves of COVID. Therefore, it is important to understand the factors that influence this behaviour and that can be modified.
This review examined the modifiable psychological or psychosocial determinants of handwashing.
1.2. What is the aim of this review?
This Campbell systematic review examines the determinants of handwashing in studies conducted during the COVID‐19. The review summarizes evidence from 56 studies.
1.3. What are the main findings of this review?
1.3.1. What studies are included?
This review included studies that looked at different determinants of handwashing. We included 56 studies in the review, 28 of these were included in our meta‐analysis, and 34 were described narratively. The studies were all conducted during the COVID‐19 pandemic and were conducted in 22 different countries. Many of the studies were good quality however 8 had some important weaknesses, including not providing enough detail about the sample, about how handwashing was measured and about the determinant they included.
1.3.2. What determinants were associated with handwashing?
Determinants such as knowledge of COVID, worry and anxiety about COVID and social norms were the most associated with COVID‐related handwashing. Perceived susceptibility to COVID and perceived severity of COVID had little to no effect on handwashing.
1.4. What do the findings of this review mean?
Understanding what determinants affect handwashing behaviour can help us develop better public campaigns for potential future waves of COVID or other respiratory infections. Knowledge, social norms, emotions (such as anxiety and worry) should be the target of future interventions aiming to increase handwashing to minimise respiratory infections.
1.5. How up‐to‐date is this review?
The authors of this review employed search strategies intended to capture studies up until October 2021.
2. SUMMARY OF FINDINGS
Summary of findings 1
Summary of findings:
| Determinant | Effect size | 95% CI | Q | I 2 | τ 2 | k |
|---|---|---|---|---|---|---|
| COVID‐related anxiety | r = 0.308*** | 0.154, 0.448 | 22.981 | 91% | 0.019 | 3 |
| COVID‐related worry | r = 0.381*** | 0.270, 0.482 | 35.762 | 92% | 0.014 | 4 |
| Perceived control | r = 0.185*** | 0.105, 0.262 | 7.013 | 57% | 0.004 | 4 |
| Attitudes | r = 0.264*** | 0.118, 0.399 | 84.743 | 94% | 0.033 | 6 |
| Self‐efficacy | r = 0.265*** | 0.146, 0.376 | 48.718 | 90% | 0.021 | 6 |
| Perceived effectiveness | r = 0.186*** | 0.090, 0.278 | 9.390 | 79% | 0.006 | 3 |
| Perceived risk | r = 0.202*** | 0.155, 0.248 | 2.237 | 0% | 0 | 5 |
| Perceived severity | r = 0.006 | −0.011, 0.023 | 0.319 | 0% | 0 | 3 |
| Perceived susceptibility | r = 0.041 | −0.034, 0.115 | 57.268 | 93% | 0.006 | 5 |
| Social norms | r = 0.291*** | 0.138, 0.431 | 34.509 | 91% | 0.025 | 4 |
| Knowledge about behaviour | r = 0.261* | 0.007, 0.484 | 60.292 | 97% | 0.051 | 3 |
| Knowledge about the disease | r = 0.337*** | 0.238, 0.428 | 65.716 | 92% | 0.016 | 6 |
Abbreviations: CI, confidence interval; I 2, percentage of variability due to between‐study heterogeneity; k, number of effect sizes; Q, test for heterogeneity; r, correlations; SMD, standardised mean difference; τ 2, random effects variance component.
*p < 0.05
***p < 0.001.
3. BACKGROUND
3.1. The problem, condition or issue
Severe acute respiratory coronavirus 2 (SARS‐CoV‐2) emerged in late 2019 and spread rapidly around the globe (Cucinotta & Vanelli, 2020; Wu et al., 2020). The pandemic of COVID‐19 disease, caused by SARS‐CoV‐2, has resulted in short and long‐term illness, deaths and societal disruption. Societies implemented control measures to reduce the transmission of the virus. Individual behaviour change is crucial to the success of these measures through reducing the frequency of social contacts, mitigating the risk of those social contacts and reducing the amount of time that infectious people are in contact with others whom they may infect. Despite vaccine programmes being introduced in December 2020, waning immunity and the evolution of new variants, indicate the significance of behavioural measures to reduce the spread (Girum et al., 2021; Michie & West, 2020).
The behaviours to reduce the risk of catching or spreading SARS‐CoV‐2 including: handwashing or use of hand sanitiser, wearing masks or face coverings, physical distancing, social distancing, isolation or quarantine, respiratory hygiene, cleaning surfaces, avoiding touching the ‘T‐zone’ (mouth, nose and eyes) (Elder et al., 2014) as well as other composite measures that include these behaviours.
The evidence for the effectiveness of these measures has been established during previous pandemics of similar serious viral respiratory infections such as pandemic Influenza A (H1N1), SARS and MERS (Flumignan et al., 2020; Jefferson et al., 2020; Seto et al., 2003; Warren‐Gash et al., 2013; Webster et al., 2020; West et al., 2020). It is important to synthesise the evidence on the determinants of these measures during the COVID‐19 pandemic, that may be applied to future pandemics of influenza and other serious respiratory infectious diseases.
3.2. Exposure/determinants
The exposure in this review was psychological or psychosocial determinants of handwashing. To be included, determinants were malleable factors that could, theoretically, be changed by a public health intervention.
3.3. Why it is important to do this review
Handwashing cannot be effective on a societal level if it is not adopted widely and consistently. Variables such as individual health beliefs, social support, culture, and social norms can all influence the likelihood of someone undertaking and maintaining health behaviours such as handwashing. To develop appropriate public health interventions to improve uptake and adherence to handwashing, including effective messaging, it is important to understand the malleable factors that influence this behaviour. We identified and examined all existing research evidence that described a relationship between any malleable factor or determinant (or those that can be most effectively targeted as part of public health interventions) and handwashing in the context of SARS‐CoV‐2.
In this review, we are interested in the evidence on malleable and non‐malleable psychological and psychosocial factors associated with uptake and adherence to health protective behaviours. Malleable determinants in this EGM refer to psychological and psychosocial factors that can be developed, shaped or altered. Factors such knowledge, access to information, emotions, and perceptions. Non‐malleable determinants in this EGM refer to factors or attributes that are fixed or unchangeable through public health intervention. Factors such as age, sex, income, past behaviour, and health status.
In any future severe viral outbreaks, health‐protective behaviours, such as handwashing, will be vital to reducing risk of infection and transmission. Non‐pharmaceutical interventions that are designed to improve the uptake and adherence to protective behaviours are essential in an outbreak, and in particular when vaccines and treatments are not yet established. The effectiveness of these behaviour change interventions will be determined, to some extent, by how they address the psychological and psychosocial variables that influence behaviour. To optimise public health intervention, we need to know which specific variables are most likely to influence the target behaviours, such as handwashing, in this context. Evidence gathered in the context of COVID‐19 can inform who, when and under what circumstances people do or do not adopt recommended preventive behaviours.
There are a number of related published and ongoing reviews on individual determinants of COVID‐19 health‐related behaviours but none with the broad scope of this review. Using robust search, retrieval, and methodological approaches to minimise potential sources of bias, this review examines the existing and emerging evidence on determinants of handwashing in the context of the COVID‐19 pandemic.
3.4. Overview of the COHeRe project
COHeRe is a UKRI funded project https://www.qub.ac.uk/schools/psy/Research/OurResearchThemes/HealthWelfareClinicalPsychology/COHeRe/ made up of a team with substantial expertise in systematic reviews, health behaviour and infectious diseases. The overall aim of the project was to identify, synthesis, and examine evidence on determinates of COVID‐19 health‐related behaviours. The specific behaviours of interest were as follows:
Handwashing
Wearing masks/face coverings
Physical Distancing
Social Distancing
Isolation/quarantine
Respiratory hygiene
Cleaning surfaces
Avoiding t‐zone
Other composite measures that include the above.
During Phase 1 of the project a rapid review was conducted, which examined determinants of protective behaviours during COVID‐19 and during previous outbreaks of similar serious respiratory infections, for example, SARS, MERS and H1N1 (swine flu) (Hanratty et al., 2021). Of the 233 studies included in the rapid review, 54 were conducted in the context of COVID‐19, while the remainder were conducted in the context of other respiratory infections. Over the course of conducting the rapid review, it became apparent that the evidence base examining determinants in the context of COVID‐19 was rapidly expanding and further identification and examination was needed of this new evidence.
On this basis, further funding was secured to conduct Phase 2 of the project, which identified and mapped the existing evidence (published and unpublished between January 2020 and October 2021) on malleable and non‐malleable psychological and psychosocial factors that determine uptake and adherence to behaviours aimed at reducing the risk of infection or transmission of COVID‐19 (Hanratty et al., 2022, 2023). As of 1 June 2022 the Evidence and Gap Map (EGM) includes 1034 records https://eppi.ioe.ac.uk/eppi-vis/login/open?webdbid=188.
This current review is the final phase of the wider project. Based on those studies included in the EGM we further examined these, through a series of systematic reviews examining which malleable determinants (or those that can be most effectively targeted as part of public health interventions) are more closely associated with uptake and maintenance of individual protective behaviours. This current review examines the protective behaviour of handwashing, however is part of a series of reviews considering the 8 other behaviours of interest.
4. OBJECTIVES
We intended to identify and synthesise the existing evidence on malleable psychological and psychosocial factors that determine uptake and adherence to handwashing that can reduce the risk of infection or transmission of COVID‐19.
5. METHODS
None
5.1. Criteria for considering studies for this review
5.1.1. Types of studies
This systematic review contains studies that quantify the relationship between a malleable determinant and handwashing. Included study designs consisted of observational studies (both retrospective and prospective) and experimental studies that measure and report malleable psychological and psychosocial determinants and handwashing at an individual level. We did not include narrative reviews, modelling studies, letters, editorials, opinion pieces, news, commentaries, or any other publications that did not report primary data.
5.1.2. Types of participants
The population of interest is members of the general public, of any age. Within the group of studies of the general public, we included studies on specific groups of people that may be at increased risk of catching the virus for example, people who work in essential retail services. Similarly, we included studies of specific patient groups at increased risk of becoming seriously ill if infected, for example, those with existing chronic respiratory disorders. However, we did not include studies on health care workers (HCWs), defined as someone who works in a hospital or health care setting or delivers health care in the community. This population typically have, or should have additional knowledge, training and resources to support the adoption of behaviours to mitigate against the increased risk of exposure to infectious diseases. A rapid review on barriers and facilitators to HCWs adherence to infection prevention and control guidelines has been published (Houghton et al., 2020). For those studies that included both HCWs and the public, were only included if data on the public is presented separately from data on healthcare workers.
5.2. Exposure/determinants
The exposure in this review was psychological or psychosocial determinants of handwashing. To be included determinants were malleable factors that could, theoretically, be changed by a public health intervention.
We developed 10 categories of determinants for phase 2 of this project. These included, behaviour, cognition, demographics, disease, emotions, health status, information, intervention, knowledge and other Table 1. Each category was divided into subcategories of various determinants. As above, only malleable determinants were included in this review. Therefore, the following determinants were included:
Table 1.
Determinant categories and subcategories.
| Determinant category | Subcategories | ||||
|---|---|---|---|---|---|
| Emotions | Feelings about the disease | 'Other’ emotion‐related determinants (e.g., general emotional state or mood) | |||
| Cognition (thoughts or perceptions) | About the protective behaviours | About COVID‐19 | Motivations to engage in behaviour | Social cognition (e.g., perceived social norms) | Cognitive capacity indicating a person's ability to understand or retain information |
| Knowledge (knowledge of) | Protective behaviours | COVID‐19 | Any other types of assessed knowledge, such as knowledge of regulations or knowledge of vaccines | ||
| Information | Seeking and consuming information | The quality or source of information | Public health messaging (e.g. message content or framing) | ||
| Other | Beliefs (e.g., political beliefs) | social (e.g., social capital, social networks) | Practical resources (i.e., access to masks) | Cultural (i.e. collectivist vs. individualist cultures) | |
Emotions captured determinants related to feelings about the disease and ‘other’ emotion‐related determinants for example general emotional state or mood.
Cognition was broken down into six subcategories: thoughts or perceptions about the protective behaviours; about COVID‐19; motivations; social cognition (e.g., perceived social norms); cognitive capacity indicating a person's ability to understand or retain information; ‘other’ to capture any other cognitive determinant that did not fit into the previous five subcategories.
Knowledge included determinants relating to knowledge about protective behaviours, knowledge about the disease and any other types of assessed knowledge, such as knowledge of regulations or knowledge of vaccines.
Information included seeking and consuming information, the quality or source of information, and determinants related to public health messaging, for example, message content or framing.
Other was the final category of determinants and includes any determinants that did not fit within the previous broad categories. This was divided into subcategories of beliefs, for example, political beliefs, social (e.g., social capital, social networks), practical resources such as access to masks, paid sick leave, time included time since the outbreak began, cultural determinants such as collectivist vs individualist cultures, and a final ‘other’ subcategory for any remaining determinant that did not fit into the previous subcategories.
The determinants of behaviour, demographics, disease, and health status were not included as these were categorised as non‐malleable. We also did not include studies that examined interventions as a determinant of handwashing as this will be analysed in a separate review.
Comparators were the absence of the determinant (compared to its presence) or, where a determinant is presented as a continuous measure, then analysis will be based on correlation between handwashing and determinants.
We included studies that measured determinants at an individual level and group level, for example, country‐level data on the number of cases.
We included studies on self‐reported or observed determinants. Self‐reports included actual or perceived determinants, for example ‘risk of contracting the virus’ could be measured by quantifying actual risk based on individual circumstances and behaviour or through self‐reported perceived risk.
5.2.1. Types of outcome measures
While our searches sought to identify evidence on commonly recommended behaviours to mitigate human‐to‐human spread of COVID‐19 as described by (West et al., 2020), this current review focuses on handwashing only. We define handwashing as, washing hands more frequently with soap and water or the use of hand sanitizer if handwashing facilities are not available.
We included studies on actual handwashing behaviour, through self/other report and/or observation, measured at the individual level. We excluded studies that measured intended behaviour or hypothetical behaviour.
Primary outcomes
The primary outcome of this review was handwashing. No secondary outcome was considered.
5.3. Search methods for identification of studies
To ensure that the literature contained in the review was relevant and useful to key stakeholders, it was important that the literature retrieval methods followed high‐quality standards and all searches were conducted and reported following Campbell Collaboration guidelines (White et al., 2020).
Information retrieval specialist author (CK) developed and piloted a search strategy with input from clinical and behaviour change expert authors (DB and MD). This strategy was further refined by CK following expert advice from a Campbell information retrieval specialist during the editorial/peer review of the protocol. Searches strageries in the current review capture studies up until October 2021.
The search strategy was built around three concepts of interest;
-
(1)
Context (terms relating to COVID‐19). For concept one, we used an innovative and tested COVID‐19 search strategy was developed for use by NICE information specialists and was updated as recently as 21 June 2021 (Levay & Finnegan, 2021). An example of the search string was piloted in Medline (Ovid) and is presented in Table 3.
-
(2)
Behaviours of interest.
-
(3)
Terms related to psychological and psychosocial determinants of COVID Health‐Related Behaviours and adherence or compliance with recommended behaviours, to capture both malleable and non‐malleable determinants.
Table 3.
Demographics of included studies.
| Study | Country | Study design | Describe population | Age | Sex ‐number of women/girls | Sex ‐number of men/boys | Overall quality rating |
|---|---|---|---|---|---|---|---|
| Al‐Sejari (2021) | Kuwait | Cross sectional | General public (n = 1413) | Ranged from 18 to 99 years (mean = 39) | 69.2% of sample | 30.4% of sample | Low risk of bias |
| Al‐Shammary (2021) | Saudi Arabia | Cross sectional | General public (n = 400) | Mean 37.6 (10.8) | 203 | 197 | Low risk of bias |
| Al‐Wutayd (2021) | Saudi Arabia | Cross sectional | General public (n = 1323) | 30–39: (27%) | 645 (49%) female | 678 (51%) were males, | Unclear risk of bias |
| Apanga (2021) | Ghana | Cross sectional | Pregnant women (n = 527) | M 26 (SD 5.9) | 100% | 0 | Low risk of bias |
| Barrett (2021) | UK | Cross sectional | UK university students (n = 293) | 73.4% 18–25 years; 26.6% over 25 | 189 | 100 | Low risk of bias |
| Bogg (2020) | USA | Cross sectional | General public (n = 500) | M 45.4, SD 15.78 | 257 | 243 | Low risk of bias |
| Bruine de Bruin et al. ( 2020 ) | USA | Cross sectional | General public (n = 6684) | Adults 20% 65 or over | 3458 52% | 48% 3226 | Low risk of bias |
| Bruine de Bruin et al. (2020) | US | Cross sectional | General public (n = 5517) | 20% were aged 65 and older | not reported | 48% male | High risk of bias |
| Callaghan (2021) | USA | Cross sectional | General public (n = 5009) | Not reported | not reported | Not reported | Low risk of bias |
| Cowling et al. (2020) | Hong Kong | Cross sectional | General public (n = 12,965) | 18–24: 1371 (13%) 25–34: 1210 (12%) 35–44: 1915 (19%) | 61% 6308 | 39% 4026 | Low risk of bias |
| Dixon et al. (2022) | United Kingdom ‐ Scotland | Cross sectional | General public (n = 2969) | 16–24 years old: 273 25–34 years old: 385 35–44 years old: 360 45–54 years old: 540 55–64 years old: 607 65+ years old: 804 | 1,765 59.6% | 1198 40.4% | Low risk of bias |
| Dwipayanti (2021) | Indonesia | Cross sectional | General public (n = 896) | M 35 | 543 (60.60%) | 353 (39.40%) | Unclear risk of bias |
| Fujii (2021) | Italy, Japan, Korea, USA, China, UK | Cross sectional | General public (n = 5945) | 3045 women | 2900 men | Unclear risk of bias | |
| Graupensperger (2021) | United States | Cross sectional | Young adult (n = 539) (recruited from university) | 19.5 years (SD = 0.8) | 58.8% women | Not reported | High risk of bias |
| Haliwa et al. (2020) | USA | Cross sectional | General public (n = 353) | Mean = 41.47 years, SD = 12.49, range: 19–84 | 59.8% women | Not reported | Low risk of bias |
| Hsing (2021) | USA | Cross sectional |
General public (n = 71,851) (From US, Mexico, Hong Kong and Taiwan) |
18–24 years: n (%) US 110 (3.6) Mexico 507 (12.9) Hong Kong 83 (7.0) Taiwan 4969 (7.8) |
US 1683 (55.0) Mexico 2031 (51.6) Hong Kong 602 (50.4) Taiwan 31,407 (49.6) |
US 1351 (44.2) Mexico 1867 (47.4) Hong Kong 562 (47.1) Taiwan 30,034 (47.4) |
Unclear risk of bias |
| Iqbal (2021) | Pakistan | Cross sectional | General public (n = 1789) |
18–25 (49.52%) 26–30 (27%) 31–40 (19.01%) >40 years: (4.47%) |
949 (53.05%) | 840 (46.95%) | High risk of bias |
| Jang et al. (2020) | Korea | Cross sectional | General public (n = 1,004) | 19–29: (17.8%) | 50.2% | 49.8% | Low risk of bias |
| Jimenez (2020) | USA | Cross sectional | General public (n = 290) | M 37.12 (SD 12.03) | 122 (40%) | 180 (59%) | Low risk of bias |
| Jovančević & Milićević (2020) | Serbia/Latin‐America | Cross sectional | General public (n = 412) |
Serbia: (M = 30.34; SD = 9.89) Latin America (M = 33.51, SD = 11.23) |
Serbia (Female = 250) Latin‐America (Female = 95) | Serbia (N = 292, Male = 42) Latin‐America (N = 120, Male = 25) | Unclear risk of bias |
| Kebede (2020) | Ethiopa | Cross sectional | Visitors to a medical centre (n = 247) | M 30.5 (SD 10.2) | 23% 58 | 77% 189 | Unclear risk of bias |
| Kowalski (2020a) Study 1 | Poland | Cross sectional | General public (n = 507) | 44.07 (±14.41) | 253 (49.9%) | Not reported | Low risk of bias |
| Kowalski (2020b) Study 2 | Poland | Cross sectional | General public (n = 840) | 29.94 (±10.39) | 607 (72.3%) | Not reported | Low risk of bias |
| Lahiri (2021) | India | Cross sectional | General public (n = 2646) | aged ≤35 years (43.08%), | 998 (37.72%) | 1648 (62.28%) | High risk of bias |
| Lao et al. (2023) | China | Cross sectional | Residents in Hubei province (n = 229) | M(SD) 25.37(8.34) | 141 (61.6%) | 88 (38.4%) | Low risk of bias |
| Lee (2020) | South Korea, Ethiopia, and Democratic Republic of Congo | Cross sectional | General public (n = 748) (from South Korea, Ethiopia, and Democratic Republic of Congo) | South Korea M = 22.9, SD = 4.7 Ethiopia M = 26, SD = 5.7 Democratic Republic of Congo M = 26.1, SD = 4.2 | South Korea female: 215(58.1%) Ethiopia female: 60 (34.3%) Democratic Republic of Congo female: 103(52.6%) | South Korea male: 155(42.9%) Ethiopia male: 115(65.7%) Democratic Republic of Congo male: 93(47.4%) | High risk of bias |
| Lee et al. (2021) | South Korea | Cross sectional | General public (n = 970) |
M = 47.44 SD = 14.78 |
499 (51.4%) | 471 (48.6%) | Unclear risk of bias |
| Li (2021) | USA | Cross sectional | Student pharmacists (n = 326) |
18–26: 258 (79.1%) 27: 68 (20.9%) |
242 females (74.2%) | 84 males (25.8%) | Unclear risk of bias |
| Matkovic et al. (2021) | USA | Intervention study | General public (n = 344) | M = 32.69, SD = 11.60 | 54.1% | 43.9% | Unclear risk of bias |
| Milman (2020) | USA | Cross sectional | General public (n = 408) | M 37.24 (SD 10.90) | 174 | 233 | Unclear risk of bias |
| Mousavi et al. (2022) | Afghanistan | Cross sectional | General pubic (n = 450) |
17–26 (65.8%) 27–36 (22.9%) 37–46 (8.2%) 47–56 (2.2%) >57 (0.9%) |
138 (28.4%) | 322 (71.6%) | Unclear risk of bias |
| Nelson (2021) | USA | Cross sectional |
Employees of Colorado State University (n = 508) |
M 41.1 (SD12.5) | 305 (60.0%) | 200 (39.4%) | Unclear risk of bias |
| Norman (2020) | UK | Cross sectional | General public (n = 477) | M 46.22 (SD 15.20) | 243 (50.9%) | 234 (49.1%) | Low risk of bias |
| Owhonda (2022) | Nigeria | Cross sectional | General public (n = 1294) | M 39.6 (SD 11.9) | 584 (45.1%) | 710 (54.9%) | Unclear risk of bias |
| Ozdemir et al. (2022) | Singapore | Cross sectional | General public (n = 897) | M 42 (SD 12.8) | 427 (47.6%) | 470 (52.4%) | Low risk of bias |
| Pal et al. (2020) | India | Cross sectional | People with T1 Diabetes (n = 212) | M 25.1 (SD 4.3) | 52% (111) | 48% (101) | Unclear risk of bias |
| Pan (2020) | China | Cross sectional | Factory workers (n = 3035) |
<30 years of age (1552, 51.1%) |
1423 (46.9%) | 1612 (53.1%) | Low risk of bias |
| Prete (2020) | Italy | Cross sectional | General public (n = 618) | M 38.55 (SD = 15.26) | 441 (71.4%) | 177 (28.6%) | Unclear risk of bias |
| Qian (2020) | China | Cross sectional | General public (n = 1011) (from Wuhan % Shanghai) |
Wuhan: 18–24 89 (21.6%) Shanghai: 18–24 75 (13.9%) |
Not reported |
Wuhan: 255 (50.0%) Shanghai: 255 (48.7) |
Low risk of bias |
| Rattay (2021) | Germany | Cross sectional | General public (n = 27,957) |
18–29: 19.1% 30–45: 30.1% 46–60: 28% >60: 22.8% |
51% women n = 14,133 | 49% men n = 13,824 | Unclear risk of bias |
| Rui (2021) Study 1 | China | Cross sectional | General public (n = 321) |
18–30: 55 (17.1% 31–45: 97 (30.2%) >46: 169 (52.6%) |
167 (52%) | 154 (48%) | Low risk of bias |
| Rui (2021) Study 2 | China | Cross sectional | General public (n = 319) |
18–30: 64 (20.1%) 31–45: 82 (25.7%) >46:173 (54.2%) |
155 (48.6%) | 164 (51.4) | Low risk of bias |
| Rui (2021) Study 3 | China | Cross sectional | General public (n = 315) |
18–30: 63 (20%) 31–45: 87 (27.6%) >46: 165 (52.4%) |
174 (55.2%) | 141 (44.8) | |
| Rui (2021) Study 4 | China | Cross sectional | General public (n = 343) |
18–30: 84 (24.5%) 31–45: 110 (32.1%) >46: 149 (43.4%) |
186 (54.2%) | 157 (45.8) | Low risk of bias |
| Rui (2021) Study 5 | China | Cross sectional | General public (n = 329) |
18–30: 74 (22.5%) 31–45: 86 (26.1%) >46: 169 (51.4%) |
176 (53.5%) | 153 (46.5) | Low risk of bias |
| Rui (2021) Study 6 | China | Cross sectional | General public (n = 315) |
18–30: 60 (19%) 31–45: 80 (25.4%) >46: 175 (55.6%) |
152 (48.3% | 163 (51.7) | Low risk of bias |
| Sengeh (2020) | Sierra Leone | Cross sectional | General public (n = 1,253) | 18–39 (58%) | 604 (48%) | 648 (52%) | High risk of bias |
| Sharma | USA | Cross sectional | University students (n = 713) | M 24.61 (SD 8.60) | 501 (70.3%) | 176 (24.7%) | Unclear risk of bias |
| Shook (2020) | USA | Cross sectional | General public (n = 1,023) | M 46.32 (SD 16.57) | 514 (50.8%) | 497 (49.1%) | Unclear risk of bias |
| Si et al. (2021) | US | Cross sectional | General public (n = 1,019) | M 46.33 (SD 16.57) | 514 female | 497 male | Low risk of bias |
| Souliotis (2021) | Greece | Cross sectional | General public (n = 923) | 25–54 (51.4%) | 49.2% | 50.8% | Unclear risk of bias |
| Stojanovic (2021) | Italy | Cross sectional | General public (n = 1332) |
<25: (57%) 26–50 (33.3%) >51 (9.7%) |
899 (68%) | 422 (32%) | Low risk of bias |
| Trifiletti (2021) | Italy | Cross sectional | General public (n = 248) | M 34.78 (SD 14.76) | 176 females | 72 males | Unclear risk of bias |
| van den Broek‐Altenburg (2021) | Netherlands and Belgium | Cross sectional |
General public The Netherlands (n = 2637) General public Flanders (n = 1678) |
18–25: 483 (11.19%) | 2250 (52.14%) | not reported | Low risk of bias |
| Wang (2021) | China | Cross sectional | Pregnant women (n = 15,428) | <30 (59.9%) | 100% | None | Low risk of bias |
| Zewude et al. (2021) | Ethiopia | Cross sectional | People from the urban‐based informal economy (n = 384) | M 24.6 (SD 6.87) | 161 (42.5%) | 218 (57.5%) | Low risk of bias |
For concept 2 and 3 the terms used were based on those used in the rapid review (Hanratty et al., 2021) which itself was informed through consultation with the Behaviour Change Group formed in response to COVID‐19 by the Public Health Agency, Northern Ireland. The terms were then piloted and refined in two databases, with unique terms added and redundant or duplicate terms removed (Table 2).
Table 2.
Medline (Ovid) search strategy.
| Ovid MEDLINE(R) ALL <1946 to 3 September 2021> | ||
|---|---|---|
| 1 | SARS‐CoV‐2/or COVID‐19/ | 103,591 |
| 2 | (corona* adj1 (virus* or viral*)).ti,ab. | 2364 |
| 3 | (CoV not (Coefficien* or ‘co‐efficien*’ or covalent* or Covington* or covariant* or covarianc* or ‘cut‐off value*’ or ‘cutoff value*’ or ‘cut‐off volume*’ or ‘cutoff volume*’ or ‘combined optimi?ation value*’ or ‘central vessel trunk*’ or CoVR or CoVS)).ti,ab. | 51,911 |
| 4 | (coronavirus* or 2019nCoV* or 19nCoV* or ‘2019 novel*’ or Ncov* or ‘n‐cov’ or ‘SARS‐CoV−2*’ or ‘SARSCoV‐2*’ or SARSCoV2* or ‘SARS‐CoV2*’ or ‘severe acute respiratory syndrome*’ or COVID*2).ti,ab. | 181,470 |
| 5 | or/1‐4 | 187,096 |
| 6 | limit 5 to yr = ‘2020‐Current’ | 173,962 |
| 7 | (6 and english.lg.) not (letter or historical article or comment or editorial or news).pt. not (Animals/not humans/) | 134,173 |
| 8 | (Mask or masks or face?mask* or Face cover*).ti,ab. | 42,975 |
| 9 | (face adj2 (shield or shields)).ti,ab. | 414 |
| 10 | (((Hand or hands) adj2 hygiene) or Handwash* or (Wash* adj2 hand*)).ti,ab. | 11,132 |
| 11 | (hand adj1 clean*).ti,ab. | 256 |
| 12 | (hand adj2 saniti*).ti,ab. | 683 |
| 13 | (hand adj2 disinfect*).ti,ab. | 783 |
| 14 | Respiratory hygiene.ti,ab. | 79 |
| 15 | Respiratory etiquette.ti,ab. | 27 |
| 16 | ((cough* or sneeze*) and (sleeve or arm or elbow or tissue or etiquette)).ti,ab. | 2752 |
| 17 | (tissue and (dispose or disposal or bin or hygiene)).ti,ab. | 3414 |
| 18 | universal hygiene.ti,ab. | 10 |
| 19 | Social Isolation/or Patient Isolation/ | 19,284 |
| 20 | (self‐isolate or self‐isolation or self‐isolating).ti,ab. | 724 |
| 21 | (mass adj2 (behav* or gather*)).ti,ab. | 1690 |
| 22 | (social distance or social distancing).ti,ab. | 6625 |
| 23 | stay at home.ti,ab. | 1465 |
| 24 | stay home.ti,ab. | 314 |
| 25 | ((work* adj2 home) or telecommute or telework* or (remote* adj2 work*)).ti,ab. | 5262 |
| 26 | (Physical adj2 distanc*).ti,ab. | 2595 |
| 27 | (touch* and (mouth or mouths or face or faces or nose or noses or t‐zone)).ti,ab. | 1635 |
| 28 | disinfect*.ti,ab. | 31,760 |
| 29 | lockdown.ti,ab. | 8167 |
| 30 | quarantine.ti,ab. | 7821 |
| 31 | (nonpharmaceutical or non‐pharmaceutical).ti,ab. | 1831 |
| 32 | (school closure or close school* or school closing).ti,ab. | 389 |
| 33 | or/8‐32 | 140,404 |
| 34 | limit 33 to yr = ‘2020‐Current’ | 34,955 |
| 35 | (34 and english.lg.) not (letter or historical article or comment or editorial or news).pt. not (Animals/not humans/) | 31,455 |
| 36 | 7 and 35 | 20,298 |
| 37 | exp Knowledge/ | 12,323 |
| 38 | exp Health knowledge, Attitudes, Practice/ | 119,567 |
| 39 | (Knowledg* or Personal* or Attitude* or Practice* or Habit* or belie* or Behav* or Need* or prevent* or Compliance or comply* or complied or Perception* or Protect* or Predict* or view* or barrier* or facilitator* or readiness or prepar* or ability* or insight or proficien* or procedur* or adher*).ti,ab. | 10,617,318 |
| 40 | or/37‐39 | 10,635,825 |
| 41 | 7 and 35 and 40 | 14,859 |
5.3.1. Electronic databases
Based on the Queens's University Belfast database subscriptions, we searched the following key information sources to locate relevant primary research:
Medline ALL (Ovid)
Child Development & Adolescent Studies (EBSCOhost)
ERIC (EBSCOhost)
PsycInfo 1806‐present (OVID)
CINAHL Plus (EBSCOhost)
Web of Science Core Collection (the QUB subscription includes SCI‐expanded, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, ESHI)
To locate relevant secondary research for inclusion in the EGM, we searched the following information resources:
The Social Care Institute for Excellence (SCIE)
The Cochrane Library
Epistemonikos Covid‐19 evidence platform
Norwegian Institute of Public Health living maps
EPPI – centre
COVID‐END
5.3.2. Other sources
We searched for Grey literature across multiple sources. Grey literature is that which is not published, not peer reviewed, and not easily accessible. Sources of grey literature are varied and include government reports, privately and publicly funded research, conference proceedings, working papers, and posters. Some grey literature sources are captured in the Web of Science search, these include:
Conference Proceedings Citation Index‐ Science (CPCI‐S)—1990‐present
Conference Proceedings Citation Index‐ Social Science & Humanities (CPCI‐SSH)—1990‐present
We attempted to locate additional grey literature by searching sources such as the following:
Google Scholar (We will search https://scholar.google.com/ using an incognito browser and the following strategy: (coronavirus| ‘2019 nCoV’| ‘2019 novel’| ‘2019 nCoV’| ‘2019 nCoV’| CoV |‘COVID 19’ |COVID19| ‘COVID 19’| ncov |‘SARS CoV2’| ‘SARS CoV 2’|‘severe acute respiratory syndrome Coronavirus 2’) (Psychological|Psychosocial)(behavior|behaviour) we will limit returns by ‘Since 2020’ filter and sort remaining records by relevance. We downloaded the first 1000 articles (which is the upper limit set by Google) using Harzing's Publish or Perish software.
ISRCTN Registry (https://www.isrctn.com/)
-
WHO International Clinical Trials Registry Platform (ICTRP) (https://www.who.int/clinical-trials-registry-platform/the-ictrp-search-portal)
And by contacting and reviewing the information of the following key organisations in the UK with proven experience on the topics related to this project:
King's Fund (https://www.kingsfund.org.uk/)
National Institute for Health Research (https://www.nihr.ac.uk/)
NHS Evidence (https://www.evidence.nhs.uk/)
We considered searching ProQuest dissertations and theses, however, we assessed that it was unlikely that any relevant doctoral theses would be complete and available in the timeframe of the virus.
We conducted a search of reference lists of previous reviews and eligible articles to identify any additional studies not identified through the electronic search. Finally, when we compiled a list of included studies, we contacted key experts in the field via email (categorised as ‘key’ if they have published five or more included studies) to ask whether they were aware of any unpublished or ongoing research that might not have been easily accessible to the research team.
To locate additional relevant grey literature for inclusion in the EGM, we searched for ongoing or unpublished reviews via:
PROSPERO,
Figshare and the
Open Science Framework (OSF).
Any ongoing reviews were checked again before completion of the project, and, if still unpublished were excluded from the map.
5.3.3. Search limits
Due to the limited language skills of the review team, we only included studies published in English.
We limited our search to exclude opinion pieces, letters, editorials and unpublished reports in databases where these limits are supported (See Table 3: lines 7 and 35). We did not use database limiters for studies on humans only as we found these limiters excluded a substantial number of potentially relevant papers not indexed as ‘human’ studies. Instead, we have opted to use an adaptation of the Cochrane search filter for human studies (line 7 and 35).
We included only those studies which were conducted during the ongoing COVID‐19 pandemic. We included studies from Jan 2020 until the date of the final search.
5.4. Data collection and analysis
5.4.1. Selection of studies
All search results were first screened on titles and abstracts against the eligibility criteria by three independent screeners. Screening at this first stage was supported by the Cochrane Crowd. We retrieved a full‐text copy of all potentially relevant studies during the title and abstract screening. Following this, all potentially relevant studies were screened independently by at least two reviewers from the research team at full‐text level. All conflicts between screeners were resolved by discussion between the core research team.
5.4.2. Data extraction and management
All data extraction was managed in EPPI‐Reviewer software. All eligible studies, identified through full‐text screening were extracted by one author, who also completed the quality appraisal assessment. Any studies identified as ineligible during data extraction stage were listed as ‘excluded’. A second author checked the data extraction and risk of bias assessments on 20% of all included papers. The two people who completed the data extraction for each study discussed any discrepancies until they reach a consensus or, referred to a third author to make a final decision. In addition, the research team met on a weekly basis to discuss extraction and discrepancies, in aid coherence to the extraction protocol. Where data was not available or was missing within an included study, the research team attempted to obtain or clarify data from the relevant authors.
Extracted information included (Supporting Information 5):
Study information: Author, year, country, study design, when the study was conducted, sample size.
Population: description of the population, age, sex.
Exposure: determinant measured, description of the determinant, who measured the determinant, type of measurement (observation, self‐reported, etc.), direction and quality of the scale.
Outcome: behaviour measured, description of the behaviour, who measured the behaviour, type of measurement (observation, self‐reported, etc.), direction and quality of the scale.
Effects: Narrative description of the finding, effect size information or sufficient numerical data to allow us to calculate the effect size.
5.4.3. Quality appraisal
The JBI tool for cross‐sectional studies was used to assess the quality of included studies (The Joanna Briggs Institute, 2017; The Joanna Briggs Institute, 2020). After piloting the JBI tool on some known studies we decided to modify the tool to ensure that they are fit for our purposes (Supporting Information 6). We changed the wording of the second item ‘were the study subjects and the setting described in detail’ to ‘was the sample included in the study representative of the population of interest?’ to assess whether or not the sample was representative of the population of interest. We also changed the wording slightly, replacing condition and exposure with behaviours of interest and determinants, respectively.
The eight questions were answered with either ‘yes’, ‘no’, or ‘unclear’. For the questions on scale validity and reliability, we indicated whether a single‐item or multiple‐item scale was used and whether or not this was reliable and valid. Each study was rated either low, high or unclear risk of bias through adding up the total number of items answered ‘yes’. For example, >70% yes = Low Risk of Bias, 50%–70% yes = Unclear Risk of Bias, and <50% ‘Yes’ = High Risk of Bias.
5.4.4. Measures of treatment effect
We extracted data on the relationship between handwashing and determinants of that behaviour. Outcomes were reported in both dichotomous and continuous data. The meta‐analysis was performed using Comprehensive Meta‐Analysis Version 4 (Comprehensive Meta‐Analysis Version 4, 2022), and conducted using correlation coefficients (r), as that was the effect size statistic most commonly reported in the papers. Therefore, data was extracted that allowed us to convert or calculate r. For example, where summary statistics were not presented, we extracted data such as means and standard deviations that allowed us to calculate a standardised mean difference that was then converted to r. Effect sizes were interpreted according to thresholds suggested by Cohen 1988: weak (r = 0.1), moderate (r = 0.3), and strong (r = 0.5).
5.4.5. Unit of analysis issues
There are two reports that include multiple studies (Rui et al., 2021; Kowalski 2020a). Given that these separate studies utilised different samples, we treated as individual studies. Each individual study is referred to Author study 1, Author Study 2 and so on.
5.4.6. Assessment of heterogeneity
Heterogeneity was assessed first, through visual inspection of the forest plot and checking for overlap of confidence intervals and second through the Q, I 2 and τ 2 statistic. Investigation of the source of heterogeneity is addressed in data synthesis section.
5.4.7. Data synthesis
Given the diverse range of behaviour and determinant relationship examined across the included studies, we used random effects models, using inverse‐variance estimation. We conducted separate meta‐analyses for each determinant of the behaviour of interest, handwashing.
-
–
Determinants were grouped based on previous mapping (Hanratty et al., 2023);
-
–
Determinant groups were included in the meta‐analysis if they included data that was suitable for meta‐analysis (i.e. unadjusted data) and there was a minimum of three data points;
-
–
We excluded adjusted estimates from meta‐analyses as there is considerable variation in the covariates used to adjust these estimates across studies and, therefore, we judged that the adjusted estimates were not suitable for statistical aggregation;
-
–
Data that was not suitable was synthesised narratively.
Treatment of qualitative research
The review does not include qualitative research.
6. RESULTS
6.1. Description of studies
6.1.1. Results of the search
As seen in Figure 1, our searches yielded a total of 23,587 results. After screening out titles/abstracts we were left with 2444 results. Of these 2444 reports 2388 were excluded. Reasons included being directly COVID‐related, using predictive modelling methods, not relevant behaviour (including behaviours like mask‐wearing and distancing included in our other reviews reported elsewhere) or determinant, ineligible population or publication, no relationship measured between behaviour and determinant or a duplicate not found at the initial screening stage. Following full‐text screening of these results yielded 56 eligible studies.
Figure 1.
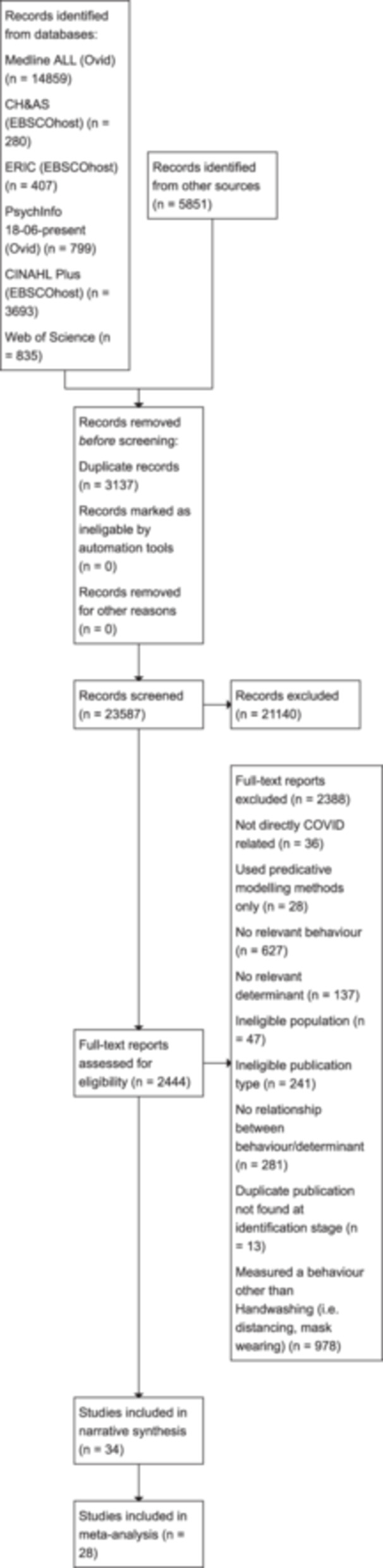
PRISMA flow diagram.
6.1.2. Included studies
A total of 56 studies were included in this review. Of these 56 studies, all used a cross sectional design. As detailed above, two of the reports (Kowalski 2020a (Kowalski et al., 2020a); Rui et al., 2021 (Rui et al., 2021) included separate studies. Kowalski 2020a reported two studies, and Rui et al., 2021 reported six separate studies. The 56 studies came from 22 different countries, with the majority coming from the USA (12). Other countries included China (10), UK (3), Italy (2) and Saudi Arabia (2). Four studies had data from across multiple countries (Fujii 2021 (Fujii et al., 2021); Jovančević & Milićević 2020 (Jovančević & Milićević, 2020); Lee 2020 (Lee et al., 2020); van den Broek‐Altenburg (van den Broek‐Altenburg & Atherly, 2021). Full details of included studies can be found in Table 3.
There was a total of 199,376 participants across the 56 studies, ranging from 71,851 (Hsing 2021 (Hsing Julianna et al., 2021) to 212 (Pal et al. 2020 (Pal et al., 2020). The vast majority of studies had samples from the general public, with eight of the studies focusing on specific samples. These included; pregnant women (Wang 2021 (Wang et al., 2021); Apanga 2021 (Apanga & Kumbeni, 2021), factory workers (Pan 2020 (Pan et al., 2020), people with type 1 diabetes (Pal et al., 2020), student pharmacists (Li 2021 (Li et al., 2021), visitors to a medical centre (Kebede 2020 (Kebede et al., 2020), and university students (Graupensperger 2021 (Graupensperger et al., 2021); Barrett 2021 (Barrett & Cheung, 2021).
All studies included participants over 18 years old. Reporting of age varied between studies, some providing mean age of participants, others providing percentage of age ranges and some not reporting age (Callaghan 2021 (Callaghan et al., 2021); Fujii 2021). For those studies that did report on age of participants, the average age was 35.5 years.
Reported outcome: Studies varied in their approaches to measuring hand washing. Measures ranged from scales (e.g. Hsing 2021) to single items (e.g., Are you regularly washing you hands with soap and water?, Pal et al., 2020). Handwashing was defined as using soap and water or using hand sanitizer within the included studies. Some studies measured adherence to specific hand washing guidance within the country of origin (e.g., Al‐Shammary 2021 (Al‐Shammary et al., 2021), some measured the frequency of handwashing (e.g., washed hands with soap or used hand sanitizer several times a day, Bruine de Bruin et al. 2020 (Bruine de Bruin et al., 2020), or measured handwashing following various activities (e.g. I have washed my hands every time I came into contact with objects or external environments, Trifiletti 2021 (Trifiletti et al., 2021).
Determinants: There were 18 determinants analysed across the 56 studies, including worry, perceived risk, knowledge, perceived barriers, and beliefs and motivation. Multiple determinants were reported within individual studies, for example Rui et al., 2021 reported on perceived self‐efficacy, perceived risk, perceived susceptibility, and knowledge. The most commonly reported determinant was perceived susceptibility of COVID‐19 (n = 25), followed by perceived severity of COVID‐19 (n = 21). Perceived effectiveness of handwashing (n = 3), fear of COVID (n = 3) and COVID‐related anxiety (n = 3) were the least reported determinants.
Following assessment of the data, 28 studies were deemed suitable to include in the meta‐analysis. These 28 studies reported on 12 determinants. A total of 34 studies were included in the narrative synthesis, reporting six determinants. Studies were considered not suitable for meta‐analysis due to not reporting unadjusted data. Given the multiple determinants reported in individual studies, 6 studies were included in both the narrative synthesis and meta‐analysis (Al‐Sejari 2021 (Al‐Sejari Maha and Al‐Ma'Seb Hend, 2021); Al‐Shammary 2021; Apanga 2021; Barrett 2021; Kowalski 2020b (Kowalski et al., 2020b); Norman 2020 (Norman et al., 2020).
6.1.3. Excluded studies
A total of 87 studies were excluded from this review, a list of which can found in the references.
6.2. Risk of bias in included studies
A detailed summary of risk of bias for the 56 included studies is shown in Table 4. All 56 studies were utilised a cross sectional design and were rated using the JBI tool for cross‐sectional studies (The Joanna Briggs Institute, 2017, 2020). Studies were scored based on the number of items answered ‘yes’, with >70% yes = Low Risk of Bias, 50%–70% yes = Unclear Risk of Bias, and <50% ‘Yes’ = High Risk of Bias.
Table 4.
Quality appraisal of included studies.
| Study | Were the criteria for inclusion in the sample clearly defined and adhered to? | Was the sample included in the study representative of the population of interest? | Were the determinants measured in a valid and reliable way? | Were the behaviours measured in a valid and reliable way? | Were confounding factors/covariates identified? | Were strategies to deal with confounding factors/covariates stated and used? | Was appropriate statistical analysis used? | Is there evidence of selective reporting? | Overall Quality Rating |
|---|---|---|---|---|---|---|---|---|---|
| Al‐Sejari (2021) | Yes | No | Yes—scale | No—single item | Yes | Unclear | Yes | No | Low risk of bias |
| Al‐Shammary (2021) | Yes | Unclear | Yes—single item | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Al‐Wutayd (2021) | No | Yes | Yes—single item | Yes—single item | Unclear | Yes | Yes | No | Unclear risk of bias |
| Apanga (2021) | Yes | Unclear | Yes—single item | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Barrett (2021) | Yes | Unclear | Unclear | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Bogg (2020) | Yes | Unclear | Yes—scale | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Bruine de Bruin et al. (2020) | Yes | Yes | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Bruine de Bruin et al. (2020) | No | Yes | Yes—scale | Unclear | Unclear | Unclear | Yes | No | High risk of bias |
| Callaghan (2021) | Yes | Yes | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Cowling et al. (2020) | Yes | No | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Dixon et al. (2022) | Yes | Yes | Yes—scale | Yes—scale | Yes | Yes | Yes | Yes | Low risk of bias |
| Dwipayanti (2021) | Unclear | No | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Unclear risk of bias |
| Fujii (2021) | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | No | Unclear risk of bias |
| Graupensperger (2021) | No | Unclear | Yes—scale | Yes—single item | No | No | Yes | No | High risk of bias |
| Haliwa et al. (2020) | No | Yes | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Hsing (2021) | No | Yes | No—scale | Yes—scale | Yes | Yes | Yes | No | Unclear risk of bias |
| Iqbal (2021) | No | Unclear | Yes—single item | Yes—single item | Yes | No | Unclear | No | High risk of bias |
| Jang et al. (2020) | Yes | Yes | Yes—scale | Unclear | Yes | Yes | Yes | No | Low risk of bias |
| Jimenez (2020) | Yes | No | Yes—scale | Yes—scale | Yes | No | Unclear | No | Low risk of bias |
| Jovančević & Milićević (2020) | No | No | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Unclear risk of bias |
| Kebede (2020) | No | No | Unclear | Unclear | Unclear | Unclear | Yes | No | High risk of bias |
| Kowalski (2020a) Study 1 | Yes | Unclear | Yes—scale | Yes—single item | Yes | Yes | Yes | Yes | Low risk of bias |
| Kowalski (2020b) Study 2 | Yes | Unclear | Yes—scale | Yes—single item | Yes | Yes | Yes | Yes | Low risk of bias |
| Lahiri (2021) | Yes | No | No—scale | Unclear | Yes | Unclear | Yes | Yes | High risk of bias |
| Lao et al. (2023) | Yes | Unclear | Yes—scale | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Lee (2020) | Yes | No | Yes—single item | Unclear | Unclear | Unclear | Yes | No | High risk of bias |
| Lee (2021) | Yes | Yes | Yes—scale | Yes—scale | Yes | Yes | Yes | Yes | Unclear risk of bias |
| Li (2021) | Unclear | Unclear | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Unclear risk of bias |
| Matkovic et al. (2021) | No | Unclear | Yes—scale | Yes—scale | No | Unclear | Yes | No | Unclear risk of bias |
| Milman (2020) | Yes | No | Yes—scale | Unclear | Yes | Yes | Yes | Yes | Unclear risk of bias |
| Mousavi et al. (2022) | Yes | No | Yes—single item | Unclear | Yes | Yes | Yes | Yes | Unclear risk of bias |
| Nelson (2021) | Yes | No | Unclear | Yes—scale | Yes | No | Yes | No | Unclear risk of bias |
| Norman (2020) | Yes | Yes | Unclear | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Owhonda (2021) | No | Yes | No—scale | Yes—scale | Yes | Yes | Yes | Unclear | Unclear risk of bias |
| Lee et al. (2021) | Yes | Yes | Yes—scale | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Pal et al. (2020) | Yes | Unclear | Unclear | Unclear | Yes | Yes | Yes | No | Unclear risk of bias |
| Pan (2020) | No | Yes | Yes—single item | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Prete (2020) | No | No | Yes—scale | Yes—single item | Yes | No | Yes | No | Unclear risk of bias |
| Qian (2020) | Yes | Yes | Unclear | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Rattay (2021) | Unclear | Yes | Yes—single item | Unclear | Yes | Yes | Yes | No | Unclear risk of bias |
| Rui (2021) Study 1 | Yes | Unclear | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Rui (2021) Study 2 | Yes | Unclear | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Rui (2021) Study 3 | Yes | Unclear | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Rui (2021) Study 4 | Yes | Unclear | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Rui (2021) Study 5 | Yes | Unclear | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Rui (2021) Study 6 | Yes | No | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Sengeh (2020) | Yes | Unclear | No—scale | No—scale | Yes | No | Yes | Yes | High risk of bias |
| Sharma | Yes | No | Unclear | Yes—Scale | Yes | Yes | Yes | No | Unclear risk of bias |
| Shook (2020) | No | No | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Unclear risk of bias |
| Si et al. (2021) | Yes | Yes | Yes—scale | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Souliotis (2021) | Yes | Yes | Unclear | Unclear | Yes | Yes | Yes | No | Unclear risk of bias |
| Stojanovic (2021) | Yes | No | Yes—scale | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
| Trifiletti (2021) | No | No | Yes—scale | Yes—single item | Yes | Yes | Yes | No | Unclear risk of bias |
| van den Broek‐Altenburg (2021) | Yes | Yes | Yes—scale | Yes—scale | Yes | Yes | Yes | No | Low risk of bias |
| Wang (2021) | Yes | Yes | Yes—scale | Yes—scale | Yes | No | Yes | No | Low risk of bias |
| Zewude et al. (2021) | Yes | Unclear | Yes—single item | Yes—single item | Yes | Yes | Yes | No | Low risk of bias |
Overall, 30 studies were rated low risk of bias, 18 unclear risk of bias, and 8 were rated as high risk bias. Those studies deemed high risk of risk predominately received this rating due to lack of detail on measurement of handwashing and determinants (Bruine 2020; Kebede 2020) or the measure used was deemed not to be a reliable or valid measure (Sengeh 2020 (Sengeh et al., 2020). There was also poor reporting of study design and methodology (Graupensperger 2021; Iqbal 2021 (Iqbal & Younas, 2021); Kebede 2020; Lahiri 2021 (Lahiri et al., 2021); Lee 2020) and lack of sample demographics, making it difficult to determine representativeness (Graupensperger 2021; Iqbal 2021). In three studies it was evident that the sample was not representative (Kebede 2020; Lahiri 2021; Lee 2020).
6.3. Data and analysis
6.3.1. Meta‐analysis
In total we analysed 52 effect sizes across 6 determinant groups, and included 28 studies. The summary effect of each determinant group can be seen in the Summary of findings table 1 along with 95% confidence intervals (CIs) and heterogeneity statistics. As shown in the summary of findings table, our analyses indicate significant relationships between knowledge about behaviour and disease, social norms, COVID‐related worry and anxiety and handwashing behaviour. There is no significant relationship observed between perceived severity and handwashing or between perceived susceptibility and handwashing. All data is reported in Tables 5, 6, 7.
Table 5.
Handwashing and anxiety and worry.
| Study | n | Description of determinant | Effect size | CI | ||
|---|---|---|---|---|---|---|
| Anxiety | ||||||
| Milman (2020) | 408 | COVID anxiety | Unadjusted | r | 0.32 | |
| Kowalski (2020a) S1 | 507 | Coronavirus‐related anxiety | Unadjusted | r | 0.42 | |
| Kowalski (2020b) S2 | 840 | Coronavirus‐related anxiety | Unadjusted | r | 0.18 | |
| Worry | ||||||
| Prete (2020) | 618 | Worry | Unadjusted | d | 1.02 | |
| Jang et al. (2020) | 1004 | Worried about disease | Unadjusted | OR | 4.25 | (3.10 −5.85) |
| Jimenez (2020) | 290 | Worry | Unadjusted | OR | 0.16 | (0.09, 0.23) |
| Al‐Sejari (2021) | 1413 | Worry about illness | Unadjusted | r | 0.239 | |
Abbreviation: CI, confidence interval.
Table 6.
Handwashing and cognition.
| Study | n | Description of determinants | Effect size | CI | ||
|---|---|---|---|---|---|---|
| Perceived control | ||||||
| Lao et al. (2023) | 229 | Action control | Unadjusted | r | 0.28 | |
| Bogg (2020) | 500 | Perceived control | Unadjusted | r | 0.22 | |
| Trifiletti (2021) | 248 | Perceived behavioural control of HW | Unadjusted | r | 0.06 | |
| Norman (2020) | 477 | Autonomy | Unadjusted | r | 0.17 | |
| Attitudes towards behaviour | ||||||
| Trifiletti (2021) | 248 | Attitude towards handwashing | Unadjusted | r | 0.22 | |
| Barrett (2021) | 292 | Attitudes | Unadjusted | r | 0.26 | (0.15, 0.37) |
| Bogg (2020) | 500 | Attitudes | Unadjusted | r | 0.29 | |
| Norman (2020) | 477 | Attitude towards handwashing | Unadjusted | r | 0.37 | |
| Norman (2020) | 477 | Injunctive norms | Unadjusted | r | 0.30 | |
| Matkovic et al. (2021) | 344 | Attitudes towards handwashing | Unadjusted | r | 0.41 | |
| Al‐Wutayd (2021) | 1323 | Attitudes towards handwashing behaviour | Unadjusted | t | 0.417 | |
| Perceived self‐efficacy | ||||||
| Lee et al. (2021) | Perceived self‐efficacy | Unadjusted | OR | 1.19 | (0.88, 1.61) | |
| Kebede (2020) | 247 | Efficacy—self‐control | Unadjusted | OR | 3.54 | (1.9, 6.57) |
| Barrett (2021) | 293 | Self‐efficacy—infection avoidance | Unadjusted | r | −0.08 | (−0.2, 0.04) |
| Barrett (2021) | 293 | Self‐efficacy—hand hygiene | Unadjusted | r | 0.38 | (0.27, 0.48) |
| Bogg (2020) | 500 | Self‐efficacy | Unadjusted | r | 0.28 | |
| Norman (2020) | 477 | Capacity | Unadjusted | r | 0.33 | |
| Lao et al. (2023) | 229 | Action self‐efficacy | Unadjusted | r | 0.22 | |
| Perceived effectiveness of behaviour | ||||||
| Lee et al. (2021) | 897 | Perceived efficacy of anti‐COVID strategies | Unadjusted | OR | 2.66 | (2.02, 3.51) |
| Al‐Shammary (2021) | 400 | Perceived effectiveness of preventive measures | Unadjusted | SMD | 0.355 | |
| Sharma et al. (2021) | 713 | Advantages of behaviour | Unadjusted | SMD | 0.23 | |
| Perceived risk | ||||||
| Barrett (2021) | 293 | Risk perception | Unadjusted | r | 0.2 | (0.1, −0.29) |
| Bogg (2020) | 500 | Perceived risk of exposure | Unadjusted | r | 0.05 | |
| Bogg (2020) | 500 | Perceived risk of health consequence | Unadjusted | r | 0.17 | |
| Trifiletti (2021) | 248 | risk perception | Unadjusted | r | 0.26 | |
| Lao et al. (2023) | 229 | Risk perception | Unadjusted | r | 0.16 | |
| Al‐Shammary (2021) | 400 | Risk perception | Unadjusted | Mean (SD) | 6.9 (3.2), 5.61 (2.21) | |
| Perceived severity | ||||||
| Bruine & Bennett (2020) | 6684 | Risk of dying if infected | Unadjusted | r | 0.01 | |
| Bruine de Bruin et al. (2020) | 5517 | Risk of Dying if infected | Unadjusted | r | 0 | |
| Lee et al. (2021) | 897 | Likelihood of requiring ICU admission with COVID | Unadjusted | OR | 1.05 | (0.81, 1.37) |
| Lee et al. (2021) | 897 | Perceived disease severity | Unadjusted | OR | 0.75 | (0.58, 0.98) |
| Perceived susceptibility | ||||||
| Haliwa et al. (2020) | 353 | Perceived likelihood of contracting COVID‐19 | Unadjusted | r | −0.02 | |
| Bruine (2020) | 5517 | Risk of getting infected | Unadjusted | r | 0.03 | |
| Si et al. (2021) | 1019 | Perceived infectability | Unadjusted | r | −0.1 | |
| Bruine de Bruin et al. (2020) | 6684 | Perceived susceptibility | Unadjusted | r | 0.11 | |
| Norman (2020) | 477 | Perceived susceptibility | Unadjusted | r | 0.18 | |
| Social norms | ||||||
| Bogg (2020) | 500 | Perceived norms | Unadjusted | r | 0.29 | |
| Graupensperger (2021) | 539 | Perceived peer norms | Unadjusted | r | 0.49 | |
| Graupensperger (2021) | 539 | Perceived peer norms | Unadjusted | r | 0.47 | |
| Trifiletti (2021) | 248 | Social norms about handwashing | Unadjusted | r | 0.13 | |
| Norman (2020) | 477 | Injunctive norms | Unadjusted | r | 0.23 | |
| Norman (2020) | 477 | Descriptive norms | Unadjusted | r | 0.13 | |
Abbreviation: CI, confidence interval.
Table 7.
Handwashing and knowledge.
| Study | n | Description of determinants | Effect size | CI | ||
|---|---|---|---|---|---|---|
| Knowledge of behaviour | ||||||
| Barrett (2021) | 290 | Hand hygiene effectiveness knowledge | Unadjusted | r | −0.07 | (0.77, 0.95) |
| Al‐Wutayd (2021) | 1323 | Knowledge of handwashing | Unadjusted | r | 0.375 | (0.33, 0.42) |
| Apanga (2021) | 527 | Knowledge of behaviours to prevent COVID infection | Unadjusted | r | 0.435 | (0.36, 0.50) |
| Knowledge of disease | ||||||
| Barrett (2021) | 287 | Knowledge | Unadjusted | r | 0.1 | |
| Iqbal (2021) | 1789 | COVID knowledge | Unadjusted | r | 0.418 | (0.37, 0.46) |
| Pal et al. (2020) | 212 | Knowledge of disease | Unadjusted | OR | 1.07 | (0.97, 1.18) |
| Sengeh (2020) | 1253 | Knowledge about COVID (low vs high) | Unadjusted | OR | 6.33 | (2.98, 13.45) |
| Apanga (2021) | 527 | Knowledge about COVID symptoms and transmission | Unadjusted | r | 0.279 | |
| Owhonda (2022) | 1294 | Knowledge about COVID (poor vs good) | Unadjusted | OR | 1.16 | (1.1, 1.24) |
Below we present forest plots (Figures 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13) for each determinant and interpret these findings further.
Figure 2.
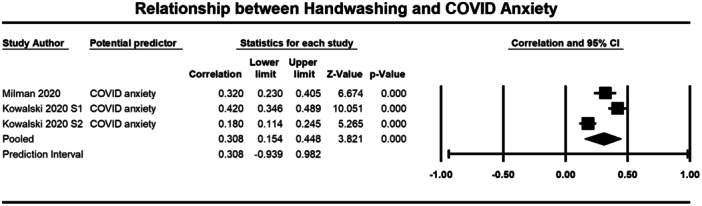
Relationship between handwashing and COVID anxiety. CI, confidence interval.
Figure 3.
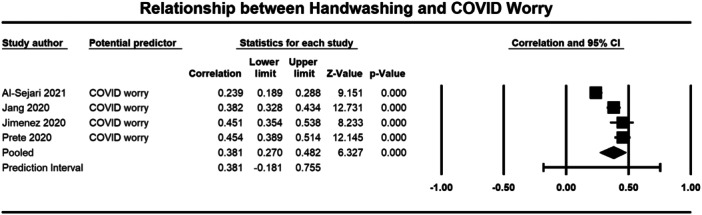
Relationship between handwashing and COVID worry. CI, confidence interval.
Figure 4.
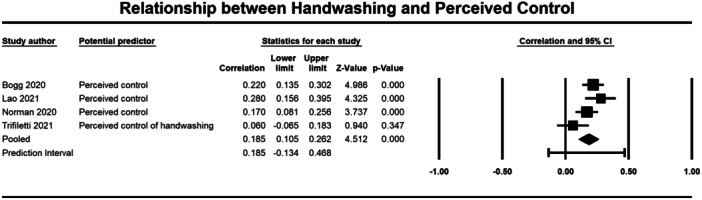
Relationship between handwashing and percieved control. CI, confidence interval.
Figure 5.
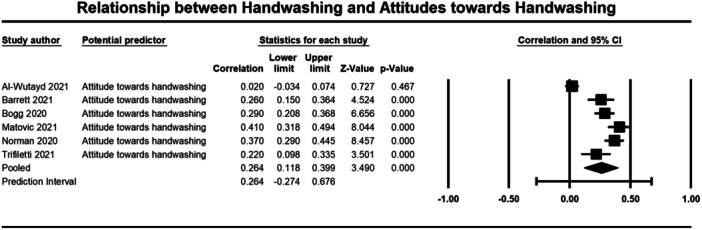
Relationship between handwashing and attitude towards handwashing. CI, confidence interval.
Figure 6.
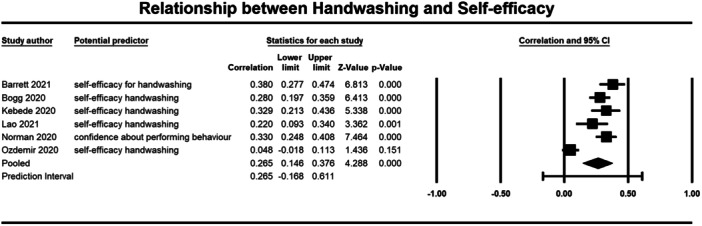
Relationship between handwashing and self‐efficacy. CI, confidence interval.
Figure 7.
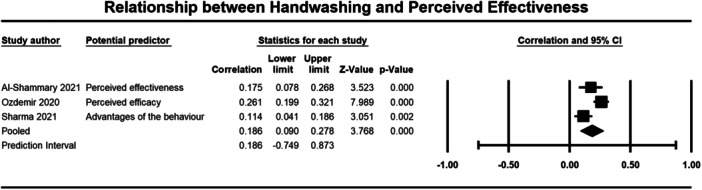
Relationship between handwashing and perceieved effectiveness. CI, confidence interval.
Figure 8.
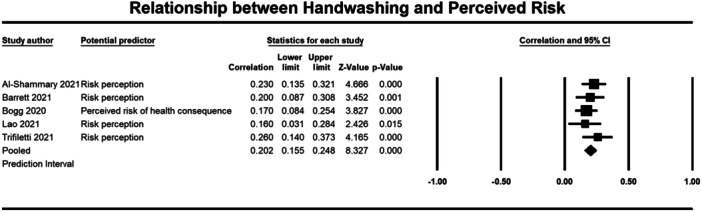
Relationship between handwashing and perceieved risk. CI, confidence interval.
Figure 9.
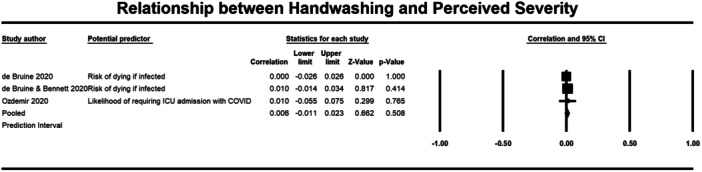
Relationship between handwashing and perceived severity. CI, confidence interval.
Figure 10.
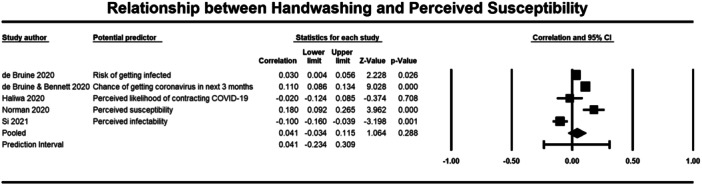
Relationship between handwashing and perceived susceptibility. CI, confidence interval.
Figure 11.
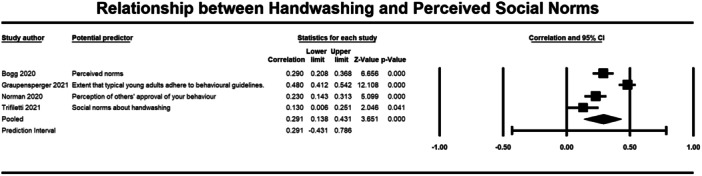
Relationship between handwashing and social norms. CI, confidence interval.
Figure 12.
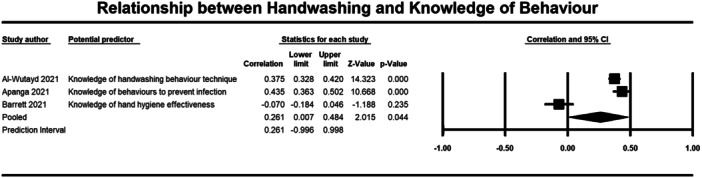
Relationship between handwashing and knowledge of behaviour. CI, confidence interval.
Figure 13.
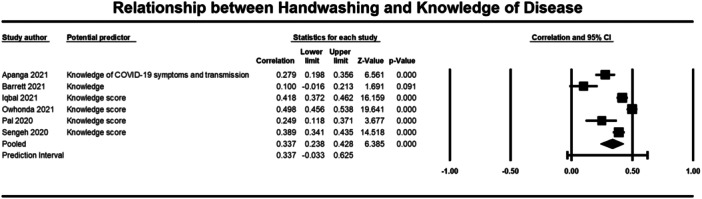
Relationship between handwashing and knowledge of disease. CI, confidence interval.
Emotions
Three studies were included in the meta‐analysis that examined the relationship between COVID‐related anxiety and handwashing behaviour (1755 participants) (Kowalski 2020a; Kowalski 2020b; Milman 2020 (Milman, 2020). The average correlation between COVID related anxiety and handwashing across the three studies was moderate (r = 0.308, 95% CI = 0.154, 0.448), but was significant (p ≤ 0.001) (Figure 2). There was significant heterogeneity across studies (τ² = 0.019; Q = 22.981, df = 2; p ≤ 0.001; I² = 91%). There were similar results for COVID‐related worry (3325 participants). With a moderate and significant correlation observed across the four included studies (r = 0.381, 95% CI = 0.270, 0.482, p ≤ 0.001) (Al‐Sejari 2021; Jang et al. 2020 (Jang et al., 2020); Jimenez 2020 (Jimenez et al., 2020); Prete 2020 (Prete et al., 2020) (Figure 3). Again, there was significant heterogeneity across studies (τ² = 0.014; Q = 35.762, df = 3; p ≤ 0.001; I² = 92%). These results indicate that experiencing more COVID‐related anxiety and worry was significantly correlated to handwashing behaviour.
Cognitions
The meta‐analysis included four studies which examined the relationship between perceived control (1454 participants) and handwashing (Bogg 2020; Lao et al. 2023; Norman 2020; Trifiletti 2021). Results showed a weak but significant relationship (r = 0.185, 95% CI = 0.105, 0.262, p ≤ 0.001), with no significant heterogeneity across studies (τ² = 0.004; Q = 7.013, df = 3, p = 0.071; I² = 57%) (Figure 4).
A weak but significant (p ≤ 0.001) relationship was also observed between attitudes (3184 participants) (r = 0.264, 95% CI, 0.118, 0.399), self‐efficacy (2643 participants) (r = 0.265, 95% CI = 0.146, 0.376), perceived effectiveness (2010 participants) (r = 0.186, 95% CI = 0.090, 0.278), perceived risk (1670 participants) (r = 0.202, 95% CI = 0.155, 0.248), and social norms (1764 participants) (r = 0.291, 95% CI = 0.138, 0.431) and handwashing behaviour (Figures 5, 6, 7, 8, 9). Heterogeneity was significant across all these determinants. For the meta‐analysis of attitudes, Norman (2020) provided two effect sizes: one for experiential attitudes (r = 0.44) and one for instrumental attitudes (r = 0.30). We used an average of these two estimates in the meta‐analysis. For the meta‐analysis of perceived effectiveness, Al‐Shammary (2021) provided four effect sizes for the relationship between handwashing and perceived effectiveness of preventive measures in the marketplace (r = 0.26), in the workplace (r = 0.17), in healthcare settings (r = 0.10), and in travel settings (r = 0.16). We used the average of these estimates in the meta‐analysis. In the case of social norms, Graupensperger (2021) provided correlations between social norms and handwashing with soap and water (r = 0.49) and also using hand sanitiser (r = 0.47). We used the average of these two correlations in the meta‐analysis.
Both perceived severity (13,098 participants) and susceptibility (14,050 participants) had a non‐significant correlation with handwashing behaviour (r = 0.006, 95% CI = −0.011, 0.023; r = 0.041, 95% CI = −0.034 to 0.115, respectively) (Figures 10 and 11).
Knowledge
Seven studies were included in the meta‐analysis that examined the relationship between knowledge of behaviour (2140 participants) and disease (4893 participants) and handwashing behaviour (Al‐Wutayd 2021; Apanga 2021; Barrett 2021; Iqbal 2021; Owhonda 2022; Pal et al., 2020; Sengeh 2020). For knowledge of behaviour the average correlation with handwashing was small (r = 0.261, 95% CI = 0.007, 0.484, p = 0.044) (Figure 12). To conduct this meta‐analysis, we averaged the correlations provided by Al‐Wutyad (2021) and we averaged the correlations provided by Apanga (2021). Al‐Wutyad (2021) had provided correlations between handwashing and knowledge about recommendations around handwashing that comprised knowledge about: following the correct technique (r = 0.08), duration of handwashing (r = 0.21), handwashing after visiting public places (r = 0.88), and handwashing after touching high touch surfaces outside (r = 0.33). Apanga (2021) provided correlations between handwashing and knowledge about behaviours that reduce COVID‐19 infection, including avoiding touching the T‐zone (r = 0.46) and avoiding crowded places (r = 0.41).
For knowledge of disease, a moderate average correlation was found with handwashing across the studies (r = 0.337, 95% CI = 0.238, 0.428, p ≤ 0.001) (Figure 13). Apanga (2021) provided correlations between handwashing and knowledge of: COVID symptoms (r = 0.29), transmission via respiratory droplets (r = 0.09), and transmission via touching contaminated surfaces (r = 0.45). We used the average correlation from this study in the meta‐analysis.
There was significant heterogeneity for both knowledge of behaviour and disease (τ² = 0.051; Q = 60.292, df = 2; p ≤ 0.001; I² = 97%; τ² = 0.016, Q = 65.716, df = 5; p = <0.001; I² = 92%, respectively). These results indicate that having more knowledge about behaviours and COVID was significantly correlated to handwashing behaviour.
6.3.2. Narrative synthesis of results
A total of 34 studies were included in the narrative synthesis. Details of the individual studies that contribute to this synthesis are show in Table 3.
Barriers influencing handwashing behaviour
Four studies (Barrett 2021; Dwipayanti 2021 (Dwipayanti Ni Made et al., 2021); Hsing 2021; Li 2021) examined the relationship between perceived barriers and handwashing behaviour Table 8. One study (Hsing 2021) recruited samples from four different counties and found generally weak associations between barriers and using either hand sanitiser or hand soap. In participants living in one of these locations (Hong Kong), a larger effect was observed. However, it should be noted that the sample size in this location was much smaller (around 1200 participants) in comparison to the other countries where participants were recruited from the USA, Mexico and Taiwan, which had sample sizes ranging from approximately 3000 to 640,000). Weak associations were also found in the studies of Dwipayanti 2021 and Li 2021.
Table 8.
Handwashing and perceived barriers.
| Study ID | Determinant | Effect size (CI) | n |
|---|---|---|---|
| Hsing (2021) | Perceived barriers to using hand sanitiser (USA) | AOR: 0.88 (0.74–1.03) | 3070 |
| Perceived barriers to using hand sanitiser (Mexico) | AOR: 1.01 (0.88–1.15) | 3946 | |
| Perceived barriers to using hand sanitiser (Hong Kong) | AOR: 1.14 (0.74–1.77) | 1201 | |
| Perceived barriers to using hand sanitiser (Taiwan) | AOR: 0.86 (0.79–0.94) | 63,634 | |
| Perceived barriers to using hand soap (USA) | AOR: 0.73 (0.49–1.07) | 3070 | |
| Perceived barriers to using hand soap (Mexico) | AOR: 1.35 (0.98–1.87) | 3946 | |
| Perceived barriers to using hand soap (Hong Kong) | AOR: 7.59 (1.88–53.9) | 1201 | |
| Perceived barriers to using hand soap (Taiwan) | AOR: 1.01 (0.81–1.27) | 63,634 | |
| Dwipayanti (2021) | Perceived barriers | AOR: 1.3 (0.9–1.9) | |
| Li et al. (2021) | Perceived barriers | Adjusted regression coefficient: 0.00 (−0.03 to 0.02) | 326 |
| Barrett (2021) | Perceived barrier (focused on time) | r = 0.49 (0.4–0.58) | 293 |
| ORa = 7.68 (4.87–13.23) |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Converted to OR to allow comparison with other studies in the table.
COVID‐19‐related fear or worry
Weak, but positive associations were reported in three studies (Al‐Shammary 2021; Jovančević & Milićević 2020; Rattay 2021 (Petra et al., 2021) which examined the role of fear on handwashing, supporting the contention that these behaviours may be driven or motivated by the level of COVID‐19 related fear (Table 9). Worry or concern about COVID‐19 was also consistently found to be associated with handwashing behaviours in five of the included studies (Al‐Sejari 2021; Callaghan 2021; Rattay 2021; Shook 2020 (Shook Natalie et al., 2020); Nelson 2021 (Nelson Tracy et al., 2021), but again, the reported effect sizes for these associations were weak (Table 10). One of these studies (Nelson 2021) did not report any differences based on whether handwashing behaviour were being carried out in or outside of work contexts.
Table 9.
Handwashing and fear.
| Study ID | Determinant | Effect size (CI) | n |
|---|---|---|---|
| Rattay (2021) | Fear | AOR: 1.05 for women, 1.03 for men | 13,430 women, 13,037 men |
| Jovancevic & Milićević (2020) |
Fear of others being infected Fear of self‐being infected |
Multiple regression coefficients: 0.02 in Latin America 0.13 in Serbia 0.23 in Latin America 0.14 in Serbia |
412 Latin America; 120 Sebia |
| Al‐Shammary (2021) | Fear of COVID‐19 |
Level of fear was higher in those who engaged in hand hygiene procedures: M (SD) yes = 7.42 (2.91), no = 6.59 (3.08) Cohen's d = 0.28 OR* = 1.66 |
400 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
p < 0.05.
Table 10.
Handwashing and worry and concern.
| Study ID | Determinant | Effect size (CI) | n |
|---|---|---|---|
| Rattay (2021) | Worries | AOR: 1.14 for women, 1.14 for men | 13,430 women; 13,037 men |
| Callaghan (2021) | COVID worry | AOR: 1.28 (1.07–1.52) | 5009 |
| Al‐Sejari (2021) | Concern about pain |
r = 0.148 OR* = 1.72 |
1413 |
| Shook (2020) | COVID‐19 concern | Multiple regression coefficient: 0.13 | 1019 |
| Nelson (2021) |
Level of concern about contracting COVID‐19 Level of concern about exposing others to COVID‐19 |
r = 0.14 (washing hands at work), OR* = 1.67 r = 0.17 (washing hands outside of work), OR* = 1.87 r = 0.10 (washing hands at work), OR* = 1.44 r = 0.13 (washing hands outside of work), OR* = 1.61 |
508 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
p < 0.05.
Perceived susceptibility to COVID‐19 and severity of COVID‐19
Findings related to the influence of perceived susceptibility on handwashing or hand sanitising behaviours were mixed across the 14 included studies (Cowling et al., 2020 (Cowling et al., 2020); Dwipayanti 2021; Fujii 2021; Hsing 2021; Lahiri 2021; Lee 2020; Lee et al. (2021); Mousavi et al. 2022 (Mousavi et al. 2022); Pan 2020; Rui et al., 2021; (Rui et al., 2021); Qian 2020 (Mengcen et al., 2020); Rattay 2021; Shook 2020; Zewude et al. 2021). While the majority of these reported weak effect sizes, the direction of these effects varied, with both positive and negative associations being observed (Table 11). Two studies (Dwipayanti 2021; Mousavi et al., 2022) which recruited participants in Indonesia and Afghanistan, respectively, did report larger associations between variables. One of these (Mousavi et al., 2022), differed from other studies in that it examined the likelihood of family members getting infected, and included a relatively small sample size. In comparison to other evidence included in the analysis, both of these studies had larger confidence intervals around the reported odds ratios.
Table 11.
Handwashing and perceived susceptibility.
| Study ID | Determinant | Effect size (CI) | n |
|---|---|---|---|
| Shook (2020) | Perceived infectability | Multiple regression coefficient: −0.04 | 1019 |
| Lee (2020) | Perceived susceptibility | Multiple regression coefficient: 0.03 (−0.01 to 0.08) | 973 |
| Lee et al. (2021) | Perceived susceptibility | Multiple regression coefficient: 0.02 | 990 |
| Hsing (2021) |
Perceived susceptibility of infection: USA Mexico Hong Kong Taiwan |
AOR: 1.12 (0.95–1.33) AOR: 1.23 (1.06–1.42) AOR: 1.44 (1.11–1.87) AOR: 1.08 (1.04–1.12) |
3070 3946 1201 63,634 |
| Rattay (2021) | Perceived susceptibility | AOR: 0.97 (women), 0.99 (men) | 13,430 women; 13,037 men |
| Dwipayanti (2021) | Perceived susceptibility | AOR: 6.34 (2.28–17.62) | 896 |
| Pan (2020) | Perceived risk of contracting COVID‐19 | AOR: 0.58 (0.50–0.68) | 3035 |
| Cowling et al. (2020) |
Those with thought they were likely to contract the virus Those with thought they were unlikely to contract the virus Those with thought they were very likely to contract the virus Those with thought they were very unlikely to contract the virus Those with thought they would never contract the virus |
AORs: Handwashing after returning home: 1.12 (0.91–1.38) Handwashing after sneezing: 0.93 (0.80–1.09) Handwashing after touching common objects: 1.01 (0.87–1.18) Use of liquid soap: 0.96 (0.82–1.14) Handwashing after returning home: 0.82 (0.71–0.95) Handwashing after sneezing: 0.91 (0.81–11.03) Handwashing after touching common objects: 0.95 (0.85–1.06) Use of liquid soap: 0.93 (0.82–1.05) Handwashing after returning home: 0.86 (0.45–1.63) Handwashing after sneezing: 1.15 (0.68–1.94) Handwashing after touching common objects: 1.67 (1.04–2.67) Use of liquid soap: 1.47 (0.79–2.74) Handwashing after returning home: 0.87 (0.69–1.10) Handwashing after sneezing: 0.99 (0.81–1.20) Handwashing after touching common objects: 0.94 (0.79–1.13) Use of liquid soap: 0.98 (0.81–1.18) Handwashing after returning home: 0.88 (0.71–1.09) Handwashing after sneezing: 1.06 (0.89–1.27) Handwashing after touching common objects: 0.99 (0.84–1.16) Use of liquid soap: 1.00 (0.83–1.19) |
12,965 |
| Mousavi et al. (2022) | High likelihood of family getting infected | OR = 3.63 (1.89–6.98) | 64 |
| Lahiri (2021) |
Higher vulnerability of the participants to COVID‐19, with progression of pandemic (time) Higher vulnerability of a respondent to COVID‐19 in comparison to others Higher vulnerability of the participants to COVID‐19, due to current residence area Higher vulnerability of the participants to COVID‐19, with progression of pandemic (time) Higher vulnerability of a respondent to COVID‐19 in comparison to others Higher vulnerability of the participants to COVID‐19, due to current residence area |
Adjusted prevalence ratios: Frequently washing hands with soap and water 1.01 (1.00–1.02) 1.03 (1.01–1.05) 1.00 (0.97–1.02) Frequently cleaning hands with sanitizer 0.92 (0.91–0.94) 1.21 (1.14–1.28) 1.13 (1.10–1.16) |
2615 2617 |
| Fujii (2021) |
Perceived susceptibility China Italy Japan Korea UK USA |
AORs: 0.81 (0.71–0.91) 0.99 (0.84–1.18) 0.98 (0.90–1.09) 0.77 (0.66–0.90) 1.05 (0.89–1.27) 0.91 (0.80–1.03) |
994 1020 981 918 994 1038 |
| Zewude et al. (2021) | Think can be infected by COVID‐19 | AOR: 0.68 (0.35–1.32) | 379 |
| Qian (2020) | Likelihood of contracting virus | AOR: 0.8 (0.7–1.0) | 1011 |
| Rui (2021) Study 5 | Perceived susceptibility | AOR 0.92 (0.73–1.16) | 329 |
| Rui (2021) Study 4 | Perceived susceptibility | AOR 0.86 (0.69–1.07) | 343 |
| Rui (2021) Study 3 | Perceived susceptibility | AOR 0.85 (0.69–1.05) | 315 |
| Rui (2021) Study 2 | Perceived susceptibility | AOR 0.93 (0.73–1.19) | 319 |
| Rui (2021) Study 1 | Perceived susceptibility | AOR 1.01 (0.79–1.3) | 321 |
| Rui (2021) Study 6 | Perceived susceptibility | AOR 0.92 (0.67–1.25) | 315 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Similar findings were also observed for perceived severity of COVID‐19, with 18 studies (Dwipayanti 2021; Fujii 2021; Hsing 2021; Lahiri 2021; Lee 2020; Lee et al. 2021; Mousavi et al., 2022; Pan 2020; Qian 2020; Rattay 2021; Rui et al., 2021; Zewude et al. 2021) finding associations that were in both directions but which had weak effect sizes (Table 12).
Table 12.
Handwashing and perceived severity.
| Study ID | Determinant | Effect size (CI) | n |
|---|---|---|---|
| Lee (2020) | Perceived severity | Multiple regression coefficient: 0.08 (0.03–0.13) | 973 |
| Lee et al. (2021) | Perceived susceptibility | Multiple regression coefficient: 0.05 | 990 |
| Hsing (2021) |
Perceived severity of COVID‐19: USA Mexico Hong Kong Taiwan |
AOR: 0.33 (1.09–1.61) AOR: 1.06 (0.91–1.22) AOR: 1.22 (0.90–1.65) AOR: 1.24 (1.20–1.29) |
3070 3946 1201 63,634 |
| Rattay (2021) | Perceived severity | AOR: 1.17 (women), 1.14 (men) | 13,430 women; 13,037 men |
| Dwipayanti (2021) | Perceived severity—fatal | AOR: 1.06 (0.38–2.96) | 896 |
| Pan (2020) | Perceived severity of COVID‐19 | AOR: 1.03 (0.99–1.07) | 3035 |
| Cowling et al. (2020) | AORs: | 12,965 | |
| Mousavi et al. (2022) | Low likelihood of survival if infected | OR = 2.01 (1.09–3.69) | 64 |
| Lahiri (2021) |
Higher perceived severity of the disease compared to existing reports Higher perceived severity of the disease compared to existing reports |
Adjusted prevalence ratios: Frequently washing hands with soap and water 1.01 (0.98–1.04) Frequently cleaning hands with sanitizer 0.91 (0.86–0.97) |
2615 2617 |
| Fujii (2021) |
Perceived severity China Italy Japan Korea UK USA |
AORs: 1.02 (0.93–1.13) 1.05 (0.90–1.25) 0.96 (0.88–1.06) 1.12 (0.98–1.30) 1.01 (0.85–1.21) 0.92 (0.81–1.06) |
994 1020 981 918 994 1038 |
| Zewude et al. (2021) | Think you will die if infected by COVID‐19 | AOR: 0.74 (0.39–1.41) | 379 |
| Qian (2020) | Perceived severity | AOR: 0.9 (0.8–1.1) | 1011 |
| Rui (2021) Study 1 | Perceived severity | AOR 0.75 (0.96–1.93) | 321 |
| Rui (2021) Study 2 | Perceived severity | AOR 1.36 (1.22–2.35) | 319 |
| Rui (2021) Study 3 | Perceived severity | AOR 1.69 (0.67–1.31) | 315 |
| Rui (2021) Study 4 | Perceived severity | AOR 0.94 (1.1–1.9) | 343 |
| Rui (2021) Study 5 | Perceived severity | AOR 1.45 (1.07–2.1) | 329 |
| Rui (2021) Study 6 | Perceived severity | AOR 1.5 (1.03–1.81) | 315 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Other Beliefs and motivations about COVID‐19
Ten studies (Al‐Shammary 2021; Apanga 2021; Dixon et al. 2022 (Dixon et al., 2022); Kowalski 2020b; Norman 2020; Souliotis 2021 (Kyriakos et al., 2021); Stojanovic 2021 (Jovana et al., 2021); van den Broek‐Altenburg; Wang 2021; Zewude et al. 2021) were included in this category, which included views on the need for control measures, on how similar COVID‐19 is to influenza, and on which factors influenced people to followed preventative recommendations (Table 13). Like the relationships between handwashing and susceptibility, or severity of COVID‐19, the effect sizes found here were weak. Studies in this section did suggest that handwashing was more likely when people held beliefs that COVID‐19 should be taken more seriously. The strongest associations were found for motivations that were around protecting others. For example, it was observed that while self‐protection was a predictor of handwashing, protecting family members and the general public, was more strongly associated with these behaviours (Stojanovic 2021; van den Broek‐Altenburg).
Table 13.
Handwashing and beliefs and motivations about COVID‐19.
| Study ID | Determinant | Effect size (CI) | n |
|---|---|---|---|
| Al‐Shammary (2021) | Misconceptions about COVID‐19 |
Level of misconceptions was higher in those who did not engage in hand hygiene procedures: M(SD) yes = 8.01 (2.43), no = 9.09 (3.98) Cohen's d = 0.33 OR* = 1.82 |
Yes: 366, No: 34 |
| Souliotis (2021) |
Perceiving the virus to be airborne neutral vs. agree disagree vs. agree Perception that the virus is similar to common flu neutral vs. agree disagree vs. agree Perception that the virus may be asymptomatic neutral vs. agree disagree vs. agree Perception that the virus is dangerous for older people and for those with underlying health problems neutral vs. agree disagree vs agree Perceived control ‘the virus is out of control’ neutral vs. agree disagree vs. agree |
AORs: 0.83 (0.61–1.12) 0.61 (0.48–0.78) 1.33 (0.92–1.94) 1.65 (1.22–2.24) 0.75 (0.4–1.38) 0.71 (0.22–2.28) 0.83 (0.62–1.12) 1.12 (0.75–1.66) 0.95 (0.67–1.34) 0.63 (0.46–0.88) |
923 |
| Apanga (2021) | No need for preventive measures, COVID‐19 is not deadly | AOR: 0.6 (0.4–1.0) | 624 |
| Wang (2021) | COVID‐19 will be under control in the coming month | AOR: 1.03 (0.91–1.18) | 15428 |
| Zewude et al. (2021) |
Belief that COVID exists in the country Belief that COVID causes severe illness Think can be infected by covid |
AOR: 1.60 (0.67–3.84) AOR: 0.71 (0.35–1.42) AOR: 0.68 (0.35–1.32) |
379 |
| Van den Broek Altenburg (2021) |
Motivated to adhere to handwashing guidelines by Protect family Protect public Conformity Family/friends recommend Physician recommendation Politician recommendation Legal restrictions Self‐protection |
Multiple regression coefficients: 0.516 0.207 −0.139 −0.176 0.107 0.135 0.075 0.24 |
4311 |
| Norman (2020) | Instrumental attitude | r = 0.3 | 477 |
| Kowalski (2020a) Study 1 | Motivation for adherence: internal, e.g., to protect my and/or others health | r = 0.22 | 840 |
| Stojanovic (2021) |
Health concerns about oneself Health concerns about others |
Multiple regression coefficients: −0.333 (−0.703 to 0.036) 0.831 (0.376 to 1.286) |
1332 |
| Dixon et al. (2022) |
Your COVID‐19 symptoms will last a long time You could get COVID‐19 again beliefs about Belief about cause (my not wearing a face covering) Belief about cause (other people not keeping their distance) |
Multiple regression coefficients: 0.027 0.064 0.028 0.074 |
2969 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
p < 0.05.
7. DISCUSSION
7.1. Summary of main results
This systematic review aimed to synthesise the evidence examining psychosocial factors that determine the uptake and adherence to handwashing and hand sanitising behaviours for reducing the risk of infection or transmission of severe acute respiratory coronavirus 2 (SARS‐CoV‐2) in the general public.
The review forms part of the CoHeRe project (Hanratty et al., 2022). This interdisciplinary, multinational project has involved the development of an Evidence and Gap Map to identify and summarise current research on determinants of COVID‐19 protective behaviours, and a series of individual reviews examining the determinants of these specific behaviours (Hanratty et al., 2022).
This review provides one of the first studies to synthesis, using meta‐analyses and narrative summaries, evidence on the malleable factors that are most associated with handwashing and hand sanitising behaviours. The focus on only malleable factors, excluding determinants such as demographic characteristics, is important, as it provides evidence to inform the development of interventions promoting handwashing. Specifically, intervention targeted at malleable determinants of protective behaviours could be used as part of effective public health messages implemented to promote handwashing and hand sanitising behaviours in the context of potential future waves of COVID‐19, and other respiratory infections with pandemic potential.
A total of 56 studies were suitable for inclusion in the review, representing 199,376 participants. All the included studies were online, cross‐sectional studies, with the majority being published in the United States (n = 12) or China (n = 10). Thirty‐five studies were published in 2021, within the first 12 months of the COVID‐19 pandemic being declared. Across all 56 included studies the most common malleable determinants of handwashing behaviours were perceived susceptibility [n = 25 studies (45%) and perceived severity (n = 21 studies (38%)]. Smaller numbers of studies examined determinants such as COVID‐related anxiety and perceived effectiveness of handwashing [n = 3 (5%) and 3 (5%) respectively].
Overall findings based on the results of the meta‐analysis indicated that emotions about COVID, knowledge of COVID‐19, and perceived social norms regarding behaviours were among the malleable determinants most associated with handwashing. Perceived effectiveness, attitudes towards behaviours, and self‐efficacy were also linked with these behaviours, albeit with a smaller effect.
Perceived severity and susceptibility of COVID‐19 were not associated with handwashing behaviour.
Findings from the meta‐analysis and narrative synthesis did therefore show some agreement, particularly related to the association between handwashing behaviours and people's emotions around COVID‐19.
It is important to note that the meta‐analyses presented in this review have a high degree of heterogeneity (apart from the two meta‐analyses that found no significant association between handwashing and perceived severity and susceptibility). This heterogeneity could be a result of variation in the measurement or operational definition of the determinants, or variation in the measurement or operational definition of handwashing, or variation in the timing of the study in relation to government‐led initiatives or mandates within each country. Furthermore, the evidence presented in the review is drawn from cross‐sectional studies, which prevents any conclusions being drawn that go beyond associations between variables. In other words, the review does not help us to understand how change in the determinants might be related to change in handwashing behaviour. This is a gap for further research.
7.2. Overall completeness and applicability of evidence
To the best of our knowledge, the evidence presented in this review represents the entirety of research to date (completed searches October 2021) on malleable determinants of handwashing as a COVID‐related behaviour. During this review, we followed a pre‐registered peer‐reviewed protocol that was developed in consultation with expert stakeholders and methods experts. A comprehensive search was conducted to identify relevant studies and a team of experts and reviewers worked independently to select studies using the predetermined eligibility criteria and extract outcome data using a standardised data extraction form.
Twenty‐eight studies (61,956 participants) were suitable for pooling of data in the meta‐analysis.
Samples from 22 countries were represented in the 56 included studies. The majority of these being from the USA (n = 12) and China (n = 10). Given that COVID‐19 is a global pandemic the more narrow geographical coverage of the studies may limit the applicability of the evidence.
This was a large review examining data from a total of 199,376 participants across the 56 studies on one COVID‐related behaviour. The research on COVID‐19 has been published at a rapid rate since the beginning of the pandemic. A rapid review conducted in 2020 as part of the CoHeRe project (Hanratty et al., 2021), included 54 studies looking at 9 different COVID‐related behaviours. This review included 56 studies looking at handwashing alone, evidencing the rapidly increasing volume of COVID‐related research. This review and subsequent reviews are highly applicable to those involved in the development and implementation of public health decisions, interventions, and messaging to promote health behaviours in the context of COVID‐19, and other respiratory infections.
7.3. Quality of the evidence
The majority of the included studies were of fair methodological quality. However, a number of studies [n = 8 (15%)], were assessed as being of low quality due to the presence of methodological limitations, primarily, lack of clarity over recruitment and methods (see Table 4).
7.4. Potential biases in the review process
To limit potential bias, a systematic approach, which included input from an information retrieval specialist, was used to plan and conduct the searches and the study identification process. Searches also included information sources such as trial registers and repositories, which were used to identify recent and rapidly emerging evidence. Other strengths include the extensive use of stakeholder involvement via advisory panel input, and through participation of the Cochrane Crowd, who contributed to the screening of a large number of potential records for inclusion. Screening was completed by three reviewers independently. In addition, 20% of all studies were checked by a second author throughout the screening and extraction process.
7.5. Agreements and disagreements with other studies or reviews
There are a number of related published and ongoing reviews on determinants of COVID‐19 health‐related behaviours but none with the broad scope of this review. A recently published review by (Liang et al., 2022) examined the psychosocial determinant of hand hygiene, mask wearing and physical distancing. They included 24 studies examining hand hygiene and applied the Risk, Attitudes, Norms, Abilities, and Self‐Regulation (RANAS) model when determining determinants of interest. They found that perceived susceptibility and severity was not a significant determinant of hand hygiene, while knowledge, perceived norms, and self‐efficacy was significant. Our findings concur and add to those found by (Liang et al., 2022).
8. AUTHORS’ CONCLUSIONS
8.1. Implications for practice and policy
The findings from this review indicate that emotions towards COVID (COVID‐related anxiety and worry), knowledge about COVID and perceived social norms are the determinants most associated with handwashing. While determinants like perceived severity and perceived susceptibility have little to no effect on handwashing behaviour. An understanding of how these malleable determinants impact hand washing behaviour provides evidence to inform the development of future interventions, and public health campaigns. Moreover, this evidence provides important insights regarding the determinants of handwashing for potential future waves of COVID‐19, and other respiratory infections.
8.2. Implications for research
The volume of research on COVID has rapidly increased from the beginning of the pandemic, and continues to emerge. Increased demand to understand the determinants of COVID‐19 related behaviour has resulted studies being completed rapidly, often at the expense of the quality of the research (Park et al., 2021). Other studies have similarly pointed to the need for well‐designed, good quality studies (Park et al., 2021), on the determinants of COVID related behaviour. In addition, the majority of our studies were from high‐income countries, largely the USA and China. COVID‐19 is a global pandemic, thus we need to understand how and if the determinants of behaviour vary globally. Finally, the most commonly reported determinants were perceived susceptibility and severity. Our research has shown these to have little to no effect on handwashing, albeit these results must be interpreted cautiously. Determinants such as emotions relating to COVID, knowledge about COVID and social norms were less commonly reported; however had a larger effect on handwashing behaviour. These determinants should be considered further.
CONTRIBUTIONS OF AUTHORS
This review was undertaken by a team with substantial expertise in systematic reviews, health behaviour and infectious diseases. Professor Martin Dempster, Principal Investigator (PI) of the project had overall responsibility for its conduct and delivery. Dr Sean O'Connor, Dr Rachel Leonard and Dr Jennifer Hanratty was responsible for the day‐to‐day operation of the review, led screening, data extraction, quality assessment and reporting. Dr Ciara Keenan acted as an information retrieval specialist, designed and conducted the searches, and contributed to screening and data extraction. Ariana Axiaq, Yuan Chi, Victoria Hawkins, Kerry Campbell, Ceri Welsh, Anna Volz and Janet Ferguson contributed to screening and data‐extraction. Professor Miller acted as advisor on evidence synthesis methodology. Dr Bradley was the content expert on communicable diseases and reviewed and commented on drafts.
Dr Jennifer Hanratty is a psychologist and expert in evidence synthesis. She has worked in evidence synthesis since 2012 and published reviews with Campbell, Cochrane and NIHR Health Technology Assessment among others, was editor with Campbell Education Co‐ordinating group, Fellow with Campbell UK & Ireland and an invited member of the international advisory board for Evidence Synthesis Ireland.
Dr Sean O'Connor is a Physiotherapist and an experienced health care researcher. He has undertaken a number of systematic reviews and studies related to behavioural interventions, including in the context of COVID‐19. He has an extensive knowledge of theory‐based implementation models for maximising integration of evidence into practice, systematic review methods including methodological quality/risk of bias assessment and the examination of stakeholder perspectives in healthcare delivery.
Dr Rachel Leonard is a Social Worker and an experienced health care researcher. She has experience of conducting and leading on a number of systematic reviews, meta‐analyses, and studies related to health interventions.
Dr Ciara Keenan is a methods editor and information retrieval specialist for the Campbell collaboration. She has considerable experience conducting and leading the creation of EGMs and systematic reviews.
Ariana Axiaq is a third year medical student with an interest in health promotion and extensive research experience in thematic analyses and systematic reviews.
Yuan Chi is Cochrane Information Specialist, Founder CEO of Yealth Technology, core team member with Cochrane COVID‐19 Study Register (https://covid-19.cochrane.org/), and the only Chinese executive team member for COVID19 Recommendation Map. She has 8 years experience on evidence synthesis, assisted 50+ international projects, resulting in 11 authorships and 28 recommendations from Cochrane editors, information specialists and authors.
Dr Janet Ferguson is a researcher with a background in the use of technology to provide training in social communication to parents of autistic children. She has experience in assisting and conducting Systematic Literature Reviews across a number of related topics.
Victoria Hawkins is a Masters student in the School of Psyhcology, QUB.
Kerry Campbell is a PhD student in the School of Psyhcology, QUB.
Ceri Welsh is a PhD student in the School of Psyhcology, QUB.
Anna Volz is a third year undergraduate psychology student.
Professor Sarah Miller is Director of Campbell UK & Ireland. She is co‐chair and co‐editor of the Campbell Education Coordinating Group.
Dr Bradley is a consultant in public health medicine and clinical lecturer in public health and was consultant in health protection (communicable disease control) before taking up his current post. His publishing record includes several systematic reviews and studies of healthcare‐related behaviour. He is a member of the Northern Ireland COVID‐19 Modelling and Behaviour Change Groups.
Professor Dempster, is a registered Health Psychologist and Chartered Statistician, with over 20 years’ experience in conducting research on the determinants of behaviour change. He has published 14 reviews, including reviews of effectiveness and reviews of covariates. He is currently a member of the Northern Ireland Public Health Agency COVID‐19 Behaviour Change Group.
Content: Bradley, Dempster, Hanratty, Miller, Keenan, O'Connor, Leonard
Systematic review methods: Hanratty, Miller, Dempster, Keenan, O'Connor, Leonard
Statistical analysis: Dempster, Miller, Hanratty, Keenan, O'Connor, Leonard, Ferguson, Axiaq, Chi, Volz, Welsh, Campbell, Hawkins
Qualitative Evidence Synthesis: n/a
Information retrieval: Hanratty, Keenan, O'Connor
DECLARATIONS OF INTEREST
None of the review team have any present or past affiliations or other involvement in any organisation or entity with an interest in the review's findings that might lead to a real or perceived conflict of interest.
PLANS FOR UPDATING THIS REVIEW
This review will not be updated by the project team as the end of our funding period is on 18th October 2022. Teams interested in building on the review or contributing to updating beyond the project end date are encouraged to contact the corresponding author.
SOURCES OF SUPPORT
Internal sources
No sources of support provided
External sources
No sources of support provided
Supporting information
Supporting information.
ACKNOWLEDGEMENTS
We gratefully acknowledge the invaluable support of the Cochrane Crowd, (https://crowd.cochrane.org/(https://crowd.cochrane.org/). The Crowd screened over 25,000 records for the project and we are indebted to each individual who contributed to this effort and to Anna‐Noel Storr at Cochrane for coordinating.
We also wish to acknowledge the contribution of our advisory groups. Our expert advisory group provided insights and guidance from their collective expertise in COVID‐related policy‐making, behaviour change and evidence synthesis methodology. Our citizen advisors have generously shared their personal experiences and insights which directly led to improvements in how determinants in the map were categorised and identified gaps in the evidence base that would not have been identified otherwise. Thank you.
Finally, we wish to thank the Campbell editorial team for their support in reviewing and producing this review.
Leonard, R. , O'Connor, S. R. , Hanratty, J. , Keenan, C. , Chi, Y. , Ferguson, J. , Axiaq, A. , Volz, A. , Welsh, C. , Campbell, K. , Hawkins, V. , Miller, S. , Bradley, D. , & Dempster, M. (2024). Psychological and psychosocial determinants of COVID‐related handwashing behaviours: A systematic review. Campbell Systematic Reviews, 20, e1421. 10.1002/cl2.1421
Linked Article
REFERENCES
- Al‐Sejari, M. M. , & Al‐Ma'seb, H. B. (2021). Precautionary measures and illness attitudes toward COVID‐19 among a sample of the Kuwaiti population. Social Work in Public Health, 36(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Al‐Shammary, A. A. , Hassan, S. N. , Zahra, A. , Algahtani, F. B. Z. , & Suleiman, S. (2021). Role of community‐based measures in adherence to self‐protective behaviors during first wave of COVID‐19 pandemic in Saudi Arabia. Health Promotion Perspectives, 11(1), 69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Wutayd, O. , Mansour, A. E. , Aldosary, A. H. , Hamdan, H. Z. , & Al‐Batanony, M. A. (2021). Handwashing knowledge, attitudes, and practices during the COVID‐19 pandemic in Saudi Arabia: A non‐representative cross‐sectional study. Scientific Reports, 11(1), 16769. 10.1038/s41598-021-96393-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apanga, P. A. , & Kumbeni, M. T. (2021). Adherence to COVID‐19 preventive measures and associated factors among pregnant women in Ghana. Tropical Medicine & International Health: TM & IH, 26(6), 656–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett, C. , & Cheung, K. L. (2021). Knowledge, socio‐cognitive perceptions and the practice of hand hygiene and social distancing during the COVID‐19 pandemic: A cross‐sectional study of UK university students. BMC Public Health, 21(1), 426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogg, T. , & Milad, E . (2020). Demographic, personality, and social cognition correlates of coronavirus guideline adherence in a U.S. sample. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association, 39(12), 1026–1036. 10.1037/hea0000891 [DOI] [PubMed] [Google Scholar]
- van den Broek‐Altenburg, E. , & Atherly, A. (2021). Adherence to COVID‐19 policy measures: Behavioral insights from The Netherlands and Belgium. PLoS One, 16(5), e0250302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin, W. , & Bennett, D . (2020). Relationships between initial COVID‐19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine, 59(2), 157–167. 10.1016/j.amepre.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin, W. , Htay‐Wah, S. , & Goldman Dana, P. (2020). Political polarization in US residents’ COVID‐19 risk perceptions, policy preferences, and protective behaviors. Journal of Risk and Uncertainty, 61(2), 177–194. 10.1007/s11166-020-09336-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan, T. , Lueck, J. A. , Trujillo, K. L. , & Ferdinand, A. O. (2021). Rural and urban differences in COVID‐19 prevention behaviors. The Journal of Rural Health, 37(2), 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge Academic. [Google Scholar]
- Comprehensive Meta‐Analysis Version 4 . Borenstein, M. , Hedges, L. , Higgins, J. , & Rothstein, H. Biostat, Englewood, NJ. (2022). [Google Scholar]
- Cowling, B. J. , Ali, S. T. , Ng, T. W. Y. , Tsang, T. K. , Li, J. C. M. , Fong, M. W. , Liao, Q. , Kwan, M. Y. , Lee, S. L. , Chiu, S. S. , Wu, J. T. , Wu, P. , & Leung, G. M. (2020). Impact assessment of non‐pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. The Lancet Public Health, 5(5), e279–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta, D. , & Vanelli, M. (2020). WHO declares COVID‐19 a pandemic. Acta Bio‐Medica: Atenei Parmensis, 91(1), 157–160. 10.23750/abm.v91i1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon, D. , Den Daas, C. , Hubbard, G. , & Johnston, M. (2022). Using behavioural theory to understand adherence to behaviours that reduce transmission of COVID‐19; evidence from the CHARIS representative national study. British Journal of Health Psychology, 27(1), 116–135. 10.1111/bjhp.12533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwipayanti Ni Made, U. , Lubis Dinar, S. , & Harjana Ngakan Putu, A. (2021). Public perception and hand hygiene behavior during COVID‐19 pandemic in Indonesia. Frontiers in Public Health, 9, 621800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder, N. C. , Sawyer, W. , Pallerla, H. , Khaja, S. , & Blacker, M. (2014). Hand hygiene and face touching in family medicine offices: A Cincinnati Area Research and Improvement Group (CARInG) network study. The Journal of the American Board of Family Medicine, 27(3), 339–346. [DOI] [PubMed] [Google Scholar]
- Flumignan, R. L. G. , Nakano, L. C. U. , Pascoal, P. I. F. , Santos, B. C. , Correia, R. M. , Silveira, B. P. , Takihi, F. A. , Flumignan, C. D. Q. , Amorim, J. E. , & Atallah, Á. N. (2020). Evidence from Cochrane systematic reviews for controlling the dissemination of COVID‐19 infection. A narrative review. Sao Paulo Medical Journal, 138(4), 336–344. 10.1590/1516-3180.2020.029105062020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujii, R. , Suzuki, K. , & Niimi, J. (2021). Public perceptions, individual characteristics, and preventive behaviors for COVID‐19 in six countries: A cross‐sectional study. Environmental Health and Preventive Medicine, 26(1), 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girum, T. , Lentiro, K. , Geremew, M. , Migora, B. , Shewamare, S. , & Shimbre, M. S. (2021). Optimal strategies for COVID‐19 prevention from global evidence achieved through social distancing, stay at home, travel restriction and lockdown: A systematic review. Archives of Public Health, 79(1), 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger, S. , Lee, C. M. , & Larimer, M. E. (2021). Young adults underestimate how well peers adhere to COVID‐19 preventive behavioral guidelines. The Journal of Primary Prevention, 42(3), 309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haliwa, I. , Lee, J. , Wilson, J. , & Shook, N. J. (2020). Mindfulness and engagement in COVID‐19 preventive behavior. Preventive Medicine Reports, 20, 101246. 10.1016/j.pmedr.2020.101246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanratty, J. , Bradley, D. T. , Miller, S. J. , & Dempster, M. (2021). Determinants of health behaviours intended to prevent spread of respiratory pathogens that have pandemic potential: A rapid review. Acta Psychologica, 220, 103423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanratty, J. , Keenan, C. , O'Connor, S. , Miller, S. , Bradley, D. , & Dempster, M. (2022). PROTOCOL: Psychological and psychosocial determinants of COVID Health Related Behaviours (COHeRe): A suite of systematic reviews and an evidence and gap map. Campbell Systematic Reviews, 18(1), e1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanratty, J. , Keenan, C. , O'connor, S. R. , Leonard, R. , Chi, Y. , Ferguson, J. , Axiaq, A. , Miller, S. , Bradley, D. , & Dempster, M. (2023). Psychological and psychosocial determinants of COVID Health Related Behaviours (COHeRe): An evidence and gap map. Campbell Systematic Reviews, 19(3), 1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houghton, C. , Meskell, P. , Delaney, H. , Smalle, M. , Glenton, C. , Booth, A. , Chan, X. H. S. , Devane, D. , & Biesty, L. M. (2020). Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: A rapid qualitative evidence synthesis. Cochrane Database of Systematic Reviews, 21(4), CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsing, J. C. , Ma, J. , Barrero‐Castillero, A. , Jani, S. G. , Pulendran, U. P. , Lin, B. J. , Thomas‐Uribe, M. , & Wang, C. J. (2021). Influence of health beliefs on adherence to COVID‐19 preventative practices: International, social media‐based survey study. Journal of Medical Internet Research, 23(2), e23720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal, M. A. , & Younas, M. Z. (2021). Public knowledge, attitudes, and practices towards COVID‐19 in Pakistan: a cross‐sectional study. Children and Youth Services Review, 120, 105784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang, W. M. , Jang, D. H. , & Lee, J. Y. (2020). Social distancing and transmission‐reducing practices during the 2019 coronavirus disease and 2015 Middle East respiratory syndrome coronavirus outbreaks in Korea. Journal of Korean Medical Science, 35(23), e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson, T. , Del Mar, C. B. , Dooley, L. , Ferroni, E. , Al‐Ansary, L. A. , Bawazeer, G. A. , van Driel, M. L. , Jones, M. A. , Thorning, S. , Beller, E. M. , Clark, J. , Hoffmann, T. C. , Glasziou, P. P. , & Conly, J. M. (2020). Physical interventions to interrupt or reduce the spread of respiratory viruses. The Cochrane Database of Systematic Reviews, 11(11), 006207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez, T. , Restar, A. , Helm, P. J. , Cross, R. I. , Barath, D. , & Arndt, J. (2020). Fatalism in the context of COVID‐19: Perceiving coronavirus as a death sentence predicts reluctance to perform recommended preventive behaviors. SSM—Population Health, 11, 100615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovančević, A. , & Milićević, N. (2020). Optimism‐pessimism, conspiracy theories and general trust as factors contributing to COVID‐19 related behavior—A cross‐cultural study. Personality and Individual Differences, 167, 110216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kebede, Y. , Yitayih, Y. , Birhanu, Z. , Mekonen, S. , & Ambelu, A. (2020). Knowledge, perceptions and preventive practices towards COVID‐19 early in the outbreak among Jimma University Medical Center visitors, Southwest Ethiopia. PLoS One, 15(5), e0233744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalski, J. , Marta, M. , Zuzanna, M. , Paulina, G. , & Lukasz, G. (2020a). Adherence to safety and self‐isolation guidelines, conspiracy and paranoia‐like beliefs during COVID‐19 pandemic in Poland—Associations and moderators. Psychiatry Research, 294, 113540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalski, J. , Marta, M. , Zuzanna, M. , Paulina, G. , & Lukasz, G. (2020b). Adherence to safety and self‐isolation guidelines, conspiracy and paranoia‐like beliefs during COVID‐19 pandemic in Poland—Associations and moderators. Psychiatry Research, 294, 113540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahiri, A. , Jha, S. S. , Chakraborty, A. , Dobe, M. , & Dey, A. (2021). Role of threat and coping appraisal in protection motivation for adoption of preventive behavior during COVID‐19 pandemic. Frontiers in Public Health, 9, 678566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lao, C. K. , Li, X. , Zhao, N. , Gou, M. , & Zhou, G. (2023). Using the health action process approach to predict facemask use and hand washing in the early stages of the COVID‐19 pandemic in China. Current Psychology, 42(8), 6484–6493. 10.1007/s12144-021-01985-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, M. , Kang, B. A. , & You, M. (2021). Knowledge, attitudes, and practices (KAP) toward COVID‐19: A cross‐sectional study in South Korea. BMC Public Health, 21, 295. 10.1186/s12889-021-10285-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, H. , Moon, S. J. , Ndombi, G. O. , Kim, K. N. , Berhe, H. , & Nam, E. W. (2020). COVID‐19 perception, knowledge, and preventive practice: Comparison between South Korea, Ethiopia, and Democratic Republic of Congo. African Journal of Reproductive Health, 24(s1), 66–77. [DOI] [PubMed] [Google Scholar]
- Levay, P. , & Finnegan, A. (2021). The NICE COVID‐19 search strategy for Ovid MEDLINE and Embase: Developing and maintaining a strategy to support rapid guidelines. medRxiv;21258749(1):1–61. 10.1101/2021.06.11.21258749 [DOI] [Google Scholar]
- Li, M. , Lv, G. , Hsieh, S. , Shao, R. , & Yuan, J. (2021). Pandemic worry and preventive health behaviors during the cOVID‐19 outbreak. Frontiers in Medicine, 8, 700072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, W. , Duan, Y. , Li, F. , Rhodes, R. E. , Wang, X. , Peiris, D. L. I. H. K. , Zhou, L. , Shang, B. , Yang, Y. , Baker, J. S. , Jiao, J. , & Han, W. (2022). Psychosocial determinants of hand hygiene, facemask wearing, and physical distancing during the COVID‐19 pandemic: A systematic review and meta‐analysis. Annals of Behavioral Medicine, 56(11), 1174–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matkovic, J. , Clemens, K. S. , Faasse, K. , & Geers, A. L. (2021). Handwashing message type predicts behavioral intentions in the United States at the beginning of the global COVID‐19 pandemic. Frontiers in Public Health, 9, 583491. 10.3389/fpubh.2021.583491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie, S. , & West, R. (2020). Behavioural, environmental, social, and systems interventions against covid‐19. BMJ, 370, m2982. [DOI] [PubMed] [Google Scholar]
- Milman, E. , Lee, S. A. , & Neimeyer, R. A. (2022). Social isolation and the mitigation of coronavirus anxiety: the mediating role of meaning. Death Studies, 46, 1–13. [DOI] [PubMed] [Google Scholar]
- Mousavi, S. H. , Delshad, M. H. , Acuti Martellucci, C. , Bhandari, D. , Ozaki, A. , Pourhaji, F. , Pourhaji, F. , Reza Hosseini, S. M. , Roien, R. , Ramozi, A. A. , Wafaee, M. , Qaderi, S. , Delsoz, M. , Sigdel, S. , Kotera, Y. , Sawano, T. , Dhama, K. , Rodríguez‐Morales, A. J. , Wang, J. , … Sah, R. (2022). Community behavioral and perceived responses in the COVID‐19 outbreak in Afghanistan: A cross‐sectional study. Disaster Medicine and Public Health Preparedness, 16(6), 2464–2470. 10.1017/dmp.2021.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, T. L. , Fosdick, B. K. , Biela, L. M. , Schoenberg, H. , Mast, S. , McGinnis, E. , Young, M. C. , Lynn, L. , Fahrner, S. , Nolt, L. , Dihle, T. , Quicke, K. , Gallichotte, E. N. , Fitzmeyer, E. , Ebel, G. D. , Pabilonia, K. , Ehrhart, N. , & VandeWoude, S. (2021). Association between COVID‐19 exposure and self‐reported compliance with public health guidelines among essential employees at an institution of higher education in the US. JAMA Network Open, 4(7), e2116543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman, P. , Wilding, S. , & Conner, M. (2020). Reasoned action approach and compliance with recommended behaviours to prevent the transmission of the SARS‐CoV‐2 virus in the UK. British Journal of Health Psychology, 25(4), 1006–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owhonda, G. , Maduka, O. , Nwadiuto, I. , Tobin‐West, C. , Azi, E. , Ojimah, C. , Alasia, D. , Olofinuka, A. M. , Agala, V. , Paul, J. N. , Nria, D. , Okafor, C. , Ndekwu, I. , Opara, C. , & Newsom, C. (2022). Awareness, perception and the practice of COVID‐19 prevention among residents of a state in the South‐South region of Nigeria: implications for public health control efforts. International Health, 14(3), 309–318. 10.1093/inthealth/ihab046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozdemir, S. , Ng, S. , Chaudhry, I. , & Finkelstein, E. A. (2022). Adoption of preventive behaviour strategies and public perceptions about COVID‐19 in Singapore. International Journal of Health Policy and Management, 11(5), 579–591. 10.34172/ijhpm.2020.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal, R. , Yadav, U. , Grover, S. , Saboo, B. , Verma, A. , & Bhadada, S. K. (2020). Knowledge, attitudes and practices towards COVID‐19 among young adults with Type 1 Diabetes Mellitus amid the nationwide lockdown in India: A cross‐sectional survey. Diabetes Research and Clinical Practice, 166, 108344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, Y. , Xin, M. , Zhang, C. , Dong, W. , Fang, Y. , Wu, W. , Li, M. , Pang, J. , Zheng, Z. , Wang, Z. , Yuan, J. , & He, Y. (2020). Associations of mental health and personal preventive measure compliance with exposure to COVID‐19 information during work resumption following the COVID‐19 outbreak in China: Cross‐sectional survey study. Journal of Medical Internet Research, 22(10), e22596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, J. J. H. , Mogg, R. , Smith, G. E. , Nakimuli‐Mpungu, E. , Jehan, F. , Rayner, C. R. , Condo, J. , Decloedt, E. H. , Nachega, J. B. , Reis, G. , & Mills, E. J. (2021). How COVID‐19 has fundamentally changed clinical research in global health. The Lancet. Global health, 9(5), e711–e720. 10.1016/S2214-109X(20)30542-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prete, G. , Fontanesi, L. , Porcelli, P. , & Tommasi, L. (2020). The psychological impact of COVID‐19 in Italy: Worry leads to protective behavior, but at the cost of anxiety. Frontiers in Psychology, 11, 566659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian, M. , Wu, Q. , Wu, P. , Hou, Z. , Liang, Y. , Cowling, B. J. , & Yu, H. (2020). Anxiety levels, precautionary behaviours and public perceptions during the early phase of the COVID‐19 outbreak in China: A population‐based cross‐sectional survey. BMJ Open, 10(10), e040910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rattay, P. , Michalski, N. , Domanska, O. M. , Kaltwasser, A. , De Bock, F. , Wieler, L. H. , & Jordan, S. (2021). Differences in risk perception, knowledge and protective behaviour regarding COVID‐19 by education level among women and men in Germany. Results from the COVID‐19 Snapshot Monitoring (COSMO) study. PLoS One, 16(5), e0251694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rui, J. , Raymond, Y. K. , & Juan, C. (2021). Information sources, risk perception, and efficacy appraisal's prediction of engagement in protective behaviors against COVID‐19 in China: Repeated cross‐sectional survey. JMIR Human Factors, 8(1), e23232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengeh, P. , Jalloh, M. B. , Webber, N. , Ngobeh, I. , Samba, T. , Thomas, H. , Nordenstedt, H. , & Winters, M. (2020). Community knowledge, perceptions and practices around COVID‐19 in Sierra Leone: A nationwide, cross‐sectional survey. BMJ Open, 10(9), e040328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto, W. , Tsang, D. , Yung, R. , Ching, T. , Ng, T. , Ho, M. , Ho, L. , & Peiris, J. (2003). Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). The Lancet, 361(9368), 1519–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, M. , Batra, K. , Davis, R. E. , & Wilkerson, A. H. (2021). Explaining handwashing behavior in a sample of college students during COVID‐19 pandemic using the multi‐theory model (MTM) of health behavior change: A single institutional cross‐sectional survey. Healthcare, 9(1), 55. 10.3390/healthcare9010055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shook, N. J. , Sevi, B. , Lee, J. , Oosterhoff, B. , & Fitzgerald, H. N. (2020). Disease avoidance in the time of COVID‐19: The behavioral immune system is associated with concern and preventative health behaviors. PLoS One, 15(8), e0238015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si, R. , Yao, Y. , Zhang, X. , Lu, Q. , & Aziz, N. (2021). Investigating the links between vaccination against COVID‐19 and public attitudes toward protective countermeasures: Implications for public health. Frontiers in Public Health, 9, 702699. 10.3389/fpubh.2021.702699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souliotis, K. , Giannouchos, T. V. , Peppou, L. E. , Samara, M. T. , Nimatoudis, J. , Papageorgiou, C. , & Economou, M. (2021). Public health behaviors during the COVID‐19 pandemic in Greece and associated factors: A nationwide cross‐sectional survey. Inquiry: A Journal of Medical Care Organization, Provision and Financing, 58, 469580211022913. 10.1177/00469580211022913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stojanovic, J. , Raparelli, V. , Boccia, S. , Bacon, S. L. , Lavoie, K. L. , & i Care Study Team . (2021). Public perceptions and behavioural responses to the first COVID‐19 pandemic wave in Italy: Results from the iCARE study. European Journal of Public Health, 31(6), 1270–1277. 10.1093/eurpub/ckab147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Joanna Briggs Institute . (2017). The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. Checklist for Analytical Cross Sectional Studies. The Joanna Briggs Institute.
- The Joanna Briggs Institute . (2020). The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. Checklist for Cohort Studies. The Joanna Briggs Institute.
- Trifiletti, E. , Shamloo Soraya, E. , Martina, F. , & Agustina, Z. (2021). Psychological predictors of protective behaviours during the Covid‐19 pandemic: Theory of planned behaviour and risk perception. Journal of Community & Applied Social Psychology, 32(3), 382–397. 10.1002/casp.2509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Q. , Mo, P. K. H. , Song, B. , Di, J. L. , Zhou, F. R. , Zhao, J. , Wu, Y. L. , Tian, H. , Qiu, L. Q. , Xia, J. , Wang, L. , Li, F. , & Wang, L. H. (2021). Mental health and preventive behaviour of pregnant women in China during the early phase of the COVID‐19 period. Infectious Diseases of Poverty, 10(1), 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren‐Gash, C. , Fragaszy, E. , & Hayward, A. C. (2013). Hand hygiene to reduce community transmission of influenza and acute respiratory tract infection: A systematic review. Influenza and Other Respiratory Viruses, 7(5), 738–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster, R. K. , Brooks, S. K. , Smith, L. E. , Woodland, L. , Wessely, S. , & Rubin, G. J. (2020). How to improve adherence with quarantine: Rapid review of the evidence. Public Health, 182, 163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West, R. , Michie, S. , Rubin, G. J. , & Amlôt, R. (2020). Applying principles of behaviour change to reduce SARS‐CoV‐2 transmission. Nature Human Behaviour, 4(5), 451–459. [DOI] [PubMed] [Google Scholar]
- White, H. , Albers, B. , Gaarder, M. , Kornør, H. , Littell, J. , Marshall, Z. , Mathew, C. , Pigott, T. , Snilstveit, B. , Waddington, H. , & Welch, V. (2020). Guidance for producing a Campbell evidence and gap map. Campbell Systematic Reviews, 16(4), e1125. 10.1002/cl2.1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, F. , Zhao, S. , Yu, B. , Chen, Y. M. , Wang, W. , Song, Z. G. , Hu, Y. , Tao, Z. W. , Tian, J. H. , Pei, Y. Y. , Yuan, M. L. , Zhang, Y. L. , Dai, F. H. , Liu, Y. , Wang, Q. M. , Zheng, J. J. , Xu, L. , Holmes, E. C. , & Zhang, Y. Z. (2020). A new coronavirus associated with human respiratory disease in China. Nature, 579(7798), 265–269. 10.1038/s41586-020-2008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zewude, B. , Melese, B. , Habtegiorgis, T. , Tadele, M. , & Solomon, W. (2021). Compliance with protective behavioral recommendations in the outbreak of COVID‐19 among people working in the urban‐based informal economy in Southern Ethiopia. Frontiers in Public Health, 9, 716814. 10.3389/fpubh.2021.716814 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.


