Abstract
Molluscum contagiosum is a common skin infection affecting different body areas, including the face. Previous data have shown cases of atypical lesions, notably on the face, and it was thought relevant to further examine differences between facial and non-facial lesions. All cases of children (0–18) diagnosed with molluscum contagiosum from 2013–2022 at the paediatric dermatology clinic of Soroka University Medical Center were retrospectively reviewed, and 615 children were included in the study. Facial lesions tended to be found in younger children (p = 0.018). Non-facial lesions were more erythematous (p < 0.001), itchier (p < 0.001), and showed similar patterns of ulceration (p = 0.078) and purulence (p = 0.779). The average lesion diameter was similar in patients with or without facial lesions (p = 1). Children with facial lesions were treated differently from patients without facial lesions (p < 0.001); however, there were no differences in treatment response. This research challenges assumptions concerning the severity of facial lesions, including eyelid lesions, by revealing that, overall, they exhibit less inflammation than non-facial lesions. Despite the potential for greater psychosocial burdens and impacts on self-esteem associated with lesions on the sensitive facial area, this study provides evidence that they are not inherently more worrisome and can be managed similarly to lesions found elsewhere in the body.
SIGNIFICANCE
Molluscum contagiosum is a prevalent skin infection with distinctive features, but at times it exhibits atypical manifestations, particularly on the face, where the skin differs from the rest of the body. Our study aimed to investigate potential variations in the presentation of molluscum contagiosum infections between facial and non-facial areas. After analysing 615 children, we observed that both facial and non-facial lesions shared similar characteristics regarding inflammation risk and responses to conventional treatments for this condition; thus, they can be managed similarly.
Key words: inflammation, molluscum contagiosum, paediatric dermatology
Molluscum contagiosum (MC) is a common skin infection with a worldwide prevalence of 5–11.5% in children aged 0–16 (1). It is caused by a poxvirus that usually presents as rounded, skin-coloured papules with an umbilicated surface (2). As a benign condition, most MC cases self-resolve within 6 to 9 months, but the duration may vary and may last up to 4 years (2). Diagnosis relies on clinical assessment, with tools such as dermoscopy, confocal microscopy, or skin biopsy when needed (2).
Due to its typical self-limiting course, MC is traditionally left untreated. Nevertheless, the substantial potential for transmission and the associated risks of secondary complications, such as bacterial superinfection, molluscum dermatitis, scarring, and aesthetic disturbances, could serve as compelling reasons to consider treatment, depending on the individual patient’s circumstances (3). These interventions encompass various approaches, including surgical methods like curettage and cryotherapy administered in clinical settings. Alternatively, chemical or immunomodulatory approaches involve the application of creams containing tretinoin, salicylic acid, and podophyllotoxin, which can be self-administered at home. Notably, cantharidin has gained prominence as the first FDA-approved medication for MC, signalling a recent increase in its utilization (4).
Though the clinical presentation of MC may be straightforward, MC can show an atypical presentation depending on its location. For instance, periocular lesions have been described as erythematous, nodular umbilicated, big/giant, conglomerated, inflamed, or pedunculated (5). Additionally, the literature has reported some unusual presentations of MC infections on the face and scalp in both immunocompetent adults and children (6, 7). Because of marked differences in the skin microbiome, thickness of skin layers, levels of natural moisturizing factor, and sebaceous glands concentration, facial skin is anatomically and physiologically distinct from the skin found on the rest of the body (8). These differences hold not only biological significance but also influence how the skin responds to various pathological processes and treatments, such as atopic dermatitis (8), psoriasis (9), or leishmaniosis (10) for instance. Despite these observations, it is noteworthy that, to our knowledge, no comprehensive study has systematically explored the distinctions between facial and non-facial MC lesions. This gap in research leaves room for further investigation into the unique aspects of MC infection in specific regions like the face.
Here, we aim to delve into this issue by evaluating various patient characteristics and their clinical presentations in individuals with facial and non-facial MC lesions. In this manner, we hope to address a knowledge gap in MC’s diagnostic approach and management.
METHODS
This study was performed at the paediatric dermatology clinic of Soroka University Medical Center (SUMC). SUMC is a university-affiliated referral centre in Southern Israel, directly serving a population of 600,000 and serving as a tertiary hospital for more than 1 million people. Our data were collected from patients’ medical records from SUMC. The IRB number for this study was SOR-0305-21.
We retrospectively examined all cases of children (0–18) diagnosed with MC from 2013–2022. Individuals who underwent assessment or treatment for MC lesions at the paediatric dermatology clinic in SUMC during the specified period were considered for inclusion. Excluded from the study were individuals aged 18 years and older and those who had not been assessed at the paediatric dermatology clinic of SUMC. We first collected demographic data such as age, ethnicity, gender, and age at which the diagnosis of MC was made. We then evaluated all parameters pertaining to MC lesions. These included the lesions’ location, number, size, and the presence of erythema, ulceration, pruritus, or purulence. A focus on which treatment each patient received, along with secondary effects such as hypopigmentation, hyperpigmentation, and scarring, was analysed. We also evaluated recurring visits related to medical complaints after removing individuals who had not undergone any treatment. This was done to minimize potential bias in visit frequency among patients scheduled for regular office follow-ups but not undergoing treatments.
We gathered data from patients categorized into 3 groups: those with exclusively facial lesions, those with solely non-facial lesions, and those with both facial and non-facial lesions, hereafter referred to as total body lesions. While our primary analysis concentrated on discerning dissimilarities between facial and non-facial lesions, the inclusion of the total body lesions parameter in our study enriches our investigation. This addition provided a more comprehensive view of the diverse manifestations of the condition across various body regions. Upon reviewing all the treatments employed within the scope of our study, we categorized them into 2 groups: MC treatments (curettage, tretinoin, fluorouracil with salicylic acid, adapalene, imiquimod, podophyllotoxin, trichloroacetic acid, and liquid nitrogen) and supportive treatments (topical and systemic steroids and antibiotics).
Variables are described with mode for dichotomous/nominal and median for numerical. We applied Shapiro–Wilk tests to numerical values that were compared in order to assess Normality. When applicable, relationships between variables were assessed through Pearson correlation, Spearman correlation, χ2 , Fisher’s exact test, t-tests, or Mann–Whitney tests. Significance was set at p < 0.05.
RESULTS
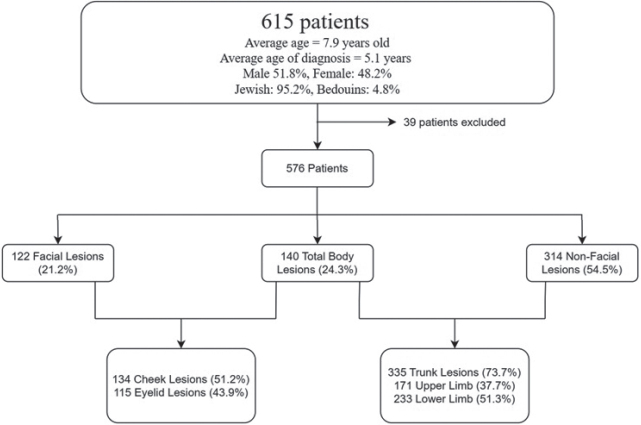
A total of 615 children were included in the study. On average, our population was 7.9 years old and had a diag-nosis of MC at 5.1 years old. Among this population, 51.8% were male, and 95.2% identified as Jewish, with the remaining portion being Bedouins (4.8%). After excluding 39 of our 615 from the study due to inaccuracies in recording the location of MC, a total of 122 individuals had only facial lesions, 314 had only non-facial lesions, and 140 had total body lesions. Of all the patients with facial lesions (n = 262), a majority occurred on the cheeks (134 cases, accounting for 51.2% of facial lesions) and eyelids (115 cases, representing 43.9%). In patients who had non-facial lesions (n = 454), the most common locations were the trunk (335 cases, 73.7%), upper limb (171 cases, 37.7%), and lower limb (233 cases, 51.3%). All characteristics are summarized in Table I and Fig. 1.
Table I.
Demographic characteristics of children with molluscum contagiosum
| Demographic | Data |
|---|---|
| Total children, n | 615 |
| Average age, years, mean | 7.9 |
| Age at diagnosis, years, mean | 5.1 |
| Gender, % | |
| Male | 51.8 |
| Female | 48.2 |
| Ethnicity, % | |
| Jewish | 95.2 |
| Bedouin | 4.8 |
| Total body lesions, n | 140 |
| Facial lesions, n (%) | 122 |
| Cheeks | 134 (51.2) |
| Eyelids | 115 (43.9) |
| Non-facial lesions, n (%) | 314 |
| Trunk | 335 (94.9) |
| Upper limb | 171 (48.4) |
| Lower limb | 233 (66) |
Fig. 1.
Flowchart summarizing characteristics of children with molluscum contagiosum.
Our analysis focused on examining different individual factors’ impact on the distinction between facial and non-facial lesions. We found that gender did not significantly affect this differentiation (p = 0.914). In contrast, age did appear to play a role in this distinction, with children with facial lesions being significantly younger than patients without facial lesions (median age of 7 years and 7.9 years respectively, p = 0.018). Though non-facial and facial lesions did not show a significant difference in terms of median lesion diameter (4 mm vs 5 mm, p = 0.314), they exhibited differences in various key aspects. Individuals with non-facial lesions tend to have a larger median number of lesions than those with facial lesions (6 vs 5, p = 0.02). Children with non-facial lesions exhibit more erythema or itchiness in association with their lesions (p < 0.001 in both cases), though patients with facial lesions tend to have more recurrent MC complaints than patients with no facial lesions (p = 0.026). However, children with facial as well as non-facial lesions demonstrate a comparable pattern regarding ulceration (p = 0.078) and purulence (p = 0.77).
Furthermore, our results suggest that of all facial lesions, eyelid lesions do not show notable distinctions concerning erythema (p = 0.163), itchiness (p = 0.229), ulceration (p = 0.478), or purulence (p = 0.540) compared with those without eyelid lesions. Additionally, gender does not play a significant role in the occurrence of eyelid lesions (p = 0.233). Importantly, our data support the observation that eyelid lesions are more common before age 8 years than after (p = 0.003).
Regarding treatments, we found notable distinctions between treatments for facial and non-facial lesions when taken individually (p < 0.001). When grouped in MC or supportive treatments, no difference was found in the distribution of these treatments between individuals with and without facial lesions (p = 0.50). Hence, curettage emerged as the predominant treatment method for facial lesions (22.2%), followed by tretinoin (17.8%) and prednisolone/gentamicin creams (15.9%). Conversely, for non-facial lesions, the most frequently employed treatments included solutions incorporating fluorouracil with salicylic acid (22.2%), followed by prednisolone/gentamicin cream (19.2%) and curettage (15%). After further investigation, the use of curettage was not more frequent in children with facial lesions compared with individuals without facial lesions (p = 0.523).
None of the treatments used showed a significant variation in response concerning ulceration (p = 0.438), itchiness (p = 0.536), erythema (p = 0.193), hyperpigmentation (p = 0.814), hypopigmentation (p = 0.330), or residual scarring (p = 0.347) following treatment for patients with facial lesions vs non-facial lesions. Key differences between facial and non-facial lesions are summarized in Table II.
Table II.
Comparison of key characteristics and treatment outcomes between facial and non-facial molluscum contagiosum lesions
| Characteristics | Non-facial lesions | Facial lesions | p-value |
|---|---|---|---|
| Lesion quantity, median | 6 | 5 | 0.02 |
| Lesion diameter, mm, median | 4 | 5 | 0.314 |
| Ulceration, n (%) | 39 (14.89) | 9 (8.18) | 0.078 |
| Purulence, n (%) | 47 (19.03) | 17 (15.32) | 0.77 |
| Itchiness, n (%) | 73 (27.04) | 11 (10.00) | < 0.001 |
| Erythema, n (%) | 181 (61.99) | 46 (40.00) | < 0.001 |
| Recurrent molluscum contagiosum complaints, n (%) | 105 (34.54) | 55 (46.22) | 0.026 |
| Mechanical removal by curettage, n (%) | 77 (25.84) | 33 (28.95) | 0.523 |
| Treatment outcome, n (%) | |||
| Ulceration | 21 (24.14) | 4 (16.67) | 0.438 |
| Itchiness | 35 (40.70) | 7 (33.33) | 0.536 |
| Erythema | 28 (33.73) | 4 (19.05) | 0.193 |
| Hyperpigmentation | 4 (26.67) | 1 (30.30) | 0.814 |
| Hypopigmentation | 10 (12.66) | 1 (5.00) | 0.330 |
| Residual scarring | 14 (17.28) | 2 (9.09) | 0.347 |
Values in bold represent statistically significant results with a p-value of less than 0.05.
With a median diameter of 6 mm and a median number of 15 lesions, we observed that individuals with total body lesions exhibited a bigger lesion diameter as well as a higher prevalence of lesions compared with those with facial lesions alone (p = 0.029 and p < 0.001 respectively) or non-facial lesions alone (p = 0.001 and p < 0.001 respectively). Total body lesions tended to be less erythematous than non-facial lesions (p = 0.008) but more pruritic than facial lesions (p = 0.035). Moreover, individuals with total body lesions were more likely to undergo curettage compared with those with facial lesions (p = 0.016) or non-facial lesions (p < 0.001). While there was no significant difference in recurrent complaints between total body and non-facial lesions (p = 0.551), patients with facial lesions had more recurrent complaints than patients with total body lesions (p = 0.016). Curettage was more likely to be done on patients with total body lesions than patients with non-facial or facial lesions only (p < 0.001 in both cases). In terms of treatment response, no significant differences were found between total body lesions and facial or non-facial lesions regarding ulceration (p = 0.634 and p = 0.762, respectively), itchiness (p = 0.708 and p = 0.211), erythema (p = 0.063 and p = 0.193), hyperpigmentation (p = 0.782 and p = 0.931), hypopigmentation (p = 0.523 and p = 0.702), and residual scarring (p = 0.238 and p = 0.625). Key differences between facial and total body lesions on one hand and between non-facial and total body lesions on the other hand are summarized in Tables SI and SII, respectively.
DISCUSSION
In this retrospective analysis, we conducted a comparative investigation between facial and non-facial MC. We aimed to explore the demographic and clinical factors contributing to this distinction. As the inaugural study of its kind, our findings revealed that facial lesions are more commonly found at a younger age. Facial lesions were notably less erythematous and itchy than non-facial lesions, but displayed similar ulceration and purulence patterns. Notably, our analysis did not identify any treatment modalities that were significantly more effective or safer for treating facial or non-facial lesions. However, we observed that patients with facial lesions tended to have more recurrent MC complaints than those without.
Our findings are compelling, indicating that facial lesions tend to demonstrate a lesser degree of inflammation compared with lesions on other body areas. This is underscored by the observation that total body lesions seemed to be less erythematous than non-facial lesions and yet showed higher levels of pruritus than facial lesions. Contrary to recent research that explored the possibility of facial skin being more prone to inflammation due to its thinner nature, distinct microbiome, and increased exposure to environmental stressors (8), our data do not align with these conclusions.
Our findings align with the recent analysis by Schisler (11), who extensively discussed the mechanism of MC infection. Following viral replication in the stratum basale, keratinocytes undergo differentiation from the stratum basale to the stratum corneum, causing the virus to be released from the stratum corneum layer (11). This results in the emergence of hypertrophied and hyperplastic epidermis projecting above the surface, forming small papules (11). The greater expansiveness and thicker epidermis of body skin compared with facial skin (12) not only account for the higher prevalence of non-facial lesions over facial lesions but also contribute to their increased erythematous nature and propensity for dermal reactions, ultimately leading to itchiness. Additional research is warranted to thoroughly evaluate these assertions to gain a more comprehensive understanding of this phenomenon.
Furthermore, our dataset challenges the prevailing assumptions concerning the severity of eyelid lesions highlighted in prior studies (13, 14). Our findings indicate that eyelid lesions exhibit no significant differences in erythema, itchiness, ulceration, or purulence. We concur that these studies might have been greatly influenced by the immunocompromised status of patients who exhibited eyelid lesions.
Our study shows that facial lesions and lesions located elsewhere on the body are treated similarly, which is consistent with current medical guidelines (15). However, we noted that patients with facial lesions exhibited a higher likelihood of recurring MC complaints compared with those without facial lesions or total body lesions. This observation gains further interest given that the primary distinction in the treatment approaches for these 3 groups was only the higher tendency to use curettage in patients with lesions on other body parts. Therefore, we infer that the increased recurrence of facial lesions might be attributed to other factors, particularly age. Younger children typically have a lesser understanding of hygiene practices and are more prone to touching their faces, potentially facilitating the spread of the condition. This echoes with other studies that have shown a similar trend to other common dermatological diseases, such as impetigo for instance (16).
Nevertheless, our results indicate no discernible distinctions in the effectiveness of various treatments, whether applied to facial or non-facial lesions, regarding reducing ulceration, erythema, or itchiness. Additionally, no notable differences were observed in side effects, including hyperpigmentation, hypopigmentation, or scarring, and none of the treatments exhibited variations in the recurrence of lesions. In light of these findings, we conclude that while lesions on the sensitive area of the face may be more burdensome and affect self-esteem (17), they are not inherently more worrisome and can be treated in the same manner as lesions elsewhere on the body.
Strength and limitations
Our study has several strengths. First, our study comprises a substantial number of cases with well-documented follow-up treatments, providing a solid foundation for confidence in our statistical analysis. Second, our patients received evaluations at a single centre by a board-certified paediatric dermatologist, thereby minimizing the potential for variations in the interpretation of skin lesions among different individuals. Third, the retrospective nature of our study enabled us to investigate potential lesion recurrence following treatment. However, our study is not without limitations. Because it was not accessible during the study period, our research was unable to make comparisons with recent FDA-approved treatments cantharidin and berdazimer gel (4).
Furthermore, we acknowledge the likelihood of selection bias, given that all cases were gathered from an in-hospital setting, possibly encompassing patients with a more pronounced perception of their symptoms. Finally, our data collection did not permit a direct intra-individual comparison of lesions in patients with total body involvement. Such a comparison could have assisted in mitigating bias, as it would have minimized variability in the immune system for each individual.
Conclusion
Our retrospective analysis compared facial and non-facial lesions, revealing that facial lesions tend to be more present at a younger age than non-facial lesions. Although facial lesions display less erythema and itchiness than non-facial lesions, both exhibit similar ulceration and purulent patterns. The study challenges assumptions regarding facial lesion severity. Although lesions on the sensitive area of the face might pose greater psychosocial burdens and impact self-esteem, they are not inherently more concerning and can be managed similarly to lesions found elsewhere on the body.
ACKNOWLEDGEMENTS
The authors acknowledge the use of OpenAI during the writing process, more specifically for revisions of possible structure and grammar mistakes.
Footnotes
The authors have no conflicts of interest to declare.
Ethical statement
Approval from Soroka Medical Center’s institutional review board was obtained prior to the study which complied with the 1964, 1975, and 2013 revisions of the Helsinki Declaration (approval number SOR-0305-21).
REFERENCES
- 1.Olsen JR, Gallacher J, Piguet V, Francis NA. Epidemiology of molluscum contagiosum in children: a systematic review. Fam Pract 2014; 31: 130–136. [DOI] [PubMed] [Google Scholar]
- 2.Meza-Romero R, Navarrete-Dechent C, Downey C. Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clin Cosmet Investig Dermatol 2019; 12: 373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van der Wouden JC, van der Sande R, Kruithof EJ, Sollie A, van Suijlekom-Smit LW, Koning S. Interventions for cutaneous molluscum contagiosum. Cochrane Database Syst Rev 2017; 2017: CD004767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hebert AA, Bhatia N, Del Rosso JQ. Molluscum contagiosum: epidemiology, considerations, treatment options, and therapeutic gaps. J Clin Aesthetic Dermatol 2023; 16: S4–11. [PMC free article] [PubMed] [Google Scholar]
- 5.Rosner M, Zloto O. Periocular molluscum contagiosum: six different clinical presentations. Acta Ophthalmol (Copenh) 2018; 96: e600–605. [DOI] [PubMed] [Google Scholar]
- 6.Sun YW, Oh CW, Kim TH. Molluscum contagiosum of the newborn: an unusual presentation. Ann Dermatol 2016; 10: 53–55. [Google Scholar]
- 7.Kim HK, Jang WS, Kim BJ, Kim MN. Rare manifestation of giant molluscum contagiosum on the scalp in old age. Ann Dermatol 2013; 25: 109–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Contento M, Maher J, Cline A, Rose S. Why does facial eczema differ from body eczema? J Drugs Dermatol 2022; 21: 1119–1123. [DOI] [PubMed] [Google Scholar]
- 9.Keshavarz E, Roknsharifi S, Shirali Mohammadpour R, Roknsharifi M. Clinical features and severity of psoriasis: a comparison of facial and nonfacial involvement in Iran. Arch Iran Med 2013; 16: 25–28. [PubMed] [Google Scholar]
- 10.Yedidia Moser R, Ben-Shimol S, Sagi O, Horev A. Comparison between cutaneous leishmaniasis patients with facial and non-facial lesions. Int J Dermatol 2021; 60: 1109–1113. [DOI] [PubMed] [Google Scholar]
- 11.Shisler JL. Immune evasion strategies of molluscum contagiosum virus. Adv Virus Res 2015; 92: 201–252. [DOI] [PubMed] [Google Scholar]
- 12.Gambichler T, Matip R, Moussa G, Altmeyer P, Hoffmann K. In vivo data of epidermal thickness evaluated by optical coherence tomography: effects of age, gender, skin type, and anatomic site. J Dermatol Sci 2006; 44: 145–152. [DOI] [PubMed] [Google Scholar]
- 13.Gaurkar SP, Pund PB, Dindore PR, Bhoi UY. Extensive molluscum contagiosum causing obstruction of vision in HIV positive woman. Indian Dermatol Online J 2016; 7: 190–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson MR, Udell IJ, Garber PF, Perry HD, Streeten BW. Molluscum contagiosum of the eyelids in patients with acquired immune deficiency syndrome. Ophthalmology 1992; 99: 1745–1747. [DOI] [PubMed] [Google Scholar]
- 15.Badri T, Gandhi GR. Molluscum contagiosum. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2023. [cited 2023 Nov 1]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK441898/ [PubMed] [Google Scholar]
- 16.Dollani LC, Marathe KS. Impetigo/staphylococcal scalded skin disease. Pediatr Rev 2020; 41: 210–212. [DOI] [PubMed] [Google Scholar]
- 17.Jankowski M, Goroncy A. Perceptive hierarchy of facial skin lesions: an eye-tracking study. Acta Derm Venereol 2022; 102: adv00799. [DOI] [PMC free article] [PubMed] [Google Scholar]