Abstract
Background
Musculoskeletal disability (MSD) has been identified as having a negative impact on oral health. Patients with MSD have a greater burden of medical expenses and are expected to have an Economic unmet dental need (UDN). This study aimed to conduct a multifactorial analysis based on the Andersen model to determine the extent to which MSD contributes to inequitable dental care use.
Methods
This study used data from the Korea National Health and Nutrition Survey VIII. The study population was 17,903 adults aged 19 years and older. All data were analyzed using IBM SPSS Statistics for Windows version 26 and the level of statistical significance was set at 0.05.
Results
The people with MSD activity limitations were rare as only 3% in this study population. There were significant differences in sex and education as predisposing factors, income, and marital status as enabling factors, and current smoking, daily brushing, and MSD activity limitation as need factors for experiencing economic UDN. MSD activity limitation was associated with 1.5-fold increased odds of Economic UDN with a fully adjusted Anderson’s Behavior Model.
Conclusions
This finding suggests poorer access to dental care among adults with MSDs owing to financial difficulties. It is necessary to explore various ways to address oral health inequalities among adults with MSD activity limitations.
Keywords: Musculoskeletal diseases, Oral health, Dental health services, Healthcare disparities
Background
Oral health is closely related to systemic health, thereby affecting quality of life [1]. Thus, good oral health must be maintained to lead a healthier life [2]. Regular oral examinations and timely access to dental care are essential [3]; otherwise, preventable and simple oral health conditions may become complex and challenging [4, 5]. Oral health is a fundamental right and should be protected as part of comprehensive health [6]; moreover, ensuring access to dental care is also crucial [7]. However, in most countries, dental services are covered less often than other types of health services and are expensive [8, 9]. Unmet dental needs (UDN) are a global public health problem, and financial barriers are one of its major causes [4, 10]. This inability due to financial barriers is a strong indicator of oral health inequality. To reduce oral health inequalities, factors that influence Economic UDN must be identified [10]. People with disabilities are a well-known vulnerable group. Disability refers to a condition that limits a person’s ability to conduct activities of daily living, participate in activities, or interact with others [11]. Oral health is the most commonly unmet health need of people with disabilities [12–14]. Moreover, these people tend to have poorer oral health than people without disabilities [15].
Musculoskeletal disability (MSD) causes problems with bones, muscles, joints, and connective tissue and significantly limits physical activity [16–18]. It is one of the most common and expensive diseases [16, 19], affecting an estimated 1.71 billion people worldwide [20]. People with MSD require social protection and care [4, 21]. MSD is frequent in younger people as well, which is even more problematic in terms of work activity and productivity [22, 23]. Indeed, chronic pain and functional impairment from MSD often lead to loss of productive capacity and unemployment, for example, back pain is reported to be the leading cause of early retirement from work [24]. The Global Burden of Disease, which provides a comprehensive annual assessment of health losses, consistently ranks MSD as the top cause of functional disabilities [23, 25, 26]. It is the most burdensome condition with the longest duration of negative health effects across a lifespan.
Both MSD and oral diseases are potentially serious problems that affect people across their lifespan, but their importance is underestimated because they are often chronic and not life-threatening [27, 28]. MSD has been identified as having a bad influence on oral health. For example, adults with osteoarthritis and rheumatoid arthritis (RA) have difficulties performing the fine motions of toothbrushing, leading to the accumulation of plaque and calculus, which can increase the risk of periodontal infection and dental caries [29–31]. RA patients also tend to have dry mouth which leads to problems in mastication, root caries, dental caries, and periodontal disease [28, 29, 32]. In addition, patients with osteoporosis and cervical spine disorders, are more likely to experience temporomandibular joint dysfunction, decreased alveolar bone density, and mastication disorders due to osteoarticular inflammatory responses [33, 34]. Adults with MSD have higher rates of tooth extraction and filling needs, denture restoration, and prosthodontic needs as well. However, they are less likely to visit the dentist for regular check-ups and preventive care even though they are more likely to be socioeconomically disadvantaged with high dental needs [35, 36].
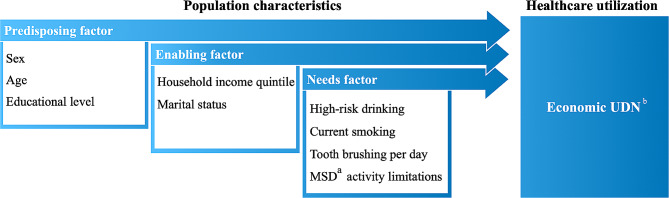
The Andersen model, a representative health behavior model of disease phenomena, suggests that an individual’s disease behavior, such as UDN, can be explained by a combination of predisposing factors, enabling factors, and need factors [37]. Predisposing factors are the inherent characteristics of an individual that precede the onset of disease behavior. Enabling factors are various environmental factors that make it possible. Needs factors most directly contribute to the development of disease behavior, such as MSD [38]. Although each of these factors varies across studies depending on the operationalization and specific population studied, lower education [39], lower income or job security [40], lower insurance coverage [41], and the presence of illnesses and disabilities [39] have generally been associated with higher odds of experiencing UDN. In other words, patients with MSDs who are more likely to be socioeconomically disadvantaged and have a greater burden of medical expenses beyond dental care are expected to have an Economic UDN. It is important to understand the barriers to care faced by patients with MSD, as it is a global problem that affects both social and oral health [42]. This study aimed to conduct a multifactorial analysis based on the Andersen model to determine the extent to which MSD contributes to inequitable dental care use.
Methods
Study design and participants
This study used data from the Korea National Health and Nutrition Survey (KNHANES VIII, 2019–2021), which is a nationwide survey under Article 16 of the National Health Promotion Act conducted every three years in a rotating survey method [43]. The sampling frame was layered according to the size of the area (cities, provinces, and districts) and housing type (general housing or apartments). Finally, 576 districts were surveyed over 3 years, with 10,409 households participating in the study. A total of 22,559 participants were recruited, with a response rate of 74.0%. Among them, 17,903 people were adults aged 19 years and older, which was 79.4% of all participants. This study used data from the Korea National Health and Nutrition Survey (KNHANES VIII, 2019–2021). The KNHANES was conducted with participants’ informed consent by themselves or a legal guardian for those aged under 18 after approval by the Research Ethics Review Committee for the Korea Disease Control and Prevention Agency (KDCA) (IRB No. 2018-01-03-C-A, 2018-01-03–2 C-A, 2018-01-03–3 C-A). This analytical study was approved again by the Institutional Review Board of Kyung Hee University (IRB No. KHSIRB-21-337) and given exemption from review because the retrospective analysis included the dataset from a national survey and did not contain personally identifiable information. All methods were performed following the survey guidelines and regulations.
Variables
The analytical model used in this study, which is based on the Andersen model is shown in Fig. 1. The selection of each factor is based on previous studies that analyzed the factors influencing the UDN using the Andersen model [39, 40, 44]. In the Andersen model, the dependent variable was an individual’s health or disease behavior, such as access to health care. In this study, it was an Economic UDN. This was the answer to a two-step question, (1) “Have you ever needed dental care in the past year but did not receive it? If answered ‘yes’, then (2) “Why is the main reason you needed dental care but did not receive it?” as “economic reasons (because the dental costs were unaffordable).” Population characteristics were divided into three categories: predisposing characteristics, enabling resources, and needs. The predisposing factors were sex, age, and education. The enabling factors were income level and marital status. The needs factors were high-risk drinking, current smoking, daily tooth brushing, and restricted MSD activity. Age was divided into three groups: young adults (20 ~ 44), middle-aged (45 ~ 64), and elderly adults (65 + years). Educational level was grouped as a university degree or higher, high school degree, or middle school degree or lower. Personal income level was expressed as quintiles and marital status was labeled as “yes” if there was a spouse and they lived together and “no” if there was a spouse, but they were separated or no longer living together due to widowhood or divorce. Current smoking status was defined according to the KNHANES guidelines as having smoked more than five packs (100 cigarettes) in his/her lifetime. The answer was dichotomized as “yes” if the respondent currently smoked regular cigarettes and “no” if the respondent smoked fewer than five packs of regular cigarettes in his/her lifetime, did not currently smoke, or had never smoked. Daily toothbrushing was classified by two times. MSD experience was defined as “experienced” if the respondent ticked at least one MSD-related illness item and “not experienced” if the respondent ticked none of the items in the health questionnaire, “What are the reasons for the activity limitations in your daily activities?”. MSD-related illnesses were defined as arthritis, rheumatism, back and neck problems, and knee and leg pain, based on previous studies on musculoskeletal disorders [18].
Fig. 1.
Model of healthcare utilization based on the Andersen conceptual framework
a: MSD (Musculoskeletal disability); b: Economic UDN (Unmet Dental Needs due to Economic reason
Analysis
Since the KNHANES is a national sample survey, the analysis reflects a complex sampling design, including weighting. This study applied complex sample analysis by considering complex sampling design factors, such as strata, clusters, and integration weights. A frequency analysis was conducted to determine the general characteristics of all participants, and a cross-tabulation analysis was conducted to determine whether there was a difference in the experience of Economic UDN according to the variables in each categorical factor. Logistic regression analysis was conducted by sequentially introducing variables to determine how the influence changed according to each category of population characteristic. To determine the correlation between the variables in the model, the Variance Inflation Factor (VIF) was analyzed. VIF > 10 indicated the presence of multicollinearity [45]. All data were analyzed using IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA), and the level of statistical significance was set at 0.05.
Results
Complex sample frequency and cross-tabulation analyses were conducted to identify differences in Economic UDN experiences based on the participants’ general characteristics (Table 1). There were more female participants (51.4%) than male participants. Young people (41.1%) and middle-aged people (40.5%) were similarly represented, whereas the elderly (18.3%) were the least. The proportion of those with a college degree or higher was almost half (43.5%). The proportion of participants who lived alone was 14%, risky drinkers (12.3%), and current smokers (18.5%). Most of the participants brushed more than twice a day (92.4%). The people with MSD activity limitations were rare (2.9%). The percentage of adults who reported not being able to meet their dental needs due to financial reasons during the past year was 8.5%. The proportion of people with Economic UDN difficulties was higher if the participants were female, older, and had lower educational levels as predisposing factors (p < 0.05). Regarding the enabling factors, people with lower income and those living alone had higher rates of Economic UDN (p < 0.05). Among the need factors, current smoking and brushing less than twice daily were associated with higher rates of Economic UDN (p < 0.05). However, there were no statistically significant differences in high-risk drinking between the two groups (p > 0.05). The prevalence of Economic UDN was higher among those with MSD activity limitations (p < 0.05).
Table 1.
Characteristics of the study population by Economic UDN
| Variables | Total | Economic UDNb | ||||
|---|---|---|---|---|---|---|
| N | Weighted % | n | Weighted % | (SE) | p-value | |
| Total | 14,046 | 100 | 1,261 | 8.5 | (0.3) | |
| Predisposing factor | ||||||
| Sex | ||||||
| Male | 6,123 | 48.6 | 502 | 7.9 | (0.4) | 0.036 |
| Female | 7,923 | 51.4 | 759 | 9.0 | (0.4) | |
| Age | ||||||
| 20–44 | 4,606 | 41.1 | 280 | 6.2 | (0.5) | < 0.001 |
| 45–64 | 5,533 | 40.5 | 526 | 9.2 | (0.5) | |
| 65 and more | 3,907 | 18.3 | 455 | 12.0 | (0.6) | |
| Educational level | ||||||
| University and more | 5,163 | 43.5 | 229 | 4.6 | (0.4) | < 0.001 |
| High school | 4,520 | 36.9 | 439 | 9.4 | (0.5) | |
| Middle school and below | 3,607 | 19.6 | 503 | 14.6 | (0.7) | |
| Missing | 765 | |||||
| Enabling factor | ||||||
| Household income quintile | ||||||
| 5th | 2,919 | 21.2 | 83 | 2.3 | (0.3) | < 0.001 |
| 4th | 2,840 | 20.4 | 133 | 4.1 | (0.4) | |
| 3rd | 2,792 | 20.0 | 233 | 7.6 | (0.6) | |
| 2nd | 2,725 | 19.3 | 333 | 11.1 | (0.7) | |
| 1st | 2,717 | 19.1 | 478 | 18.0 | (0.9) | |
| Missing | 53 | |||||
| Marital status | ||||||
| With family | 9,499 | 86.0 | 705 | 7.1 | (0.4) | < 0.001 |
| Alone | 2,044 | 14.0 | 360 | 18.1 | (1.0) | |
| Missing | 2,503 | |||||
| Needs factor | ||||||
| High-risk drinking | ||||||
| No | 12,509 | 87.7 | 1,112 | 8.4 | (0.4) | 0.346 |
| Yes | 1,535 | 12.3 | 149 | 9.2 | (0.9) | |
| Missing | 2 | |||||
| Current smoking | ||||||
| No | 11,789 | 81.5 | 966 | 7.6 | (0.3) | < 0.001 |
| Yes | 2.257 | 18.5 | 295 | 12.3 | (0.8) | |
| Tooth brushing per day | ||||||
| Twice and more | 12,871 | 92.4 | 1,082 | 7.9 | (0.3) | < 0.001 |
| Less than twice | 1,175 | 7.6 | 179 | 14.8 | (1.3) | |
| MSDa activity limitations | ||||||
| No | 13,493 | 97.1 | 1,153 | 8.1 | (0.3) | < 0.001 |
| Yes | 553 | 2.9 | 108 | 20.0 | (2.1) | |
a: MSD (Musculoskeletal disability); b: Economic UDN (Unmet Dental Needs due to Economic reasons
To examine the impact of influencing factors on Economic UDN, hierarchical multiple logistic regression analysis was conducted (Table 2). All values of VIF between the variables were less than 10; therefore, multicollinearity was not observed. First, unadjusted analyses of the predisposing, enabling, and needs variables showed statistical significance in the odds of experiencing Economic UDN, except for high-risk drinking (p < 0.05). The odds of experiencing Economic UDN were 2.8 times higher for those with activity limitations due to MSD than for those without (p < 0.001). The first model analysis, including predisposing factors and MSD activity restriction, only showed that education level had a significant differential effect on experiencing Economic UDN. High school graduates were 2.1 times more likely to experience Economic UDN than those with a university degree or higher and 3.4 times for those with a middle school degree or less (p < 0.001). In Model 2, which included predisposing or enabling factors and MSD activity limitations together, education as a predisposing factor, income and marital status as enabling factors, and MSD activity restriction variables showed statistical significance. The odds of experiencing Economic UDN according to household income showed incremental increase: 1.7, 2.8, 4.5, and 6.4 times higher in each quintile to the baseline income (p < 0.01). Those living alone had a 1.8 times higher risk of Economic UDN than those living with a spouse or partner (p < 0.001). In Model 3, which included all the factors, there were significant differences in sex and education as predisposing factors, income, and marital status as enabling factors, and current smoking, daily brushing, and MSD activity limitation as need factors. The effect of sex was statistically significant only in Model 3 with 1.2 times higher for women than for men (p < 0.05). MSD activity limitation was associated with 2.8-fold increased odds of Economic UDN in the unadjusted model, 2.0 in Model 1, 1.6 in Model 2, and 1.5-fold in Model 3 with a fully adjusted model (p < 0.01).
Table 2.
Complex sample logistic regression analysis regarding influencing factors of economic unmet dental need (UDN)
| (= Reference) | Unadjusted | Model1 | Model2 | Model3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Predisposing factor | ||||||||||||
| Sex (= Male) | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Female | 1.144 | 1.009–1.298 | 0.036 | 1.035 | 0.903–1.186 | 0.620 | 1.013 | 0.857–1.199 | 0.876 | 1.226 | 1.011–1.486 | 0.038 |
| Age (= 20–44) | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| 45–64 | 1.529 | 1.259–1.857 | < 0.001 | 1.165 | 0.950–1.430 | 0.142 | 1.240 | 0.940–1.635 | 0.127 | 1.307 | 0.993–1.722 | 0.057 |
| 65 and more | 2.065 | 1.719–2.480 | < 0.001 | 0.969 | 0.760–1.236 | 0.799 | 1.204 | 0.878–1.650 | 0.249 | 1.335 | 0.972–1.834 | 0.074 |
| Educational level (= University+) | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| High school | 2.172 | 1.764–2.675 | < 0.001 | 2.116 | 1.711–2.617 | < 0.001 | 1.642 | 1.262–2.137 | < 0.001 | 1.551 | 1.192–2.019 | 0.001 |
| Middle school and below | 3.593 | 2.949–4.376 | < 0.001 | 3.388 | 2.657–4.322 | < 0.001 | 2.040 | 1.538–2.706 | < 0.001 | 1.865 | 1.404–2.477 | < 0.001 |
| Enabling factor | ||||||||||||
| Household income quintile (= 5th) | 1.000 | 1.000 | 1.000 | |||||||||
| 4th | 1.831 | 1.329–2.523 | < 0.001 | 1.732 | 1.211–2.478 | 0.003 | 1.727 | 1.206–2.473 | 0.003 | |||
| 3rd | 3.471 | 2.522–4.777 | < 0.001 | 2.889 | 2.027–4.119 | < 0.001 | 2.827 | 1.984–4.026 | < 0.001 | |||
| 2nd | 5.327 | 4.015–7.067 | < 0.001 | 4.528 | 3.270–6.270 | < 0.001 | 4.443 | 3.206–6.158 | < 0.001 | |||
| 1st | 9.299 | 6.878–12.572 | < 0.001 | 6.469 | 4.608–9.081 | < 0.001 | 6.215 | 4.424–8.731 | < 0.001 | |||
| Marital status (= with family) | 1.000 | 1.000 | 1.000 | |||||||||
| Alone | 2.864 | 2.414–3.399 | < 0.001 | 1.882 | 1.547–2.290 | < 0.001 | 1.811 | 1.494–2.195 | < 0.001 | |||
| Needs factor | ||||||||||||
| High-risk drinking (= No) | 1.000 | 1.000 | ||||||||||
| Yes | 0.903 | 0.729–1.117 | 0.346 | 0.953 | 0.715–1.271 | 0.743 | ||||||
| Current smoking (= No) | 1.000 | 1.000 | ||||||||||
| Yes | 1.698 | 1.437–2.006 | < 0.001 | 1.575 | 1.262–1.965 | < 0.001 | ||||||
| Tooth brushing per day (= twice+) | 1.000 | 1.000 | ||||||||||
| Less than twice | 2.009 | 1.625–2.484 | < 0.001 | 1.469 | 1.144–1.885 | 0.003 | ||||||
| MSDa activity limitations (= No) | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 2.829 | 2.139–3.742 | < 0.001 | 2.009 | 1.501–2.687 | < 0.001 | 1.554 | 1.142–2.116 | 0.005 | 1.528 | 1.126–2.073 | 0.007 |
| Nagelkerke r² | 0.048 | 0.121 | 0.128 | |||||||||
a: MSD (Musculoskeletal disability); b: Economic UDN (Unmet Dental Needs due to Economic reasons
*Model 1: adjusted for predisposing factors and MSD activity limitation in Needs factors, Model 2: Model 1 plus Enabling factors, Model 3: Model 2 plus needs factors
Discussion
MSDs mostly have adverse effects on oral health. Patients with MSDs may be at risk of the financial burden of UDN due to reduced productivity and ongoing medical expenses. This study determined the likelihood of Economic UDN among adults with MSDs and examined multiple influencing factors using the Andersen model.
Adults with MSDs were 1.5 times more likely to experience Economic UDN than those without MSD. This finding is similar to that of previous research on dental care utilization among disabled people, indicating poorer access to dental care among adults with MSDs [14]. A study from 15 European Union countries found that MSDs were a major cause of lost working days, 50% of absences over three days, 49% of absences over two weeks, and approximately 60% of early retirements [46]. Work loss and unemployment due to health problems can cause financial difficulties and social isolation. Patients experiencing economic hardship generally tend to forgo dental services [47], particularly vulnerable populations [48]. Dental treatments are mainly not or less covered by governments for health care, so the economic condition has a great impact on the availability of dental services. UDN due to economic reasons can be diminished when the personal economic conditions are improved, or the governments provide financial support. Therefore, governmental support for the dental treatment of vulnerable groups, including those with disabilities, is required.
Among the enabling factors, household income was the most influential factor associated with Economic UDN in the Andersen model. Moreover, a lower income level indicates a higher probability of experiencing Economic UDN by up to 6.21 times. Income has the greatest impact on UDN [49], and the unmet need for dental care is more pronounced in groups with greater economic hardship because of poor public coverage [50]. Out-of-pocket expenses for dental care are higher in South Korea. According to the 2016 World Health Organization (WHO) Health Data, dental coverage in major Organization for Economic Co-operation and Development (OECD) countries was 73.1% on average, while that of Korea was 56.5% [51]. This risk is greater for patients with MSD because they are more likely to have difficulties finding jobs or working life. Dental coverage should be extended to alleviate this burden and increase access to dental care for vulnerable people accordingly.
Men were less likely to experience Economic UDN than women among the predisposing factors. This finding is similar to those of previous studies that explained the reason for the lower incomes for women than those for men [52]. Korea has the largest gender wage gap among the OECD countries [53, 54]. MSDs are more frequent in women; however, the rate of MSD compensation support for female workers was only a quarter of that of male workers [55, 56]. Women with disabilities are more likely to be part-time or temporary employees, putting them at greater risk of living in poverty [57]. These sex inequalities may contribute to the deterioration of inequalities in Economic UDN experienced by people with MSDs.
Those living alone were slightly more likely to experience Economic UDN than those living with a partner or spouse. Married people generally showed higher rates of UDN than single or widowed people [47, 58]. Having someone to live with increases awareness of health care and healthy behaviors, while people living alone tend to lack financial support and help for health care from family members [59, 60]. People with disabilities are mainly cared for by family members; therefore disabled people without family members or cohabitants experience difficulties in daily life, including health care [61]. It is even more devastating for people with MSDs, as they are more likely to experience poverty [16] and difficulties leaving the house owing to physical dysfunction [46]. To ensure dental care for people with MSDs who live alone, policies that support caregivers who can provide appropriate oral health information and accompany them during dental visits are necessary.
Regarding the needs factor, current smokers were more likely to experience Economic UDN than non-smokers, which is similar to the findings of previous studies [62, 63]. Cigarette use is a major factor that negatively affects general and oral health. Smokers are more likely to have poor oral health and higher unmet needs for dental care [64–66]. Furthermore, smoking has serious adverse effects on bones, muscles, tendons, ligaments, and nerves, aggravating MSDs. The American Academy of Orthopedic Surgeons strongly recommends that individuals with MSDs quit smoking. Therefore, future oral health programs for MSDs should consider smoking cessation.
The odds of experiencing Economic UDN were higher for those who brushed less than twice a day than for those who brushed more than twice a day, which is similar to the findings of previous studies [67]. People with MSDs brush less often than the general population [68]. They tend to experience stiffness and pain in their finger joints, which is associated with dysfunction [69, 70]. This makes it difficult for them to maintain their oral hygiene, leading to higher plaque accumulation [68]. Experts recommend the use of high-fluoride toothpaste, chlorhexidine mouthwash, and electric toothbrushes for individuals with limited mobility due to joint pain [71]. Therefore, it is necessary to provide more oral health information to people with MSDs.
The limitations of this study were as follows. First, the KNHANES used in this study is a cross-sectional study; thus, the timing of the observed outcomes cannot be identified. Further research is needed to determine the time order between the diagnosis of MSDs and the occurrence of UDN using longitudinal data, such as panel data. Second, this study focused on Economic UDN and did not explore other causes of UDN. Several UDN reasons, such as lack of time, mildness of symptoms, and inconvenience of transport, have been investigated in the KNHANES; therefore, it would be meaningful to examine various reasons for UDN that are predominantly experienced by people with MSDs. Lastly, this study only used survey data from the KNHANES and did not include diagnostic data. Future studies should combine survey data and MSD diagnosis or dental examination data to better understand the relationship between dental healthcare utilization and actual oral health status among people with MSDs. This study confirmed that MSD activity limitations affect Economic UDN using Korean national-level research data and comprehensively examined and suggested various influencing factors. The findings of this study may provide a basis for institutional policies and intervention programs to address oral health inequalities among patients with MSDs.
Conclusions
This study analyzed the impact of MSD activity limitations on Economic UDN in adults using the 8th KNHANES. Adults with MSD were more likely to have UDN due to economic reasons even after adjusting all factors in Anderson’s behavior model. This finding suggests poorer access to dental care among adults with MSDs owing to financial difficulties. It is necessary to explore various ways to address oral health inequalities among adults with MSD activity limitations, for example, providing socioeconomic support, dental care services, or oral health promotions.
Acknowledgements
Not applicable.
Abbreviations
- MSD
Musculoskeletal Disability
- UDN
Unmet Dental Need
- KNHANES
Korea National Health and Nutrition Survey
- RA
Rheumatoid Arthritis
- KDCA
Korea Disease Control and Prevention Agency
- IRB
the Institutional Review Board
- SPSS
Statistical Packages for Social Science
- WHO
World Health Organization
- OECD
Organization for Economic Co-operation, and Development
Author contributions
All authors, including Tak NY and Ryu JI, participated in the design of the study. All authors together analysed the data, wrote, revised, read, and approved the final version of the manuscript.
Funding
The study was supported by the National Research Foundation of Korea (NRF) grant, Ministry of Science, and ICT (MIST), Republic of Korea, under Grant number 2021R1F1A1063105.
Data availability
The 8th KNHANES data that support the findings of this study are available from the Korea Centre for Disease Control and Prevention Agency (KCDC). Restrictions apply to the availability of these data, which were used under license for this study. Data are available at https://knhanes.kdca.go.kr/knhanes/eng/index.do with the permission of the KCDC.
Declarations
Ethics approval and consent to participate
This study used data from the Korea National Health and Nutrition Survey (KNHANES VIII, 2019–2021). The KNHANES was conducted with participants’ informed consent by themselves or a legal guardian for those aged under 18 after approval by the Research Ethics Review Committee for the Korea Disease Control and Prevention Agency (KDCA) (IRB No. 2018-01-03-C-A, 2018-01-03–2 C-A, 2018-01-03–3 C-A). This analytical study was approved again by the Institutional Review Board of Kyung Hee University (IRB No. KHSIRB-21-337) and given exemption from review because the retrospective analysis included the dataset from a national survey and did not contain personally identifiable information. All methods were performed following the survey guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Global oral health status report: towards universal health coverage for oral health by 2030. In. Geneva: World Health Organization; 2022. pp. 1–120. [Google Scholar]
- 2.Baiju RM, Peter E, Varghese NO, Sivaram R. Oral health and quality of life: current concepts. J Clin Diagn Res. 2017;11(6):ZE21–6. doi: 10.7860/JCDR/2017/25866.10110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saito M, Shimazaki Y, Fukai K, Furuta M, Aida J, Ando Y, Miyazaki H, Kambara M. A multilevel analysis of the importance of oral health instructions for preventing tooth loss: the 8020 Promotion Foundation Study of Japanese Dental patients. BMC Oral Health. 2020;20(1):328. doi: 10.1186/s12903-020-01319-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uhlig T, Moe RH, Kvien TK. The burden of disease in rheumatoid arthritis. PharmacoEconomics. 2014;32(9):841–51. doi: 10.1007/s40273-014-0174-6. [DOI] [PubMed] [Google Scholar]
- 5.Malecki K, Wisk LE, Walsh M, McWilliams C, Eggers S, Olson M. Oral health equity and unmet dental care needs in a population-based sample: findings from the Survey of the Health of Wisconsin. Am J Public Health. 2015;105(Suppl 3):S466–474. doi: 10.2105/AJPH.2014.302338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jean G, Kruger E, Lok V. Oral health as a human right: support for a rights-based Approach to oral Health System Design. Int Dent J. 2021;71(5):353–7. doi: 10.1016/j.identj.2020.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghoneim A, Ebnahmady A, D’Souza V, Parbhakar KK, He H, Gerbig M, Singhal S, Quinonez C. The impact of dental care programs on healthcare system and societal outcomes: a scoping review. BMC Health Serv Res. 2022;22(1):1574. doi: 10.1186/s12913-022-08951-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allin S, Farmer J, Quinonez C, Peckham A, Marchildon G, Panteli D, Henschke C, Fattore G, Lamloum D, Holden ACL, et al. Do health systems cover the mouth? Comparing dental care coverage for older adults in eight jurisdictions. Health Policy. 2020;124(9):998–1007. doi: 10.1016/j.healthpol.2020.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Vujicic M, Buchmueller T, Klein R. Dental Care presents the highest level of Financial barriers, compared to other types of Health Care services. Health Aff. 2016;35(12):2176–82. doi: 10.1377/hlthaff.2016.0800. [DOI] [PubMed] [Google Scholar]
- 10.Taylor H, Holmes AM, Blackburn J. Prevalence of and factors associated with unmet dental need among the US adult population in 2016. Community Dent Oral Epidemiol. 2021;49(4):346–53. doi: 10.1111/cdoe.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.International Classification of Functioning, Disability and Health (ICF) [https://icd.who.int/dev11/l-icf/en]
- 12.Salvador-Carulla L, Symonds S. Health services use and costs in people with intellectual disability: building a context knowledge base for evidence-informed policy. Curr Opin Psychiatry. 2016;29(2):89–94. doi: 10.1097/YCO.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 13.Azadnia A, Mohamadi Bolbanabad A, Safari H, Afkhamzadeh A, Piroozi B, Ghamari D, Khosravi S, Banafshi Z, Ebrahimi R. Self-reported unmet health needs of adults with disabilities in Kurdistan, Iran. Int J Hum Rights Healthc 2022, ahead-of-print.
- 14.Chavis SE, Macek M. Impact of disability diagnosis on dental care use for adults in the United States: status matters. J Am Dent Assoc. 2022;153(8):797–804. doi: 10.1016/j.adaj.2022.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.da Rosa SV, Moyses SJ, Theis LC, Soares RC, Moyses ST, Werneck RI, Rocha JS. Barriers in Access to Dental Services Hindering the Treatment of People with Disabilities: A Systematic Review. Int J Dent 2020, 2020:9074618. [DOI] [PMC free article] [PubMed]
- 16.Georgopoulos V, Akin-Akinyosoye K, Zhang W, McWilliams DF, Hendrick P, Walsh DA. Quantitative sensory testing and predicting outcomes for musculoskeletal pain, disability, and negative affect: a systematic review and meta-analysis. Pain. 2019;160(9):1920–32. doi: 10.1097/j.pain.0000000000001590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomez-Galan M, Perez-Alonso J, Callejon-Ferre AJ, Lopez-Martinez J. Musculoskeletal disorders: OWAS review. Ind Health. 2017;55(4):314–37. doi: 10.2486/indhealth.2016-0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu S, Wang B, Fan S, Wang Y, Zhan Y, Ye D. Global burden of musculoskeletal disorders and attributable factors in 204 countries and territories: a secondary analysis of the global burden of Disease 2019 study. BMJ Open. 2022;12(6):e062183. doi: 10.1136/bmjopen-2022-062183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Academies of Sciences Engineering Medicine, Health and, Division M, Board on Health Care Services, Committee on Identifying Disabling Medical Conditions Likely to Improve with Treatment: Selected Health Conditions and Likelihood of Improvement with Treatment. Washington (DC); 2020.
- 20.Disability. and health [https://www.who.int/news-room/fact-sheets/detail/disability-and-health]
- 21.Elderly people statistics [https://sgis.kostat.go.kr/publicsmodel]
- 22.Henschke N, Harrison C, McKay D, Broderick C, Latimer J, Britt H, Maher CG. Musculoskeletal conditions in children and adolescents managed in Australian primary care. BMC Musculoskelet Disord. 2014;15:164. doi: 10.1186/1471-2474-15-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Musculoskeletal. health [https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions]
- 24.Yelin E, Weinstein S, King T. The burden of musculoskeletal diseases in the United States. Semin Arthritis Rheum. 2016;46(3):259–60. doi: 10.1016/j.semarthrit.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 25.Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The Global Burden of Musculoskeletal Pain-where to from Here? Am J Public Health. 2019;109(1):35–40. doi: 10.2105/AJPH.2018.304747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DALYs GBD, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1859–922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelsey JL, Lamster IB. Influence of musculoskeletal conditions on oral health among older adults. Am J Public Health. 2008;98(7):1177–83. doi: 10.2105/AJPH.2007.129429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.da Silva AP, Bissada NF. Arthritis and Periodontitis: An Association debated for over two centuries. Curr Rheumatol Rev. 2016;12(3):202–7. doi: 10.2174/1573397111666151026223058. [DOI] [PubMed] [Google Scholar]
- 29.Tang Q, Fu H, Qin B, Hu Z, Liu Y, Liang Y, Zhou L, Yang Z, Zhong R. A possible link between rheumatoid arthritis and periodontitis: a systematic review and Meta-analysis. Int J Periodontics Restor Dent. 2017;37(1):79–86. doi: 10.11607/prd.2656. [DOI] [PubMed] [Google Scholar]
- 30.Callhoff J, Dietrich T, Chubrieva M, Klotsche J, Zink A. A patient-reported questionnaire developed in a German early arthritis cohort to assess periodontitis in patients with rheumatoid arthritis. Arthritis Res Ther. 2019;21(1):197. doi: 10.1186/s13075-019-1982-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mercado F, Marshall RI, Klestov AC, Bartold PM. Is there a relationship between rheumatoid arthritis and periodontal disease? J Clin Periodontol. 2000;27(4):267–72. doi: 10.1034/j.1600-051x.2000.027004267.x. [DOI] [PubMed] [Google Scholar]
- 32.Coburn BW, Sayles HR, Payne JB, Redman RS, Markt JC, Beatty MW, Griffiths GR, McGowan DJ, Mikuls TR. Performance of self-reported measures for periodontitis in rheumatoid arthritis and osteoarthritis. J Periodontol. 2015;86(1):16–26. doi: 10.1902/jop.2014.140339. [DOI] [PubMed] [Google Scholar]
- 33.Witulski S, Vogl TJ, Rehart S, Ottl P. Evaluation of the TMJ by means of clinical TMD examination and MRI diagnostics in patients with rheumatoid arthritis. Biomed Res Int. 2014;2014:328560. doi: 10.1155/2014/328560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sadura-Sieklucka T, Gebicki J, Sokolowska B, Markowski P, Tarnacka B. Temporomandibular joint disorders in patients with rheumatoid arthritis. Reumatologia. 2021;59(3):161–8. doi: 10.5114/reum.2021.107593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martinez-Martinez RE, Dominguez-Perez RA, Sancho-Mata J, Abud-Mendoza C, Ayala-Herrera JL, Popoca-Hernandez EA. The frequency and severity of dental caries, and counts of cariogenic bacteria in rheumatoid arthritis patients. Dent Med Probl. 2019;56(2):137–42. doi: 10.17219/dmp/105340. [DOI] [PubMed] [Google Scholar]
- 36.Mok MY, Kong WY, Leung KCM, Chow MK, Lo Y, Tsang CPL, Fung HKK, Lau WCS, Leung WK. Severe Periodontitis Is a Major Contributory Factor to Unmet Dental Healthcare Needs among Rheumatoid Arthritis Patients in Hong Kong. Int J Dent 2022, 2022:8710880. [DOI] [PMC free article] [PubMed]
- 37.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 38.Hajek A, Kretzler B, Konig HH. Determinants of Dental Service Use based on the Andersen Model: a study protocol for a systematic review. Healthc (Basel) 2020, 8(3). [DOI] [PMC free article] [PubMed]
- 39.Gaskin DJ, Zare H, McCleary R, Kanwar O, Davis AL. Predictors of Unmet Dental Health Needs in US adults in 2018: a cross-sectional analysis. JDR Clin Trans Res. 2022;7(4):398–406. doi: 10.1177/23800844211035669. [DOI] [PubMed] [Google Scholar]
- 40.Choi JW, Choi Y, Lee TH, Lee HJ, Ju YJ, Park EC. Employment status and unmet dental care needs in South Korea: a population-based panel study. BMJ Open. 2019;9(3):e022436. doi: 10.1136/bmjopen-2018-022436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jang Y, Yoon H, Park NS, Chiriboga DA, Kim MT. Dental care utilization and unmet dental needs in older Korean americans. J Aging Health. 2014;26(6):1047–59. doi: 10.1177/0898264314538663. [DOI] [PubMed] [Google Scholar]
- 42.Williams A, Kamper SJ, Wiggers JH, O’Brien KM, Lee H, Wolfenden L, Yoong SL, Robson E, McAuley JH, Hartvigsen J, et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16(1):167. doi: 10.1186/s12916-018-1151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Korea Disease Control and Prevention Agency . The eighth Korea National Health and Nutrition Examination Survey (KNHANES VIII-3) analysis Guideline. In. Osong: Ministry of Health and Welfare; 2021. pp. 1–312. [Google Scholar]
- 44.Wiener RC, Sambamoorthi U, Shen C, Alwhaibi M, Findley P. Food Security and Unmet Dental Care needs in adults in the United States. J Dent Hyg. 2018;92(3):14–22. [PMC free article] [PubMed] [Google Scholar]
- 45.Hair JF. Multivariate data analysis. 7. Upper Saddle River, NJ: Prentice Hall; 2010. [Google Scholar]
- 46.Bevan S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract Res Clin Rheumatol. 2015;29(3):356–73. doi: 10.1016/j.berh.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 47.Amoak D, Braimah JA, Agyemang-Duah W, Sano Y, Osei-Kye N, Anfaara FW, Antabe R, Dassah E. Understanding the association between unmet dental care needs and household food security status among older people in Ghana. BMC Oral Health. 2023;23(1):323. doi: 10.1186/s12903-023-03019-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Calzon Fernandez S, Fernandez Ajuria A, Martin JJ, Murphy MJ. The impact of the economic crisis on unmet dental care needs in Spain. J Epidemiol Community Health. 2015;69(9):880–5. doi: 10.1136/jech-2014-204493. [DOI] [PubMed] [Google Scholar]
- 49.Ghanbarzadegan A, Balasubramanian M, Luzzi L, Brennan D, Bastani P. Inequality in dental services: a scoping review on the role of access toward achieving universal health coverage in oral health. BMC Oral Health. 2021;21(1):404. doi: 10.1186/s12903-021-01765-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Northridge ME, Kumar A, Kaur R. Disparities in Access to oral Health Care. Annu Rev Public Health. 2020;41:513–35. doi: 10.1146/annurev-publhealth-040119-094318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization . World health statistics 2016: monitoring health for the SDGs, sustainable development goals. In. Geneva: World Health Organization; 2016. [Google Scholar]
- 52.Socias ME, Koehoorn M, Shoveller J. Gender inequalities in Access to Health Care among adults living in British Columbia, Canada. Women’s Health Issues: Official Publication Jacobs Inst Women’s Health. 2016;26(1):74–9. doi: 10.1016/j.whi.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 53.Gender. equality and work [https://www.oecd.org/stories/gender/gender-equality-and-work]
- 54.Gender wage gap [https://data.oecd.org/earnwage/gender-wage-gap.htm]
- 55.Hunter TM, Boytsov NN, Zhang X, Schroeder K, Michaud K, Araujo AB. Prevalence of rheumatoid arthritis in the United States adult population in healthcare claims databases, 2004–2014. Rheumatol Int. 2017;37(9):1551–7. doi: 10.1007/s00296-017-3726-1. [DOI] [PubMed] [Google Scholar]
- 56.Gikaro JM, Xiong H, Lin F. Activity limitation and participation restriction in Osteoarthritis and rheumatoid arthritis: findings based on the National Health and Nutritional Examination Survey. BMC Musculoskelet Disord. 2022;23(1):647. doi: 10.1186/s12891-022-05607-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pough L, Eid N. Disability employment gap among women and girls with disabilities. In.: Ruh Global IMPACT; 2021.
- 58.Inoue Y, Zaitsu T, Oshiro A, Ishimaru M, Taira K, Takahashi H, Aida J, Tamiya N. Association of marital status and access to dental care among the Japanese population: a cross-sectional study. BMC Oral Health. 2022;22(1):278. doi: 10.1186/s12903-022-02311-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Portacolone E, Nguyen TT, Bowers BJ, Johnson JK, Kotwal AA, Stone RI, Keiser S, Tran T, Rivera E, Martinez P, et al. Perceptions of the Role of Living Alone in Providing Services to patients with cognitive impairment. JAMA Netw Open. 2023;6(8):e2329913. doi: 10.1001/jamanetworkopen.2023.29913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenwohl-Mack A, Dubbin L, Chodos A, Dulaney S, Fang ML, Merrilees J, Portacolone E. Use of services by people living alone with cognitive impairment: a systematic review. Innov Aging. 2021;5(1):igab004. doi: 10.1093/geroni/igab004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim SH, Lee MK, Oh WC, Oh DE, HJ H, Oh MA, Kim JM, Lee YH, Kang DW, Gwon SJ et al. 2020 Survey on the Status of Persons with Disabilities. In. Edited by Center of Rehabilitation Support. Sejong: Ministry of Health and Welfare; 2020: 1-751.
- 62.More AB, Rodrigues A, Sadhu BJ. Effects of smoking on oral health: awareness among dental patients and their attitude towards its cessation. Indian J Dent Res. 2021;32(1):23–6. doi: 10.4103/ijdr.IJDR_711_18. [DOI] [PubMed] [Google Scholar]
- 63.Jang JH, Kim JL, Kim JH. Associations between Dental checkups and Unmet Dental Care needs: an examination of cross-sectional data from the Seventh Korea National Health and Nutrition Examination Survey (2016–2018). Int J Environ Res Public Health 2021, 18(7). [DOI] [PMC free article] [PubMed]
- 64.Sigaux J, Biton J, Andre E, Semerano L, Boissier MC. Air pollution as a determinant of rheumatoid arthritis. Joint Bone Spine. 2019;86(1):37–42. doi: 10.1016/j.jbspin.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 65.Conigliaro P, Triggianese P, De Martino E, Fonti GL, Chimenti MS, Sunzini F, Viola A, Canofari C, Perricone R. Challenges in the treatment of rheumatoid arthritis. Autoimmun rev. 2019;18(7):706–13. doi: 10.1016/j.autrev.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 66.Degens H, Gayan-Ramirez G, van Hees HW. Smoking-induced skeletal muscle dysfunction: from evidence to mechanisms. Am J Respir Crit Care Med. 2015;191(6):620–5. doi: 10.1164/rccm.201410-1830PP. [DOI] [PubMed] [Google Scholar]
- 67.Shim HS, Kim SS, Kim JH. Influencing factors of non-utilization of dental care among adults in Korea: using 2012 Korean National Health and Nutrition Survey. J Korean Soc Dent Hygiene. 2015;15(5):823–9. doi: 10.13065/jksdh.2015.15.05.823. [DOI] [Google Scholar]
- 68.Ahmad I, Togoo RA, DS MA, AA MA, DA OA, Mukherjee D, Alharthi MS, Ahmad F, Ahmed H, Hasan S et al. Influence of Joint Flexibility, Hand grip Strength and Pain on oral Hygiene in Musculoskeletal Disorders-A non-interventional clinical study. J Clin Med 2023, 12(6). [DOI] [PMC free article] [PubMed]
- 69.El-Sherif HE, Kamal R, Moawyah O. Hand osteoarthritis and bone mineral density in postmenopausal women; clinical relevance to hand function, pain and disability. Osteoarthritis and cartilage / OARS. Osteoarthr Res Soc. 2008;16(1):12–7. doi: 10.1016/j.joca.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 70.Henderson J, Condell J, Connolly J, Kelly D, Curran K. Review of Wearable Sensor-Based Health Monitoring Glove devices for Rheumatoid Arthritis. Sens (Basel) 2021, 21(5). [DOI] [PMC free article] [PubMed]
- 71.Slot DE, Lindeboom R, Rosema NA, Timmerman MF, van der Weijden GA. The effect of 0.12% chlorhexidine dentifrice gel on plaque accumulation: a 3-day non-brushing model. Int J Dental Hygiene. 2007;5(1):45–52. doi: 10.1111/j.1601-5037.2007.00227.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The 8th KNHANES data that support the findings of this study are available from the Korea Centre for Disease Control and Prevention Agency (KCDC). Restrictions apply to the availability of these data, which were used under license for this study. Data are available at https://knhanes.kdca.go.kr/knhanes/eng/index.do with the permission of the KCDC.