The use of antithrombotic therapy in acute coronary syndromes has reduced the incidence of death and Q wave myocardial infarction dramatically in recent years. Antithrombotic drugs in routine use include antiplatelet drugs (aspirin, clopidogrel, and glycoprotein IIb/IIIa receptor antagonists) and anticoagulants (unfractionated and low molecular weight heparin, warfarin, and direct thrombin inhibitors).
Pathogenesis
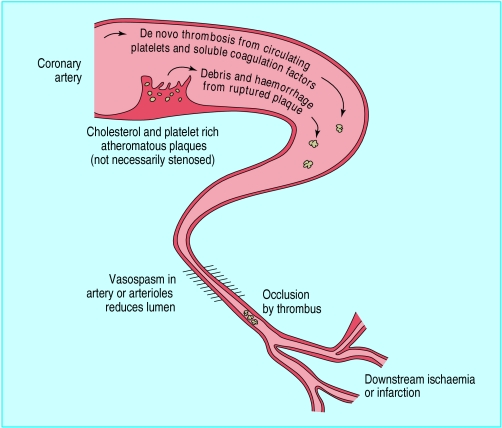
Thrombosis is the basic pathophysiological process underlying the acute coronary syndromes. Thus, antithrombotic therapy is the cornerstone of management, and the appropriate choice of antithrombotic drugs to reduce platelet aggregation or interfere with the clotting process can be critical.
Rupture of the fibrous cap of an atheromatous plaque exposes the lipid core, which is highly thrombogenic and contains an abundance of procoagulant tissue factor. Plaque rupture (exposing surface binding glycoproteins) allows platelets to adhere to the plaque, become activated, and release thromboxane A2, which causes further platelet aggregation and vasoconstriction. As the platelets aggregate around the ruptured plaque, membrane glycoprotein IIb/IIIa receptors undergo a configuration change to bind fibrinogen and form a complex platelet linkage. Further incorporation of fibrin and red blood cells within this platelet-rich thrombus results in a partial or total occlusion of the coronary artery. Alternatively, thrombus may break off from a ruptured plaque and occlude a downstream vessel. Occlusion may also follow from trapping of circulating thrombi formed elsewhere in the circulation.
Antithrombotic drugs
Antiplatelet drugs
Aspirin
Aspirin has been in use for more than 150 years and is cheap and effective. It has been shown to reduce the risk of fatal and non-fatal myocardial infarction by at least 50% in patients with unstable angina. Aspirin blocks cyclo-oxygenase and formation of thromboxane A2, thus reducing platelet aggregation induced via this pathway.
Aspirin is the cornerstone of treatment in acute coronary syndromes and chronic coronary artery disease. The beneficial effects of aspirin seem to be sustained for at least two years and regardless of the dose used. However, 75-150 mg daily may have a lower incidence of gastrointestinal side effects than the higher doses used in some randomised studies.
ADP receptor antagonists
Ticlopidine and clopidogrel are ADP inhibitors. Evidence exists that ticlopidine reduces mortality, recurrent infarction, stroke, and angina at least to six months after myocardial infarction or unstable angina. Ticlodipine has fewer gastrointestinal effects than aspirin but may cause reversible neutropenia and thrombocytopenia (<1% of patients), which dictates therapeutic monitoring with regular blood counts.
Clopidogrel is a derivative of ticlopidine that seems to be six times more effective than its predecessor in preventing platelet aggregation. Clopidogrel has shown better tolerability with less bleeding than aspirin and fewer haematological side effects than ticlopidine. In the CURE trial—a randomised, double blind, parallel group study of 12 562 patients with acute coronary syndrome or non-Q wave myocardial infarction—patients received aspirin 75-325 mg and then were randomly assigned to additional clopidogrel (300 mg load followed by 75 mg daily) or placebo for three months to a year. Additional clopidogrel resulted in a 20% relative risk reduction in the primary end point (cardiovascular death, myocardial infarction, or stroke) (P <0.0001), mainly caused by a 23% relative reduction in myocardial infarction. However, there was a 34% excess of major bleeding (3.6% v 2.7% in placebo; P=0.003).
These observations raise the question of whether combination antiplatelet treatment (such as aspirin with clopidogrel) is preferable to other treatments (such as heparin with glycoprotein IIb/IIIa receptor inhibitors) in the acute phase of acute coronary syndromes and suggest that prolonged antiplatelet treatment is better for high risk patients.
Glycoprotein IIb/IIIa receptor inhibitors
Abciximab is a (large molecule) monoclonal antibody and the first glycoprotein IIb/IIIa receptor antagonist to be developed. Eptifibatide is a peptide receptor antagonist, whereas tirofiban is a non-peptide receptor antagonist. Both eptifibatide and tirofiban are small molecules, apparently non-immunogenic, and therefore suitable for repeat infusions. They have a shorter half life (90-120 minutes) than abciximab (12 hours). Because they are mainly renally cleared, their doses should be adjusted in patients with renal impairment.
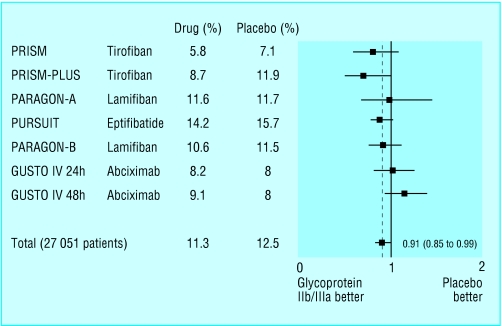
In trials with patients with acute coronary syndromes the rate of death, reinfarction, and refractory angina was reduced when glycoprotein IIb/IIIa inhibitors were added to aspirin and heparin. In the largest study, PURSUIT, a bolus injection of eptifibatide followed by a 72 hour infusion resulted in a 9.6% relative risk reduction in death and myocardial infarction when given to patients with acute coronary syndromes already receiving aspirin and heparin. In the PRISM and PRISM-PLUS studies, tirofiban, when given in addition to aspirin and heparin, achieved a 43% relative risk reduction in mortality and reinfarction at seven days. This benefit was sustained at 30 days. Patients taking tirofiban and aspirin without heparin had an excess mortality rate, and this treatment arm was stopped early.
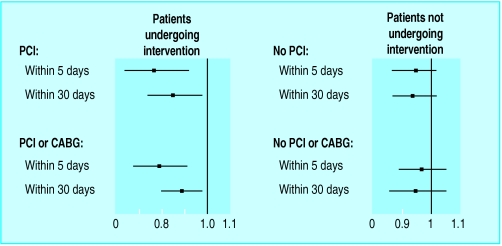
The CAPTURE trial studied patients with acute coronary syndromes scheduled for percutaneous coronary angioplasty. The use of abciximab for about 24 hours before the procedure substantially reduced the risk of mortality, myocardial infarction, or need to proceed to other revascularisation.
The benefits are greatest in patients with elevated levels of troponin T or I, indicating that assessment of subtle indices of cardiac damage predicts patients at higher risk and those most likely to benefit from treatment. Economic evaluations of the costs of using intravenous glycoprotein IIb/IIIa inhibitors suggest that, for patients with elevated troponin levels, 11 are needed to be treated to prevent one death or acute myocardial infarction at 30 days. The equivalent cost effectiveness is about £5000 an outcome.
Using glycoprotein IIb/IIIa inhibitors for acute coronary syndrome in addition to conventional antithrombotic therapy is approved by the British National Institute for Clinical Excellence (NICE). However, interpretation of trial evidence is complicated by patient heterogeneity. Although adjunctive treatment before revascularisation procedures in acute coronary syndromes shows clear benefit, there is some uncertainty of benefit if these drugs are used only as “medical” management without revascularisation.
Anticoagulant treatment
Low molecular weight heparin
Low molecular weight heparins possess more anti-Xa activity than unfractionated heparins. They have a more predictable anticoagulant effect and cause less thrombocytopenia. Titrated appropriately against body weight, low molecular weight heparin provides effective anticoagulation and does not need regular monitoring of the activated partial thromboplastin time. However, platelet count monitoring to detect thrombocytopenia is recommended if treatment is extended beyond a few days. Studies suggest similar safety profiles to unfractionated heparin when used with glycoprotein IIb/IIIa inhibitors.
Antithrombotic therapy is the cornerstone of management in acute coronary syndromes
The therapeutic benefits of low molecular weight heparins are now clear. Recent randomised trials comparing the efficacy of various low molecular weight heparins showed enoxaparin and nadroparin to be more effective in reducing mortality in unstable angina than either aspirin or unfractionated heparin alone. In the ESSENCE study, enoxaparin reduced the incidence of death, myocardial infarction, and reccurent angina at 14 days from 19.6% to 16.6% when compared with unfractionated heparin. This benefit was maintained at 30 days and a year.
Dalteparin in addition to aspirin was more effective than aspirin alone in the FRISC study. It reduced cardiac events and death (1.8% v 4.8%) when used in acute coronary syndromes but was no better than adjusted dose unfractionated heparin.
Low molecular weight heparin is, therefore, at least as good as unfractionated heparin in managing unstable angina (with trials showing enoxaparin and nadroparin to be even better). It has practical advantages because it has more consistent antithrombin effects and is easier to administer, and frequent assessment of antithrombotic effect (activated partial thromboplastin time monitoring) is not neccesary. In view of these findings, low molecular weight heparins (enoxaparin and nadroparin) should be used routinely to treat unstable angina concurrently with aspirin in place of unfractionated heparin.
Unfractionated heparin
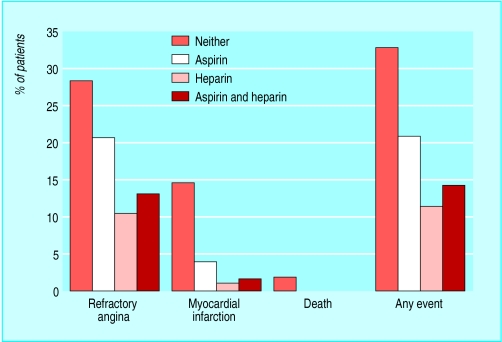
An uncontrolled study showed that heparin treatment in unstable angina reduced the risk of progression to myocardial infarction by 80%. Other studies show a definite reduction in the incidence of refractory angina and myocardial infarction with the use of unfractionated heparin compared with placebo (risk reduction 0.29). Treatment with heparin and aspirin seems to be more effective than either heparin or aspirin alone. In a meta-analysis on the effect of adding heparin to aspirin in patients with unstable angina, combination treatment resulted in 33% reduction in deaths or myocardial infarction.
Direct thrombin inhibitors
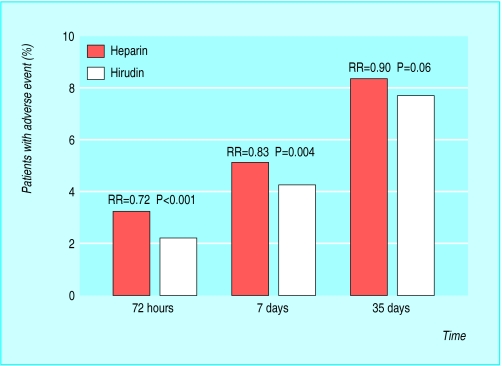
Newer and powerful anticoagulants, such as the direct thrombin inhibitor hirudin, are being investigated. Several trials compared the effects of hirudin with unfractionated heparin and showed a slight reduction in primary end points, and a pooled analysis of these trials showed a 22% relative risk reduction in myocardial infarction or deaths at 72 hours. Bleeding, however, may be a problem. Hirudin is now approved for patients with heparin induced thrombocytopenia but is not yet licensed for treatment of acute coronary syndromes. The direct thrombin inhibitors melagatran and ximelagatran are currently under investigation for use in patients with acute coronary syndromes.
Warfarin
Several trials have investigated using warfarin for unstable angina. In many studies, warfarin was given to patients two days after unfractionated heparin infusion and continued for ten weeks to six months with an international normalised ratio (INR) adjusted to between 2.0 and 3.0. Earlier studies showed low fixed doses of warfarin gave no benefit. However, limited evidence suggests that in patients with acute coronary syndromes, combination treatment with aspirin and warfarin adjusted to INR 2.0-3.0 may reduce event rates and hospitalisations.
Antithrombotic therapy in acute coronary syndromes: a summary
Aspirin
Acute treatment with aspirin is used in all patients with suspected acute coronary syndromes in the absence of contraindications and for long term treatment thereafter
Clopidogrel
In acute coronary syndrome patients clopidogrel is used for acute treatment and for longer term treatment for at least 9-12 months. Beyond this, treatment will depend on the risk status of the patient and individual clinical judgment
Clopidogrel is used for immediate and long term treatment in patients who do not tolerate aspirin and in patients receiving a stent
Clopidogrel is given to acute coronary syndrome patients scheduled for angiography unless there is a likelihood that the patient will proceed to urgent surgery (within 5 days)
Low molecular weight heparin
In aspirin treated patients, low molecular weight heparin is better than placebo. There are also data in favour of low molecular weight heparin (enoxaparin) over unfractionated heparin when administered as an acute regimen
Glycoprotein IIb/IIIa receptor inhibitors
Treatment with a glycoprotein IIb/IIIa receptor blocker is recommended in all patients with acute coronary syndromes undergoing percutaneous coronary interventions. The infusion should be continued for 12 hours (abciximab) or 24 hours (eptifibatide, tirofiban) after the procedure
Medical treatment with a glycoprotein IIb/IIIa receptor blocker during the first days after admission, followed by percutaneous coronary intervention or bypass surgery, yields a significant reduction in death and non-fatal myocardial infarction at 72 hours, from 4.3 to 2.9%
Diabetic patients with acute coronary syndrome derive particular benefit from glycoprotein IIb/IIIa receptor inhibitors
Fibrinolytic treatment
In contrast to acute coronary syndromes with ST segment elevation, thrombolytic therapy is not recommended for patients with acute coronary syndromes without persistent ST segment elevation
Pending further trials and in view of potential bleeding risks and need for INR monitoring, warfarin is best reserved for patients with other indications for warfarin use such as coexistent atrial fibrillation, known left ventricular aneurysm with mural thrombus formation, or previous recurrent thromboembolic stroke. Warfarin should not be used as the sole antithrombotic drug in acute cases because of its delayed onset of action.
Thrombolytic treatment
Thrombolytic treatment is not recommended for unstable angina and non-Q wave infarction. It has not been shown to reduce cardiovascular events and death and may worsen clinical outcomes by increasing bleeding complications, as well as increasing bleeding within a ruptured atherosclerotic plaque. This worsens obstruction to coronary flow and exposes clot-bound thrombin to flowing blood, creating an even more prothrombotic environment. In addition, the thrombus in unstable angina is platelet-rich, unlike the fibrin-rich thrombus seen in infarction, and thus may be less responsive to thrombolytic treatment.
Further reading
Anand SS, Yusuf S, Pogue J, Weitz JI, Flather M. Long term oral anticoagulant therapy in patients with unstable angina or suspected non-Q wave myocardial infarction. The OASIS (warfarin) substudy. Circulation 1998;98:1064-70
British Cardiac Society Guidelines and Medical Practice Committee, and Royal College of Physicians Clinical Effectiveness and Evaluation Unit. Guideline for the management of patients with acute coronary syndrome without persistent ECG ST segment elevation. Heart 2001;85:133-42
The CAPTURE Investigators. Randomised placebo controlled trial of abciximab before and during intervention in refractory unstable angina: The CAPTURE study. Lancet 1997;349:1429-35
Cohen M, Demers C, Gurfinkel EP, Turpie AG, Fromell GJ, Goodman S, et al. A comparison of low molecular weight heparin with unfractionated heparin for unstable coronary artery disease (ESSENCE). N Engl J Med 1997;337:447-52
Fragmin and fast revascularisation during instability in coronary artery disease (FRISC-II) Investigators. Long term low molecular mass heparin in unstable coronary artery disease: FRISC-II prospective multicentre randomised study. Lancet 1999;354:701-7
PRISM-PLUS Investigators. Inhibiton of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non Q-wave myocardial infarction. N Engl J Med 1998;338:1488-97
The PURSUIT Trial Investigators. Inhibiton of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998;339:436-43
National Institute for Clinical Excellence (NICE). Guidance on the use of glycoprotein IIb/IIIa inhibitors in the treatment of acute coronary syndromes. NICE Technology Appraisal Guidance No 12. London: NICE, 2000
Task force on the management of acute coronary syndromes of the European Society of Cardiology. Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2002;23:1809-40
Figure.
Thrombosis in relation to acute coronary syndromes
Figure.

Thrombus within right coronary artery (arrow) in a patient with unstable angina
Figure.
Reduction of adverse events in patients treated with aspirin, heparin, or both compared with neither drug
Figure.

Effects of clopidogrel plus aspirin in patients with acute coronary syndromes without ST segment elevation. From the clopidogrel in unstable angina to prevent recurrent events (CURE) trial investigators
Figure.
Glycoprotein IIb/IIIa inhibitors v conventional treatment in six trials. Results show odds ratio (95% confidence interval) for death and myocardial infarction at 30 day follow up
Figure.
Glycoprotein IIb/IIIa inhibitors in patients with acute coronary syndromes: patients undergoing percutaneous coronary intervention and patients not undergoing percutaneous coronary intervention. Results show odds ratio (95% confidence interval) for death or myocardial infarction (CABG=coronary artery bypass graft surgery, PCI=percutaneous coronary intervention)
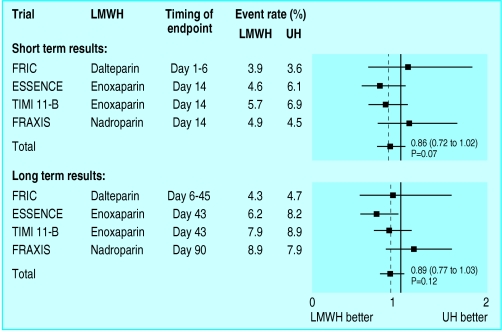
Figure.
Comparison of low molecular weight heparins with unfractionated heparins in patients with acute coronary syndromes. Results show odds ratio (95% confidence interval) for death and myocardial infarction at long and short term follow up (LMWH=low molecular weight heparin, UH=unfractionated heparin)
Figure.
Comparison of hirudin therapy with unfractionated heparin in patients with acute coronary syndromes (RR=relative risk)
Acknowledgments
The figure showing reduction of adverse events in patients treated with aspirin, heparin sodium, or both compared with neither drug is adapted from Theroux P et al, N Engl J Med 1988:319;1105-11. The effects of clopidogrel plus aspirin in patients with acute coronary syndromes is adapted from the CURE trial investigators, N Engl J Med 2001;345: 494-502. The figures showing glycoprotein IIb/IIIa inhibitors v conventional treatment, comparing the effects glycoprotein IIb/IIIa inhibitors in acute coronary syndrome patients who are undergoing percutaneous coronary intervention with those who are not, and comparing low molecular weight heparin with unfractionated heparin in patients with acute coronary syndrome are all adapted from Bertrand M, et al, Eur Heart J 2002;23:1809-40. The figure comparing hirudin treatment with unfractionated heparin in patients with acute coronary syndromes is adapted from Glenn N et al, Arch Intern Med 2001;161:937-48
Footnotes
Robert D S Watson is consultant cardiologist, Bernard S P Chin is research fellow, and Gregory Y H Lip is professor of cardiovascular medicine. All are at the haemostasis thrombosis and vascular biology unit, university department of medicine, City Hospital, Birmingham.
The ABC of antithrombotic therapy is edited by Gregory Y H Lip and Andrew D Blann, senior lecturer in medicine, haemostasis thrombosis and vascular biology unit, university department of medicine, City Hospital, Birmingham. The series will be published as a book in spring 2003.