Acute coronary syndromes
All patients suspected of having acute coronary syndrome should be managed as medical emergencies and monitored in the critical care unit. Baseline tests must include 12 lead electrocardiography, chest x ray examination, and venous blood samples for analyses of haemoglobin and markers of myocardial damage, preferably cardiac troponin T or I.
High and low risk patients with suspected acute coronary syndromes
High risk
Recurrent or persistent chest pains with associated electrocardiographic changes (ST segment depression or transient ST elevation) despite anti-ischaemic treatment
Elevated troponin concentrations
Age >65 years
Comorbidity, especially diabetes
Development of pulmonary oedema or haemodynamic instability within observation period
Development of major arrhythmias (repetitive ventricular tachycardia or ventricular fibrillation)
Early postinfarction unstable angina
Low risk
No recurrence of chest pains within observation period
Troponin or other markers of myocardial damage not elevated
No ST segment depression or elevation on electrocardiogram (T wave inversion is classified as intermediate risk)
Initial management
Assessment
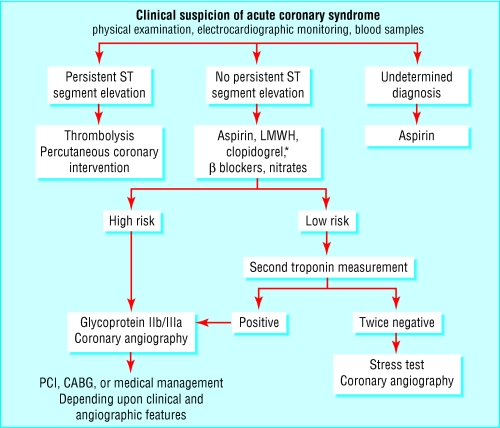
Patients with persistent ST segment elevation on 12 lead electrocardiography need immediate reperfusion treatment (thrombolysis or intervention). Patients with ST segment depression, inverted T waves, or pseudonormalisation of T waves on the electrocardiogram, but with a clinical history suggesting cardiac ischaemia should receive initial treatment for angina.
This would include aspirin 300 mg followed by a low dose of 75-150 mg daily. In cases of aspirin intolerance, clopidogrel should be used. β Blockers and nitrates should also be given. Rate limiting calcium antagonists can be used if β blockers are contraindicated or are already being used. Ideally, patients should be given low molecular weight heparin (enoxaparin) according to their weight. If low molecular weight heparin is unavailable, unfractionated heparin may be used. A bolus of 5000 U is given, followed by an infusion adjusted to get an activated partial thromboplastin time (APTT) ratio of 1.8 to 2.5. In light of data from the CURE and PCI-CURE study, clopidogrel (given for at least one month and up to nine months) should be considered in addition to aspirin when an early non-interventional approach is planned. The optimal dose of aspirin to limit bleeding is probably 75 mg, particularly with clopidogrel. A glycoprotein IIb/IIIa receptor inhibitor should be added to aspirin and heparin for patients in whom catheterisation and percutaneous coronary intervention are planned. In these patients clopidogrel could be considered if they are not at high risk for bleeding.
Management strategies for patients with suspected acute coronary syndromes, with risk stratification by troponin and stress tests*
Low risk
Results of tests
Cardiac troponin result is negative or low (troponin T <0.01 μg/l or troponin I equivalent) on two occasions
Stress test indicates a low risk category
Action
If free from cardiac symptoms, no more cardiac interventions needed
Subsequent outpatient review appropriate for further investigations and adjustment of drug treatment
Intermediate risk
Results of tests
Impaired left ventricular function, or haemodynamic abnormalities or arrhythmia during the acute phase but
Normal cardiac troponin result (troponin T <0.01 μg/l, or troponin I equivalent), with a stress test indicating intermediate risk or
Moderately elevated cardiac troponin (troponin T 0.01-0.1 μg/l, or troponin I equivalent) with stress test indicating low risk category
Action
Many cardiologists perform coronary angiography on these patients, but clear evidence is lacking
High risk
Results of tests
Maximal cardiac troponin result is high (troponin T >0.1 μg/l, or troponin I equivalent) or
Stress test indicates high risk category
Action
Coronary angiography should be arranged, unless contraindicated, and performed urgently, before discharge from hospital
Patients with suitable lesions for percutaneous coronary intervention should be given clopidogrel, which should also be given to patients with coronary lesions not suitable for any revascularisation
*If patient is unable to perform an exercise electrocardiogram, an alternative non-exercise (pharmacological) stress test, such as a stress echocardiograph or isotope myocardial stress perfusion study, should be arranged unless contraindicated. In all cases, aggressive risk factor management and regular aspirin treatment (or clopidogrel, or both, depending on clinical situation) is necessary
Observation
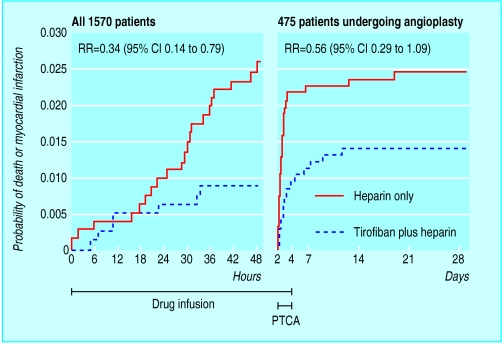
Patients should be observed over the next eight to 12 hours. Patients at high risk of progressing to acute myocardial infarction or death should receive a glycoprotein IIb/IIIa receptor inhibitor (eptifibatide or tirofiban) in addition to heparin and aspirin or clopidogrel (alone or with asprin). Abciximab would be used in high risk patients undergoing percutaneous coronary intervention. There is no role for thrombolytic therapy in patients without acute ST segment elevation, a true posterior myocaridal infarction, or a presumed new left bundle branch block.
Subsequent management
When patients have been free from symptoms and ischaemic electrocardiographic changes for >48 hours, and any intravenous treatments and heparin have been stopped for >24 hours, risk assessment with stress testing should be performed unless contraindicated. Stress testing for risk assessment is unnecessary if a patient is already in a high risk category for which coronary angiography is indicated.
Antithrombotic treatment
Low molecular weight heparin should be given for at least two days, and for up to eight days or longer in cases of recurrent ischaemia or where myocardial revascularisation is delayed or contraindicated. Patients requiring a bypass operation may have their glycoprotein IIb/IIIa receptor antagonist infusion stopped before or at the time of cardiac surgery, although clopidogrel should be withheld for five to seven days.
Risk stratification and antithrombotic strategies
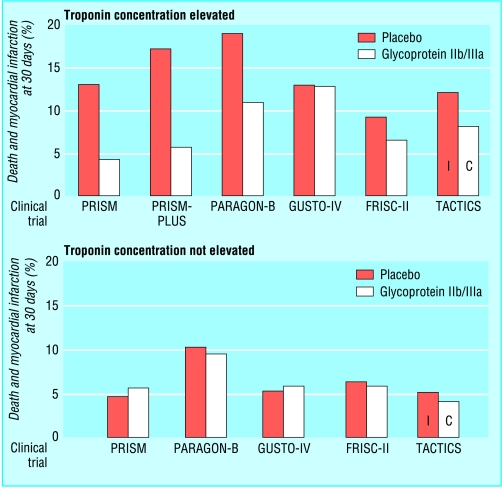
Recent trials have shown that patients with elevated troponin benefit from treatment with low molecular weight heparin, glycoprotein IIb/IIIa blockers, or an invasive strategy, whereas patients without troponin elevation showed no such benefit.
In these high risk patients, angiography with a view to revascularisation should be performed on the same admission. Infusion of glycoprotein IIb/IIIa receptor inhibitors should be started while waiting and preparing for angiography and continued for 12 hours (abciximab) or 24 hours (tirofiban) after angioplasty is performed.
Low risk patients can be mobilised and discharged if (at least 12 hours after the onset of symptoms of a suspected acute coronary syndrome) the symptoms have not recurred, cardiac troponin concentrations are normal, electrocardiograms remain normal (or unchanged compared with a recording from before the current presentation), and cardiac enzyme activities are not raised. Risk assessment with stress testing should be performed before a patient is discharged unless contraindicated.
Pros and cons of invasive strategy
There are arguments for and against an invasive approach to acute coronary syndromes. In the FRISC-II trial an invasive strategy had, after a year, saved 1.7 lives in 100 patients and prevented 2.0 non-fatal myocardial infarctions and 20 readmissions. It provided earlier and better symptom relief at the cost of 15 more patients with coronary artery bypass grafting and 21 more with percutaneous transluminal coronary angioplasty, and these results were independent of treatment with dalteparin or placebo. In the BHF RITA3 trial of patients with unstable angina, myocardial infarction, or non-ST segment elevation, an invasive strategy reduced refractory or severe angina, with no increase of death or myocardial infarction, compared with a conservative strategy. Against these benefits is the need to have adequate provision of facilities and trained staff to undertake such procedures.
Percutaneous coronary intervention
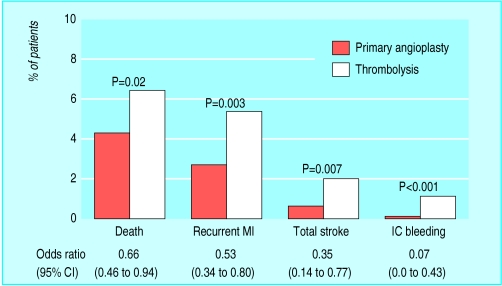
Arterial thrombi occur soon after percutaneous coronary interventions for coronary artery disease, usually at the site of the dilated segment. Arterial thrombi are rich in platelets, red blood cells, fibrin, and leucocytes and may contribute to vessel reocclusion with the consequent need for revascularisation. The risk of reocclusion depends on the extent of segment dilatation and vessel injury, as well as local shear forces. Antiplatelet and antithrombin drugs generally reduce the risk of occlusion or the need for further intervention but are not perfect. Where facilities are available, percutaneous coronary angioplasty is an alternative to thrombolytic treatment as a means of reperfusion in acute myocardial infarction.
Antiplatelet treatment
Patients with coronary artery disease undergoing angioplasty should continue taking antiplatelet drugs as usual. For patients not receiving regular antiplatelet treatment, aspirin 100-325 mg should be given orally at least two hours before angioplasty.
Aspirin substantially reduces the rate of intracoronary thrombus formation at the treatment site and restenoses. The addition of dipyridamole to aspirin adds little extra benefit and is not recommended. Ticlopidine alone has not been shown to be more effective than aspirin alone in patients undergoing percutaneous interventions. Although clopidogrel is marginally better than aspirin in patients with atherosclerotic vascular disease (CAPRIE study), direct comparisons between aspirin and clopidogrel in coronary intervention have not revealed marked differences. Thus, ticlopidine and clopidogrel are useful alternatives for patients scheduled for percutaneous coronary angioplasty who are unable to take aspirin.
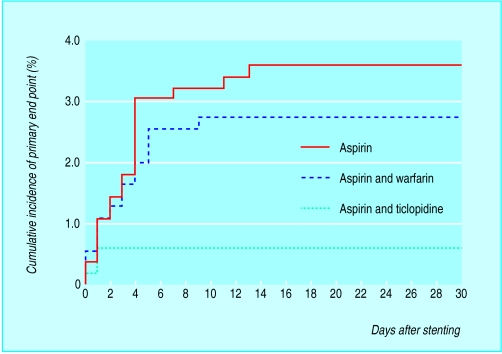
After intervention, antiplatelet combination treatment (aspirin plus ticlopidine) is superior to aspirin alone at reducing ischaemic complications and cardiac events, particularly after intracoronary stent placements. The stent anticoagulation restenosis investigators (SARI) trial, compared aspirin-ticlopidine combination treatment with aspirin-warfarin combination treatment and aspirin alone and showed that patients taking aspirin-ticlopidine had the best 30 day mortality (0.5% v 2.7% v 3.6% respectively, P=0.001). Total bleeding complications occurred in 5.5% of those taking aspirin-ticlopidine, quite high when compared with 1.8% in those taking aspirin only (P<0.001), and the incidence of neutropenia was not significantly different. The CLASSICS trial showed clopidogrel-aspirin combination treatment to be as effective as ticlopidine-aspirin combination treatment after angioplasty and stent placement.
Glycoprotein IIb/IIIa receptor antagonists
Despite adequate treatment with antiplatelet drugs, platelet activation still continues along other pathways not blocked by these agents. This is where the glycoprotein IIb/IIIa receptor antagonists, which block the final common pathways of platelet aggregation, have contributed most to the management of angioplasty and stenting.
Some factors prediposing to in stent thrombosis after placement
| • Underdilation of the stent | • Poor inflow |
| • Proximal and distal dissections | • Outflow obstruction |
| • Vessel diameter <3 mm | |
Abciximab, eptifibatide, and tirofiban have all been shown to reduce reocclusion and cardiovascular events, including deaths and myocardial infarctions, at 30 days when used in patients undergoing elective and urgent angioplasty and stenting. These benefits are additional to those achieved with antiplatelet drugs, and the effects were most prominent with abciximab. The EPIC, EPILOG, and CAPTURE trials all showed that abciximab infusion reduced major complication rates during balloon angioplasty, a benefit that was sustained at 30 days' follow up. The EPISTENT trial showed that abciximab reduces major complications during stent placement and was superior to a combination of abciximab and balloon angioplasty. In the only direct comparison of glycoprotein IIb/IIIa antagonists, the TARGET trial randomised 5308 patients to tirofiban or abciximab before percutaneous transluminal coronary angioplasty or stent, or both: by six months the primary end point was similar in both treatment arms (14.9% with tirofiban v 14.3% with abciximab, P>0.05), as was mortality (1.9% v 1.7%, P>0.05). Patients with unstable angina, acute myocardial infarction, and other risk factors (such as diabetes) for postprocedure in stent thrombosis or restenosis stand to benefit most from glycoprotein IIb/IIIa receptor antagonists.
In light of this, glycoprotien IIb/IIIa drugs should be considered in all patients at risk of developing in stent stenosis or with acute coronary syndrome scheduled for percutaneous coronary interventions. If percutaneous coronary intervention is planned in unstable angina, glycoprotein IIb/IIIa receptor antagonist infusions should be started before intervention and continued for 12 hours (abciximab) or 24 hours (tirofiban, eptifibatide) after the procedure.
Several economic evaluations have found that routine use of glycoprotein IIb/IIIa drugs after percutaneous coronary interventions is extremely cost effective for patients at high risk of myocardial infarction or death. In such patients, the number needed to treat to save one life or prevent one acute myocardial infarction at 30 days may be as low as 30, or about £5000 per outcome.
Antithrombotic therapy in coronary angioplasty and stent placement procedures
Before procedure
Aspirin 80-325 mg once daily at least 2 hours before procedure. Ticlopidine 250 mg twice daily or clopidogrel 75 mg once daily started 24 hours before procedure if aspirin contraindicated
Glycoprotein IIb/IIIa receptor antagonists should be considered in high risk patients with acute coronary syndromes
During and after procedure
Heparin* bolus to achieve activated clotting time (ACT) ∼300 seconds. Give 70-150 U/kg or 7000 U for women and 8000 U for men. If ACT not achieved give extra bolus of 2500-5000 U. Reduce heparin bolus to achieve ACT ∼200 seconds if glycoprotein IIb/IIIa receptor agonist is to be used
In high risk patients, abciximab as bolus and infusion should be given at least 10 minutes before angioplasty and stent placement and continued for 12 hours after procedure
After procedure
Start clopidogrel 300 mg orally, followed by 75 mg daily for 4 weeks
Remove femoral sheath as soon as ACT falls below 150-180 seconds
Heparin infusion is not routinely necessary after uncomplicated angioplasty
Heparin infusion after a procedure is indicated if
Femoral sheath to be retained—Heparin infusion 1000-1200 U/hour until 4 hours before sheath is to be removed. Check ACT and remove sheath when ACT <150 seconds
Patients at high risk for in stent thrombosis
Patients with other indications for anticoagulation, such as atrial fibrillation or mechanical heart valves
*Details given for unfractionated heparin, but low molecular weight heparin can be used as an alternative in percutaneous coronary interventions
Anticoagulant treatment
Most patients with acute coronary syndromes undergoing angioplasty would have been pretreated with heparin. Several small studies have shown that patients with unstable angina who receive heparin before intervention have a higher rate of success and lower postprocedure reocclusion rates.
Increasing numbers of patients with unstable angina are now being treated with low molecular weight heparin. However, such drugs tend to have a longer half life than unfractionated heparin and their effects are not completely reversed by protamine sulphate if necessary. Low molecular weight heparins can be safely substituted for unfractionated heparin as a procedural anticoagulant during percutaneous coronary intervention.
During percutaneous coronary interventions, heparin should be given to avoid postprocedure complications. The dose of unfractionated heparin given should be sufficient to increase the activated clotting time (ACT) to 250-300 seconds as measured with the HemoTec device (or 300-350 seconds with the Hemochron device). Unfractionated heparin dose may need to be adjusted for weight or sex. If glycoprotein IIb/IIIa receptor agonists are being used, then unfractionated heparin boluses should be reduced to achieve a target ACT of about 200 seconds. Although the traditional means of assessing heparin anticoagulation has been with the APTT, the ACT is an assay of whole blood clotting time that can be performed rapidly at the bedside and catheterisation laboratory.
Routine use of unfractionated heparin (either as infusion or subcutaneously) after angioplasty is probably not indicated for uncomplicated procedures. Studies have shown excess bleeding complications with heparin treatment without a reduction in the number of cardiac ischaemic events. Patients who do not receive heparin treatment after coronary interventions can have their femoral sheaths removed earlier, resulting in shorter hospital stays, fewer bleeding complications, at the risk of a similar incidence of cardiac end points including reocclusion.
Further reading
The Task Force on the management of acute coronary syndromes of the European Society of Cardiology. Management of acute coronary syndromes in patients presenting without persistent ST segment elevation. Eur Heart J 2002;23:1809-40
Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST segment elevation myocardial infarction. J Am Coll Cardiol 2002;40:1366-74
Fox KA, Poole-Wilson PA, Henderson RA, Clayton TC, Chamberlin DA, Shaw TR, et al for the Randomized Intervention Trial of Unstable Angina (RITA) Investigators. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: the British Heart Foundation RITA3 randomised trial. Lancet 2002;360:743-51
Leon MB, Baim DS, Popma JJ, Gordon PC, Cutlip DE, Ho KK, et al for the Stent Anticoagulation Restenosis Study Investigators. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting. N Engl J Med 1998;339:1665-71
Roffi M, Moliterno DJ, Meier B, Powers ER, Grines CL, DiBattiste PM, et al. Impact of different platelet glycoprotein IIb/IIIa receptor inhibitors among diabetic patients undergoing percutaneous coronary intervention: do tirofiban and Reopro give similar efficacy outcomes trial (TARGET) 1 year follow up? Circulation 2002;105:2730-6
With the advent of glycoprotein IIb/IIIa receptor antagonists, heparin infusions postprocedure should not be necessary routinely. Femoral sheaths should be removed once the ACT has fallen to less than 150-180 seconds. Adjunctive treatment with low molecular weight heparin or unfractionated heparin may still be warranted after angioplasty and stent implantation in patients at high risk of in stent thrombosis.
Full anticoagulation with heparin followed by warfarin in patients undergoing angioplasty with stenting is no better at reducing the number of adverse effects than combination treatment with aspirin and ticlopidine, but at increased risk of bleeding with warfarin. Use of hirudin, the direct thrombin inhibitor, was associated with a reduction of early cardiac events and restenosis at 96 hours but was no different from the heparin treatment arm at seven months.
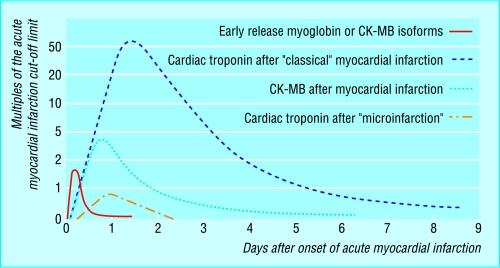
Figure.
Time course of different cardiac biochemical markers
Figure.
Death or myocardial infarction in patients with elevated troponin concentration or negative troponin result in contemporary trials. The FRISC-II trial also used low molecular weight heparin, and the bars for the TACTICS trial show the strategies used (I=invasive strategy, C=conservative strategy)
Figure.
European Society of Cardiology recommended strategy for acute coronary syndromes (CABG=coronary artery bypass graft, LMWH=low molecular weight heparin, PCI=percutaneous coronary intervention. *Omit clopidogrel if patient likely to go to CABG within 5 days)
Figure.
Meta-analysis of 10 randomised trials that compared thrombolytic treatment with primary angioplasty in acute myocardial infarction (MI=myocardial infarction, IC=intracranial)
Figure.
Cumulative incidence of primary end points (mortality, target lesion revascularisation or thrombosis, non-fatal myocardial infarction) in patients treated with aspirin alone (557 patients), aspirin and warfarin (550 patients), or aspirin and ticlopidine (546 patients) after coronary artery stenting
Figure.
PRISM-PLUS results showing cumulative incidence of death or myocardial infarction (PTCA=percutaneous transluminal coronary angioplasty, RR=relative risk)
Acknowledgments
The meta-analysis of trials comparing thrombolytic treatment with primary angioplasty is adapted from Weaver WD, et al, JAMA 1997;278:2093. The figure showing incidence of primary end point in patients treated with aspirin alone, aspirin and warfarin, or aspirin and ticlopidine after coronary artery stenting is adapted from Leon MB, et al, N Engl J Med 1998;339:1665-71. The figure showing the results from the PRISM-PLUS study is adapted from PRISM-PLUS Study Investigators. N Engl J Med 1998;338:1488-97. The figure showing the time course of cardiac biochemical markers is adapted from Wu AH, et al, Clin Chem 1999;45:1104-21. The figures of death or myocardial infarcton in patients with elevated troponins or negative troponin result, and the strategy for acute coronary syndromes are adapted from Bertrand ME, et al, Eur Heart J 2002;23:1809-40.
Footnotes
Derek L Connolly is a consultant cardiologist, from the department of cardiology and vascular medicine, Sandwell and West Birmingham Hospitals NHS Trust, Birmingham, Gregory Y H Lip is professor of cardiovascular medicine, and Bernard S P Chin is research fellow at the haemostasis thrombosis and vascular biology unit, university department of medicine, City Hospital, Birmingham.
The ABC of antithrombotic therapy is edited by Gregory Y H Lip and Andrew D Blann, senior lecturer in medicine, haemostasis thrombosis and vascular biology unit, university department of medicine, City Hospital, Birmingham. The series will be published as a book in spring 2003.