Perhaps surprisingly there are as yet no guidelines for managing acute renal colic in primary care. A group of Durham general practitioners and specialists endeavour to remedy the deficiency
Acute renal colic is a common, often recurrent condition with an annual incidence of 1-2 cases per 1000 and a lifetime risk of 10-20% for men and 3-5% for women.1–3 Patients usually present with acute pain and pose management challenges for the general practitioner, who may be uncertain whether immediate hospital admission is needed and, if not, how and when patients should be followed up.4 In many patients sent to hospital the pain remits on the way to hospital, or soon after admission, in response to the analgesia given by the general practitioner, making the admission perhaps unnecessary.5 The majority of those calling NHS Direct with acute renal colic are advised to contact their general practitioners “urgently”; a small number are referred to the accident and emergency services; and some are advised how to treat themselves.6
Summary points
There is uncertainty about the immediate management of patients presenting with acute renal colic in primary care, and whether this can be overcome by adopting a pre-established integrated pathway of care across the primary-secondary care interface
Intramuscular diclofenac 75 mg is recommended as first line of treatment when the diagnosis is clear and there are no signs of complications
If the severe pain does not remit within an hour the patient should be admitted to hospital
All patients, whether managed at home or in hospital, should be offered fast track urological investigation with follow up
Opaque radiography and ultrasound are being augmented by the use of spiral computed tomography in some centres in certain situations
Methods
We aimed to develop, by evidence based consensus, a management plan for patients with acute renal colic which would improve the accuracy of the diagnosis and facilitate follow up, while reducing pressure on hospital admissions. No guidelines have been published on the management of such patients in primary care by the key professionals—general practitioners, urologists, and radiologists.
Our research involved clinicians from all six primary care trusts in County Durham in north east England, in which a population of 300 000 is served by 215 general practitioners. The local hospital has three urologists and a radiologist specialising in urology. Firstly, we systematically reviewed the literature (see bmj.com), grading evidence according to the Scottish Intercollegiate Guidelines Network (box B1).7 All data discovered were in the lower categories, 3 and 4, apart from papers on the use of specific analgesics and imaging during acute colic, and we found no guidelines covering the interface between primary and secondary care.
Box 1.
Scottish Intercollegiate Guidelines Network grading system
Secondly, four focus groups of 33 general practitioners provided information and views on the management of patients in primary care; standard procedures for recording, transcribing, and analysis were used, together with respondent validation.8,9 The findings reflected general practitioners' uncertainties about the best analgesics, whether or not to admit the patient immediately, and anxieties about revisiting. Some general practitioners routinely admitted all patients with acute renal colic because they felt that this expedited further management, particularly imaging.
Thirdly, we interviewed local specialists: the urologist voiced frustration about “frequent and often unnecessary admissions of otherwise healthy patients, many of whom were pain free when they arrived or shortly after admission” and the radiologist was concerned about “ad hoc and poorly justified” radiology requests, usually some time after the acute episode, with resulting poor yield.
Finally, a multidisciplinary guideline group of 11 clinicians drew up a draft management plan for consideration. This consensus group comprised two urologists, two radiologists, clinical governance representatives from five primary care groups, the clinical head of the health authority primary care support unit, and the moderator (PJW).10 The discussion focused on a draft management plan that incorporated a fast track investigation pathway. The proceedings were taped, the tapes were transcribed, and outcomes were graded according to criteria for guidelines.7 The analysis followed standard guidelines, and respondent validation was obtained by circulating the results to the participating group members and inviting their responses.8–10
Results
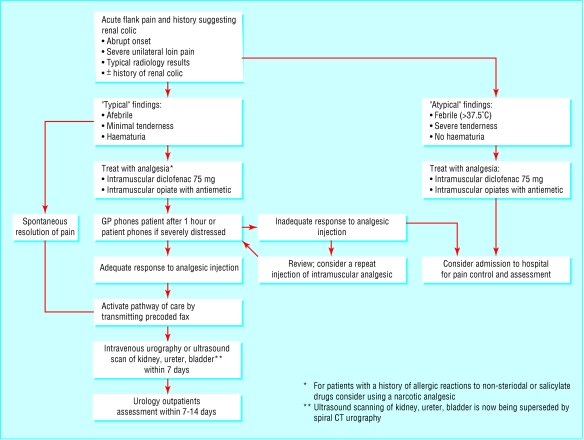
The table summarises the findings of the consensus group and the figure shows the management pathway that the group formulated.
Dealing with medical emergencies presenting in primary care
Consensus: patients with acute symptoms should receive a medical assessment within 30 minutes; recommendation grade D; level of evidence 3 or 4.
The consensus group debated priority to be given to patients with acute renal colic, especially in the presence of competing demands for attention from others with acute problems. If the patient could not be seen within 30 minutes the consensus was that paramedical services should be sent to give appropriate analgesia and take the patient to a local accident and emergency department.
The group also considered the current outcomes of NHS Direct's nurse led triage for renal colic: 80% of callers are instructed to contact a general practitioner immediately; 10% are directed to the local accident and emergency department; and the 10% with a history of renal colic are advised to treat themselves and to contact their doctor within 24 hours. Nurse triage has been confirmed as safe and effective, and callers obtain advice more quickly than by direct contact with a general practitioner.11
Assessment
Consensus: the diagnosis is centred on the history of an abrupt onset of severe unilateral flank pain radiating into the groin or genitals12; recommendation grade C; level of evidence 3 or 4.
The group considered using a visual analogue scale to assess the severity of pain, but the overwhelming view was that the general practitioners would judge severity themselves. Other potentially dangerous diagnoses needing immediate admission to hospital need to be considered, particularly a leaking abdominal aortic aneurysm, especially in patients aged over 60 years, or rupture of an ectopic pregnancy.13
Urinalysis: to test or not to test?
Consensus: haematuria supports the diagnosis; recommendation grade C; level of evidence 2++.
The need for urinalysis was debated. Over 80% of patients with acute renal colic test positive for haematuria.14 Ideally, if practicable, the urine should be tested and alternative diagnoses considered in those in whom the test is negative.12 However, not all patients can void a specimen, and menstruation can be a confounding factor.
Examination of the patient
Consensus: an optimal assessment must include examination of the abdomen, to establish the site of maximal tenderness and to exclude signs of other conditions such as peritonitis, and consideration of the vital signs, to exclude shock and systemic infection12; recommendation grade C or D; level of evidence 2–.
Patients with shock or fever must be admitted to hospital immediately.4
Treatment
Consensus: after assessment, analgesia should be given quickly to provide pain relief within half an hour; recommendation grade A; level of evidence 1–.
Complete or acceptable pain control should be maintained for six hours or longer. The best route for administration of an analgesic is by intramuscular injection; oral and rectal administration are considered unreliable,15 and the intravenous route impractical in the patient's home. An injectable non-steroidal analgesic, preferably diclofenac 75 mg, is recommended.16,17 Where a non-steroidal analgesic is definitely contraindicated an opiate combined with an antiemetic, such as morphine sulphate and cyclizine, should be given.18
Admission to hospital
Consensus: patients failing to respond to analgesia within one hour should immediately be admitted to hospital; recommendation grade D; level of evidence 4.
The effect of analgesia can normally be checked by telephone; this does not require a second visit. If pain has not been alleviated within 60 minutes, admission to hospital should be arranged by telephone. Abrupt recurrence of severe pain also warrants immediate admission, again arranged by telephone. Some participants said that patients who have a good initial response but develop pain again deserve special consideration and they favoured issuing the patient a limited quantity of oral or rectal analgesics,18 but there were reservations about this because of the possibility of drug misuse.
All patients managed at home should drink a lot of fluids and, if possible, void urine into a container or through a tea strainer or gauze to catch any identifiable calculus, as this will help in the diagnosis.4,19
Follow up
Consensus: the general practitioner should follow the assessment visit with a telephone call one hour after initial assessment and administration of analgesia; recommendation grade D; level of evidence 4.
The patient should be instructed to contact the doctor if the pain worsens or if unexpected or more distressing symptoms develop. Investigations to determine the following points are an important component of the follow up of all patients whose symptoms resolve19:
Was a calculus identified? If so what was its size and location?
If a calculus is still present, is intervention likely to be needed?
If no calculus is present should alternative diagnoses be considered?
Is the patient at risk of developing further episodes?
Acute renal colic: management at home or in hospital?
Criteria for management at home
Pain from new or recurrent renal colic subsiding either spontaneously or after administration of analgesia
Adequate social support
Contact by telephone possible
Willingness to stay at home
Ideally age under 60, which reduces risk of leaking abdominal aortic aneurysm
Criteria for admission to hospital
Persistent pain unrelieved by analgesia
Women of reproductive age and history of delayed menstruation (risk of ectopic pregnancy)
Symptoms of systemic illness, infection, or anuria
Patient's preference for admission
Contact by telephone not possible
No reliable social support
Documented history of only one functioning kidney
Pregnancy or age over 60
A primary-secondary care management pathway
Consensus: a conjoint management pathway between primary and secondary care, using a multidisciplinary approach, would facilitate management of patients; recommendation grade D; level of evidence 4.
Patients fulfilling the criteria for home management should be offered fast track investigation initiated by the hospital on receipt of a faxed template completed by the general practitioner. The radiologists agreed that to facilitate earlier, more accurate diagnosis the majority should receive an appointment for radiology within seven days of the onset of symptoms. All the specialists agreed that an urgent appointment at urology outpatients should be arranged within a week if renal imaging showed a problem requiring intervention. General practitioners should receive copies of renal imaging reports before the urology appointment.
Workload implications
There was uncertainty as to whether introducing the pathway would result in more patients being referred for radiology and whether this might prove unmanageable. However, this might be counterbalanced by a reduction in admissions and thus inpatients competing for the same investigations. There was agreement that a pilot study would be necessary to evaluate the safety and efficacy of a fast track pathway.
Discussion
This study highlights a situation where prompt and effective action is needed but reliable evidence as to what is best is scanty. This is typical of many conditions where hospital practice is extrapolated to primary care. Defining good clinical practice across the primary-secondary interface lent itself to a consensus based approach. This project aimed to integrate primary and secondary care aspects of management of acute renal colic.
Patients with acute renal colic usually present in primary care and they are often admitted to hospital even as their symptoms are subsiding. One reason why general practitioners admit these patients is their expectation that they will have to revisit if the symptoms do not settle.
This study established a management pathway based on emergency intervention by the general practitioner but with a mechanism for hospital admission without a revisit if the patient did not settle. Radiologists and urologists were involved to enable an earlier and more accurate evaluation and to direct subsequent management.19 Within the current NHS ethic of integrated care this combined approach represents an advance.
We used accepted principles of guideline development, starting with a literature review. The subsequent interviews and meetings followed accepted methods of qualitative research, and we believe the results to be an accurate reflection of the participants' views. The management pathway represented a synthesis of evidence by professional consensus.10
A weakness of this study is that it was set within one locality. However, we believe that the results are transferable, as the clinical and management factors are unlikely to vary much. We accept that other clinicians might have different views; inviting participants from outside the locality might have enriched the process but it also might have negatively influenced ownership of the local template we were aiming to develop.
The process described in this paper involves a relatively minor alteration to routine care but has the potential for reducing the workload in primary care and the number of admissions to hospital, while increasing diagnostic accuracy by providing for earlier imaging. Research has indicated that if properly developed, communicated, and implemented, guidelines can improve patient care,20 but doctors differ in their willingness to accept new management patterns. To facilitate change, general practitioners require sufficient knowledge, skills, and motivation to adapt to the proposed changes. Interventions that induce change must focus on the removal of existing barriers, while supporting the change process by education and consolidation of the new practice.21
A protocol for acute renal colic led from primary care is timely, and this one is attractive because it does not demand a major change in clinical practice. It is well defined, pragmatic, with guidance supporting decisions and actions in each clinical setting.22 Because research evidence for the management of such medical emergencies in primary care is scarce, there is a need for such initiatives to be evaluated.23 A protocol derived from this research is currently being evaluated in a randomised controlled trial.
Supplementary Material
Table.
Summary of the consensus group's findings
| Aspect of care
|
Consensus reached
|
Consensus recommendation
|
Level of evidence
|
Grade of recommendation
|
|---|---|---|---|---|
| Timing of assessment | Yes | Patients with acute symptoms should receive a medical assessment within 30 minutes | 3/4 | D |
| Establishing a diagnosis | Yes | Diagnosis is centred on abrupt onset of severe unilateral flank pain radiating into the groin or genitals | 3/4 | D |
| Atypical cases | Yes | Over 60 years of age: consider a leaking abdominal aortic aneurysm; women with delayed menses: consider ectopic pregnancy | 2++ | B |
| Assessment of pain | No | Use of visual analogue scale considered helpful, but view among general practitioners was that they would prefer to judge severity themselves | 4 | D |
| Urinalysis for blood on site | No | General agreement that haematuria supports the diagnosis, but urinalysis considered impractical by those preferring to rely on clinical judgment, and often patients are unable to void on demand | 2++ | C |
| Examination | Yes | Assessment must include examination of abdomen and exclude signs consistent with other conditions (for example, peritonitis). Assessment of vital signs (pulse, blood pressure, and temperature) to exclude signs of shock and systemic infection | 2− | C/D |
| Treatment | Yes | After assessment, analgesia should be given to provide rapid pain relief (within half an hour). Consensus favoured giving diclofenac given by intramuscular injection | 1− | A |
| Failure of analgesia | Yes | Failure of analgesia after 1 hour: immediately admit patient to hospital (by phone) without further consultation | 4 | D |
| Recurrent pain | No | Some general practitioners in favour of issuing limited supplies of oral or rectal analgesia with instruction for self administration | 4 | D |
| Follow up | Yes | General practitioner to initiate follow up by phone 1 hour after initial assessment | 4 | D |
| Investigation | Yes | Investigate all patients with suspected acute renal colic to identify the calculus and determine management | 4 | D |
| Advice to patient | Yes | Maintain higher fluid intake and attempt to sieve urine | 4 | D |
| Written information | Yes | Issuing written information by general practitioners for patients considered impractical in the acute setting | 4 | D |
| Fast track investigation | Yes | All in favour of fast track general practitioner access for renal imaging within 7 days of onset and urology outpatients within 14 days of onset (if a calculus is identified), plus immediately sending results to general practitioner | 4 | D |
| Workload | No | Some participants anticipated an increase in workload for radiologists and general practitioners | ||
| Pilot study | Yes | All in favour of a pilot or feasibility study to evaluate fast track path of care for patients with suspected acute renal colic | ||
| Hospital admissions | Yes | Anticipated reduction in number of urgent hospital admissions for suspected acute renal colic resulting from fast track path for renal imaging combined with urology review |
Figure.
Pathway for management of acute renal colic
Acknowledgments
We thank the general practitioners and consultants who participated in the study, and Debbie King for transcribing the tapes. PW is grateful to his general practice partners for allowing him the time to conduct the research.
Footnotes
Funding: A research training fellowship was awarded to PW from the Northern and Yorkshire Regional Health Authority.
Competing interests: APSH has received funding from Novartis in relation to research on another topic. PW received a £200 donation from Novartis to assist in a related follow up study for acute renal colic.
Additional references appear on bmj.com
References
- 1.Scott R. Prevalence of calcified upper urinary tract stone disease in a random population survey. Br J Urol. 1987;59:111–117. doi: 10.1111/j.1464-410x.1987.tb04799.x. [DOI] [PubMed] [Google Scholar]
- 2.Scott R. Epidemiology of stone disease. Br J Urol. 1985;57:491–497. doi: 10.1111/j.1464-410x.1985.tb05853.x. [DOI] [PubMed] [Google Scholar]
- 3.Ahlstrand C, Tiselius H. Renal stone disease in a Swedish district during one year. Scand J Nephrol. 1981;15:143–146. doi: 10.3109/00365598109179591. [DOI] [PubMed] [Google Scholar]
- 4.Dawson C, Whitfield H. Urological emergencies in general practice. BMJ. 1996;312:838–840. doi: 10.1136/bmj.312.7034.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menon M, Parulkar BG, Drach GW. Urinary lithiasis: aetiology, diagnosis and medical management. In: Walsh PC, Retik AB, Stamey TA, Vaughan ED, editors. Campbells urology. 7th ed. Philadelphia: Saunders; 1998. pp. 2661–2733. [Google Scholar]
- 6.Morris SB, Hampson SJ, Gordon EM, Shearer RJ, Woodhouse CRJ. Should all patients with ureteric colic be admitted? Ann R Coll Surg Engl. 1995;77:450–452. [PMC free article] [PubMed] [Google Scholar]
- 7.Banks I. NHS Direct healthcare guide. London: NHS Direct; 2000. [Google Scholar]
- 8.Scottish Intercollegiate Guidelines Network. Edinburgh: SIGN; 2002. SIGN 50: a guideline developers' handbook.www.sign.ac.uk/guidelines/fulltext/50/section5.html . (Section 5: systematic literature review.) www.sign.ac.uk/guidelines/fulltext/50/section5.html (accessed 29 Oct 2002). (accessed 29 Oct 2002). [Google Scholar]
- 9.Carter Y, Thomas C. Research methods in primary care. Oxford: Radcliffe Medical Press; 1997. [Google Scholar]
- 10.Coffey A, Atkinson P. Making sense of qualitative data. Complementary research strategies. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- 11.Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J, et al. Consensus development methods and their use in clinical guideline development. Health Technol Asses. 1998;2:1–88. [PubMed] [Google Scholar]
- 12.Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbulll J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. BMJ. 1998;317:1054–1059. doi: 10.1136/bmj.317.7165.1054. . Eskelinen M. Usefulness of history-taking, physical examination and diagnostic scoring in acute renal colic. Eur Urol 1998;34:467-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acheson A G. Prospective study on factors delaying surgery in ruptured abdominal aortic aneurysms. J R Coll Surg Edin. 1998;43:182–184. [PubMed] [Google Scholar]
- 14.Press SM. Incidence of negative haematuria in a patient with acute urinary lithiasis presenting to the emergency room with flank pain. Urology. 1995;45:753–757. doi: 10.1016/S0090-4295(99)80078-8. [DOI] [PubMed] [Google Scholar]
- 15.Thompson J F, Pike JM, Chumas PD, Rundle JS. Rectal diclofenac compared with pethidine injection in acute renal colic. BMJ. 1989;299:1140–1141. doi: 10.1136/bmj.299.6708.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Labrecque M, Dostaler LP, Rousselle R, Nguyen T, Poirier S. Efficacy of nonsteroidal anti-inflamatory drugs in the treatment of acute renal colic. Arch Intern Med. 1994;154:1381–1387. [PubMed] [Google Scholar]
- 17.Tramer MR, Williams JE, Carroll D, Wiffen PJ, Moore RA, McQuay HJ. Comparing analgesic efficacy of non-steroidal anti-inflamatory drugs given by different routes in acute and chronic pain: a qualitative systematic review. Acta Anaesthiol Scand. 1998;42:71–79. doi: 10.1111/j.1399-6576.1998.tb05083.x. [DOI] [PubMed] [Google Scholar]
- 18.Hetherington JW. Diclofenac sodium versus pethidine in acute renal colic. BMJ. 1986;292:237–238. doi: 10.1136/bmj.292.6515.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997;158:1915–1921. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 20.Eccles M. North of England evidence based guidelines development project: methods of guideline development. BMJ. 1996;312:760–761. doi: 10.1136/bmj.312.7033.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grol R. Attributes of clinical guidelines that influence use of guidelines in general practice. BMJ. 1998;317:858–861. doi: 10.1136/bmj.317.7162.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grol R. Implementing guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48:991–997. [PMC free article] [PubMed] [Google Scholar]
- 23.Mant D. R&D in primary care—an NHS priority. Br J Gen Pract. 1998;48:871. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.