Abstract
BACKGROUND
Dynesys dynamic stabilization (DDS) is an alternative to surgical fusion for the operative management of degenerative lumbar spondylosis. Compared to rigid instrumentation and fusion, DDS is purported to preserve a higher degree of spinal range of motion and reduce the risk of developing adjacent segment disease (ASD).
OBSERVATIONS
A 60-year-old female presented with severe back pain and bilateral leg pain, which had progressed over the prior 4 years. Nine years earlier, she had undergone DDS system implantation at L5–S1 for lumbar stenosis and spondylosis. Repeat imaging revealed an unintended fusion at the index level (L5–S1) and ASD causing severe lateral recess stenosis at L4–5. She underwent DDS system removal, decompression at L4–5, and extension of the fusion to L4.
LESSONS
Although DDS has been marketed as a motion-preserving system that avoids fusion and reduces the risk of ASD, unintended index-level fusion and ASD can still occur after DDS system surgery. These potential complications should be assessed when determining the optimal primary surgical treatment for patients with lumbar degenerative disc disease.
Keywords: adjacent segment disease, dynamic stabilization, intervertebral disc degeneration, spinal fusion
ABBREVIATIONS: ASD = adjacent segment disease, CT = computed tomography, DDS = Dynesys dynamic stabilization, MRI = magnetic resonance imaging
Lumbar fusion surgery remains the gold-standard treatment for severe degenerative spine disease requiring operative management. While fusion surgery has been demonstrated to improve back pain and overall quality of life for select patient populations, it does lead to a reduced range of motion across the fused lumbar segment.1–3 Additionally, the fused segment can exert increased mechanical stress on adjacent levels and lead to earlier degeneration, a condition known as “adjacent segment disease” (ASD). Symptomatic ASD is reported to develop in 5%–18.2% of patients following lumbar fusion surgery.4 Additionally, rates of reoperation for the treatment of ASD have been reported to be 7.7% at 2 years5 and 16.5%–20% at 5 years.6, 7 ASD requiring reoperation has also been reported to occur in approximately 10% of patients who have undergone laminectomy alone.8 Thus, not all adjacent level disease is attributable to prior fusion. ASD can develop as part of the natural history of spondylosis even in the absence of any surgical intervention.9
The Dynesys dynamic stabilization (DDS) system was introduced in 1994 as a surgical alternative to rigid fixation and fusion.10 Its purported benefits include preserving a higher degree of mobility and reducing the risk of ASD while providing comparable symptomatic relief.11–15 A number of small clinical investigations comparing short- and long-term outcomes have reported lower rates of ASD after DDS system implantation.16–18 However, one study found that ASD still developed in approximately 29% of cases and can result in fusion at the adjacent level.19 Additionally, rates of unintended facet joint fusion after DDS system surgery have been reported to be as high as 52.1%.20 Evidently, although DDS has been marketed as a procedure that avoids fusion and prevents ASD, half of these patients ultimately demonstrated unintended fusion. We report the case of a patient who presented with both ASD and index-level fusion after DDS system implantation.
Illustrative Case
A 60-year-old female presented with increasingly severe lower-back and bilateral leg pain. Nine years prior to this encounter, she had undergone DDS system implantation at the L5–S1 level for the treatment of spondylolisthesis and underlying stenosis at an outside institution. Approximately 4 years after the procedure, she experienced lower-back pain, which increased in severity over time despite conservative management, including physical therapy and epidural steroid injections.
Lumbar computed tomography (CT) demonstrated fusion across the L5–S1 segment, the level at which the DDS system had been implanted (Fig. 1). Lumbar magnetic resonance imaging (MRI) showed adjacent level disease at L4–5 with severe central stenosis, foraminal stenosis, and facet arthropathy and grade I anterolisthesis of the L4 vertebra on L5 (Fig. 2).
FIG. 1.
CT scans demonstrating a solid fusion at the L5–S1 level 9 years after index-level DDS system surgery. A: Right parasagittal image. B: Left parasagittal image. C: Axial cut of the L5–S1 facet joints.
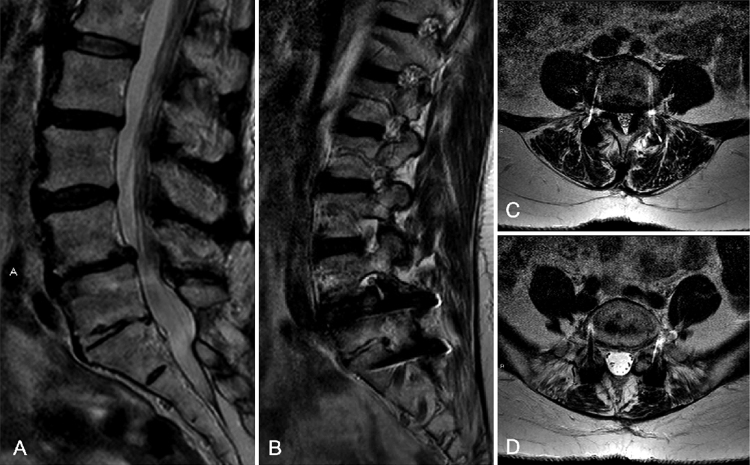
FIG. 2.
Lumbar MRI showing the L4–5 adjacent segment 9 years after index-level DDS system surgery at L5–S1. A: Sagittal T2-weighted image. B: Parasagittal T2-weighted image. C: Axial T2 cut at the L4–5 level showing ligamentous hypertrophy and severe lateral recess stenosis. D: Axial T2 cut at the L5–S1 level.
The patient underwent removal of the DDS system, decompression, and stabilization at L4–5.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
The motion-preserving lumbar DDS system is marketed as an alternative to fusion, with the ability to maintain motion and reduce the risk of ASD. Despite these claims, our patient developed concomitant index-level fusion where the DDS system had been implanted, as well as ASD above it, requiring revision surgery. Previous studies have reported that ASD and unintended fusion can develop after DDS system implantation, but there has been limited investigation into how these complications can co-occur.19–22 Importantly, our patient did not have prior ASD, which has been shown to increase the risk of progressive ASD after DDS system implantation.19 Therefore, our illustrative case reveals that ASD and unintended fusion can co-occur in patients without prior ASD.
Lessons
Treating degenerative spine disease with the motion-preserving DDS system does not necessarily prevent index-level fusion, nor does it prevent ASD.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Ran, Azad, Bydon. Acquisition of data: Ran, Azad. Analysis and interpretation of data: Ran, Bydon. Drafting the article: Ran, Azad, Bernhardt. Critically revising the article: all authors. Reviewed submitted version of manuscript: Ran, Azad, Pahwa, Bernhardt. Approved the final version of the manuscript on behalf of all authors: Ran. Administrative/technical/material support: Bernhardt. Study supervision: Azad.
Correspondence
Kathleen R. Ran: Johns Hopkins University School of Medicine, Baltimore, MD. kran2@jh.edu.
References
- 1.Evaniew N, Swamy G, Jacobs WB, et al. Lumbar fusion surgery for patients with back pain and degenerative disc disease: an observational study from the Canadian spine outcomes and research network. Glob Spine J. 2022;12(8):1676-1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fritzell P, Hagg O, Wessberg P, Nordwall A, Swedish Lumbar Spine Study Group. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976). 2001;26(23):2521-2534. [DOI] [PubMed] [Google Scholar]
- 3.Ghogawala Z, Resnick DK, Glassman SD, Dziura J, Shaffrey CI, Mummaneni PV. Randomized controlled trials for degenerative lumbar spondylolisthesis: which patients benefit from lumbar fusion? J Neurosurg Spine. 2017;26(2):260-266. [DOI] [PubMed] [Google Scholar]
- 4.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila PA 1976). 2004;29(17):1938-1944. [DOI] [PubMed] [Google Scholar]
- 5.Aiki H, Ohwada O, Kobayashi H, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 2005;10(5):490-495. [DOI] [PubMed] [Google Scholar]
- 6.Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004;86(7):1497-1503. [DOI] [PubMed] [Google Scholar]
- 7.Lee CS, Hwang CJ, Lee SW, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009;18(11):1637-1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bydon M, Macki M, De la Garza-Ramos R, et al. Incidence of adjacent segment disease requiring reoperation after lumbar laminectomy without fusion: a study of 398 patients. Neurosurgery. 2016;78(2):192-199. [DOI] [PubMed] [Google Scholar]
- 9.Song KJ, Choi BW, Jeon TS, Lee KB, Chang H. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. Eur Spine J. 2011;20(11):1940-1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11(suppl 2):S170-S178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akyoldas G, Cevik OM, Suzer T, Sasani M, Oktenoglu T, Ozer AF. Dynamic stabilization of the lumbar spine using the Dynesys® system. Turk Neurosurg. 2020;30(2):190-193. [DOI] [PubMed] [Google Scholar]
- 12.Zhang C, Wang L, Hou T, et al. The influence of L4–S1 Dynesys® dynamic stabilization versus fusion on lumbar motion and its relationship with lumbar degeneration: a retrospective study. J Orthop Surg Res. 2017;12(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu SW, Yang SC, Ma CH, Wu CH, Yen CY, Tu YK. Comparison of Dynesys posterior stabilization and posterior lumbar interbody fusion for spinal stenosis L4L5. Acta Orthop Belg. 2012;78(2):230-239. [PubMed] [Google Scholar]
- 14.Wu H, Pang Q, Jiang G. Medium-term effects of Dynesys dynamic stabilization versus posterior lumbar interbody fusion for treatment of multisegmental lumbar degenerative disease. J Int Med Res. 2017;45(5):1562-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005;30(3):324-331. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Shan JL, Liu XM, Li F, Guan K, Sun TS. Comparison of the Dynesys dynamic stabilization system and posterior lumbar interbody fusion for lumbar degenerative disease. PLOS ONE. 2016;11(1):e0148071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu A, Sun C, Liang Y, Wang H, Li X, Dong J. Multi-segmental lumbar spinal stenosis treated with Dynesys stabilization versus lumbar fusion in elderly patients: a retrospective study with a minimum of 5 years’ follow-up. Arch Orthop Trauma Surg. 2019;139(10):1361-1368. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Zhang ZC, Li F, et al. Long-term outcome of Dynesys dynamic stabilization for lumbar spinal stenosis. Chin Med J (Engl). 2018;131(21):2537-2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.St-Pierre GH, Jack A, Siddiqui MM, Henderson RL, Nataraj A. Nonfusion does not prevent adjacent segment disease: Dynesys long-term outcomes with minimum five-year follow-up. Spine. 2016;41(3):265-273. [DOI] [PubMed] [Google Scholar]
- 20.Fay LY, Huang WC, Chang CC, et al. Unintended facet fusions after Dynesys dynamic stabilization in patients with spondylolisthesis. J Neurosurg Spine. 2018;30(3):353-361. [DOI] [PubMed] [Google Scholar]
- 21.Fay LY, Chang PY, Wu JC, et al. Dynesys dynamic stabilization-related facet arthrodesis. Neurosurg Focus. 2016;40(1):E4. [DOI] [PubMed] [Google Scholar]
- 22.Pham MH, Mehta VA, Patel NN, et al. Complications associated with the Dynesys dynamic stabilization system: a comprehensive review of the literature. Neurosurg Focus. 2016;40(1):E2. [DOI] [PubMed] [Google Scholar]