In extolling the benefits of potassium an editorial in the BMJ recently advocated that people should increase their intake of potassium.1 Its benefits include lowering blood pressure in both hypertensive and normotensive people. A high potassium intake reduces the risk of stroke, and in rats it prevents renal vascular, glomerular, and tubular damage. Increasing potassium concentrations also reduces the risk of ventricular arrhythmias in patients with heart disease, heart failure, and left ventricular hypertrophy.1 Using a salt substitute that contains potassium combines the advantages of reducing sodium intake and increasing potassium intake.
However, in the high risk population that may benefit most from an increased consumption of potassium, several medical conditions predispose to the development of hyperkalaemia through impairing renal excretion of potassium. These conditions include renal failure, diabetes mellitus with hyporeninaemic hypoaldosteronism, and obstructive uropathy. The risk of hyperkalaemia is further increased by the frequent prescription in these patients of angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, and potassium sparing diuretics.2 Elderly patients with osteoarthritis may also use non-steroidal anti-inflammatory drugs, which also may contribute to increased plasma potassium values.2
Salt substitutes that contain potassium may cause hyperkalaemia with life threatening consequences in susceptible patients, as the following case report illustrates.
Case report
A 74 year old woman had developed end stage renal disease due to nephrolithiasis, hypertension, and renal vascular disease. She also had chronic obstructive pulmonary disease after 30 years of smoking. In November 2000 chronic intermittent haemodialysis was started three times weekly.
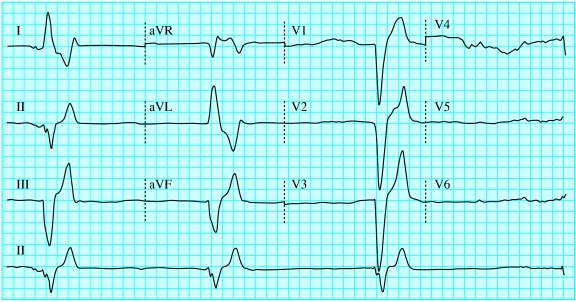
In March 2001 she was admitted urgently to our hospital on the day after dialysis because of malaise and abdominal pain. She had bradycardia (40 beats/min) in the ambulance, which responded to atropine infusion. On arrival in the emergency room an electrocardiogram showed bradycardia, absence of P waves, severely widened QRS complexes to 240 milliseconds, and tall peaked T waves (figure). She developed asystole, and cardiopulmonary resuscitation was performed for 20 minutes. Her serum potassium concentration was 9.2 mmol/l and she was given calcium levulinate 10 ml 10% twice, glucose 50% and insulin and sodium bicarbonate 8.4% 100 ml intravenously, and sodium polystyrene sulphonate 30 g orally. Her serum potassium concentration fell to 7.2 mmol/l and subsequently she underwent emergency haemodialysis. Her recovery was rapid and without sequelae. The cause of her unexpected life threatening hyperkalaemia was not established. The predialysis plasma potassium concentration in previous months had increased slowly from 4.1 to 6.4 mmol/l on the day before the incident. She was not taking angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, potassium sparing diuretics, or non-steroidal anti-inflammatory drugs. A dietician repeated the recommendation to reduce the potassium intake to 2400 mg/day.
In May 2001, the night before a scheduled dialysis treatment, she was again urgently transferred by ambulance to our hospital because of a paresis of her arms and legs. She developed asystole and was treated with cardiopulmonary resuscitation for several minutes. Hyperkalaemia was suspected and immediately treated with calcium levulinate, sodium bicarbonate, glucose-insulin, and salbutamol inhalation. Her serum potassium was later reported to be 9.7 mmol/l, and it declined to 7.9 mmol/l with the measures taken. She received emergency haemodialysis and again recovered without sequelae. She admitted to the consumption of some grapes, and the dietary advice was repeated. On further questioning it turned out she had used the salt substitute LoSalt, which contains at least two thirds potassium chloride and less than one third sodium chloride. She handed the LoSalt over and was advised strongly never to take a salt substitute again. Since then no further episodes of severe hyperkalaemia have occurred.
Comment
A patient on maintenance haemodialysis developed cardiopulmonary arrest due to severe hyperkalaemia on two occasions, probably because of her use of a potassium-containing salt substitute. Fortunately, she responded well to appropriate treatment.3
The beneficial effects of potassium and the harmful effects of sodium have recently received attention.1 Consumption of fruit and vegetables is the preferred source of potassium, but the use of a salt substitute also increases the intake of potassium at the same time as reducing the use of sodium. A similar case of cardiac arrest due to hyperkalaemia in a patient with mild renal insufficiency treated with nabumetone and also taking LoSalt has been reported previously.4 The label of LoSalt does state that it is not suitable for people who must follow a salt restricted diet.
Patients are often not aware that their medical condition may reduce potassium excretion or of the potassium content of the salt substitute they may use to reduce their sodium intake. Carers may not always know of a patient's use of a salt substitute. Our patient initially denied the use of LoSalt, and its use was established only after we questioned her family after the second episode. Because of the increasing prevalence of diabetes, renal failure, and the use of drugs that increase potassium concentration, the number of patients at risk of developing life threatening hyperkalaemia is likely to increase.
We recommend that patients with impaired renal potassium excretion due to renal disease, especially those taking angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, potassium sparing diuretics, or non-steroidal anti-inflammatory drugs, should be warned by their doctors and dieticians about the danger of hyperkalaemia. Prescribers of these drugs to such patients should inquire about their use of potassium-containing salt substitutes. The product information of salt substitutes containing potassium should also include clearer warnings.
Figure.
Electrocardiogram showing bradycardia, absence of P waves in leads II and V1, severely widened QRS complexes in all leads, and tall peaked T waves in the inferior and precordial leads, caused by severe hyperkalaemia
Salt substitutes may cause severe hyperkalaemia in patients with impaired renal potassium handling
Footnotes
Competing interests: None declared.
References
- 1.He FJ, MacGregor GA. Beneficial effects of potassium. BMJ. 2001;323:497–501. doi: 10.1136/bmj.323.7311.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perazella MA. Drug-induced hyperkalemia: old culprits and new offenders. Am J Med. 2000;109:307–314. doi: 10.1016/s0002-9343(00)00496-4. [DOI] [PubMed] [Google Scholar]
- 3.Rose BD. UpToDate Version 9.2. Wellesley, MA: Uptodate; 2001. Treatment of hyperkalemia.www.uptodate.com [Google Scholar]
- 4.Pal B, Hutchinson A, Bhattacharya A, Ralston A. Cardiac arrest due to severe hyperkalaemia in patient taking nabumetone and low salt diet. BMJ. 1995;311:1486–1487. doi: 10.1136/bmj.311.7018.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]