ABSTRACT
Common bile duct duplications represent exceptionally rare congenital anomalies of the biliary tract. In this case report we document an unusual variant of common bile duct duplication in a 79-year-old man who underwent a pancreaticoduodenectomy for ampullary cancer. The duplication consisted of two unseparated, completely-layered, common bile ducts which originated above the cystic duct junction and terminated prior to the point of insertion into the pancreas, where the two lumens converged into a single duct. Duplication of the bile duct is rare and often goes undetected. In the present case, the anomaly was found incidentally in a patient who had a pancreaticoduodenectomy for an ampullary carcinoma. However, duplication may be associated with choledocholithiasis, cholangitis, pancreatitis, and pancreaticobiliary malignancies and it is important to be aware of the condition.
Keywords: common bile duct, duplication, ampullary carcinoma, pancreaticoduodenectomy, computed tomography
INTRODUCTION
Duplication of the common bile duct is a rare anatomical variant of the biliary tree characterized by the presence of a septum within the common bile duct or in an accessory branch of the common bile duct [1]. The first documented case of duplication of the common bile duct dates back to the mid-16th century CE by the anatomist and physicist Vesalius [2]. The classification of duplicated common bile ducts was introduced in 1972 by Goor and Ebert [1] which was later modified by Choi et al. in 2007 [3] and includes five types of common bile duct duplication. This system was revised in 2022 by Sheng et al. [4] who included a subdivision of type I into a (partial) and b (complete septum within the bile duct lumen), along with minor additions to type V (Figure 1).
Fig. 1.
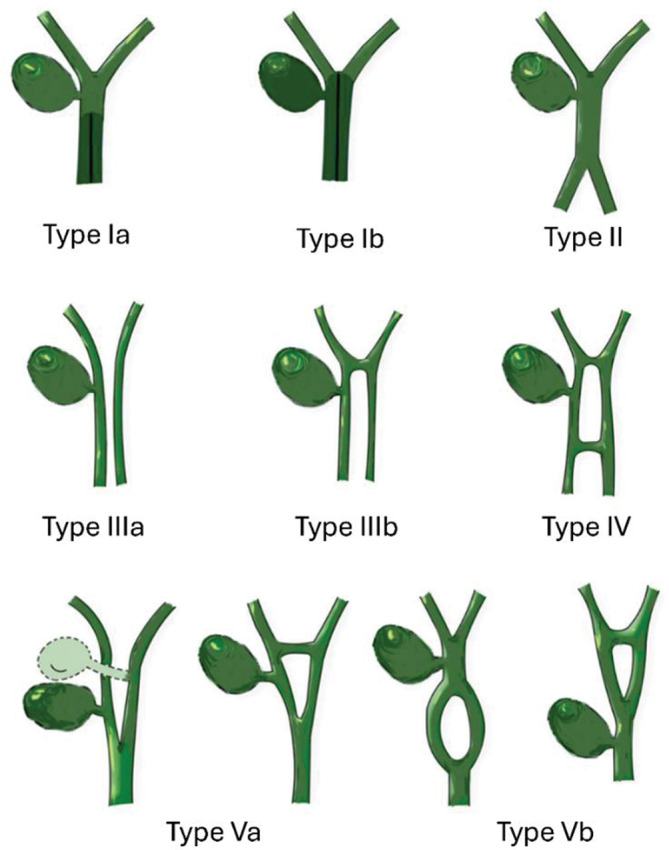
Classification of bile duct duplication as revised by Sheng et al. in 2022 [4]. Redrawn from Sheng et al. [4].
We report a variant of a type Ia common bile duct duplication, which was incidentally identified on pathological examination of a pancreaticoduodenectomy specimen for an ampullary cancer.
CASE HISTORY
A 79-year-old man with a history of systemic hypertension was referred to a tertiary center with a 2-week history of jaundice. He had pale stools and dark urine and had recently sought medical attention for vague upper abdominal pain. He experienced nausea which was worse on eating and had lost 4 kg in weight over the past month. The patient’s brother has previously been diagnosed to have pancreatic cancer. Physical examination demonstrated jaundice with scleral icterus. He was afebrile. Liver function tests demonstrated an obstructive pattern: Bilirubin 172 μmol/L (normal range 0-21 μmol/L), ALP 1747 U/L (normal range 40-150 U/L), ALT 341 U/L (normal range 0-50 U/L), AST 244 U/L (normal range 8-33 U/L.) Inflammatory markers were normal: WCC 9.28 × 109 cells/L (normal range 4-11 × 109 cells/L), CRP 6 mg/L (normal range 0-10 mg/L).
A portal venous contrast-enhanced CT abdomen demonstrated biliary and pancreatic duct dilatation extending down to the ampulla where there was abrupt tapering of the terminal common bile duct secondary to a small hyperattenuating periampullary lesion. The appearances were concerning for periampullary carcinoma. The peripancreatic vascular anatomy was normal and there was no evidence of distant metastasis. The patient underwent ERCP and biliary stent insertion with brushings confirming periampullary carcinoma.
Following multidisciplinary discussion, the patient underwent a pancreaticoduodenectomy. At the preoperative stage biliary duct duplication was not identified on CT or ERCP. The patient made a good recovery following the pancreaticoduodenectomy.
Pathological findings
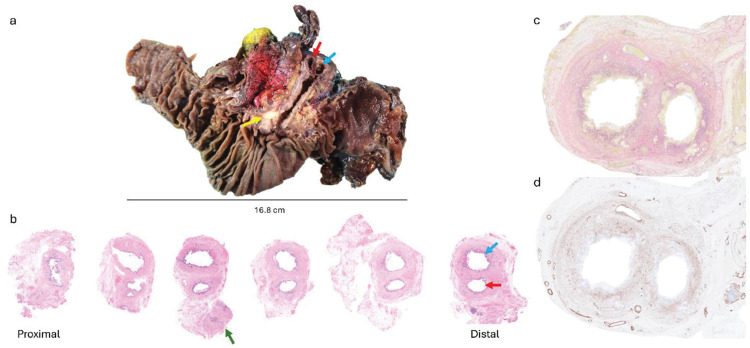
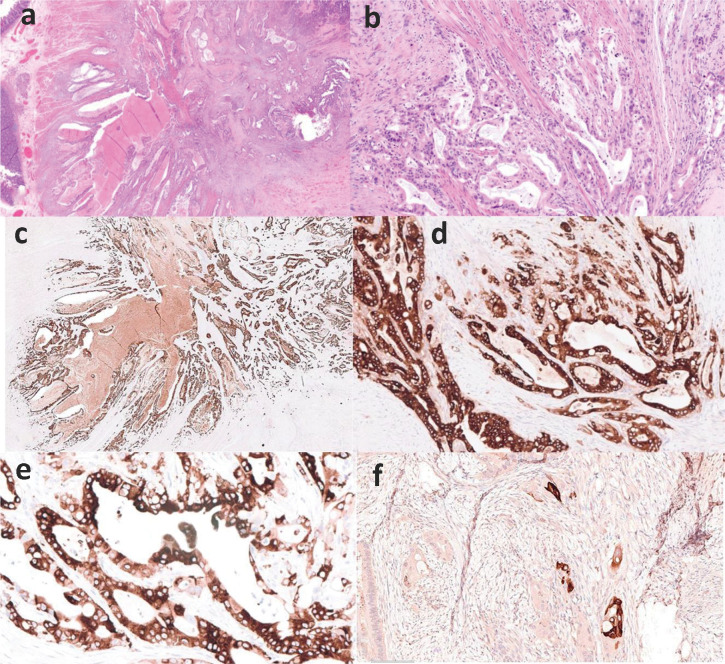
Macroscopic and histopathological analysis of the resected specimen demonstrated isolated duplication of the extrapancreatic common bile duct (Figure 2a and b). The bile duct was opened longitudinally from the ampulla to the distal part of the bile duct. Serial transverse sections were taken from the distal to the proximal aspect of the common bile duct duplication, and examined histologically. The duplication originated above the level of the cystic duct insertion into the right-sided duplicated bile duct, and terminated in the distal portion of the common bile duct prior to traversing through the pancreas. The intrapancreatic part of the duct had a single lumen. Ancillary studies demonstrated complete and continuous layering of each individual duct by smooth muscle (Figure 3). The ampullary tumor showed features of an ampullary adenocarcinoma, predominantly of the pancreaticobiliary type (Figure 3c and d). The tumor measured 30 mm in greatest diameter and showed local invasion (>0.5 cm) into the pancreas (pT3b). There were multiple foci of lymphovascular and perineural invasion, and a total of 6 sampled lymph nodes were involved by tumor (pN2). Moreover, the uncinate surgical margin was infiltrated by tumor cells (R1). The pancreatic tissue surrounding the tumor showed features of chronic pancreatitis. On immunohistochemistry, the malignant glands were positive for epithelial markers (CK7, epithelial membrane antigen, CA19.9) including epithelial mucin stains (MUC5AC and focal staining for MUC2). Occasional small foci of squamous differentiation were highlighted by CK5/6 (Figure 4).
Fig. 2.
(a) Macroscopic photograph of the pancreaticoduodenectomy specimen, demonstrates a duplicated common bile duct as indicated by the red (right duct) and blue (left duct) arrows. The yellow arrow points to the ampullary tumor. (b) Serial sections from the duplicated common bile duct. The green arrow highlights the cystic duct adjacent to the right-sided duplicated bile duct. The bile duct at the proximal resection margin was single (HE, x4). (c) Elastin van Gieson stain and (d) immunohistochemistry for smooth muscle actin showing complete layering by smooth muscle of each individual duct (x10).
Fig. 3.
Histology and immunohistochemistry of ampullary adenocarcinoma (a – HE, x14) and (b – HE, x20) with positive expression for CK7 (c – IHC, anti-CK7 mAb, x20), epithelial membrane antigen (d – IHC, anti-EMA mAb, x20) and MUC5AC (E – IHC, anti-MUC5AC, x400). There is focal squamous differentiation highlighted by CK5/6 (F – IHC, anti-CK5/6, x20).
Fig. 4.
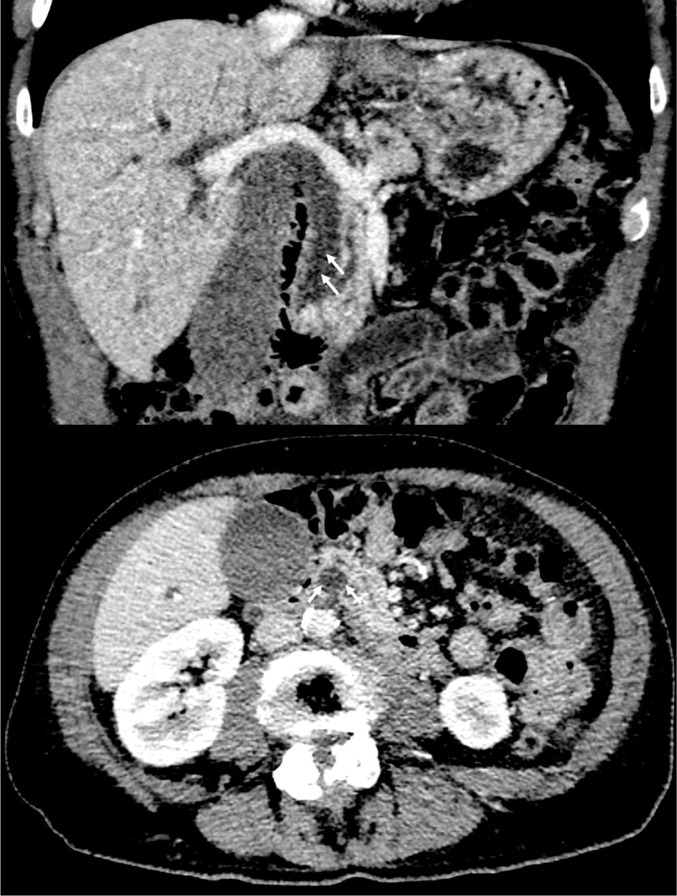
Contrast-enhanced CT abdomen – coronal reconstruction (top) and axial image (bottom). On narrowing the image window there is the impression of a thin dividing septum between two lumens of the extrapancreatic common bile duct (arrows).
Radiological findings revisited
The pathological findings prompted re-examination of the preoperative imaging. Upon narrowing the CT window level a subtle layered double lumen was appreciable in the extrapancreatic common bile duct on coronal and axial images (Figure 4). The rate of contrast opacification of the dual common bile duct lumens was uniform at ERCP meaning the duplication was not apparent in this modality even in retrospect.
DISCUSSION
Common bile duct duplication is rare developmental abnormality of the biliary system. This entity is common in fish, reptiles and birds but is very rare in the adult human biliary tree [5]. Curiously, duplicated bile ducts are considered a normal step in the earlier stages of human embryo development, but they eventually regress and form a single common bile duct [6]. The mechanism behind the persistence of this anomaly in adult humans is related to an early developmental disturbance resulting in persistence of an accessory extrahepatic duct [3]. In the medical literature, Type I common bile duct duplications are documented to represent a very low proportion of bile duct duplications in the Western (3.6%) and Japanese populations (6.8%) whilst they are more common in Chinese individuals (58.3%) [7-10]. Our case report shows a few similarities to this type of common bile duct duplication, including the recently described type Ia variant by Sheng et al. [4]. This reported variant is characterized by the presence of a complete septum in the bile duct lumen which is connected to the right and left hepatic ducts, and shows two distal openings into the duodenum. Our case, however, did not show a relationship with the hepatic ducts and demonstrated a lower origin, above the insertion of the cystic duct. Although there is a similar pattern of cystic duct drainage into the right-sided duplicated common bile duct as described in type Ib, in our case, the septum was incomplete (as in type Ia) with the two lumens merging together to form a single lumen in the intrapancreatic portion of the common bile duct. Furthermore, our case was associated with the finding of ampullary malignancy, which has not been previously documented in type I CBD duplications [8]. Therefore, the hypothesis of continuous reflux of bile and pancreatic secretions suggested in cancers associated with the other types (II-V) of common bile duct duplications may play a role in tumor development associated with type I variants as well. It is also possible that this anatomical variant described in our case allows for a more turbulent bile flow which eventually interferes with the pancreatic juice leading to chronic and persistent stimulation of the distal biliary tract.
Radiologically, the duplication would have been best demonstrated by MRCP but this was not performed for our patient. Type Ia and Ib duplications of the CBD are especially challenging to detect on CT as the layered lumens are more difficult to distinguish than the discrete lumens seen in the other subtypes of duct duplication. Previously reported cases of duplicated CBD have demonstrated that the other more discrete subtypes of duct duplication can be readily identified on CT, MRCP and ERCP [3,5,11-13].
CONCLUSION
In conclusion, duplication of the bile duct is rare and often goes undetected. A double bile duct is part of normal embryogenesis and failure of regression of the double bile duct is the mechanism for the development of the type I anomaly. In the present case, the anomaly was found incidentally in a patient who had a pancreaticoduodenectomy for an ampullary carcinoma. However, duplication may also be associated with choledocholithiasis, cholangitis and pancreatitis and it is important for clinicians to be aware of this condition.
Conflict of Interest
None of the authors has a direct conflict of interest to declare. DNL has received an unrestricted educational grant from B. Braun for unrelated work. He has also received speaker’s honoraria for unrelated work from Abbott, Nestlé and Corza.
Funding
This work was supported by the National Institute for Health Research Nottingham Biomedical Research Centre (NIHR203310) and a charitable grant from the Legacy of Norton and Anne Collier. The funders had no role in the design or conduct of the work, or in the decision to publish. This paper presents independent research. The views expressed are those of the authors and not necessarily those of the funders, NHS or the Department of Health.
Patient consent
Written informed consent has been obtained from the patient for publication of this case report.
Acknowledgements
The authors thank Maria Birch for drawing Figure 1 and for the photomicrographs.
REFERENCES
- 1.Goor DA, Ebert PA. Anomalies of the biliary tree. Report of a repair of an accessory bile duct and review of the literature. Arch Surg. 1972 Mar;104(3):302–9. doi: 10.1001/archsurg.1972.04180030050012. [DOI] [PubMed] [Google Scholar]
- 2.Vesalius A. Andreae Vesalii Bruxellensis, Invictissimi Caroli V. Imperatoris medici, de Humani corporis fabrica Libri septem. Per Ioannem Oporinum; p. 1555. [Google Scholar]
- 3.Choi E, Byun JH, Park BJ, et al. Duplication of the extrahepatic bile duct with anomalous union of the pancreaticobiliary ductal system revealed by MR cholangiopancreatography. Br J Radiol. 2007 Jul;80(955):e150–4. doi: 10.1259/bjr/50929809. [DOI] [PubMed] [Google Scholar]
- 4.Sheng H, Chen G, Yang M, et al. A proposed feasible classification of common bile duct duplications based on a newly described variant and review of existing literature. BMC Pediatr. 2022 Nov 8;22(1):647. doi: 10.1186/s12887-022-03708-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arora A, Sureka B, Kasana V, et al. Common bile duct duplication: the more the murkier. Saudi J Gastroenterol. 2015 Jan-Feb;21(1):51–4. doi: 10.4103/1319-3767.151231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta V, Chandra A. Duplication of the extrahepatic bile duct. Congenit Anom (Kyoto) 2012 Sep;52(3):176–8. doi: 10.1111/j.1741-4520.2011.00341.x. [DOI] [PubMed] [Google Scholar]
- 7.Chen G, Wang H, Zhang L, et al. Double common bile duct with choledochal cyst and cholelithiasis: report of a case. Surg Today. 2014 Apr;44(4):778–82. doi: 10.1007/s00595-013-0561-1. Epub 2013 Apr 4. [DOI] [PubMed] [Google Scholar]
- 8.Fan X, He L, Khadaroo PA, et al. Duplication of the extrahepatic bile duct: A case report and review of the literatures. Medicine (Baltimore) 2018 Feb;97(8):e9953. doi: 10.1097/MD.0000000000009953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teilum D. Double common bile duct. Case report and review. Endoscopy. 1986 Jul;18(4):159–61. doi: 10.1055/s-2007-1018360. [DOI] [PubMed] [Google Scholar]
- 10.Yamashita K, Oka Y, Urakami A, et al. Double common bile duct: a case report and a review of the Japanese literature. Surgery. 2002 Jun;131(6):676–81. doi: 10.1067/msy.2002.124025. [DOI] [PubMed] [Google Scholar]
- 11.Djuranovic SP, Ugljesic MB, Mijalkovic NS, et al. Double common bile duct: a case report. World J Gastroenterol. 2007 Jul 21;13(27):3770–2. doi: 10.3748/wjg.v13.i27.3770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim SW, Park DH, Shin HC, et al. Duplication of the extrahepatic bile duct in association with choledocholithiasis as depicted by MDCT. Korean J Radiol. 2008 Nov-Dec;9(6):550–4. doi: 10.3348/kjr.2008.9.6.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JH, Yu JS, Park MS, et al. MR cholangiography of accessory bile duct connected to the stomach. AJR Am J Roentgenol. 2007 Dec;189(6):W344–7. doi: 10.2214/AJR.05.1570. [DOI] [PubMed] [Google Scholar]