Abstract
Purpose:
In this study the relationship between intraoperative haemodynamic status and postoperative intensive care unit (ICU) admission among older patients with cancer is explored.
Methods:
Patients aged ≥75 who underwent elective oncologic surgery lasting ≥120 minutes were analysed. Chi-squared and t-tests were used to assess the associations between intraoperative variables with postoperative ICU admission. Multivariable regressions were used to analyse potential predict risk factors for postoperative ICU admission.
Results:
Out of 994 patients, 48 (4.8%) were admitted to the ICU within 30-days following surgery. ICU admission was associated with the presence of ≥4 comorbid conditions, intraoperative blood loss ≥100mL, and intraoperative tachycardia and hypertensive urgency. On multivariable analysis, operation time ≥240 minutes (OR=2.29, p=0.01), and each minute spent with intraoperative hypertensive urgency (OR=1.06, p=0.01) or tachycardia (OR=1.01, p=0.002) were associated with postoperative ICU admission.
Conclusion:
Intraoperative hypertensive urgency and tachycardia were associated with postoperative ICU admission in older patients undergoing cancer surgery.
Keywords: Geriatrics, Hypertensive Urgency, Intensive Care Unit Admission, Perioperative Outcome, Haemodynamics, Tachycardia
INTRODUCTION
The average age of much of the industrialized world is continuing to rise. For example, Parry et al (2011) estimated that by 2030, 19.3% of the population of the United States will be over the age of 65 and Ortman et al (2014) estimated that by 2050 the number of people over 65 will nearly double. This concept is not new to the population of Europe and the United Kingdom, where the phenomena of aging was first described and which have some of the oldest populations in the world (Carpenter 2005). Since older age has been previously shown to be the most significant factor for developing cancer (Howlader et al 2011), the number of older adults with cancer will almost surely continue to rise.
Surgery is one of the primary treatment options for many cancers. While it has been previously thought that old age should be a deterrent for undergoing surgery, recent studies (Korc-Grodzicki et al 2014, Marsoner et al 2016) have shown that in oncologic surgical decision making, age per se, should not be a factor. Instead of age, fitness or frailty of patients should be evaluated in the preoperative evaluation. The gold standard for assessing frailty is the comprehensive geriatric assessment (CGA) (Feng et al 2015, Wildiers et al 2014). CGA is a multidimensional assessment of older patients with cancer which includes assessment of various significant health factors such as functional activity, nutritional status, and comorbidities. Previous studies (Feng et al 2015, Partridge et al 2015) have shown that CGA is a better predictor of postoperative outcomes in older patients with cancer than age alone. Frailty, as measured by CGA, has been strongly associated with increased postoperative complications and mortality (Cadwell et al 2020, Handforth et al 2015, Kristjansson et al 2010, Lin et al 2016).
Another, less studied, factor associated with postoperative complications and mortality is intraoperative haemodynamic variables. The literature strongly suggests that intraoperative hypotension correlates with a variety of negative outcomes. For example, Sessler and Khanna, in their 2018 systematic review, described the association between intraoperative hypotension and myocardial injury, kidney injury, and postoperative mortality. A review of the literature suggested no benefit of managing intraoperative hypertension below 180/110mmHg. In fact, the management of mild intraoperative hypertension may cause more harm due to the increased risk of hypotension (Ahuja & Charap 2010). However, the literature on intraoperative hypertension and outcomes, especially amongst older patients, has been scarce and inconclusive (Abbott et al 2018, Wu et al 2017, Yang et al 2016).
Among adverse postoperative outcomes, admission to the intensive care unit (ICU) is one of the most significant postoperative events. It causes a significant medical, social, psychological, and economic burden on patients and their families (Gruenberg et al 2006), especially in the cancer population (Staudinger et al 2000). However, research on the impact of various intraoperative haemodynamic variables on the incidence of postoperative ICU admission among older patients with cancer is limited. In this study, the authors aim to assess the relationship between intraoperative variables and the incidence of postoperative ICU admission among older adults with cancer who underwent surgery lasting ≥120 minutes.
METHODS
Study Population:
A retrospective analysis of patients with cancer age 75 or older presenting to the geriatrics service of the authors’ institution for preoperative evaluation before undergoing oncologic surgery was undergone. At the authors’ institution, approximately 80% of patients age 75 or older are referred to the geriatrics service for preoperative evaluation. At this evaluation, all patients undergo a CGA by electronic Rapid Fitness Assessment (eRFA) (Cadwell et al 2020, Shahrokni et al 2017b). Geriatricians discussed the result of their evaluation with the surgical and anaesthesiology teams via email. Patients were followed by the geriatrics service in the postoperative period in a shared care model (Shahrokni et al 2017a). The remainder of patients receive preoperative clearance by either their local primary care provider or other subspecialists such as cardiologists. Surgical services at the authors’ institution do not use standard frailty screening tools for referral to the geriatrics service. Patients were included in the study if their surgery lasted ≥120 minutes. This study protocol received Institutional Review Board approval.
Measurements:
Outcome of Interest:
The primary outcome of interest was admission to the ICU within 30 days after surgery. This length of time has been used in various studies across cancer and non-cancer surgical fields to assess for postoperative complications (Fisher et al 2017, Goel et al 2019, Quero-Valenzuela et al 2018, Wu et al 2019). This was retrieved from electronic medical records.
Major covariates:
-
Intraoperative variables:
The variables retrieved from the anaesthesia information management system (AIMS) included total operation time (in minutes), intraoperative blood loss (in millilitres), average intraoperative heart rate, mean arterial blood pressure (MABP), non-invasive systolic blood pressure (SBP), and non-invasive diastolic blood pressure (DBP). Average pulse pressure was calculated as average SBP minus average DBP. Initial intraoperative data captures included first intraoperative heart rate, MABP, SBP, and DBP.
Lastly, minutes spent in opposing extremes of intraoperative conditions was recorded: 1- heart rate of <60 beats per minute, 2- heart rate of >100 beats per minute, 3- systolic blood pressure <80mmHg, 4- systolic blood pressure >180mmHg, 5- diastolic blood pressure <40mmHg, 6- diastolic blood pressure >100mmHg, 7- MABP <60mmHg, and 8- MABP >130mmHg. Similar intraoperative categorizations have been used in numerous studies on the effects of intraoperative haemodynamics on surgical outcomes. (Abbott et al 2018, Monk et al 2015, Reich et al 2002, Yang et al 2016).
Preoperative CGA (via the eRFA): The domains, instruments, ranges, and cut-offs of the CGA can be found in Table 1.
Table 1:
Electronic Rapid Fitness Assessment Domains and Instruments
| Domain | Instrument | Description | Score range or answers | Abnormal cutoff score |
|---|---|---|---|---|
| Functional Domain | Basic Activities of Daily Living (bADL) | Assesses patients’ level of independence in performing seven activities; bathing, dressing, grooming, feeding, bladder and bowel control, and walking inside and outside of the house. | Limited a lot (0 points), a little (1 point), or not at all (2 points) | Patients with any limitation in any of these activities (<14 points) |
| Instrumental Activities of Daily Living (iADL) | Assesses patients’ level of independence in eight activities; telephone use, doing laundry, shopping, preparing meals, doing housework, handling own medications, handling money and finances, and transportation. | Unable to perform activity (0 points), needed some help (1 point), did not need any help (2 points) | Patients who needed any help with any of these activities (<16 points) | |
| Patient-rated Karnofsky Performance Status (p-KPS) | Patients were asked to rate their performance status using p-KPS. A higher score indicates better performance. | 30–100 | ≤80 | |
| Fall in the past year | Number of falls | No falls,1 fall, >1 fall | ≥1 fall | |
| Timed Up and Go test | Patients were asked by the geriatrics nurses to stand from the chair, walk ten feet, turn and return to the chair. | < 10 seconds, 10–19 seconds, ≥ 20 seconds |
≥10 seconds | |
| Social Support/Activity | Medical Outcome Study-Social Support Survey- | Four 5-point Likert scale questions addressing 4 domains of social support: emotional/informational, tangible, affectionate, and positive social interaction. A higher score indicates better social support. | 4–20 | ≤16 |
| Medical Outcome Study, Social Activity survey | Three 5-point Likert scale questions addressing the interference of patient’s health condition with the social activity. A higher score means more health-related interference with social activities. | 3–15 | ≥8 | |
| Cognition | Mini-Cog | Clock-drawing test (CDT) and 3-word recall. Normal CDT gets 2 points, and each recalled word gets 1 point. | 0–5 | ≤2 |
| Emotional wellbeing | Distress-Measured by Distress Thermometer | Patients are asked about level of distress in the past 2 weeks. 0 means no distress at all; 10 means extreme distress | 0–10 | ≥4 |
| Depression-Measured by Geriatric Depression Scale-4 item questionnaire | Four yes/no questions regarding patient’s psychological status | 0–4 | ≥1 | |
| Poly-pharmacy | Patient-reported | Number of medications | ≥0 medications | ≥5 medications |
| Nutritional Status | Patient-reported | Weight change in the past 6 months | ≥0 pounds lost | ≥10 pounds loss |
| Poly-comorbid conditions | ICD9/10 codes for claims submitted within the first 48 hours of hospital stay. | The 13 comorbid conditions of interest were: coronary artery disease, or atrial fibrillation, or atrial flutter, or myocardial infarction, or cardiomyopathy, or heart failure; dementia, or Alzheimer’s, or Lewy body disease, or memory loss, or MCI, or delirium; arthritis or degenerative joint disease; chronic obstructive pulmonary disease/asthma or pneumonia; cerebrovascular accident or transient ischemic attack; diabetes; hypertension; kidney failure; lipid disorders; liver diseases; peptic ulcer disorder; peripheral vascular disease; and thyroid diseases | 0–13 conditions | ≥4 comorbid |
Other covariates:
Sociodemographic characteristics (age, gender, marital status, educational status and living condition), American Society of Clinical Anesthesiologists – Performance Status (ASA-PS) classification, and type of surgery.
Statistical analysis:
Chi-squared and t-tests were used to assess the association between categorical and continuous variables with postoperative ICU admission. Significant associations (p<0.05) were included in the multivariable regression analyses with postoperative ICU admission as dependent and all other variables as independent variables. Furthermore, the association between frailty and time spent with intraoperative SBP >180mmHg and/or heart rate >100 beats per minute was assessed.
RESULTS
Patient characteristics
The patient sample included a total of 994 patients with a median age of 79 (range 75–100) undergoing cancer surgery between 2015 and 2017. In total, 482 were male (48.5%), 557 were married (56.0%), and 673 (67.7%) were living with their spouse, family, or partner. The most common surgical procedures, with more than 5% of the whole cohort, were gynaecological surgery (164 patients, 16.5%), hemi-colectomy (152 patients, 15.3%), modified and radical neck dissection (99 patients, 10.0%), pancreatectomy (90 patients, 9.1%), cystectomy (77 patients, 7.7%), hepatobiliary surgery (75 patients, 7.5%), lung resection (70 patients, 7.0%), orthopaedic surgery (57 patients, 5.7%), and small bowel resection (51 patients, 5.1%).
Out of 994 patients, 48 (4.8%) were admitted to the ICU within 30-days postoperatively, while 946 (95.2%) patients were not. Patients with ICU admission were more likely to be male (62.5% vs. 47.8%, p=0.04) and to be living with family (77.1% vs 67.5%, p=0.03). Patients who were admitted to the ICU had longer operation times (p=0.005) and experienced more intraoperative blood loss compared to patients without ICU admission (p=0.01) [Table 2].
Table 2:
Sociodemographic and intraoperative characteristics of older patients with cancer who were and were not admitted to ICU postoperatively
| No Postoperative ICU Admission N=946, 95.2% |
Postoperative ICU admission N=48, 4.8% | P-Value | |
|---|---|---|---|
|
| |||
| Age (mean/SD) | 79.9 (4.1) | 80.3 (5.0) | 0.5 |
|
| |||
| Male | 452 (47.8%) | 30 (62.5%) | 0.04 |
|
| |||
| Married | 526 (55.8%) | 31 (66%) | 0.6 |
|
| |||
| College graduate or higher | 455 (48.3%) | 18 (38.3%) | 0.5 |
|
| |||
| Living with family | 636 (67.5%) | 37 (77.1%) | 0.03 |
|
| |||
| ASA-PS | 0.07 | ||
| II | 78 (8.2%) | 2 (4.2%) | |
| III | 818 (86.5%) | 40 (83.3%) | |
| IV | 50 (5.3%) | 6 (12.5%) | |
|
| |||
| Operation time | 0.005 | ||
| 120–239 minutes | 605 (64%) | 21 (43.8%) | |
| ≥240 minutes | 341 (36%) | 27 (56.3%) | |
|
| |||
| Intraoperative blood loss | 0.01 | ||
| <100 mL | 346 (40%) | 9 (21.4%) | |
| ≥100 mL | 518 (60%) | 33 (78.6%) | |
|
| |||
| Average intraoperative heart rate (beats per min) | 68 (8) | 71 (9) | 0.006 |
|
| |||
| Average intraoperative MABP (mmHg) | 82 (10) | 83 (10) | 0.29 |
|
| |||
| Average intraoperative SBP (mmHg) | 121 (17) | 124 (17) | 0.20 |
|
| |||
| Average intraoperative DBP (mmHg) | 63 (8) | 64 (7) | 0.46 |
|
| |||
| First intraoperative heart rate (beats per min) | 71 (14) | 72 (15) | 0.65 |
|
| |||
| First MABP (mmHg) | 94 (21) | 98 (26) | 0.16 |
|
| |||
| First DBP (mmHg) | 71 (15) | 75 (19) | 0.08 |
|
| |||
| First SBP (mmHg) | 141 (35) | 146 (43) | 0.31 |
|
| |||
| Time spent with heart rate <60 (min) | 97 (132) | 89 (122) | 0.66 |
|
| |||
| Time spent with heart rate >100 (min) | 5.44 (18) | 18.12 (35) | <0.001 |
|
| |||
| Time spent with SBP <80 (min) | 2.9 (4.3) | 3.3 (5.1) | 0.48 |
|
| |||
| Time spent with SBP >180 (min) | 2.3 (4.1) | 4.33 (9.1) | 0.003 |
|
| |||
| Time spent with DBP <40 (min) | 0.6 (1.7) | 0.9 (2.6) | 0.45 |
|
| |||
| Time spent with DBP >100 (min) | 0.74 (2.1) | 1.0 (2.1) | 0.29 |
|
| |||
| Time spent with MABP <60 (min) | 4.0 (6.2) | 4.7 (7.7) | 0.46 |
|
| |||
| Time spent with MABP >130 (min) | 0.78 (2.2) | 1.33 (2.9) | 0.09 |
|
| |||
| Pulse pressure (mmHg) | 57 (15) | 57 (14) | 0.16 |
ICU, Intensive care unit
ASA-PS, American Society of Clinical Anesthesiologists – Performance Status
MABP, Mean arterial blood pressure
SBP, Systolic blood pressure
DBP, Diastolic blood pressure
Table 2 also shows the relationship between intraoperative variables and ICU admission. The average intraoperative heart rate was higher in ICU patients than in non-ICU patients (p=0.006). Patients admitted to the ICU postoperatively spent longer times with heart rate >100 beats per minute intraoperatively (18.12 vs. 5.44 minutes p<0.001) compared to those without ICU admission. Finally, patients who were subsequently admitted to the ICU spent more time with intraoperative SBP of >180mmHg (4.33 vs. 2.3 minutes, p=0.003) compared to patients without an ICU admission.
Figure 1 shows the relationship between presence of frailty markers measured for in the eRFA and prevalence of postoperative ICU admission. The only frailty measure significantly different between patients with and without an ICU admission was the presence of ≥4 poly-comorbid conditions (p<0.01). Of the 13 comorbid conditions tested for in the eRFA, cerebrovascular accident (CVA), peripheral vascular disease (PVD), kidney disease, and coronary artery disease (CAD) were significantly associated with postoperative ICU admission (p<0.05) [Figure 2].
Figure 1: Prevalence of geriatric deficits among patients who were or were not admitted to the ICU after surgery.
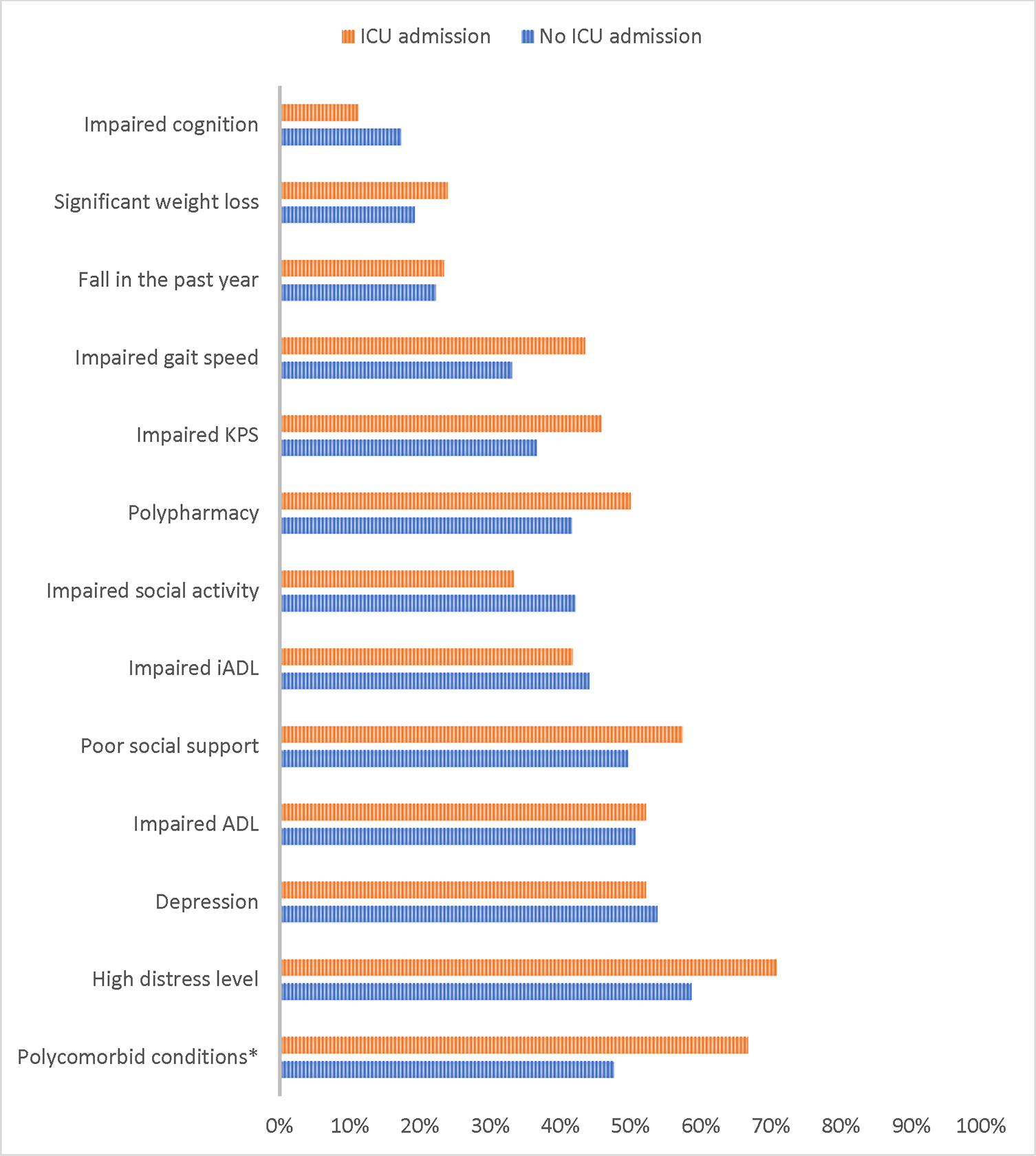
*p<0.05
ICU, Intensive care unit
KPS, Karnofsky performance status
iADL, Instrumental activities of daily living
ADL, Activities of daily living
Figure 2: Prevalence of comorbid conditions among patients who were or were not admitted to the ICU after surgery.
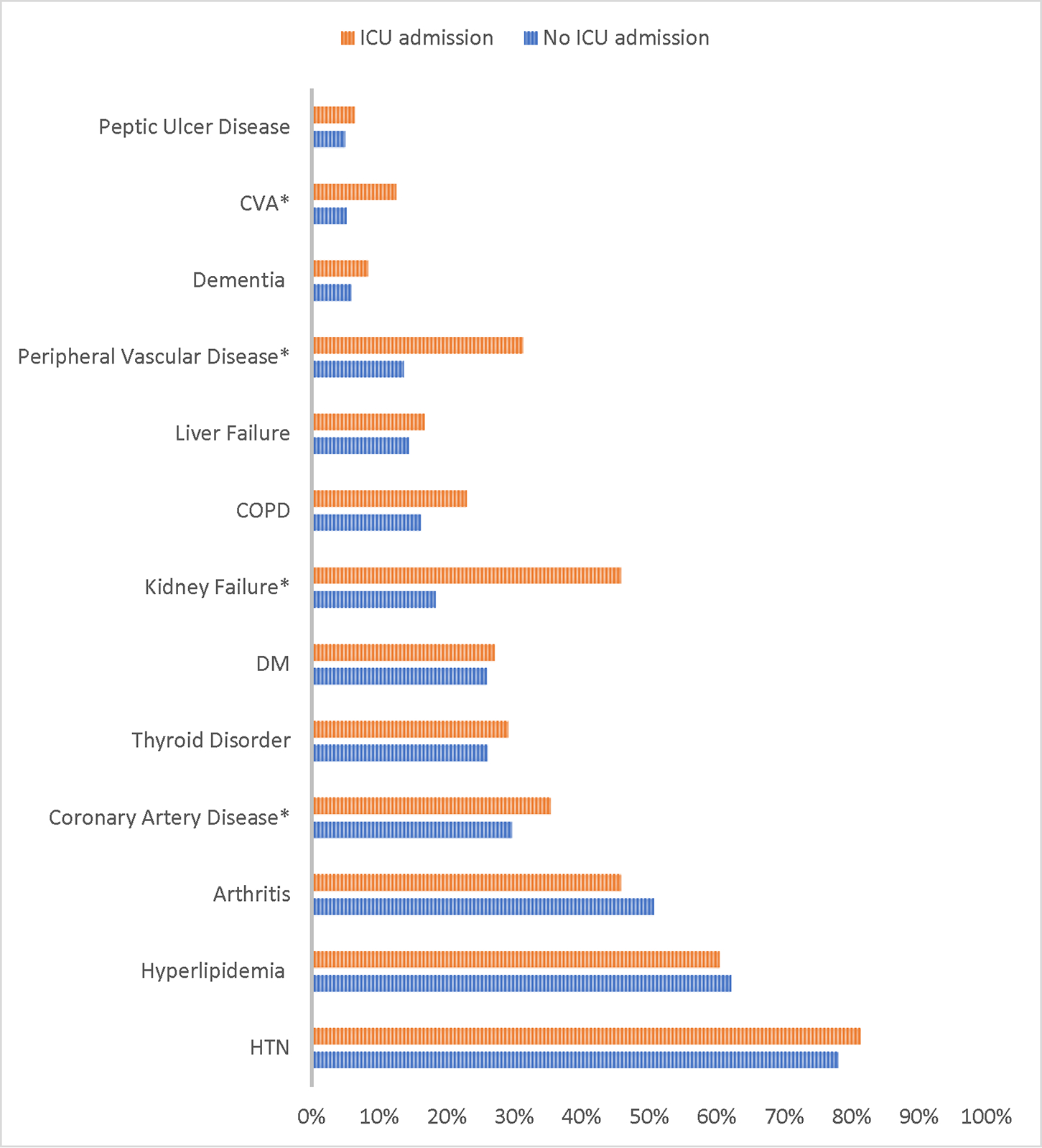
*p<0.05
ICU, Intensive care unit
CVA, Cerebrovascular accident
COPD, Chronic obstructive pulmonary disease
DM, Diabetes mellitus
HTN, Hypertension
Table 3 shows the result of the multivariable analysis. Operation time ≥240 minutes was shown to be associated with an increased odds of ICU admission (OR=2.29, p=0.01). Each minute of time spent with SBP >180mmHg or heart rate >100 had a 6% (OR=1.06, p=0.01) or 1% (OR=1.01, p=0.002) increased odds of postoperative ICU admission, respectively. Following adjustment for associated polycomorbid conditions and gender, time spent with heart rate >100 and SBP >180mmHg were still shown to be associated with postoperative ICU admission.
Table 3:
Multivariable analyses of the relationship between intraoperative haemodynamic status and ICU admission
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Operation time ≥240 minutes | 2.29 | 1.17–4.50 | 0.01 | ||||||
| Intraoperative blood loss ≥100 mL | 1.87 | 0.85–4.11 | 0.1 | ||||||
| Time spent with heart rate >100 (min) | 1.01 | 1.005–1.023 | 0.002 | 1.01 | 1.004–1.021 | 0.004 | |||
| Time spent with SBP >180 (min) | 1.06 | 1.01–1.10 | 0.01 | 1.04 | 1.003–1.094 | 0.03 | |||
| Average heart rate (beats per min) | 1.035 | 0.87–1.22 | 0.690 | ||||||
| Coronary Artery Disease | 1.46 | 0.76–2.81 | 0.2 | 1.45 | 0.75–2.81 | 0.2 | |||
| Cerebrovascular Disease | 1.58 | 0.59–4.22 | 0.3 | 1.61 | 0.60–4.32 | 0.3 | |||
| Peripheral Vascular Disease | 2.01 | 1.01–3.99 | 0.04 | 2.16 | 1.10–4.23 | 0.02 | |||
| Kidney Failure | 3.26 | 1.76–6.04 | <0.001 | 2.87 | 1.54–5.38 | 0.001 | |||
ICU, Intensive care unit
SBP, Systolic blood pressure
DISCUSSION
In this study the relationship between intraoperative haemodynamic variables and the likelihood of ICU admission among older patients who underwent cancer surgery lasting ≥120 minutes was assessed. This analysis suggests that among intraoperative variables, operation time ≥240 minutes, time spend with heart rate >100, and time spent with SBP >180mmHg were associated with a higher likelihood of ICU admission after adjustment for comorbid conditions and gender.
Preoperative hypertension affects 25% of patients undergoing surgery, however, the incidence increases significantly with older age (Varon & Marik 2008). SBP of >180mmHg is often considered a hypertensive urgency (Desai et al 2009). However, in contrast to intraoperative hypotension which is well studied and is strongly correlated with postoperative adverse outcomes such as acute kidney injury (AKI) (Salmasi et al 2017, Sun et al 2015, Walsh et al 2013), myocardial injury (Salmasi et al 2017, Walsh et al 2013), and delirium (Hirsch et al 2015), the relationship between intraoperative hypertensive urgency and postoperative adverse outcomes is less investigated. In a study of 797 patients who underwent non-cardiac surgery, Reich et al (2002) evaluated the relationship between intraoperative variables and negative surgical outcomes defined as length of stay greater than ten days and postoperative mortality or morbidity. While they found no relationship between intraoperative variables and negative surgical outcomes among patients who underwent surgery of shorter duration, patients with intraoperative SBP of >160mmHg experienced higher rates of negative surgical outcomes (OR=2.09, p=0.009). It is important to note that the median age of this cohort (60 years) was younger than the cohort of this study which only included patients aged 75 or older.
In a prospective international cohort study of noncardiac surgeries, Abbott et al (2018) assessed the relationship between intraoperative haemodynamic variables and myocardial injury. The average age of the cohort was 65 years. In this study, 1,197 of 15,109 patients (7.9%) had myocardial injury after surgery. Maximum SBP of >160mmHg was associated with an increased likelihood of myocardial injury (OR=1.16, p=0.04) as well as myocardial infarction (OR=1.34, p=0.01).
Yang et al (2016) also found that intraoperative hypertension and tachycardia negatively affect outcomes, specifically postoperative delirium in older patients undergoing major surgery. Wu et al (2017) studied a population of patients with chronic hypertension undergoing major gastrointestinal surgery. They performed a prospective randomized study assigning patients into three groups that determined their strictly controlled range of intraoperative MAP: level I (65–79mmHg), level II (80–95mmHg), and level III (96–110mmHg). The results of the study revealed that level I and level III patients had an increased risk for AKI while level II patients were at a reduced risk for pneumonia and ICU admission, while having a lower average length of stay.
This study provides evidence that intraoperative hypertensive urgency and tachycardia are associated with an increased risk of postoperative ICU admission among older patients with cancer undergoing surgical procedures lasting more than two hours. In addition, the relationship between aging-related impairments assessed via GA and postoperative ICU admission was assessed. A systematic review by Lin et al (2016) found frailty to be associated with postoperative complications. However, in this analysis it was found that other than multiple comorbid conditions, no other factor in the CGA was associated with ICU admission. Moreover, specific comorbid conditions associated with postoperative ICU admission were mainly vascular diseases such as peripheral vascular disease, coronary artery disease, cerebrovascular disease, and kidney failure. However, even after adjusting for these variables, the duration of intraoperative time that older patients with cancer spent with SBP of >180mmHg and heart rate >100 were still associated with an increased risk of postoperative ICU admission [Table 3].
There are few studies which look at the relationship between frailty, intraoperative haemodynamics, and negative surgical outcomes. A recent study by James et al (2019) investigated this relationship, however their primary aim was to explore blood pressure variability, whereas this study takes into account additional variables. Furthermore, this analysis was unique to older patients with cancer, a cohort that has not had a comparable study done as of this time.
By recognizing the association between intraoperative hypertension and negative outcomes, hospital staff can work to manage hypertension in the preoperative setting, making it easier for anaesthesiologists to manage it in the intraoperative setting. Future larger studies should further assess this relationship among older patients with cancer. Studies should also investigate the relationship between intraoperative SBP of >180mmHg and other postoperative outcomes aside from ICU admission such as kidney function, myocardial injury, and delirium. Considering these findings, it is important to study hypertension in addition to hypotension when reporting intraoperative haemodynamics and postoperative outcomes of older patients with cancer.
This study, especially given its exploratory nature, has its limitations. It is a single institution study in which all older patients with cancer were comanaged by the geriatrics service perioperatively. Assessment of correlation between intraoperative SBP and postoperative outcomes in a larger multi-institutional study will provide further evidence about the strength of such a relationship. Moreover, the authors’ retrieved comorbid conditions from ICD9/10 codes submitted within the first 48 hours of hospital stay. Especially given the four significant comorbid conditions associated with postoperative ICU admission (CVA, PVD, CAD, and kidney disease), future studies should be focused on these four comorbid conditions by further defining their effects. The authors’ also did not take into account the perioperative anti-hypertensive medications of patients, nor did they assess the intraoperative interventions before and after extreme haemodynamic changes. Because of the low event rate of just 48 ICU admissions, further adjustment for other potential confounding variables such as these could not be done. Lastly, this study combines multiple types of geriatric cancer surgeries. This could lead to the results over or understating the effect of intraoperative hypertension from certain types of cancer. Future studies should be done that stratify based on type of cancer in older patients.
Nonetheless, this study has its strengths. It is based on one of the largest cohorts of older patients with cancer. The average age of the cohort is 79, which is significantly older than the vast majority of studies that have explored the correlation between intraoperative haemodynamic variables and postoperative outcomes. There was also extensive data on frailty using the CGA, the gold standard frailty measure, and aging-related impairments which is missing from many prior studies.
CONCLUSION
The duration of intraoperative hypertensive urgency and tachycardia were associated with an increased likelihood of ICU admission among this cohort of older patients with cancer. Future studies should further explore this finding.
Funding:
The project was supported, in part, by the Beatriz and Samuel Seaver Foundation, the Memorial Sloan Kettering Cancer and Aging Program, and NIH/NCI Cancer Center Support Grant P30 CA008748 and R25 CA020449.
Footnotes
Declaration of interests: GWF discloses personal fees and non-financial support from Edwards Life Sciences, outside of submitted work. AMA is a consultant for Pacira and Merck. All remaining authors have nothing to disclose.
References
- Abbott TEF, Pearse RM, Archbold RA, et al. 2018. A Prospective International Multicentre Cohort Study of Intraoperative Heart Rate and Systolic Blood Pressure and Myocardial Injury After Noncardiac Surgery: Results of the VISION Study. Anesthesia & Analgesia 126 (6) 1936–1945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahuja K and Charap MH 2010. Management of perioperative hypertensive urgencies with parenteral medications. Journal of Hospital Medicine 5 (2) E11–16 [DOI] [PubMed] [Google Scholar]
- Cadwell JB, Afonso AM and Shahrokni A 2020. Prognostic nutritional index (PNI), independent of frailty is associated with six-month postoperative mortality. Journal of Geriatric Oncology 11 (5) 880–884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter GI 2005. Aging in the United Kingdom and Europe—A Snapshot of the Future? Journal of the American Geriatrics Society 53 (9s) S310–S313 [DOI] [PubMed] [Google Scholar]
- Desai RG, Muntazar M and Goldberg ME 2009. Strategies for managing perioperative hypertension. Current Hypertension Reports 11 (3) 173–177 [DOI] [PubMed] [Google Scholar]
- Feng MA, McMillan DT, Crowell K, et al. 2015. Geriatric assessment in surgical oncology: a systematic review. Journal of Surgical Research 193 (1) 265–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher AV, Fernandes-Taylor S, Campbell-Flohr SA, et al. 2017. 30-day Readmission After Pancreatic Resection: A Systematic Review of the Literature and Meta-analysis. Annals of Surgery 266 (2) 242–250 [DOI] [PubMed] [Google Scholar]
- Goel AN, Badran KW, Mendelsohn AH, et al. 2019. Readmission after surgery for oropharyngeal cancer: An analysis of rates, causes, and risk factors. Laryngoscope 129 (4) 910–918 [DOI] [PubMed] [Google Scholar]
- Gruenberg DA, Shelton W, Rose SL, et al. 2006. Factors influencing length of stay in the intensive care unit. American Journal of Critical Care 15 (5) 502–509 [PubMed] [Google Scholar]
- Handforth C, Clegg A, Young C, et al. 2015. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Annals of Oncology 26 (6) 1091–1101 [DOI] [PubMed] [Google Scholar]
- Hirsch J, DePalma G, Tsai TT, et al. 2015. Impact of intraoperative hypotension and blood pressure fluctuations on early postoperative delirium after non-cardiac surgery. British Journal of Anaesthesia 115 (3) 418–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlader N, Noone A, Krapcho M, et al. 2011. SEER cancer statistics review, 1975–2008, National Cancer Institute. Bethesda, MD [Google Scholar]
- James LA, Levin MA, Lin H-M, et al. 2019. Association of Preoperative Frailty With Intraoperative Hemodynamic Instability and Postoperative Mortality. Anesthesia & Analgesia 128 (6) 1279–1285 [DOI] [PubMed] [Google Scholar]
- Korc-Grodzicki B, Downey RJ, Shahrokni A, et al. 2014. Surgical considerations in older adults with cancer. Journal of Clinical Oncology 32 (24) 2647–2653 [DOI] [PubMed] [Google Scholar]
- Kristjansson SR, Nesbakken A, Jordhøy MS, et al. 2010. Comprehensive geriatric assessment can predict complications in elderly patients after elective surgery for colorectal cancer: a prospective observational cohort study. Critical Reviews in Oncology/Hematology 76 (3) 208–217 [DOI] [PubMed] [Google Scholar]
- Lin HS, Watts JN, Peel NM, et al. 2016. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatrics 16 (1) 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsoner K, Kornprat P, Sodeck G, et al. 2016. Pancreas Cancer Surgery in Octogenarians - Should We or Should We Not? Anticancer Research 36 (4) 1979–1984 [PubMed] [Google Scholar]
- Monk TG, Bronsert MR, Henderson WG, et al. 2015. Association between Intraoperative Hypotension and Hypertension and 30-day Postoperative Mortality in Noncardiac Surgery. Anesthesiology 123 (2) 307–319 [DOI] [PubMed] [Google Scholar]
- Ortman JM, Velkoff VA and Hogan H 2014. An aging nation: the older population in the United States. Current Population Reports, P25–1140. U.S. Census Bereau, Washington, DC [Google Scholar]
- Parry C, Kent EE, Mariotto AB, et al. 2011. Cancer survivors: a booming population. Cancer Epidemiology, Epidemiology, Biomarkers & Prevention 20 (10) 1996–2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partridge JS, Harari D, Martin FC, et al. 2014. The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia 69 Suppl 1 8–16 [DOI] [PubMed] [Google Scholar]
- Quero-Valenzuela F, Piedra-Fernández I, Martínez-Ceres M, et al. 2018. Predictors for 30-day readmission after pulmonary resection for lung cancer. Journal of Surgical Oncology 117 (6) 1239–1245 [DOI] [PubMed] [Google Scholar]
- Reich DL, Bennett-Guerrero E, Bodian CA, et al. 2002. Intraoperative tachycardia and hypertension are independently associated with adverse outcome in noncardiac surgery of long duration. Anesthesia & Analgesia 95 (2) 273–277 [DOI] [PubMed] [Google Scholar]
- Salmasi V, Maheshwari K, Yang D, et al. 2017. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology 126 (1) 47–65 [DOI] [PubMed] [Google Scholar]
- Sessler DI and Khanna AK 2018. Perioperative myocardial injury and the contribution of hypotension. Intensive Care Medicine 44 (6) 811–822 [DOI] [PubMed] [Google Scholar]
- Shahrokni A, Kim SJ, Bosl GJ, et al. 2017a. How We Care for an Older Patient With Cancer. Journal of Oncology Practice 13 (2) 95–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahrokni A, Tin A, Downey RJ, et al. 2017b. Electronic Rapid Fitness Assessment: A Novel Tool for Preoperative Evaluation of the Geriatric Oncology Patient. Journal of the National Comprehensive Cancer Network 15 (2) 172–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staudinger T, Stoiser B, Müllner M, et al. 2000. Outcome and prognostic factors in critically ill cancer patients admitted to the intensive care unit. Critical Care Medicine 28 (5) 1322–1328 [DOI] [PubMed] [Google Scholar]
- Sun LY, Wijeysundera DN, Tait GA, et al. 2015. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 123 (3) 515–523 [DOI] [PubMed] [Google Scholar]
- Varon J and Marik PE 2008. Perioperative hypertension management. Vascular Health and Risk Management 4 (3) 615–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh M, Devereaux PJ, Garg AX, et al. 2013. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology 119 (3) 507–515 [DOI] [PubMed] [Google Scholar]
- Wildiers H, Heeren P, Puts M, et al. 2014. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. Journal of Clinical Oncology 32 (24) 2595–2603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu WW, Zhang WH, Zhang WY, et al. 2019. Risk factors of the postoperative 30-day readmission of gastric cancer surgery after discharge: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 98 (10) e14639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X, Jiang Z, Ying J, et al. 2017. Optimal blood pressure decreases acute kidney injury after gastrointestinal surgery in elderly hypertensive patients: A randomized study: Optimal blood pressure reduces acute kidney injury. Journal of Clinical Anesthesia 43 77–83 [DOI] [PubMed] [Google Scholar]
- Yang L, Sun DF, Han J, et al. 2016. Effects of Intraoperative Hemodynamics on Incidence of Postoperative Delirium in Elderly Patients: A Retrospective Study. Medical Science Monitor 22 1093–1100 [DOI] [PMC free article] [PubMed] [Google Scholar]


