Abstract
Participatory approaches to implementation science (IS) offer an inclusive, collaborative, and iterative perspective on implementing and sustaining evidence-based interventions (EBIs) to advance health equity. This review provides guidance on the principles and practice of participatory IS, which enables academic researchers, community members, implementers, and other actors to collaboratively integrate practice-, community-, and research-based evidence into public health and health care services. With a foundational focus on supporting academics in coproducing knowledge and action, participatory IS seeks to improve health, reduce inequity, and create transformational change. The three main sections of this review provide (a) a rationale for participatory approaches to research in implementation science, (b) a framework for integrating participatory approaches in research utilizing IS theory and methods, and (c) critical considerations for optimizing the practice and impact of participatory IS. Ultimately, participatory approaches can move IS activities beyond efforts to make EBIs work within harmful systems toward transformative solutions that reshape these systems to center equity.
Keywords: community-based participatory research, implementation science, health inequities, social justice, implementation science, community engagement
1. INTRODUCTION
Participatory approaches to implementation science (IS) offer an inclusive, collaborative, and iterative perspective on promoting, implementing, and sustaining evidence-based interventions (EBIs) to advance health equity. This review provides an overview of the rationale and critical considerations for pursuing this approach to research, as well as a framework to guide participatory IS efforts. A participatory approach engages a wide range of actors to integrate practice-, community-, and research-based evidence into public health and health care services. Through inclusive coconstruction of knowledge and action, participatory IS aims to improve health, reduce health inequities, and create transformational change in systems that influence health (92, 93). Drawing on long-standing and critical principles of community engagement and participatory research traditions (50, 130), we describe how a participatory IS approach can enhance implementation and sustainment of EBIs to advance health equity. We illustrate this approach with examples drawn from existing literature. Our review offers tools and strategies for conducting participatory IS and critical considerations for enhancing effective participation. We also invite further reflection on persistent challenges and opportunities to optimize the potential of participatory IS to advance public health and health equity.
IS offers tools to increase the quality and accessibility of services delivered to the public by integrating EBIs into routine public health and health care practice (10). However, many common IS approaches and frameworks lack an explicit, foundational focus on addressing health inequities (16, 87). Additionally, IS efforts typically employ a top-down approach, emphasizing expertise held by academics and positioning other vital actors in the system (e.g., implementers, policy makers, or service users) as passive information sources or executors of tasks and activities (54). In contrast with linear knowledge transfer models, participatory approaches are rooted in a model of iterative cocreation of knowledge and action within a given context (43), with an emphasis on including perspectives often excluded from the scientific and practice evidence base (e.g., perspectives rooted in lived experience) (50, 92). Participatory IS prompts teams to expand their focus beyond making EBIs work within harmful systems toward implementation efforts that transform systems to center equity. Thus, participatory IS uses inclusive approaches to advance the commitment to addressing health inequities and the unequal/unjust distribution of resources needed for health that so profoundly impacts marginalized populations (13). While scholars are increasingly interested in the connection between participatory approaches and equity-focused IS [e.g., work on integrated knowledge translation (57)], such approaches are not the norm. As an illustration, an examination of IS grants that were active from 2021 to 2022 in the National Institutes of Health portfolio found that of 103 grants, fewer than half (44%) included community/partner engagement and a focus on health inequities (127). Among the grants using engaged approaches, 56% used consultation models, reflecting the lowest levels of engagement, and only 3% used partnership models, reflecting the highest levels of engagement, as defined by Sanders Thompson and colleagues (105).
The COVID-19 pandemic’s trajectory in the United States offers a compelling illustration of the inequitable consequences of top-down approaches. The evidence base highlighting the utility of COVID-19 vaccinations, diagnostic tools, and other mitigation strategies was developed quite quickly. However, taking vaccination as an example, there were striking inequities in accessibility and uptake for groups based on race, ethnicity, socioeconomic status, immigrant status, and other sociodemographic factors. Structural influences impacted social groups differently, resulting in an inequitable distribution of the benefits of EBIs (111). Successful efforts to ensure a more equitable rollout of this EBI (i.e., vaccination) offer insights into the value of a participatory approach. For example, Alonso and colleagues (5) describe how local partners (including government entities, nonprofits, and start-ups) collaborated to analyze data on COVID prevalence to inform targeted, community-led outreach in a low-income, densely populated neighborhood in Massachusetts, home to many Latinx immigrants. By August 2021, adult vaccination rates in this neighborhood exceeded 90%, one of the highest rates in the country among cities with similar demographics (5).
This article introduces readers to the value of participatory approaches for strengthening implementation and sustainment of health-related EBIs and provides a framework for applying the principles, practices, and lessons from participatory research to IS. In Section 2 of this article, we offer a high-level overview of the origins and rationale for participatory research. In Section 3, we provide a framework for integrating participatory approaches into IS theory and methods. In Section 4, we outline selected challenges and considerations for optimizing the potential of participatory IS in future research.
2. CORE ELEMENTS OF PARTICIPATORY APPROACHES TO RESEARCH
Participatory approaches to health-focused research have a long and rich history (for helpful introductions, see 28, 49, 130). While a comprehensive review is beyond the scope of this article, we highlight core elements to support their application to IS. Varied terms are used to describe participatory approaches to research, including community-based participatory research (CBPR), community-engaged research, citizen science, and participatory action research (28, 76, 107). Although not synonymous, these approaches emphasize respect for diverse expertise and processes that enable researchers, community members, and other relevant actors to work together, learn from each other, generate knowledge, and instigate change (33). These varied approaches to engaged research are compatible with various research methods (i.e., tools and techniques for generating and analyzing data). Pioneering early examples of participatory approaches include Kurt Lewin’s model of action research in the 1940s, which centered on the expertise of workers who were engaged in research to improve company operations, and Paulo Freire’s work in the 1960s, which prompted academics to move from conceptualizing individuals and communities as subjects of study to coleaders of inquiry and societal change (35, 62, 75).
Participatory approaches differ from conventional approaches to research by centering relationships between academics and those with lived or professional experience of the focal issue in the knowledge production process. Mutual respect, equitable participation, and trust building are seen as essential to knowledge production alongside the use of rigorous research methods (28, 49). This research approach decenters the hegemonic perspectives of dominant majorities—a pattern that has resulted in a partial and incomplete knowledge base, which in turn has contributed to or reinforced health inequities (78). Participatory approaches grounded in emancipatory principles or Indigenous knowledge production traditions explicitly engage with issues of power and representation to facilitate the meaningful participation of marginalized groups in creating transformational knowledge and change (23, 33, 35). Such change is expansive, with the goal of long-term, radical, and systemic alterations in structures, relationships, and organizations to disrupt the underlying drivers of health inequity (9).
Both instrumental and normative rationales are advan7ced for participatory approaches (41, 68, 79, 82, 119). Fundamental to both is the value of centering the resources and knowledge of actors historically excluded by more top-down approaches. The intentional friction generated through the engagement of diverse perspectives can produce new and different types of knowledge (71). Instrumental arguments focus on the outputs and impacts of participatory research, such as developing (a) a more relevant and useable evidence base; (b) a deeper understanding of local contexts; and (c) capacity, resources, and solutions to address health issues (126, 130). Normative arguments emphasize the value of the research process, as well as outputs, and the potential to advance justice, inclusion, and equity so that marginalized groups can better address factors shaping their health (81, 133a). In these ways, participatory approaches contrast with “helicopter research,” as described by Deloria (31), in which academic researchers enter a site, extract data, and leave without providing value (as defined by the community) to those who participated in or supported the work. Effectively used, participatory approaches can also avoid “damage-centered research,” Tuck’s (123) term for deficit-focused work that creates or cements a narrative that a given community is fundamentally lacking instead of recognizing community assets and focusing on structural forces driving inequities. To advance health equity goals, research teams can strategically select and be guided by participatory approaches that explicitly include health equity improvement as a foundational principle.
3. INTEGRATING PARTICIPATORY APPROACHES INTO IS STUDIES
Participatory IS absorbs the lessons and principles of the rich participatory research traditions described above and situates them relative to the focus of IS, the integration of evidence-based solutions into practice. For example, the CBPR conceptual model developed by Wallerstein and colleagues can be used as a roadmap for using participatory approaches to guide equity-focused IS research and practice (104). Figure 1 illustrates opportunities to apply participatory research principles and processes to IS studies (1, 98, 110, 113, 130, 137).
Figure 1.
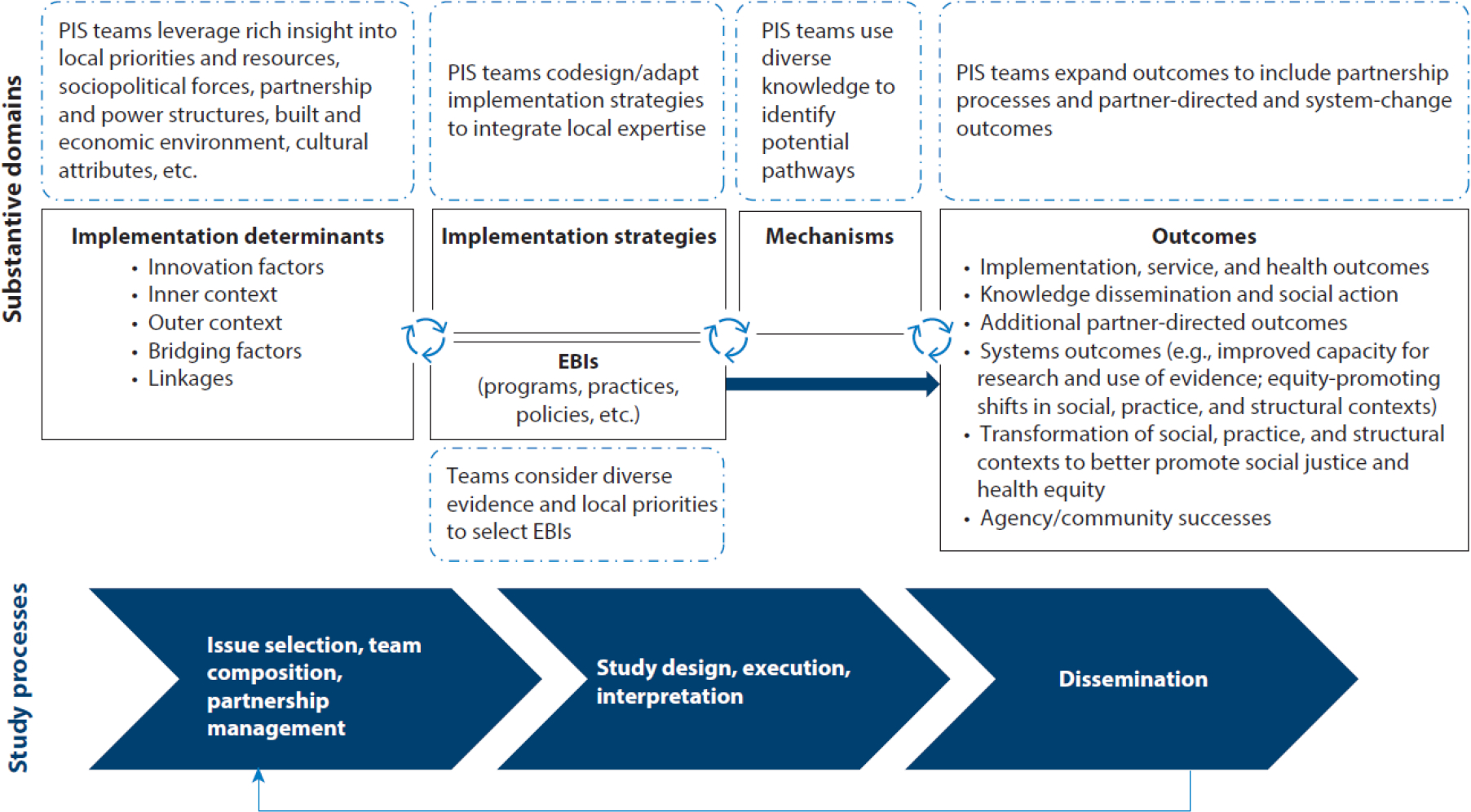
Integrating participatory approaches into IS efforts. “PIS teams” includes all actors involved in the IS project, e.g., researchers, practitioners, community members. Abbreviations: EBIs, evidence-based interventions; IS, implementation science; PIS, participatory implementation science. Figure adapted with permission from Reference 92.
3.1. Integrating Participatory Approaches into Study Design
The integration of participatory approaches into study activities can be accomplished in several ways. Here, we offer examples of such integration related to the selection of the focal issue, composition of study teams, and management of research partnerships. We also describe the ways in which participatory approaches can and should influence study design and execution, interpretation of results, and dissemination. As seen in Sidebar 1, it can be helpful to use a range of entry points to help teams consider and apply core principles of participatory IS.
Sidebar: Alternate entry points into thinking about participatory IS.
In addition to the literature and examples presented in this review, the authors offer a series of quotations that represent aspects of participatory IS that offer reminders of the importance of centering diverse expertise, ensuring the focus of the research and ways in which it is conducted meet all partners’ needs, and remaining vigilant against falling into extractive patterns.
Nothing about us without us (a phrase with roots in Eastern Europe and popularized in English by disability activists; now used as a rallying cry by many identity groups to promote democratic social transformation).
Every single person has their very singular concerns (Tamil colloquial saying).
A room can be what you inhabit, but it can also be an activity—to make room with each other, for each other. (Ahmed (2))
Yesterday I was clever, so I wanted to change the world. Today I am wise, so I am changing myself. (a quotation from Rumi)
Tell me only what I want/ came here to hear/ and then I will retell it / in such a way that it becomes my knowledge/ and benefits me (socially, professionally, economically./ And you?/ You will hardly recognize/ yourself— / especially in my ‘fully adjusted models.’/ Also, you’ll need $39.95 and an Internet connection (a quotation from Petteway (86))
3.1.1. Issue selection, team composition, and partnership management.
By agreeing on the health issue, scope, and value of the implementation effort and goals related to engagement, participatory IS teams can increase buy-in, commitment, and sustainment of implementation (50, 116). Yet, as Tuhiwai Smith (114) emphasizes, careful consideration of who is included or excluded in defining the problem and determining the worth and utility of the research is essential. For this reason and others, team composition is critical. Participatory IS teams include academic researchers, community members, practice partners, and other actors. The 7Ps Framework suggests that actors may include patients/service recipients, providers, purchasers, payers, policy makers, product developers, and principal investigators/researchers (25). Participatory IS can benefit from further creativity in the selection of partners. For example, a recent project examining the impact of small businesses on the health of a historically Black neighborhood was dramatically improved by adding a local historian and small business owner to the team, initially as an advisor and then as a partner. The study design and scope were reframed through this partnership, as were the business- and community-facing dissemination products (99).
As prompted by the double rainbow model (11, 69), strategic team composition moves beyond identities and roles to consider individuals’ networks, constituents, and socioecological levels at which they create change, e.g., policy. The visual representation (mirrored concentric layers of team members) emphasizes multilevel, equitable engagement. Structured processes to map relevant actors can help support strategic team composition (18). For example, to support tobacco control EBI implementation in hospitals, Bernstein and colleagues (12) mapped relevant actors and their support for or resistance to implementation, level of power in the system, and other factors to understand whom to engage and how. For practical and ethical reasons, participatory IS teams must consider which group members (e.g., more or less affluent members of a given community) can and do participate to avoid reproducing or perpetuating broader societal inequities. They must also avoid conflating group membership or credibility with representation of an entire community or group (36, 44).
Partnerships require careful management to navigate differences in perspective and positionality and differential access to resources, knowledge, agendas, needs, and time for and experience with research. As an example, one author (S.R.) participated in a project to deliver evidence-based telemedicine services in a rural, tribal village in Gujarat, India. Team members included village leadership; agricultural, sanitation, and energy companies; a local foundation; and academic institutions. The team used consensus around goals related to community development and sustainable delivery of telemedicine services to begin to bridge vast disconnects in team members’ personal and professional backgrounds and experience with research (21, 95). Considerations and resources for managing these opportunities and challenges are discussed further in Section 4.
3.1.2. Study design, execution, and interpretation.
Participatory approaches result in context-appropriate study design and instruments, improved recruitment and retention, and enhanced interpretation and dissemination (92, 126, 129, 130). The engagement of actors with a range of identities and roles also allows for research teams to examine power in the design and conduct of research. For example, Stanton, Ali, and colleagues’ (117) work with HIV-related mental health interventions attends to how implementation is impacted by different forms of power across all phases of implementation, how power influences the definition of health issues and framing of the implementation problem, power’s influence on the value placed on knowledge from diverse sources, and the impact of power on the distribution of benefits to various groups.
3.1.3. Dissemination.
Participatory research approaches include an obligation to share results with audiences who are affected by or who can affect the issue in accessible, action-oriented, credible, current, relevant, and understandable ways (115a, 133b). A ”designing for dissemination” process that engages crucial actors increases the likelihood that research products match the needs, resources, and requirements of the individuals and systems that will utilize them (15, 58). Participatory IS teams can identify and engage core dissemination audiences (e.g., service recipients, implementers, policy makers) early in the project. I team can then create a strategic communication plan addressing what to share with which audiences, how to frame the message, when to share information, and through which channels (115a, 133b).
3.2. Integrating Participatory Approaches into Theoretical IS Content
Participatory approaches can also be integrated into and enhance the theory of IS, as detailed below.
3.2.1. Implementation determinants and context.
Given the complexity of implementation contexts (80), a wide range of participatory IS team members is needed to identify and capture relevant factors. To give a sense of the magnitude of the task of capturing contextual factors, the well-known Exploration, Preparation, Implementation, and Sustainment framework highlights 16 domains of determinants (e.g., policy environment and organizational staffing patterns), each containing essential constructs (1). Participatory approaches allow IS teams to (a) prioritize determinants of interest, (b) leverage diverse resources to understand and respond to context, and (c) track relevant changes in context over time. Thus, participatory IS teams can leverage, but not be constrained by, existing IS theories, models, and frameworks. As an example, Waldron and colleagues engaged with Black and First Nations communities in Nova Scotia to examine the health impact of environmental racism (e.g., in the form of the placement of garbage dumps or effluent release). This collaboration emphasized the context of the communities’ histories with settler colonialism, including rich histories of resistance as a critical determinant for making sense of and responding to current environmental insults and informing all aspects of study design and solution generation. The project resulted in protections against ecological harm and new legislation to protect marginalized communities (30a, 128).
3.2.2. Implementation strategies and mechanisms.
For any project, several potential implementation strategies might be appropriate to increase EBI adoption, implementation, and sustainability (88). However, guidance on selecting and tailoring implementation strategies is limited, particularly concerning action at multiple levels of influence (e.g., implementation site, community, policy) (88). Diverse expertise within participatory IS teams can support the creation and selection of viable strategies while offering insight into potential mechanisms for change (63). For example, a network of African American churches involved in the Engaging Partners in Caring Communities initiative developed a menu of tailored implementation strategies to support EBI delivery through their institutions (133).
3.2.3. EBI selection and adaptation.
Participatory IS approaches attend to the collective framing and definition of problems and solutions, which significantly impact the selection and adaptation of EBIs. Existing evidence regarding EBIs reflects a limited range of populations, contexts, and issues. In addition, the evidence that “counts” is often limited to findings from academic-led trials and quantitative research (17, 70). These limitations contradict evidence-based public health goals of integrating the best available research evidence with community- and practice-based expertise and preferences (14, 27). Disputes about evidence underlying innovations can create tension among participatory IS teams, particularly when individuals value different sources or ways of generating evidence. The development of research evidence also often excludes groups that are most impacted, reducing the credibility and value of the work (101). Participatory IS teams must determine whether the evidence base meets community/practice needs. For example, rather than adapting Western interventions, Gone et al. (38) describe generating evidence for mental health interventions with Native American communities that align with the experience, worldviews, and theoretical orientations of community members and those who serve them.
When adaptation is appropriate, participatory action drives this work. Practical considerations raised by team members grounded in the implementation context help teams attend to Hawe and colleagues’ (46) prompts to focus on the innovation’s function rather than its form. For example, a participatory IS partnership including academic researchers and an advisory board used an intervention mapping approach (34) to adapt the StrongWomen–Healthy Hearts intervention to improve physical activity and nutrition for rural Latinas. They identified program elements, made changes to adjust for the context (e.g., cultural relevance), identified alterations to support implementation (e.g., modified staffing requirements), and planned for evaluation (e.g., health outcome measures and participant experience) (85). The adapted program achieved high-fidelity implementation and participant satisfaction and improved health outcomes (108).
3.2.4. Outcomes.
Participatory approaches offer an opportunity to extend target outcomes beyond those typically used in IS [for a comprehensive review, see 64). Commonly used implementation outcomes from Proctor and colleagues (89) emphasize acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration, and sustainability. These outcomes are linked with service and health outcomes and can be used as early signals to identify the differential impact of EBIs. For example, differential adoption between intended users might prompt the tailoring of implementation strategies to ensure equitable outcomes. With a focus on health equity, participatory research outcomes emphasize processes for and impacts of community engagement, dissemination, social action, capacity building, and systems changes (65, 83, 132). As seen in Figure 1, participatory IS prompts attention not only to the typical IS outcomes but also to those related to sharing knowledge, evaluating partnerships, impacting contexts of EBI delivery, building individual and collective power and agency, addressing partners’ goals, and promoting systems outcomes.
As an example of systems change outcomes, Restar and colleagues (101) are developing community-engaged and gender-affirming infrastructure for HIV pre-exposure prophylaxis systems to increase service delivery for transgender people. Outcomes relate to (a) infrastructure, e.g., participation in leadership and governance; (b) economy, e.g., investments in addressing root causes of inequities; and (c) policy, e.g., restricting the potential harm of service-tracking systems (101). Attention to systems change also includes assessing power distributions and how they can be shifted to create equity- and health-promoting contexts (33, 83). Table 1 highlights exemplar outcomes that integrate IS and participatory research outcomes.
Table 1.
Exemplar outcomes for participatory implementation science efforts (45, 65, 83, 98, 114, 121, 132, 135)
| Outcomes | Exemplar outcomes |
|---|---|
| Implementation and health | • Equity-focused implementation, service, and health outcomes for priority issue • Social action to address priority issue • Improved community health and wellbeing • Dissemination of relevant, actionable knowledge and implementation supports |
| Partnership-supporting processes and environment | • Development and sustainment of non-hierarchical partnerships • Improved participatory research context (e.g., social networks) and processes (e.g., appropriate compensation for Participatory IS team members and participants) • Transformation of researchers through use of participatory processes • Research-focused successes (e.g., changes in institutional policies to support participatory research) |
| Capacity-building and systems change to improve health and health equity | • Increased capacity for research, implementation science, and action among all team members • Agency and community successes (e.g., community renewal) • Increased use of evidence to effect change related to current and future health challenges • Transformation of social, practice, and structural contexts to better promote social justice and health equity • Positive shifts in distribution of power and social capital • Procurement of funding to advance community and practice goals |
| Partner-directed outcomes | • Determined by partners |
3.3. Determining Engagement Levels for IS Studies
Scholars of participatory research highlight the range of forms that this work may take, emphasizing a continuum of engagement that meets partners’ preferences and the needs of the research team and study (75). The central axis typically concerns the depth of involvement and the extent to which power and decision-making authority sit with academics versus other team members. Conventional research is often described as contractual and for IS might include sole reliance on agreements for implementation sites to share data and permit research activities. Figure 2 illustrates higher levels of engagement in participatory IS.
Figure 2.
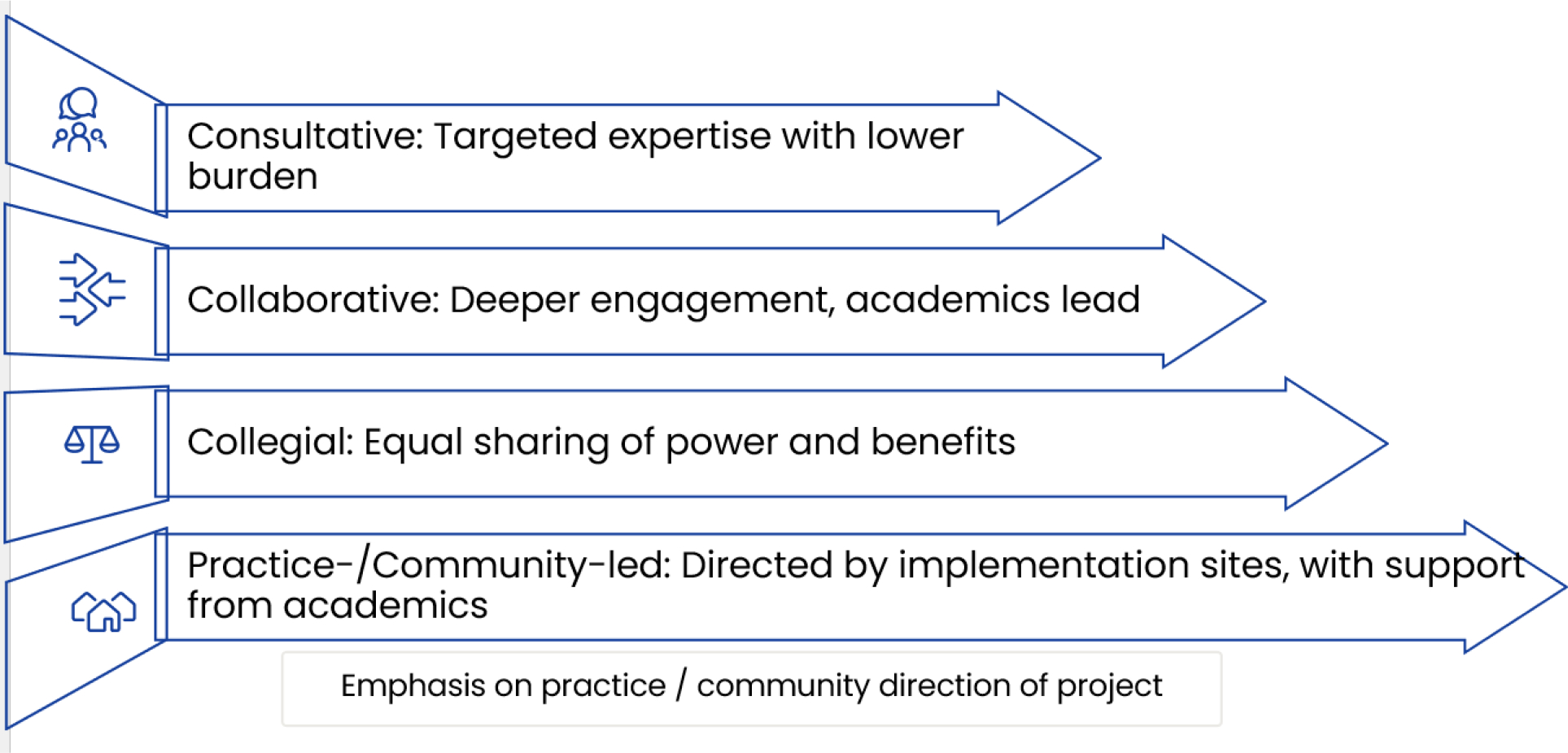
Engagement levels for participatory IS projects, including consultative, collaborative, collegial, and practice-/community-led levels. Figure adapted with permission from Reference 92.
Taking a dynamic view of engagement is essential, and participatory IS projects may engage core and ancillary team members at different levels and for varied purposes across the life of a project. Alternatively, the same set of individuals or organizations may make different levels of commitment to various projects. Helpful considerations for identifying an appropriate level of engagement include (a) project timeline and team members’/institutions’ commitment to and constraints related to project processes and outcomes, (b) team members’ capacity to engage in project processes and activities, (c) commitment among researchers to participatory approaches, and (d) existing levels of trust between academics and other team members (40). Working toward transformational change (i.e., reshaping harmful systems) typically necessitates collegial or community-/practice-led engagement levels.
3.3.1. Consultative approaches.
With consultative levels of engagement, practice/community partners are consulted infrequently for specific purposes and with minimal burden on partners (e.g., to refine the scope of the research questions or advise on dissemination audiences). This level of engagement supports accessing high-level expertise and partner networks with a limited investment of time and resources for all parties. Reviews of research projects by community members are a commonly used model for this approach (for examples, see 32, 52). With less frequent or extensive interactions, the benefits of collaborating with a diversity of partners will necessarily be circumscribed. Participatory IS teams must be proactive to ensure that the partnership is not tokenistic or performative.
As an example of a consultative approach, Project Resist addresses tobacco control among young adult sexual minority women in the United States and engages four national leaders in LGBTQ+ health as advisory committee members, meeting every 3–6 months. As part of a qualitative study to generate innovative dissemination products, the committee offered deep insight into the practice context, resources, and constraints of LGBTQ+-serving organizations, revised the interview guide to increase relevance and inclusivity, and supported recruitment. During data analysis, the committee provided critical context regarding current political and funding climates, connected the work to harm reduction and trauma-informed care, and placed the work in the historical context of these organizations. To disseminate findings, committee members and academic researchers coauthored practitioner-focused briefs and a scientific journal article (97). The process was invaluable for ensuring that solutions reflected the context of the organizations of interest and were helpful to leaders seeking to create national change.
3.3.2. Collaborative and collegial approaches.
Although they are not equivalent, collaborative and collegial approaches share many similarities, although collaborative approaches require less investment from all parties and support less sharing of power and resources. Collegial approaches are similar to CBPR approaches and emphasize ongoing, nonhierarchical partnerships between academic researchers and team members to address issues and outcomes of community importance (74). These approaches combine knowledge and action in the service of promoting social change and improving health/addressing health inequities. Collaborative and collegial engagement levels are appropriate when team members are willing to invest in long-term relationships emphasizing power sharing and sustained action. Challenges of these engagement levels include the intense investments required by all team members and readiness to engage at this level. To support successful partnership, explicit attention is paid to identity-based discrimination, challenges working across cultures and contexts, and the centering of diverse forms of expertise (49, 50, 72, 131, 136).
As one example of this approach, PLANET MassCONECT is a collegial project that aims to build capacity for EBI use among the staff of community-based organizations addressing health inequities. The gap in capacity (which was affecting organizations’ ability to secure grants) was identified by three leaders of health-focused coalitions from communities that were experiencing cancer inequities and had rich histories of social justice organizing. The partnership started in 2008, led by Viswanath, Koh, and others (56). Core to the partnership execution was a focus on building and sharing human, social, and financial capital through sustained investments (98). As partner communities’ needs, resources, and priorities evolved, so too did the project’s focus, e.g., to include policy change and adolescent health. Decision-making power and resources are shared among team members (although the constraints imposed by research institutions impact these processes), and investments are made in building infrastructure in partner communities to sustain evidence-based program planning. Local action includes delivery of cocreated workshops and technical assistance, a Web-based portal for practitioners, dissemination of findings to scientific and practice audiences, activation of practitioner social networks, internships supporting underrepresented minority students to conduct community-engaged research, and community-focused knowledge translation activities, e.g., science cafés (92, 94, 96, 98).
3.3.3. Practice-/community-led.
With this level of engagement, practice or community partners direct the research effort. This approach centers on action and co-ownership of IS research processes by inside experts (e.g., implementers, decision makers, and others), with outside experts (e.g., academic researchers) offering support as requested (55). More expansive than program evaluation, these efforts seek to contribute knowledge to a broader evidence base for use by other actors. However, as highlighted by Brownson and colleagues (17), evidence generated in ways that emphasize internal validity and tacit knowledge is often undervalued in academic research settings.
As one example of this approach, one of the authors (V.S.) was involved with Messengers for Health, which evolved into a practice-led project over time (24, 47, 112). The project started as a CBPR effort to prevent cervical cancer on the Crow Reservation. A series of grants (held by the university partner, with community partners employed by the university as project staff) addressed cervical cancer and other community priorities among members of this Native nation. As the partnership matured, the team considered methods to promote sustainability. The partnership created a 501(c)(3) nonprofit organization in 2010, allowing the community to take formal ownership of the program, access a broader range of funding opportunities, and alleviate some barriers associated with grants flowing through universities.
4. CHALLENGES AND CONSIDERATIONS TO OPTIMIZE PARTICIPATORY IS
Participatory approaches require time and resources to create transformational change through implementation efforts. Poorly executed participatory efforts risk failing to improve health outcomes and perpetuating inequities, as well as longer-term damage to trust and to the potential for future collaboration (6, 48, 125). Even within successful participatory IS projects, the benefits of a project and the emotional, economic, or political costs of participation may be unevenly distributed within the team (126). In this section, we summarize selected challenges and considerations for optimizing participatory approaches to IS.
4.1. Managing Participatory Processes and Contextual Constraints
Evaluations of participatory approaches find that effective participation processes increase the likelihood that broader desired outcomes will be achieved (51, 103). Given that participatory approaches are not yet the norm in IS, it can be helpful to assess team members’ readiness for such work (109, 132). Teams can also engage in critical reflexivity, the methodological practice of considering how one’s experiences, roles, and position impact the research and knowledge production processes (120). This practice attends to positionality, or dynamic social location compared with others, for example, reflecting relative social status or privilege (77). Through such practices, participatory IS teams can examine their project with regard to power, rights, responsibilities, and relationships/social networks (30). For instance, the authors of this review are all fundamentally concerned with social justice but approach this aim from different disciplinary and professional backgrounds, ranging from academic research to pastoral care and research review as a community member. We also enter public health spaces with intersecting identities that span a range of privileged to marginalized positions. We bring unique perspectives based on various social identities (e.g., Asian American, Black, child of immigrants, first-generation scholar, Hispanic, man, Native American, queer, rural resident, urban resident, and woman). Ongoing examination of positionality during participatory IS projects allows us to recognize how the viewpoints from which we approach the work may shape or limit our assumptions and understandings, perspectives we may be missing, how we are read by those with whom we interact, and dynamics of privilege or marginalization to be mitigated within the team (115).
Failure to ensure equitable opportunities for involvement in participatory IS (including within marginalized groups), to manage power asymmetries, and to facilitate shared decision making, coconstruction, and joint action risks undermining the value of a participatory approach to IS (48). Those whose interests and perspectives have been silenced and marginalized, and/or who stand to gain most from a more participatory approach, may equally be those who face most barriers to meaningful participation in IS, especially in contexts of poverty, prejudice, and inequality (126). Participatory IS teams must proactively institute structures and processes to facilitate transparent and equitable negotiation of differential access to resources, knowledge, time for and experience with research, and differing agendas or needs (51, 60, 73). These include early engagement of all team members, microlevel processes supporting effective communication and attention to task-oriented differences, recognition of the diverse contributions of different actors, and power-sharing governance (48, 125). Structured trainings can build capacity for research participation among community members and practice audiences (39, 84) to increase their impact on the project, their ability to collaborate with other actors in the system, and the power to instigate change (66). Equally as important, if not more significant, is the need to ensure that researchers have appropriate training and capacity to engage in participatory approaches to IS and to create enabling structures within research institutions and funding agencies (109).
One of the authors of this article (R.A.) serves as a community reviewer of research and offers several ways in which academic researchers can move from good intentions to concrete action with regard to participatory IS approaches: (a) invest time in learning about the communities and institutions meant to benefit from the work, (b) commit to build trust over the long term, (c) create inclusive work environments where diverse knowledge is respected and a sense of belonging in knowledge production is cultivated, and (d) move beyond acknowledging power imbalances toward concrete actions to level these imbalances wherever team members have influence (32). Rich resources that offer further guidance on developing, maintaining, and evolving productive participatory processes are available elsewhere (26, 48, 51, 100, 106).
The broader incentives and pressures that team members face can also create challenges for optimizing participatory IS. Hallmarks of participatory approaches are building trust and engaging authentically (often through attending events in community and practice settings), contributing to community priorities, demonstrating values through action, and being accountable for actions in community or practice settings (3, 19, 98). Yet many teams using participatory processes struggle to find institutional or funding structures that allow them to engage in this way (4, 8, 48). A related challenge is insufficient recognition of the value of participatory and impact-focused work in many academic researchers’ tenure and promotion processes (134).
4.2. Navigating Tensions Between World Views
Participatory IS team members’ divergent worldviews (e.g., about the nature of reality and how we come to know about it), cultural norms, and assumptions can facilitate productive friction), but also lead to tension and misunderstanding (48). For example, critical and transformative orientations of participatory research efforts may conflict with values often espoused in public health and medical research environments related to technical expertise, objectivity, and uncovering universal truths (50, 73). Or the challenge may come from the imposition of external standards and definitions of implementation success, which conflict with the view that action, reflection, and revision are the way to achieve long-term progress and that the nature of this progress may not be predictable at the start (37, 59). To find a path forward, participatory IS teams may find alignment in relevance, utility in practice, and contributions toward desired social change (20).
Conflicting paradigmatic stances may also create concerns about the generalizability of learning from a given project. While products of participatory IS research are expected to have greater relevance and impact than products developed without engagement, there is often a concern that these highly customized products are too context specific to be useful in other settings and contexts (42, 129). However, these concerns must be balanced with the limitations of evidence derived from settings that are artificially constructed to increase internal validity (92). Drawing on the concept of transferability from qualitative research, rich detail about context and study processes (including engagement) allows others to determine whether or how they can apply the findings to their work (67).
4.3. Defining the Scope of the Project
IS projects often focus narrowly on the integration of an EBI into a system, but this approach often conflicts with the way practitioners and other relevant parties in the implementation context view their work or the scope of what is relevant to the focus of the intervention. Our recent concept mapping work regarding the conceptualization of core skills needed community-based organizations when using EBIs offers a useful example of this contrast. Academic researchers emphasized the skills required to advance an EBI through a system to achieve specified health outcomes. Practitioners focused on skills that would support EBI implementation and address health promotion for community members and community transformation (90, 91). Viewing the EBI and implementation strategies as events in a system allows participatory IS teams to better align their focus with practitioners’ and other decision-makers’ views (46, 53). Another cost of focusing narrowly on an EBI relates to “marketing myopia,” which could translate to an overemphasis on the EBI of interest and related ways to improve implementation instead of focusing on the goal that the innovation addresses (61).
The question of scope also relates to the commitment to social change, as transforming practice and community settings requires a broader scope or scale than the typical IS project (126). However, participatory IS teams can focus on short-term service delivery and more comprehensive infrastructure development. For example, Carter-Edwards (22) and colleagues mobilized a community-centered response to develop strategies for promoting rapid, remote risk communication strategies for COVID-19 through the power of social connections within rural, Black faith communities in the Eastern North Carolina region. Built on a partnership base that started in 2014 and was formalized in 2018, the Faith-Based Organizational Network is a regional network of Black ministries functioning as cross-county infrastructure for connecting health efforts to communities through local churches. In 2020, they received a community-engaged risk communication grant related to COVID-19. They engaged congregants to adapt World Health Organization pandemic guidelines by deploying systems mapping, applying a human-centered design guided by the RE-AIM framework, and utilizing high-tech and high-touch remote data collection strategies. In addition to addressing COVID-related concerns, the work has resulted in an increased capacity of rural communities to respond to public health emergencies and influence strategies at the community and health systems levels that improve health while establishing a voice to guide the creation of programs and policies that communities want and will use. The example eof the Faith-Based Organizational Network highlights the potential for participatory IS efforts to impact important implementation and service delivery outcomes while building infrastructure, capacity, and strategies that can be leveraged for rapid public health responses needed in the future.
4.4. Developing Measures to Advance the Evidence Base for Participatory IS
More research is needed to understand the impact of participatory approaches on the quality of research, EBI implementation and sustainment practices, health outcomes, multilevel impacts, and long-term change (65, 83). A customizable set of outcomes, such as those outlined in Table 1, allows the identification of effects significant to a wide range of actors in the implementation context and opportunities to balance the needs of a specific EBI and the goals of long-term systems change. In the same way that implementation outcomes can signal potential impact on health and inequities (89), participatory IS short-term outcomes may signal progress toward social action and systems change. Dynamic models are needed to explore the costs and benefits of different levels of engagement for different groups and how these relate to context, evolution of relationships, and participatory processes over time (7). Finally, given the challenges of ensuring the high-quality participatory processes described above, developing and including measures of process (as well as outcomes) can inform ongoing participatory efforts in real time, promote accountability, and guard against tokenism or instrumental cooptation of participatory approaches (29, 33, 122)
5. CONCLUSION
This review draws on principles, practices, and lessons from participatory research and community-based work from several fields to offer a framework for applying these approaches to IS. Broadly, participatory IS an inclusive, collaborative, and iterative approach to promoting, implementing, and sustaining EBIs to advance health equity. Unlike linear, top-down transfer models of knowledge production, participatory IS utilizes the coproduction of knowledge and practice through mobilization and synthesis of diverse expertise in a relational, nonlinear, and emergent process. Participatory IS has foundational foci on including marginalized voices to shape knowledge and action and supporting systems transformation.
Participatory IS entails a dynamic process of selecting and combining approaches to create and maintain the best fit for a given project over time. Who, how, and at what level different team members are engaged must fit with the context, availability of time and resources, capacity of team members, and project goals. Optimizing fit can also improve the theory and methods of IS, e.g., expanding study teams’ understanding of complex, dynamic implementation contexts and identifying innovative ways to study them. At the same time, doing participatory IS well, and avoiding damaging tokenistic participation, requires intense investment. It demands of researchers (and their institutions) a deep commitment to developing skills, taking critical perspectives, building structures for accountability, and creating synergy with other changemakers. Ultimately, participatory IS offers the opportunity for a paradigm shift, moving beyond a focus on making specific EBIs work within harmful systems to initiating action to reshape these systems to center equity. It is up to all of us to take up this challenge.
SUMMARY POINTS.
Participatory implementation science (participatory IS) is an iterative, collaborative approach to research that engages academic researchers, community members, implementers, and other vital actors to integrate practice-, community-, and research-based evidence into public health and health care services. These efforts aim to improve health, reduce health inequities, and create transformational change.
Unlike linear, top-down transfer models of knowledge production, participatory IS utilizes coproduction of knowledge and practice through mobilization and synthesis of diverse expertise in a relational, nonlinear, and emergent process. It also emphasizes a commitment to investing deeply in the approach, including sharing resources and power, as the process can otherwise be tokenistic and harmful.
Participatory IS moves beyond attempts to make evidence-based interventions (EBIs) “work,” even within harmful systems, expanding the focus of implementation efforts to reshape systems and intervention contexts in ways that center equity.
Participatory approaches can be integrated into IS study processes, ranging from study design to dissemination, and offer the opportunity to increase the relevance, utility, and impact of EBIs and implementation efforts.
In addition to its focus on implementation, service, and health outcomes, participatory IS efforts must attend to outcomes related to partnership processes/environment, capacity building and systems change, and customized outcomes reflecting diverse team members’ goals.
A continuum of levels of engagement offers teams the opportunity to strategically select consultative, collaborative, collegial, or community-/practice-led approaches as a function of context, availability of time and resources, capacity of team members, and project/broader goals.
Key challenges and considerations to advance participatory IS include managing tensions between participatory processes and contextual constraints, navigating disconnects between team members’ world views, identifying ways to expand the scope of participatory IS projects, and developing measures to advance the evidence base for participatory IS.
ACKNOWLEDGMENTS
This study was funded by the National Cancer Institute (U54CA156732 for S.R.; 5T32CA057711 for J.C.).
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review. The article’s content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
LITERATURE CITED
- 1.Aarons GA, Hurlburt M, Horwitz SM. 2011. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm. Policy Ment. Health 38(1):4–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed S 2018. Notes on feminist survival. feministkilljoys. https://feministkilljoys.com [Google Scholar]
- 3.Alang S, Batts H, Letcher A. 2021. Interrogating academic hegemony in community-based participatory research to address health inequities. J. Health Serv. Res. Policy 26(3):215–20 [DOI] [PubMed] [Google Scholar]
- 4.Alidina S, Martelli PF, Singer SJ, Aveling E-L. 2021. Optimizing patient partnership in primary care improvement: a qualitative study. Health Care Manag. Rev. 46(2):123–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alonso C, Keppard B, Bates S, Cortez D, Amaya F, Dinakar K. 2023. The Chelsea Project: turning research and wastewater surveillance on COVID-19 into health equity action, Massachusetts, 2020–2021. Am. J. Public Health 113:627–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aveling E-L, Jovchelovitch S 2014. Partnerships as knowledge encounters: a psychosocial theory of partnerships for health and community development. J. Health Psychol. 19(1):34–45 [DOI] [PubMed] [Google Scholar]
- 7.Aveling E-L, Roberts JE, Taylor LA, Bhuiya N, Singer SJ. 2023. Business-nonprofit hybrid organizing: a dynamic approach to balancing benefits and costs. Front. Health Serv. 3:1164072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aveling E-L, Zegeye DT, Silverman M. 2016. Obstacles to implementation of an intervention to improve surgical services in an Ethiopian hospital: a qualitative study of an international health partnership project. BMC Health Serv. Res. 16(1):393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Axon S 2020. The socio-cultural dimensions of community-based sustainability: implications for transformational change. J. Cleaner Prod. 266:121933 [Google Scholar]
- 10.Bauer MS, Kirchner J. 2020. Implementation science: What is it and why should I care? Psychiatry Res. 283:112376. [DOI] [PubMed] [Google Scholar]
- 11.Behringer BA, McLean JE. 2022. Identifying key partners and stakeholders in community-engaged scholarship projects. J. Higher Educ. Outreach Engagem. 26(1):197 [Google Scholar]
- 12.Bernstein SL, Weiss J, Curry L. 2020. Visualizing implementation: contextual and organizational support mapping of stakeholders (COSMOS). Implement. Sci. Commun. 1(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braveman P, Arkin E, Orleans T, Proctor D, Acker J, Plough A. 2018. What is health equity? Behav. Sci. Policy 4(1):1–14 [Google Scholar]
- 14.Brownson RC, Baker EA, Leet TL, Gillespie KN, True WR. 2011. Evidence-Based Public Health. New York: Oxford Univ. Press [Google Scholar]; 14a. Brownson RC, Colditz GA, Proctor EK, eds. 2018. Dissemination and Implementation Research in Health: Translating Science to Practice. New York: Oxford Univ. Press [Google Scholar]
- 15.Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. 2013. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am. J. Public Health 103(9):1693–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brownson RC, Kumanyika SK, Kreuter MW, Haire-Joshu D. 2021. Implementation science should give higher priority to health equity. Implement. Sci. 16(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brownson RC, Shelton RC, Geng EH, Glasgow RE. 2022. Revisiting concepts of evidence in implementation science. Implement. Sci. 17(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brugha R, Varvasovszky Z. 2000. Stakeholder analysis: a review. Health Policy Plan. 15(3):239–46 [DOI] [PubMed] [Google Scholar]
- 19.Brush BL, Mentz G, Jensen M, Jacobs B, Saylor KM, et al. 2020. Success in long-standing community-based participatory research (CBPR) partnerships: a scoping literature review. Health Educ Behav. 47(4):556–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brydon-Miller M, Greenwood D, Maguire P. 2003. Why action research? Action Res. 1(1):9–28 [Google Scholar]
- 21.Camillus JC, Ramanadhan S, Ganapathy K. 2001. Strategy in the time of pandemics, climate change, and the Kurzweil singularity. J. Strateg. Manag. 14(3):300–14 [Google Scholar]
- 22.Carter-Edwards L 2020. Using community engagement to adapt implementation science methods in a faith setting. Presented at Consortium for Implementation Science Forum: Harnessing Implementation Science to Promote Health Equity, online, Nov. 19. https://consortiumforis.org/wp-content/uploads/2020/12/Carter-Edwards_Using-Community-Engagement-to-Adapt-IS-Methods-in-a-Faith-Setting.pdf [Google Scholar]
- 23.Caxaj CS. 2015. Indigenous storytelling and participatory action research: allies toward decolonization? Reflections from the Peoples’ International Health Tribunal. Glob. Qual. Nurs. Res. 20:2333393615580764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Christopher S, Gidley AL, Letiecq B, Smith A, McCormick AKHG. 2008. A cervical cancer community-based participatory research project in a Native American community. Health Educ. Behav. 35(6):821–34 [DOI] [PubMed] [Google Scholar]
- 25.Concannon TW, Meissner P, Grunbaum JA, McElwee N, Guise J-M, et al. 2012. A new taxonomy for stakeholder engagement in patient-centered outcomes research. J. Gen. Intern. Med. 27(8):985–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corbie-Smith G, Wynn M, Richmond A, Rennie S, Green M, et al. 2018. Stakeholder-driven, consensus development methods to design an ethical framework and guidelines for engaged research. PLOS ONE 13(6):e0199451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cornish F 2015. Evidence synthesis in international development: a critique of systematic reviews and a pragmatist alternative. Anthropol. Med. 22(3):263–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cornish F, Breton N, Moreno-Tabarez U, Delgado J, Rua M, et al. 2023. Participatory action research. Nat. Rev. Methods Primers 3(1):34 [Google Scholar]
- 29.Cornish F, Priego-Hernandez J, Campbell C, Mburu G, McLean S. 2014. The impact of community mobilisation on HIV prevention in middle and low income countries: a systematic review and critique. AIDS Behav. 18:2110–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crosschild C, Huynh N, De Sousa I, Bawafaa E, Brown H. 2021. Where is critical analysis of power and positionality in knowledge translation? Health Res. Policy Syst. 19(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]; 30a. Daniel I, Page E. 2019. There’s something in the water. Doc. Film, 73 min., 2 Weeks Notice, Woodland Hills, CA [Google Scholar]
- 31.Deloria V Jr. 1991. Research, redskins, and reality. Am. Indian Q. 15(4):457–68 [Google Scholar]
- 32.Emmons K, Curry M, Lee RM, Pless A, Ramanadhan S, Trujillo C. 2022. Enabling community input to improve equity in and access to translational research: The Community Coalition for Equity in Research. J. Clin. Transl. Sci. 6(1):e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fals-Borda O, Rahman MA. 1991. Action and Knowledge: Breaking the Monopoly with Participatory Action Research. New York: Apex Press [Google Scholar]
- 34.Fernandez ME, Ruiter RAC, Markham CM, Kok G. 2019. Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front. Public Health. 7:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Freire P 1978. From Pedagogy of the Oppressed. In Studies in Socialist Pedagogy, ed. Norton E, Ollman B, pp. 60–78. New York: Mon. Rev. Press [Google Scholar]
- 36.George S, Duran N, Norris K. 2014. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am. J. Public Health 104(2):e16–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gillespie J, Albert J, Grant S, MacKeigan T. 2020. Missing in action: Indigenous knowledge systems in evaluation of comprehensive community initiatives. Can. J. Program Eval. 35(2):170–87 [Google Scholar]
- 38.Gone JP, Tuomi A, Fox N. 2020. The urban American Indian traditional spirituality program: promoting Indigenous spiritual practices for health equity. Am. J. Community Psychol. 66(3–4):279–89 [DOI] [PubMed] [Google Scholar]
- 39.Goodman MS, Dias JJ, Stafford JD. 2010. Increasing research literacy in minority communities: CARES fellows training program. J. Empir. Res. Hum. Res. Ethics 5(4):33–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goodman MS, Sanders Thompson VL. 2017. The science of stakeholder engagement in research: classification, implementation, and evaluation. Transl. Behav. Med. 7(3):486–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goodman MS, Thompson VLS, Arroyo Johnson C, Gennarelli R, Drake BF, et al. 2017. Evaluating community engagement in research: quantitative measure development. J. Commun. Psychol. 45(1):17–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Green LW, Glasgow RE. 2006. Evaluating the relevance, generalization, and applicability of research: issues in external validation and translation methodology. Eval. Health Prof. 29:126–53 [DOI] [PubMed] [Google Scholar]
- 43.Greenhalgh T, Jackson C, Shaw S, Janamian T. 2016. Achieving research impact through cocreation in community-based health services: literature review and case study. Milbank Q. 94(2):392–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hahn DL, Hoffmann AE, Felzien M, LeMaster JW, Xu J, Fagnan LJ. 2017. Tokenism in patient engagement. Fam. Pract. 34(3):290–95 [DOI] [PubMed] [Google Scholar]
- 45.Hawe P, Noort M, King L, Jordens C. 1997. Multiplying health gains: the critical role of capacity-building within health promotion programs. Health Policy 39(1):29–42 [DOI] [PubMed] [Google Scholar]
- 46.Hawe P, Shiell A, Riley T. 2009. Theorising interventions as events in systems. Am. J. Community Psychol. 43(3–4):267–76 [DOI] [PubMed] [Google Scholar]
- 47.Held S, McCormick AKHG, Simonds V, Braun KL, Burhansstipanov L, et al. 2022. Using community-based participatory research to address Indigenous health. In Indigenous Public Health: Improvement through Community-Engaged Interventions, ed. Burhansstipanov L, Braun KL, pp. 80–102. Lexington: Univ. Press Ky. [Google Scholar]
- 48.Holt DH, Aveling E-L. 2023. Achieving partnership synergy: resource inputs, shared mission and interdependencies in Danish health promotion partnerships. Health Promot. Int. 38(1):daac203. [DOI] [PubMed] [Google Scholar]
- 49.Israel BA, Eng E, Schulz AJ, Parker EA, eds. 2012. Methods for Community-Based Participatory Research for Health. San Francisco: Wiley. 2nd ed. [Google Scholar]
- 50.Israel BA, Schulz AJ, Parker EA, Becker AB. 1998. Review of community-based research: assessing partnership approaches to improve public health. Annu. Rev. Public Health 19:173–201 [DOI] [PubMed] [Google Scholar]
- 51.Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, et al. 2012. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q. 90(2):311–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Joosten YA, Israel TL, Williams NA, Boone LR, Schlundt DG, et al. 2015. Community engagement studios: a structured approach to obtaining meaningful input from stakeholders to inform research. Acad. Med. 90(12):1646–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kenzie ES. 2021. Get your model out there: advancing methods for developing and using causal-loop diagrams. PhD Thesis 5664, Portland State Univ., Portland, OR. 10.15760/etd.7536 [DOI] [Google Scholar]
- 54.Kerner J, Gruiguis-Blake J, Hennessy KD, Brounstein PJ, Vinson C, et al. 2005. Translating research into improved outcomes in comprehensive cancer control. Cancer Causes Control 16(Suppl. 1):27–40 [DOI] [PubMed] [Google Scholar]
- 55.Key KD, Furr-Holden D, Lewis EY, Cunningham R, Zimmerman MA, et al. 2019. The continuum of community engagement in research: a roadmap for understanding and assessing progress. Prog. Commun. Health Partnersh. 13(4):427–34 [DOI] [PubMed] [Google Scholar]
- 56.Koh HK, Oppenheimer SC, Massin-Short SB, Emmons KM, Geller AC, Viswanath K. 2010. Translating research evidence into practice to reduce health disparities: a social determinants approach. Am. J. Public Health 100(Suppl. 1):S72–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kothari A, Wathen CN. 2017. Integrated knowledge translation: digging deeper, moving forward. J. Epidemiol. Commun. Health. 71(6):619–23 [DOI] [PubMed] [Google Scholar]
- 58.Kwan BM, Brownson RC, Glasgow RE, Morrato EH, Luke DA. 2022. Designing for dissemination and sustainability to promote equitable impacts on health. Annu. Rev. Public Health 43:331–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.LaFrance J, Nichols R. 2010. Reframing evaluation: defining an Indigenous evaluation framework. Can. J. Program Eval. 23(2):13–31 [Google Scholar]
- 60.Leach DK. 2013. Prefigurative politics. The Wiley-Blackwell Encyclopedia of Social and Political Movements, ed. Snow DA, della Porta D, Klandermans B, McAdam D, pp. 1004–6. Hoboken, NJ: Wiley-Blackwell [Google Scholar]
- 61.Levitt T 2004. Marketing myopia. Harv. Bus. Rev. 82(7/8):138–49 [PubMed] [Google Scholar]
- 62.Lewin K 1946. Action research and minority problems. J. Soc. Issues 2(4):34–46 [Google Scholar]
- 63.Lewis CC, Klasnja P, Powell BJ, Lyon AR, Tuzzio L, et al. 2018. From classification to causality: advancing understanding of mechanisms of change in implementation science. Front. Public Health. 6:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lewis CC, Mettert K, Proctor EK, Brownson RC. 2023. Measurement issues in dissemination and implementation research.s. In Dissemination and Implementation Research in Health: Translating Science to Practice, ed Brownson RC, Colditz GA, Proctor EK, pp. 327–44. New York: Oxford University Press [Google Scholar]
- 65.Luger TM, Hamilton AB, True G. 2020. Measuring community-engaged research contexts, processes, and outcomes: a mapping review. Milbank Q. 98(2):493–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mabetha D, Ojewola T, van der Merwe M, Mabika R, Goosen G, et al. 2023. Realising radical potential: building community power in primary health care through participatory action research. Int. J. Equity Health 22(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Maxwell JA. 2021. Why qualitative methods are necessary for generalization. Qual. Psychol. 8(1):111–18 [Google Scholar]
- 68.McCloskey DJ, McDonald A, Cook J, Heurtin-Roberts S, Updegrove S, et al. 2023. Community engagement: definitions and organizing concepts from the literature. In Principles of Community Engagement, pp. 1–42. Atlanta: Cent. Dis. Control Prev. 2nd ed. [Google Scholar]
- 69.McLean JE, Behringer BA. 2008. Establishing and evaluating equitable partnerships. J. Community Engag. Scholarsh. 1(1):66–71 [Google Scholar]
- 70.McNulty M, Smith JD, Villamar J, Burnett-Zeigler I, Vermeer W, et al. 2019. Implementation research methodologies for achieving scientific equity and health equity. Ethn. Dis. 29:83–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Medina J 2012. The Epistemology of Resistance: Gender and Racial Oppression, Epistemic Injustice, and Resistant Imaginations. Oxford, UK: Oxford Univ. Press [Google Scholar]
- 72.Minkler M 2014. Enhancing data quality, relevance and use through community-based participatory research. In What Counts: Harnessing Data for America’s Communities, ed Cytron N, Petit KLS, Kingsley GT, pp. 244–59. San Francisco/Washington, DC: Fed. Reserve Bank of San Francisco/Urban Inst. [Google Scholar]
- 73.Minkler M, Baden AC. 2008. Impacts of CBPR on academic researchers, research quality and methodology, and power relations. See Ref. 75, pp. 243–58 [Google Scholar]
- 74.Minkler M, Salvatore AL, Chang C. 2018. Participatory approaches for study design and analysis in dissemination and implementation research. See Ref. 14a, pp. 175–90
- 75.Minkler M, Wallerstein N, eds. 2008. Community-Based Participatory Research in Health: From Process to Outcomes. San Francisco: Jossey-Bass. 2nd ed. [Google Scholar]
- 76.Minkler M, Wallerstein N. 2008. Introduction to Community-Based Participatory Research. See Ref. 75, pp. 5–24
- 77.Misawa M 2010. Queer race pedagogy for educators in higher education: dealing with power dynamics and positionality of LGBTQ students of color. Int. J. Crit. Pedagog. 3(1):26–35 [Google Scholar]
- 78.Natl. Res. Counc., Div. Behav. Soc. Sci. Educ., Board Behav., Cogn., Sens. Sci., Comm. Sci. Team Sci. 2015. Enhancing the Effectiveness of Team Science, ed. Cooke NJ, Hilton ML. Washington, DC: Natl. Acad. Press [Google Scholar]
- 79.Nicolaidis C, Raymaker D. 2015. Community-based participatory research with communities defined by race, ethnicity, and disability: translating theory to practice. In The SAGE Handbook of Action Research, ed. Bradbury H, pp. 167–78. London: SAGE [Google Scholar]
- 80.Nilsen P 2015. Making sense of implementation theories, models and frameworks. Implement. Sci. 10(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nutbeam D 1996. Achieving ‘best practice’ in health promotion: improving the fit between research and practice. Health Educ. Res. 11(3):317–26 [DOI] [PubMed] [Google Scholar]
- 82.Oetzel JG, Wallerstein N, Duran B, Sanchez-Youngman S, Nguyen T, et al. 2018. Impact of participatory health research: a test of the community-based participatory research conceptual model. BioMed Res. Int. 2018:e7281405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ortiz K, Nash J, Shea L, Oetzel J, Garoutte J, et al. 2020. Partnerships, processes, and outcomes: a health equity-focused scoping meta-review of community-engaged scholarship. Annu. Rev. Public Health 41:177–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.PCORI (Patient-Cent. Outcomes Res. Inst.). 2020. Research fundamentals: preparing you to successfully contribute to research. PCORI. https://www.pcori.org/engagement/research-fundamentals [Google Scholar]
- 85.Perry CK, McCalmont JC, Ward JP, Menelas H-DK, Jackson C, et al. 2017. Mujeres Fuertes y Corazones Saludables: adaptation of the StrongWomen —healthy hearts program for rural Latinas using an intervention mapping approach. BMC Public Health 17(1):982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Petteway RJ. 2023. On epidemiology as racial-capitalist (re)colonization and epistemic violence. Crit. Public Health 33(1):5–12 [Google Scholar]
- 87.Pinto RM, Park S, Miles R, Ong PN. 2021. Community engagement in dissemination and implementation models: a narrative review. Implement. Res. Pract. 2:2633489520985305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, et al. 2017. Methods to improve the selection and tailoring of implementation strategies. J. Behav. Health Serv. Res. 44(2):177–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, et al. 2011. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Mental Health 38(2):65–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ramanadhan S, Cruz JL, Weese M, Naveed N, Kirk S, et al. 2023. Similar skills, different frames: a thematic analysis exploring conceptualizations held by community-based organization practitioners and academics regarding skills to use evidence-based interventions to address cancer inequities. Implement. Sci. Commun. 4(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ramanadhan S, Cruz J, Weese M, Rivard M, Eisenkraft A. Meaningful differences between academics and community-based organization staff regarding skills used in evidence-based program planning: a multi-dimensional scaling analysis. [AU: Is this in press yet? Please provide the anticipated year of publication, journal, and volume information if known. If not accepted for publication yet, we will convert this to an in-text reference only]
- 92.Ramanadhan S, Davis M, Donaldson S, Miller E, Minkler M. 2023. Participatory approaches in dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, ed. Brownson R, Colditz G, Proctor E, pp. 175–90. Oxford, UK: Oxford Univ. Press. 3rd ed. [Google Scholar]
- 93.Ramanadhan S, Davis MM, Armstrong RA, Baquero B, Ko LK, et al. 2018. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control 29(3):363–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ramanadhan S, Donaldson ST, Siqueira CE, Rackard-James C, Miller E, et al. 2022. Connecting implementation science, community-engaged research, and health promotion to address cancer inequities in Massachusetts: The UMB/DF-HCC U54 Outreach Core. Am. J. Health Promot. 36(4):597–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ramanadhan S, Ganapathy K, Nukala L, Rajagopalan S, Camillus JC. 2022. A model for sustainable, partnership-based telehealth services in rural India: an early process evaluation from Tuver village, Gujarat. PLOS ONE 17(1):e0261907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ramanadhan S, Minsky S, Martinez-Dominguez V, Viswanath K. 2017. Building practitioner networks to support dissemination and implementation of evidence-based programs in community settings. Transl. Behav. Med. 7(3):532–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ramanadhan S, Salvia M, Hanby E, Revette AC, Rivard MK, et al. 2023. “We’re always an afterthought”—designing tobacco control campaigns for dissemination with and to LGBTQ +-serving community organizations: a thematic analysis. Cancer Causes Control 34:673–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ramanadhan S, Viswanath K. 2018. Engaging communities to improve health: models, evidence, and the participatory knowledge translation (PaKT) framework. In Principles and Concepts of Behavioral Medicine: A Global Handbook, ed. Fisher EB, Cameron L, Christensen AJ, Ehlert U, Guo Y, et al. , pp. 679–711. New York: Springer Sci. Bus. Media [Google Scholar]
- 99.Ramanadhan S, Werts S, Knight C, Kelly S, Morgan J, et al. 2023. The role of small, locally-owned businesses in advancing community health and health equity: a qualitative exploration in a historically Black neighborhood in the USA. Crit. Public Health. 10.1080/09581596.2023.2256945. In press [DOI] [Google Scholar]
- 100.Reina DS, Reina ML. 2007. Building sustainable trust. OD Pract. 39(1):36 [Google Scholar]
- 101.Restar A, Minalga BJ, Quilantang MI, Adamson T, Dusic E, et al. 2023. Mapping community-engaged implementation strategies with transgender scientists, stakeholders, and trans-led community organizations. Curr. HIV/AIDS Rep. 20(3):160–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Deleted in proof [AU: Moved down]
- 103.Rycroft-Malone J, Burton C, Wilkinson JE, Harvey G, McCormack B, et al. 2015. Collective action for knowledge mobilisation: a realist evaluation of the Collaborations for Leadership in Applied Health Research and Care. Health Serv. Deliv. Res. 3(44). 10.3310/hsdr03440 [DOI] [PubMed] [Google Scholar]
- 104.Sánchez V, Sanchez-Youngman S, Dickson E, Burgess E, Haozous E, et al. 2021. CBPR implementation framework for community-academic partnerships. Am. J. Community Psychol. 67:284–96 [DOI] [PubMed] [Google Scholar]
- 105.Sanders Thompson VL, Ackermann N, Bauer KL, Bowen DJ, Goodman MS. 2021. Strategies of community engagement in research: definitions and classifications. Transl. Behav. Med. 11(2):441–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sandoval JA, Lucero J, Oetzel J, Avila M, Belone L, et al. 2012. Process and outcome constructs for evaluating community-based participatory research projects: a matrix of existing measures. Health Educ. Res. 27:680–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Schmittdiel JA, Grumbach K, Selby JV. 2010. System-based participatory research in health care: an approach for sustainable translational research and quality improvement. Ann. Fam. Med. 8(3):256–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Seguin RA, Perry CK, Solanki E, McCalmont JC, Ward JP, Jackson C. 2019. Mujeres Fuertes y Corazones Saludables, a culturally tailored physical activity and nutrition program for rural Latinas: findings from a pilot study. Int. J. Environ. Res. Public Health 16(4):630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shea CM, Young TL, Powell BJ, Rohweder C, Enga ZK, et al. 2017. Researcher readiness for participating in community-engaged dissemination and implementation research: a conceptual framework of core competencies. Transl. Behav. Med. 7(3):393–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shelton RC, Adsul P, Oh A, Moise N, Griffith DM. 2021. Application of an antiracism lens in the field of implementation science (IS): recommendations for reframing implementation research with a focus on justice and racial equity. Implement. Res. Pract. 2:26334895211049482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Simmons A, Chappel A, Kolbe AR, Bush L, Sommers BD. 2021. Health disparities by race and ethnicity during the COVID-19 pandemic: current evidence and policy approaches. Issue Brief, Off. Assist. Secr. Plan. Eval., Dep. Health Hum. Serv., Washington DC. https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//199516/covid-equity-issue-brief.pdf [Google Scholar]
- 112.Simonds V, Christopher S, Pease BCA, Jefferson L, Howe C, et al. 2012. Messengers for health: Apsáalooke women capture the vision of wellness. In Cancer Disparities: Causes and Evidence-Based Solutions, ed Elk R, Landrine H, pp. 277–92. New York: Springer [Google Scholar]
- 113.Smith JD, Li DH, Rafferty MR. 2020. The implementation research logic model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement. Sci. 15(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Smith LT. 2021. Decolonizing Methodologies: Research and Indigenous Peoples. London: Zed Books/Bloomsbury [Google Scholar]
- 115.Soedirgo J, Glas A. 2020. Toward active reflexivity: positionality and practice in the production of knowledge. PS Political Sci. Politics 53(3):527–31 [Google Scholar]; 115a. Sofaer S, Talis N, Edmunds M, Papa K. 2013. Navigating the translation and dissemination of PHSSR findings: a decision guide for researchers. Rep., AcademyHealth, Washington, DC [Google Scholar]
- 116.Spalluto LB, Thomas D, Beard KR, Campbell T, Audet CM, et al. 2019. A community-academic partnership to reduce health care disparities in diagnostic imaging. J. Am. Coll. Radiol. 16(4):649–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stanton MC, Ali SB, Sustain Cent. Team. 2022. A typology of power in implementation: building on the exploration, preparation, implementation, sustainment (EPIS) framework to advance mental health and HIV health equity. Implement. Res. Pract. 3:26334895211064250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Deleted in proof [AU: moved up for alphabetical order]
- 119.Torres VN, Williams EC, Ceballos RM, Donovan DM, Duran B, Ornelas IJ. 2020. Participant engagement in a community based participatory research study to reduce alcohol use among Latino immigrant men. Health Educ. Res. 35(6):627–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tracy SJ. 2019. Qualitative Research Methods: Collecting Evidence, Crafting Analysis, Communicating Impact. Hoboken, NJ: Wiley [Google Scholar]
- 121.Trickett EJ. 2009. Multilevel community-based culturally situated interventions and community impact: an ecological perspective. Am. J. Community Psychol. 43(3–4):257–66 [DOI] [PubMed] [Google Scholar]
- 122.Trickett EJ. 2011. Community-based participatory research as worldview or instrumental strategy: Is it lost in translation (al) research? Am. J. Public Health 101:1353–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tuck E 2009. Suspending damage: a letter to communities. Harv. Educ. Rev. 79(3):409–28 [Google Scholar]
- 125.Van De Ven AH, Johnson PE. 2006. Knowledge for theory and practice. Acad. Manag. Rev. 31(4):802–21 [Google Scholar]
- 126.Vaughan C, Gill-Atkinson L, Devine A, Zayas J, Ignacio R, et al. 2020. Enabling action: reflections upon inclusive participatory research on health with women with disabilities in the Philippines. Am. J. Community Psychol. 66(3–4):370–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Villalobos A, Blachman-Demner D, Percy-Laurry A, Belis D, Bhattacharya M. 2023. Community and partner engagement in dissemination and implementation research at the National Institutes of Health: an analysis of recently funded studies and opportunities to advance the field. Implement. Sci. Commun. 4(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Waldron IRG. 2021. There’s Something in the Water: Environmental Racism in Indigenous & Black Communities. Black Point, NS: Fernwood [Google Scholar]
- 129.Wallerstein N, Duran B. 2010. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am. J. Public Health 100(Suppl. 1):S40–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wallerstein N, Duran B, Oetzel J, Minkler M, eds. 2017. Community-Based Participatory Research for Health: Advancing Social and Health Equity. San Francisco: Wiley. 3rd ed. [Google Scholar]
- 131.Wallerstein N, Duran B, Oetzel J, Minkler M. 2017. Introduction to CBPR. See Ref. 130, pp. 3–16 [Google Scholar]
- 132.Wallerstein N, Oetzel J, Duran B, Tafoya G, Belone L, Rae R. 2008. What predicts outcomes in CBPR? See Ref. 75, pp. 371–92 [Google Scholar]
- 133.Waltz T, Schlundt D, Jones S, Gishe J, Alexander L, et al. 2022. Tailoring strategies for implementing behavioral health programs in churches. Poster presented at 15th Annual Conference on the Science of Dissemination and Implementation in Health, Washington, DC, Dec. 11–14 [Google Scholar]; 133a. WHO (World Health Organ.). 1986. The 1st International Conference on Health Promotion, Ottawa, 1986. Health Promotion https://www.who.int/teams/health-promotion/enhanced-wellbeing/first-global-conference [AU: Is this the intended site?] [Google Scholar]; 133b. WHO (World Health Organ.). 2017. WHO Strategic Communications Framework for effective communications. Rep., WHO, Geneva. https://www.who.int/docs/defaultsource/documents/communicating-for-health/communication-framework.pdf [Google Scholar]
- 134.Williams O, Sarre S, Papoulias SC, Knowles S, Robert G, et al. 2020. Lost in the shadows: reflections on the dark side of co-production. Health Res Policy Syst. 18(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wilson S 2008. Research Is Ceremony: Indigenous Research Methods. Black Point, NS: Fernwood [Google Scholar]
- 136.Kellogg Found WK. 2001. Community Health Scholars. W.K. Kellogg Foundation. https://www.wkkf.org/news-and-media/article/2003/07/community-health-scholars/ [AU: The existing link does not resolve for us. Edits ok?] [Google Scholar]
- 137.Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. 2019. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement. Sci. 14(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]


