Abstract
Objectives
Adults with spinal cord injury (SCI) are often sedentary, increasing their risk of cardiometabolic diseases. Leisure-time Physical Activity (LTPA) is physical activity completed during recreation time for enjoyment. We aimed to quantify LTPA in people ≥45 years with SCI and to explore its relationship with participants’ characteristics.
Methods
This is a secondary analysis on a subset of the Australian International SCI Survey in participants ≥45 years, at least 12 months post-injury. We described levels of LTPA and used multivariable regressions to estimate the associations between participant characteristics and LTPA.
Results
Of 1,281 participants (mean age: 62.7 years, mean time since injury: 18.7 years; 74% males) 44% reported no participation in LTPA. The average LTPA participation was 197 (SD 352) minutes per week (median: 50). Females (β = −62.3, 95% CI [−112.9, −11.7]), and participants with non-traumatic injuries (β = −105.2, 95% CI [−165.9, −44.6]) performed less LTPA. Time since injury was not associated with moderate-to-heavy LTPA (LR: Probability > F = 0.785).
Conclusion
LTPA promotion in the SCI population ≥45 years focusing on females and non-traumatic injuries is warranted.
Keywords: leisure-time physical activity, spinal cord injury, middle-aged, older adult, physical activity
Introduction
People with spinal cord injury (SCI) have very low levels of physical activity participation and are among the most inactive populations with physical disabilities [1]. The reasons for low engagement in physical activity vary but include loss of muscle function and strength and reduced energy expenditure [2], reduced mobility and fitness, pain, and environmental barriers, such as lack of accessible gyms, specialised programs or knowledgeable health professional in the community [3–5]. Low levels of physical activity contribute to an increased risk of cardiometabolic diseases, weight gain, pressure injuries, and infections, which may lead to frequent hospitalisations [6]. With an overall aging population and advances in medical care, the life expectancy of people living with SCI has increased, and there has been a shift in the demographic profile towards an older population sustaining and living with a SCI [7–9]. It is estimated that 20,800 people are living in Australia with an SCI, with approximately 175 new injuries each year [10]. The age-specific rate is highest for those aged 55–64 at 11.2 cases per million, closely followed by 10.1 cases per million for those aged 65–74 [10]. The main causes of traumatic injury are motor vehicle accidents (46%) and closely followed by falls (36%) [10]. Older people with SCI are usually less active than younger people and have an increased risk of developing secondary health conditions related to reduced physical activity [11, 12].
The World Health Organization (WHO) physical activity guidelines for adults with physical disabilities recommends that for cardiovascular disease risk-reduction, people need to participate in 150–300 min of moderate-intensity aerobic physical activity per week, or 75–150 min of vigorous aerobic physical activity per week, or a combination of the two, as well as strength-training at moderate intensity for all major muscle groups on 2 or more days per week [13]. Additionally, the physical activity guidelines for adults with SCI, recommend participation in at least 20 min of moderate-to-heavy intensity aerobic exercise twice a week plus three sets of strength exercises for each major functioning muscle group, at a moderate-to-heavy intensity, twice a week (for cardiorespiratory and muscle strength benefits). In addition, three times per week, including at least 30 min moderate-to-heavy intensity aerobic exercise, advised for cardiometabolic health benefits [14]. Despite these recommendations, research shows that between 27% [15] and 50% [16] of the SCI population are inactive, and those who engage in physical activity often do not meet the recommended levels of either guidelines particularly older adults [3, 11].
The risk of developing secondary cardiovascular disease and comorbidities might be reduced by participation in regular exercise and leisure-time physical activity (LTPA) [17]. LTPA is a physical activity undertaken in a person’s leisure-time or free time, such as playing sports, wheeling, walking, gardening, exercising at a gym and other recreational activities [18]. Further, increased LTPA positively impacts wellbeing, psychological health, and health-related quality of life in individuals with SCI [19–21]. Despite prior research on LTPA in the SCI population, limited evidence exists for middle-aged and older individuals with SCI regarding their participation, intensity, and duration of LTPA [11, 22]. A Swedish cohort study showed that many individuals with SCI over 50 years, and at least 10 years post-injury, did not meet minimum physical activity requirements necessary to achieve health benefits, with age and wheelchair use predicting low engagement [11].
In this study, we focussed on individuals with SCI who were ≥45 years, to represent effects of premature aging on multiple body systems [23]. At this age, many people in the general population begin to experience physical, psychological, and social changes associated with the aging process [24]. Defining “middle-aged and older” as ≥45 years is supported by multiple large-scale cohort studies that investigated the effects of aging in the general population [25–28]. These studies have provided important insights into the early stages of aging and helped to identify risk factors for age-related disabilities. This age definition allowed the investigation of physical activity participation in those experiencing the early effects of aging and acknowledges that, due to autonomic dysfunction, cardiometabolic and musculoskeletal changes associated with SCI [23, 29–31], people with SCI experience the effects of aging earlier than the general population [23]. Further, this age definition allows for future comparisons with sizeable studies in the general population. Therefore, the primary aim of this study was to describe the amount of LTPA performed by individuals with SCI ≥45 years living in Australia. The main objective was to describe levels of LTPA participation using the modified version of the Physical Activity Scale for Individuals with Physical Disabilities (PASIPD). The secondary aim was to investigate the relationships between LTPA and injury and demographic characteristics, with the objectives: 1) to determine the potential associations between LTPA and age, gender, completeness of injury and level of injury and 2) to explore the associations between time since injury and levels of LTPA.
Methods
Secondary analyses of the Australian arm of the International Spinal Cord Injury (Aus-InSCI) Community Survey was performed [32, 33]. This is a large cross-sectional survey that included questions about LTPA participation in Australians with SCI of all ages. The Aus-InSCI survey was conducted in 2018 to capture the lived experience of people living with SCI in the community in many areas including health, wellbeing, activity, independence, participation, leisure-time physical activity and sociodemographic characteristics [32, 33]. The Aus-InSCI survey was part of a larger international project investigating the lived experience of people with SCI across 22 countries. The design of the Aus-InSCI study and its cohort description have been published elsewhere [32]. The authors acknowledge that as this is a retrospective analysis, the data does not represent the lived experience of people with SCI during the COVID-19 pandemic.
The Aus-InSCI study was approved by the Northern Sydney Local Health District HREC (HREC/16/HAWKE/495) and Australian Institute of Health and Welfare Ethics Committee (EO2017/1/341). The ethical approval for this study was obtained from the Human Ethics Committee at the University of Technology Sydney (ETH22-7573).
Participants
Inclusion criteria for the Aus-InSCI study were adults aged ≥18 years old, community-dwelling, ≥12 months post-injury, traumatic (e.g., motor vehicle crash or fall) or non-traumatic/non-progressive SCI disease (e.g., spinal stenosis, infection, tumour) aetiology. Those with acute, sub-acute, congenital or neurodegenerative SCI, or severe cognitive impairment were excluded [32]. The present study used only data from participants ≥45 years of age.
Data Collection
Data from the Aus-InSCI participants extracted comprised demographic and injury information (i.e., age, gender, residential location, household income, marital status, level and completeness of injury) and levels of participation in LTPA obtained with a modified version of the PASIPD [34]. The PASIPD provides information about people’s physical activities, including participation in LTPA and activities of daily living (ADLs), where individuals respond to 2 ordinally ranked responses. Frequency options range from 1 (never) to 4 (often) while duration options range from 1 (less than 1) hour to 4 (greater than 4 h), and a total score is usually reported in metabolic equivalent of task (MET) hours per day [34, 35]. The modified version of the PASIPD, used in the Aus-InSCI, asked participants how many days per week they participated in mild, moderate, and heavy LTPA, and how many minutes per day they performed those activities at each intensity, using a free text space, to provide a value of total LTPA (in minutes per week). These data were then categorised as never (0 days/week), seldom (1–2 days/week); sometimes (3–4 days/week); or often (5–7 days/week). For this study, we only used LTPA data, and excluded data on participation in ADLs.
Data Analysis
Statistical analysis was completed in STATA-MP 17 software. Descriptive statistics were computed for sociodemographic and injury-related characteristics, as well as participation in total LTPA and moderate-to-heavy LTPA according to these characteristics.
LTPA
We used descriptive statistics to present the mean for total LTPA, moderate-to-heavy LTPA and strength-training LTPA, calculated in minutes per week. To deal with missing data on minutes per day of LTPA, we assumed that participants recording 0 days of participation in LTPA participated in 0 min of that type of LTPA. If the number of days of LTPA was missing, then minutes per day was also considered missing data. A total LTPA score combining light, moderate, heavy intensity, and strength LTPA days and minutes was calculated to determine each participant’s total LTPA volume in minutes per week (where no data was missing).
LTPA Versus Sociodemographic and Injury Characteristics
We used multivariable linear regression to estimate the association between the average minutes per week of participation in LTPA and the covariates age, gender, level and extent (completeness) of injury, time since injury, and cause of injury, based on inclusion in previous research [11, 36, 37] and the objectives of our study. Separate models were used for total LTPA, moderate-to-heavy LTPA and strength-training LTPA.
Dealing With Extreme Values and Missing Data
During initial data cleaning, 11 extreme observations (e.g., total LTPA >2,940 min per week, moderate-to-heavy LTPA >1,680 min per week) greater than the 99th percentile [38], were considered implausible and were excluded. The 11 extreme values were up to 4,620 min per week (equals 11 h per day) of total LTPA and up to 2,940 min per week (equals 7 h per day) of moderate-to-heavy LTPA.
In our statistical analysis, we evaluated patterns of missing data. We initially found a pattern of item non-response where participants reported “0” days of a type of LTPA without registering the number of minutes. We used a single-imputation strategy for these and imputed “0” into time where people had reported no days of that activity [39]. This improved the levels of missing data (Supplementary Figure S1) and we then used multiple imputation approach [deciding on 60 imputations after no change in estimated fraction of missing information (FMI)] with chained equations [40, 41] in a model with all LTPA day and time data, as well as auxiliary variables (Supplementary Table S1). Coefficients were across imputed datasets were combined with Rubin’s rules [42]. This analysis assumes data is “missing-at-random.”
LTPA Versus TSI
To investigate the association between LTPA and time since injury, a cubic spline model with four knots (at 5th, 35th, 65th, and 95th percentiles) was used as recommended [43], to allow the estimation between LTPA and the covariates without any assumption of the form of the relationship. Separate models were computed for total LTPA and moderate-to-heavy LTPA. To test the overall association of the spline form of TSI we used a likelihood ratio test.
Results
Participants’ sociodemographic and injury characteristics are presented in Table 1. There were 1,281 participants included. The mean (SD) age was 62.7 (10.1) years, the mean (SD) time since injury was 18.7 (14.8) years, and 74% were male. Most participants sustained a traumatic injury (81.5%), had paraplegia (58.3%) and an incomplete injury (67%). The majority (54%) lived in metropolitan areas, which includes capital cities or other metropolitan centres (population > 100,000), with 25.1% living in rural centres (population 10,000–99,000), and 16.8% living in remote areas (population < 10,000). Most participants (63%) were married or in a partnership.
TABLE 1.
Sociodemographic and injury characteristics in adults ≥45 years of age with spinal cord injury (n = 1,281) (Australia, 2024).
| Characteristics | |
|---|---|
| Age (years), mean (±SD), median (IQR) |
62.7 (±10.1) 62 (55–70) |
| Time since injury (years), mean (±SD), median (IQR) |
18.7 (±14.8) 14 (6–30) |
| Sex, n (%) - Male - Female |
944 (73.7) 337 (26.3) |
| Level of injury, n (%) - Paraplegia - Tetraplegia - missing |
747 (58.3) 461 (36) 73 (5.7) |
| Severity of injury, n (%) - Complete - Incomplete - missing |
391 (30.5) 858 (67) 32 (2.5) |
| Cause of Injury, n (%) - Traumatic - Non-traumatic - Unknown |
1,044 (81.5) 226 (17.6) 11 (0.9) |
| Marital status, n (%) - Single - Married - Widowed - Separated/divorced - missing |
227 (17.7) 808 (63.1) 62 (4.8) 182 (14.2) 2 (0.2) |
| Living place, n (%) - Capital city - Other metropolitan centres - Rural centres - Remote areas - missing |
410 (32) 282 (22) 322 (25.1) 215 (16.8) 52 (4.1) |
| Household income, n (%) - Less than $455 per week - $455 - $686 - $687 - $909 per week - $910 - $1,203 per week - $1,204 - $2,374 per week - $2,375 or more per week - missing |
303 (23.7) 165 (12.9) 138 (10.8) 109 (8.5) 209 (16.3) 180 (14.1) 1 (3.8) |
SD, standard deviation; IQR, Interquartile range. Residential location: Capital city, Other metropolitan centres (population > 100,000), Rural centres (population 10,000–99,000), Remote areas (population < 10,000).
The amount and intensity of LTPA is presented in Table 2. Overall, 43.8% of participants reported no participation (zero minutes per week) in total LTPA, 74.9% reported no participation in moderate-to-heavy LTPA, and 52% reported no participation in strength-training LTPA. The average participation in total weekly LTPA was 197 (SD 352) minutes/week, and the median (IQR) was 50 (IQR 0–240) minutes per week. The participation in moderate-to-heavy LTPA average was 62 (SD 174) minutes/week, with a median of 0 (IQR 0–2) minutes/week. The average participation in strength-training was 63 (SD 123) minutes per week and the median (IQR) was 0 (IQR 0–75) minutes per week.
TABLE 2.
Descriptive statistics (minutes per week) as a function of sociodemographic and injury characteristics of adults ≥ 45 years with spinal cord injury (Australia, 2024).
| LTPA (minutes per week) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Moderate-to- heavy | Strength training | |||||||
| Mean ± SD | Median | IQR | Mean ± SD | Median | IQR | Mean ± SD | Median | IQR | |
| Total sample (n = 1,281) | 197 ± 352 | 50 | 0, 240 | 62 ± 174 | 0 | 0, 2 | 63 ± 123 | 0 | 0, 75 |
| Sex | |||||||||
| - Male | 214 ± 381 | 60 | 0, 270 | 67 ± 191 | 0 | 0, 12.5 | 69 ± 131 | 0 | 0, 90 |
| - Female | 148 ± 244 | 35 | 0, 210 | 42 ± 111 | 0 | 0, 0 | 47 ± 96 | 0 | 0, 60 |
| Level of injury | |||||||||
| - Paraplegia | 192 ± 343 | 50 | 0, 242 | 61 ± 167 | 0 | 0, 20 | 62 ± 117 | 0 | 0, 90 |
| - Tetraplegia | 212 ± 374 | 60 | 0, 270 | 67 ± 188 | 0 | 0, 0 | 66 ± 130 | 0 | 0, 70 |
| Severity of injury | |||||||||
| - Complete | 183 ± 340 | 30 | 0, 242 | 67 ± 182 | 0 | 0, 30 | 61 ± 127 | 0 | 0, 70 |
| - Incomplete | 205 ± 360 | 60 | 0, 240 | 60 ± 171 | 0 | 0, 0 | 64 ± 121 | 0 | 0, 80 |
| Cause of injury | |||||||||
| - Traumatic | 213 ± 367 | 60 | 0, 280 | 68 ± 182 | 0 | 0, 30 | 67 ± 129 | 0 | 0, 80 |
| - Non-traumatic | 122 ± 253 | 0 | 0, 140 | 35 ± 117 | 0 | 0, 0 | 45 ± 85 | 0 | 0, 60 |
| Household income | |||||||||
| - Less than $455 per week | 173 ± 375 | 0 | 0, 180 | 50 ± 155 | 0 | 0, 0 | 66 ± 146 | 0 | 0, 60 |
| - $455 - $686 | 195 ± 373 | 60 | 0, 215 | 70 ± 199 | 0 | 0, 30 | 51 ± 102 | 0 | 0, 60 |
| - $687 - $909 per week | 185 ± 273 | 60 | 0, 315 | 55 ± 142 | 0 | 0, 0 | 59 ± 103 | 0 | 0, 100 |
| - $910 - $1,203 per week | 197 ± 321 | 70 | 0, 240 | 64 ± 204 | 0 | 0, 30 | 62 ± 92 | 30 | 0, 85 |
| - $1,204 - $2,374 per week | 278 ± 401 | 140 | 0, 400 | 95 ± 211 | 0 | 0, 120 | 77 ± 136 | 12 | 0, 120 |
| - $2,375 or more per week | 229 ± 376 | 150 | 0, 420 | 65 ± 169 | 0 | 0, 48 | 68 ± 124 | 0 | 0, 90 |
| Residential location | |||||||||
| - Capital city | 209 ± 335 | 60 | 0, 270 | 67 ± 181 | 0 | 0, 30 | 68 ± 119 | 0 | 0, 90 |
| - Other metropolitan centres | 194 ± 350 | 60 | 0, 220 | 67 ± 184 | 0 | 0, 40 | 62 ± 118 | 0 | 0, 80 |
| - Rural centres | 218 ± 389 | 60 | 0, 280 | 64 ± 168 | 0 | 0, 20 | 63 ± 132 | 0 | 0, 60 |
| - Remote areas | 191 ± 356 | 0 | 0, 210 | 57 ± 174 | 0 | 0, 0 | 57 ± 122 | 0 | 0, 70 |
| Marital Status | |||||||||
| - Single | 182 ± 323 | 35 | 0, 210 | 58 ± 173 | 0 | 0, 0 | 59 ± 109 | 0 | 0, 60 |
| - Married/partnership | 205 ± 352 | 60 | 0, 270 | 61 ± 170 | 0 | 0, 20 | 65 ± 123 | 0 | 0, 90 |
| - Widowed | 196 ± 401 | 30 | 0, 240 | 73 ± 225 | 0 | 0, 0 | 66 ± 141 | 0 | 0, 75 |
| - Separated/divorced | 185 ± 368 | 0 | 0, 240 | 70 ± 175 | 0 | 0, 30 | 59 ± 130 | 0 | 0, 60 |
LTPA, Leisure-time Physical Activity; SD, standard deviation; IQR, Interquartile range. The interquartile range column shows the 25th and 75th percentiles. All values in this table are untransformed but have excluded participants (n = 11) in the 99th percentile. Residential location: Capital city, Other metropolitan centres (population > 100,000), Rural centres (population 10,000–99,000), Remote areas (population < 10,000).
The multivariable regression analysis for total time spent in LTPA is presented in Table 3. Female gender (β = −62.3, 95% CI [−112.9, −11.7]), longer time since injury (β = −2.3, 95% CI [−3.9, −0.8]), and a non-traumatic cause of injury (β = −105.2, 95% CI [−165.9, −44.6]) were associated with less total time spent undertaking LTPA. Older age (β = −1.2, 95% CI [−2.4, −0.1]) and non-traumatic cause of injury (β = −32.5, 95% CI [−63.7, −1.4]) were associated with less moderate-to-heavy LTPA (Table 3). Female gender (β = −17.9, 95% CI [−34.2, −1.6]), longer time since injury (β = −1.0, 95% CI [−1.5,-0.5]) and non-traumatic cause of injury (β = −23.6, 95% CI [−43.4, −3.7]) were associated with less time performing strength-training (Table 3).
TABLE 3.
Multivariable regression analysis for total time spent in leisure-time physical activity, with beta cofficient and 95% confidence interval for each type of leisure-time physical activity (Australia, 2024).
| Covariate | Reference category | Total LTPA | Moderate-heavy LTPA | Strength training |
|---|---|---|---|---|
| Complete injury | Incomplete injury | −33.7 (−84.6; 17.1) | 0.0 (−26.2; 26.3) | 0.3 (−15.9; 16.6) |
| Tetraplegia | Paraplegia | −13.4 (−60.8; 34.1) | −7.8 (−32.5; 16.9) | −0.2 (−15.7; 15.3) |
| Non-traumatic injury | Traumatic injury | −105.2 (−165.9; −44.6)* | −32.5 (−63.7; −1.4)* | −23.6 (−43.4; −3.7)* |
| Age | /year | −1.3 (−3.6; 0.9) | −1.2 (−2.4; −0.1)* | 0.6 (−0.1; 1.4) |
| Time Since Injury | /year | −2.3 (−3.9; −0.8)* | −0.3 (−1.1; 0.5) | −1.0 (−1.5; −0.5)* |
| Female Gender | Male | −62.3 (−112.9; −11.7)* | −25.3 (−51.1; 0.4) | −17.9 (−34.2; −1.6)* |
*significant association where p < 0.05.
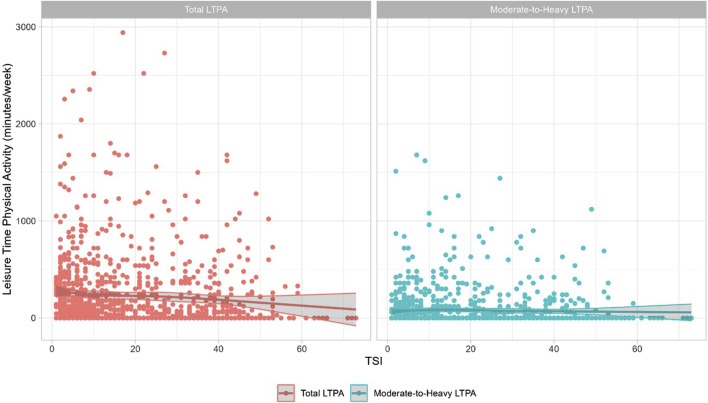
We found a statistically significant linear and negative association between total LTPA time and time since injury (Figure 1). Further analysis of the spline prediction and the likelihood ratios did not find a clear association between variables (Probability > F = 0.0506) (Figure 1). We did not find an association between moderate-to-heavy LTPA and time since injury when analysing the spline prediction and likelihood ratio (Probability > F = 0.785) (Figure 1). Overall the maximum FMI in each regression model and overall relative increase in variance were moderate (Supplementary Table S2).
FIGURE 1.
Leisure-time physical activity and time since injury with fitted cubic spline. Total Leisure-time physical activity: The relationship between total leisure-time physical activity (minutes/week) and time since injury (years) was significant for each participant (red-filled circles). Data were modelled using spine regression with four knots (five intervals) to investigate a non-linear relationship (red line). The spline prediction and likelihood ratio demonstrate there is limited evidence that time since injury (in spline form) was associated with total leisure-time physical activity (Probability > F = 0.0506). The shaded areas demonstrate 95% confidence intervals for the regression spline, which are more variable at higher time since injury. Moderate-to-Heavy leisure-time physical activity: The relationship between total moderate-to-heavy leisure-time physical activity (minutes/week) and time since injury (years) for each participant (blue-filled circles). Data were modelled using spine regression using four knots (five intervals) to investigate a non-linear relationship (blue line). The spline prediction and likelihood ratio demonstrate that time since injury (in spline form) is not associated with moderate-to-heavy leisure-time physical activity (Probability > F = 0.785). The shaded areas demonstrate 95% confidence intervals for the regression spline, which are more variable at higher time since injury (Australia, 2024).
Discussion
We undertook secondary analyses of an extensive cross-sectional survey that investigated levels of LTPA participation in Australians with SCI of all ages. The present study described the amount and intensity of LTPA participation in adults with SCI ≥45 years and assessed possible associations between LTPA participation and participants’ characteristics. While the averages for total LTPA participation and moderate-to-heavy LTPA appeared high, data were right-skewed, and the medians were very low. Three-quarters of the participants did not engage in any moderate-to-heavy LTPA and half did not engage in strength-training, meaning that a large proportion did not meet either the WHO or SCI-specific physical activity guideline recommendations [13, 14].
Our study highlights the importance of implementing early LTPA strategies for ageing women and those with non-traumatic injuries to mitigate the increased risk of reduced participation and health consequences. Despite statistically significant associations between total LTPA and time since injury, the B-Coefficients and 95% confidence intervals were small. We found limited evidence to suggest a clinically meaningful association between total LTPA and time since injury in the ≥45 years population, which differs from previous research in the general SCI population, which has suggested that those with longer time since injury (6–15 years) were more likely to be active than those injured for less than 5 years [3], and as injury duration progressed there was a increased chance that a person would be an exerciser [44]. Furthermore, this study found no evidence to suggest an association between participation in moderate-to-heavy LTPA and strength-training LTPA with time since injury, and that other personal and socioeconomic factors may be more important to identify to target those at risk of declining LTPA participation in people ≥45 years.
We found large variability in the reported time spent on total and moderate-to-heavy LTPA. This highlights the potential for some individuals with SCI ≥45 years of age to participate in long-term LTPA and maintain an active lifestyle, provided they can overcome the many psychosocial and environmental barriers to physical activity experienced in community [5, 45]. In people of all ages, the Aus-InSCI survey [44] suggested that so long as people begin LTPA post-injury, they were more likely to meet the physical activity volume recommendations. This potentially highlights that an important solution could be the development of strategies to embed LTPA into people’s lives early after injury [44].
There are differences when comparing LTPA participation in the SCI population to the non-disabled population. In the current investigation, 43.8% of participants reported no participation in LTPA, and 75% did not participate in the moderate-to-heavy intensity required to achieve health and fitness benefits. The Australian “45 and Up” study surveyed over 100,000 individuals from the general population and identified that three-quarters of respondents met the WHO physical activity recommendations [46]. Another large cross-sectional study conducted in the SCI population in Thailand found that only 14% of individuals met the SCI-specific physical activity guidelines and only 7% met the recommended WHO physical activity guidelines for adults with a disability [47], compared to 48% without a disability [14]. This confirms that a large proportion of individuals ≥45 years with SCI in Australia have a sedentary lifestyle compared to those who are non-disabled. As such, they are at increased risk of developing cardiometabolic diseases and raising the risk of poor health and wellbeing outcomes as they age [22, 48, 49]. Health promotion strategies must be explicitly tailored to adults ≥45 years with SCI, including programs and resources to promote accessible and enjoyable LTPA opportunities in the community.
The present Australian cohort showed some similarities with earlier work, which found that females with SCI have lower levels of LTPA participation [11, 50, 51]. In Sweden, it was suggested that traditional gender roles might be a barrier to access to LTPA for women [11]. Other sub-populations with low levels of LTPA (median of 0 min per week total and moderate-to-heavy LTPA) included low-income earners (<$455 per week), being separated or divorced, those living in remote areas (population < 10,000) and having non-traumatic injuries. There is the potential that adults ≥45 years with SCI living in regional and rural communities in Australia face unique geographic challenges due to the country’s size. Other key factors influencing LTPA participation in individuals with SCI include socioeconomic status. Our study revealed that those in the lower family income bracket engaged in the least LTPA. This underscores the significance of policymakers addressing barriers such as costs associated with gym attendance and sporting groups, purchasing specialised equipment and transportation expenses to enhance access and participation.
While cardiovascular fitness and health are necessary, mental health, wellbeing and quality of life outcomes are equally important for those ≥45 years with SCI. In general, people with SCI are 5% more likely to develop anxiety, 20% more likely to develop depression and 15% more likely to develop psychological issues than people without SCI [52]. However, older adults with long-term SCI report a low prevalence of depression, with one-third displaying clinically relevant depressive symptoms but only 5% displaying probable clinical depression [53]. Participation in LTPA has been shown to reduce anxiety and depression significantly and to improve the quality of life in those with long-term disabilities [21, 54]. Social exclusion can play an important factor in aging, especially for those with a disability [55], and LTPA participation could be a way for those aging with SCI to socialise, potentially improving mental health and quality of life. In summary, LTPA participation can significantly promote successful aging and overall health and quality of life for this population [21, 54].
Strengths and Limitations
This study is the first to evaluate LTPA participation in adults ≥45 years of age with SCI in Australia. Our sample (1,281 people) provides an adequate representation of the Australian population living with SCI (approximately 20,800 people) [56] in the community as it included a large number of Australians from different states and territories.
A limitation of this study was the missing data on LTPA participation, which might have affected the generalisability of the findings. Further, some participants reported excessive levels of LTPA (up to 11 h per day). The extreme ranges of the LTPA data raise questions about the accuracy of the self-reported data. A drawback was that there was no way to “validate” the survey responses in a self-reported design. One potential factor contributing to these inconsistencies could be recall bias, which is associated with self-reported assessments of LTPA, leading to over-estimating activity levels [57]. The length of the Aus-InSCI survey was up to 1-hour and could have also contributed to survey fatigue, prompting some individuals to leave the LTPA questionnaire unanswered. Alternatively, participants could have deliberately misreported their responses for various reasons. Moreover, the confusion between ADL’s and LTPA may have led respondents to score general daily activities as LTPA if they perceived them as having sufficient physical stress due to their potentially limited mobility. This response bias could have resulted from a misunderstanding of what constitutes LTPA, impacting the accuracy of reported activity levels. Given that the Aus-InSCI was a survey, using objective measures such as accelerometers was not feasible. Another limitation is that the data collected was pre-COVID 19 pandemic, therefore a more current analysis on levels of physical activity in this population is warranted due to the potential impact of the restrictions related to the pandemic on physical activity behaviours. There has been minimal research conducted post the COVID-19 pandemic on levels of physical activity in people with SCI, however, one study determined that individuals with paraplegia who were full-time manual wheelchair users displayed lower levels of physical activity during the pandemic than in the pre-pandemic period [58]. We acknowledge that immediately post-pandemic LTPA participation may have changed due to decreased access to recreational and sports facilities or fear of contracting the virus in the community [59].
Clinical Applications and Recommendations
Our findings demonstrated the importance of health promotion strategies to increase LTPA uptake among those ≥45 years with SCI, especially aging women, those with non-traumatic injuries, and those living in remote communities or with a lower socioeconomic status. To optimise LTPA engagement, we recommend the development of tailored LTPA community programs for older women and individuals with non-traumatic injuries, as they share increased susceptibility to inactive lifestyles. Health promotion strategies should include health professionals and clinicians providing education on the physical and mental health benefits of LTPA and offering information resources on local LTPA opportunities available upon discharge and within the community to maximize uptake [60]. Furthermore, extending physical activity opportunities to rural and remote regions via telehealth-exercise delivery in groups can enhance accessibility and community participation [61]. Moreover, the Australian National Disability Insurance Scheme (NDIS) and public and private sector insurers should support middle-aged and older people with SCI to access community based LTPA by providing, for example, gym memberships and funding for community sporting clubs or activities to ensure inclusivity and better health outcomes in this population.
We propose that future research should prioritise consumer-informed strategies to improve LTPA participation. By addressing inactivity in this population, we hope to minimise its health and financial burden. Further research could lead to developing new interventions and policy changes concerning LTPA, focusing on promoting healthy aging with SCI in our community from as early as 45 years. Clinicians and consumer agencies must educate these at-risk groups, which may reduce the strain on the healthcare system as the population of older people with SCI grows.
Conclusion
We found considerable variation in the weekly time spent in LTPA in older individuals with SCI in Australia, with a large proportion (44%) not participating in any LTPA, and the majority (almost 75%) not participating in moderate-to-heavy LTPA. Ageing women and those with non-traumatic injuries tend to participate less in weekly LTPA. Moreover, time since injury was not associated with LTPA participation in our sample. While some participants with SCI can maintain an active lifestyle, many are not achieving the recommended dosage of physical activity that translates into health benefits and reduction of cardiometabolic disease risk.
Acknowledgments
The authors would like to thank team members of each organisation involved in the Aus-InSCI survey and the Aus-InSCI Steering and Scientific Committee members for their time and support. In addition, the authors are grateful to Spinal Cord Injuries Australia, Forward Ability Support (Formerly Paraplegic and Quadriplegic Association of New South Wales) and The Paraplegic and Quadriplegic Association of South Australia for their commitment and support for the successful completion of the study. We would also like to acknowledge the support from the Centre for Data Linkage, Curtin University, Western Australia and the Australian Institute of Health and Welfare, Canberra, for data linkage. This study is based on the International Spinal Cord Injury (InSCI) Community Survey data [62]. The members of the InSCI Steering Committee are JM, J. Patrick Engkasan, G. Stucki, M. Brach, J. Bickenbach, C. Fekete, C. Thyrian, L. Battistella, J. Li, B. Perrouin-Verbe, C. Gutenbrunner, C. A. Rapidi, L. K. Wahyuni, M. Zampolini, E. Saitoh, B. S. Lee, A. Juocevicius, N. Hasnan, A. Hajjioui, M. W. M. Post, A. C. Martinsen, P. Tederko, D. Popa, C. Joseph, M. Avellanet, M. Baumberger, A. Kovindha, R. Escorpizo.
Funding Statement
The authors declare that financial support was received for the research, authorship, and/or publication of this article. Four state-based organisations contributed funding to undertake the Aus-InSCI survey. The coordinating National Study Centre in New South Wales based at the John Walsh Centre for Rehabilitation Research at The University of Sydney received funding from Insurance and Care NSW (icare NSW). The site in Victoria received a grant from the Spinal Research Institute (SRI) and Australasian Spinal Cord Injury Network Ltd. (voluntarily revoked, effective 31 July 2019). The site in South Australia received funding from Lifetime Support Authority South Australia. The site in Queensland was supported by the Division of Rehabilitation, Princess Alexandra Hospital, The Hopkins Centre, and Griffith University. The funding organisations do not take direct responsibility for any of the following: study design, data collection, drafting of the manuscript, or decision to publish.
Ethics Statement
The studies involving humans were approved by Northern Sydney Local Health District Human Research Ethics Committee (HREC/16/HAWKE/495) and the Australian Institute of Health and Welfare Ethics Committee (EO2017/1/341). Further ethical approval for secondary analysis was obtained from the Human Ethics Committee at the University of Technology Sydney (ETH22-7573). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author Contributions
JM is a member of the International Scientific Committee and National leader of the Aus-InSCI Community Survey. JM, TG, RM, AN, and MA developed the Aus-InSCI study concept, survey design and the Australian protocol. MA managed the project which included data collection, data entry, risk mitigation and quality checking. LS, MA, PS, GD, AV, KR, JM, and CQO were involved in the design and methodology planning of this Aus-InSCI secondary analysis. KR provided statistical analysis expertise. LS, CQO, and PS wrote the manuscript. All authors contributed to revising the data analysis, interpretation and revision of the manuscript.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2024.1607276/full#supplementary-material
References
- 1. Fernhall B, Heffernan K, Jae SY, Hedrick B. Health Implications of Physical Activity in Individuals With Spinal Cord Injury: A Literature Review. J Health Hum Serv Adm (2008) 30(4):468–502. 10.1177/107937390803000402 [DOI] [PubMed] [Google Scholar]
- 2. Buchholz AC, McGillivray CF, Pencharz PB. Physical Activity Levels Are Low in Free-Living Adults With Chronic Paraplegia. Obes Res (2003) 11(4):563–70. 10.1038/oby.2003.79 [DOI] [PubMed] [Google Scholar]
- 3. Rauch A, Hinrichs T, Oberhauser C, Cieza A, SwiSCI study group. Do People With Spinal Cord Injury Meet the WHO Recommendations on Physical Activity? Int J Public Health (2016) 61(1):17–27. 10.1007/s00038-015-0724-5 [DOI] [PubMed] [Google Scholar]
- 4. Alschuler KN, Jensen MP, Sullivan-Singh SJ, Borson S, Smith AE, Molton IR. The Association of Age, Pain, and Fatigue With Physical Functioning and Depressive Symptoms in Persons With Spinal Cord Injury. J Spinal Cord Med (2013) 36(5):483–91. 10.1179/2045772312Y.0000000072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vissers M, van den Berg-Emons R, Sluis T, Bergen M, Stam H, Bussmann H. Barriers to and Facilitators of Everyday Physical Activity in Persons With a Spinal Cord Injury After Discharge From the Rehabilitation Centre. J Rehabil Med (2008) 40(6):461–7. 10.2340/16501977-0191 [DOI] [PubMed] [Google Scholar]
- 6. Williams TL, Smith B, Papathomas A. The Barriers, Benefits and Facilitators of Leisure Time Physical Activity Among People With Spinal Cord Injury: A Meta-Synthesis of Qualitative Findings. Health Psychol Rev (2014) 8(4):404–25. 10.1080/17437199.2014.898406 [DOI] [PubMed] [Google Scholar]
- 7. Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M, et al. Spinal Cord Injury and Aging: Challenges and Recommendations for Future Research. Am J Phys Med Rehabil (2012) 91(1):80–93. 10.1097/PHM.0b013e31821f70bc [DOI] [PubMed] [Google Scholar]
- 8. Krause JS, Clark JMR, Saunders LL. SCI Longitudinal Aging Study: 40 Years of Research. Top Spinal Cord Inj Rehabil (2015) 21(3):189–200. 10.1310/sci2103-189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ, et al. Changing Demographics of Spinal Cord Injury Over a 20-Year Period: A Longitudinal Population-Based Study in Scotland. Spinal Cord (2016) 54(4):270–6. 10.1038/sc.2015.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Australian Institute of Health and Welfare. Spinal Cord Injuries in Australia 2017-18 (2021). Available from: https://www.aihw.gov.au/reports/injury/spinal-cord-injury-australia-2017-18/summary (Accessed October 10, 2023). [Google Scholar]
- 11. Jorgensen S, Ginis KAM, Lexell J. Leisure Time Physical Activity Among Older Adults With Long-Term Spinal Cord Injury. Spinal Cord (2017) 55(9):848–56. 10.1038/sc.2017.26 [DOI] [PubMed] [Google Scholar]
- 12. Jörgensen S, Iwarsson S, Lexell J. Secondary Health Conditions, Activity Limitations, and Life Satisfaction in Older Adults With Long-Term Spinal Cord Injury. Pm r (2017) 9(4):356–66. 10.1016/j.pmrj.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 13. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br J Sports Med (2020) 54(24):1451–62. 10.1136/bjsports-2020-102955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-Based Scientific Exercise Guidelines for Adults With Spinal Cord Injury: An Update and a New Guideline. Spinal Cord (2018) 56(4):308–21. 10.1038/s41393-017-0017-3 [DOI] [PubMed] [Google Scholar]
- 15. Rauch A, Fekete C, Oberhauser C, Marti A, Cieza A. Participation in Sport in Persons With Spinal Cord Injury in Switzerland. Spinal cord (2014) 52(9):706–11. 10.1038/sc.2014.102 [DOI] [PubMed] [Google Scholar]
- 16. Ginis KAM, Arbour-Nicitopoulos KP, Latimer AE, Buchholz AC, Bray SR, Craven BC, et al. Leisure Time Physical Activity in a Population-Based Sample of People With Spinal Cord Injury Part II: Activity Types, Intensities, and Durations. Arch Phys Med Rehabil (2010) 91(5):729–33. 10.1016/j.apmr.2009.12.028 [DOI] [PubMed] [Google Scholar]
- 17. Lundstrom U, Wahman K, Seiger A, Gray DB, Isaksson G, Lilja M. Participation in Activities and Secondary Health Complications Among Persons Aging With Traumatic Spinal Cord Injury. Spinal Cord (2017) 55(4):367–72. 10.1038/sc.2016.153 [DOI] [PubMed] [Google Scholar]
- 18. Bouchard C, Shephard RJ, Brubaker PH. Physical Activity, Fitness, and Health: Consensus Statement. Med Sci Sports Exerc (1994) 26(1):119. 10.1249/00005768-199401000-00024 [DOI] [Google Scholar]
- 19. Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J, et al. Long-Term Exercise Training in Persons With Spinal Cord Injury: Effects on Strength, Arm Ergometry Performance and Psychological Well-Being. Spinal Cord (2003) 41(1):34–43. 10.1038/sj.sc.3101389 [DOI] [PubMed] [Google Scholar]
- 20. Filipcic T, Sember V, Pajek M, Jerman J. Quality of Life and Physical Activity of Persons With Spinal Cord Injury. Int J Environ Res Public Health (2021) 18(17):9148. 10.3390/ijerph18179148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tomasone JR, Wesch NN, Ginis KAM, Noreau L. Spinal Cord Injury, Physical Activity, and Quality of Life: A Systematic Review. Kinesiol Rev (Champaign, Ill) (2013) 2(2):113–29. 10.1123/krj.2.2.113 [DOI] [Google Scholar]
- 22. Jörgensen S, Svedevall S, Magnusson L, Martin Ginis KA, Lexell J. Associations Between Leisure Time Physical Activity and Cardiovascular Risk Factors Among Older Adults With Long-Term Spinal Cord Injury. Spinal Cord (2019) 57(5):427–33. 10.1038/s41393-018-0233-5 [DOI] [PubMed] [Google Scholar]
- 23. Hitzig SL, Eng JJ, Miller WC, Sakakibara BM, SCIRE Research Team. An Evidence-Based Review of Aging of the Body Systems Following Spinal Cord Injury. Spinal Cord (2011) 49(6):684–701. 10.1038/sc.2010.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rowe JW, Kahn RL. Human Aging: Usual and Successful. Science (1987) 237:143–9. 10.1126/science.3299702 [DOI] [PubMed] [Google Scholar]
- 25. 45 and Up Study Collaborators, Banks E, Redman S, Jorm L, Armstrong B, Bauman A, et al. Cohort Profile: The 45 and up Study. Int J Epidemiol (2008) 37(5):941–7. 10.1093/ije/dym184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hofman A, Breteler MMB, van Duijn CM, Krestin GP, Pols HA, Stricker BHC, et al. The Rotterdam Study: Objectives and Design Update. Eur J Epidemiol (2007) 22(11):819–29. 10.1007/s10654-007-9199-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Raina PS, Wolfson C, Kirkland SA, Griffith LE, Oremus M, Patterson C, et al. The Canadian Longitudinal Study on Aging (CLSA). Can J Aging (2009) 28(3):221–9. 10.1017/S0714980809990055 [DOI] [PubMed] [Google Scholar]
- 28. Perianayagam A, Bloom D, Lee J, Parasuraman S, Sekher TV, Mohanty SK, et al. Cohort Profile: The Longitudinal Ageing Study in India (LASI). Int J Epidemiol (2022) 51:e167–e176. 10.1093/ije/dyab266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Raguindin PF, Stoyanov J, Eriks-Hoogland I, Stucki G, Jordan X, Schubert M, et al. Cardiometabolic Risk Profiling During Spinal Cord Injury Rehabilitation: A Longitudinal Analysis From the Swiss Spinal Cord Injury (SwiSCI) Cohort. PM&R (2023) 15(6):715–30. 10.1002/pmrj.12857 [DOI] [PubMed] [Google Scholar]
- 30. Charlifue S, Lammertse DP, Adkins RH. Aging With Spinal Cord Injury: Changes in Selected Health Indices and Life Satisfaction. Arch Phys Med Rehabil (2004) 85(11):1848–53. 10.1016/j.apmr.2004.03.017 [DOI] [PubMed] [Google Scholar]
- 31. Szlachcic Y, Adkins R, Govindarajan S, Cao Y, Krause J. Cardiometabolic Changes and Disparities Among Persons With Spinal Cord Injury: A 17-Year Cohort Study. Top Spinal Cord Inj Rehabil (2014) 20(2):96–104. 10.1310/sci2002-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Middleton JW, Arora M, Kifley A, Geraghty T, Borg SJ, Marshall R, et al. Australian Arm of the International Spinal Cord Injury (Aus-InSCI) Community Survey: 1. Population-Based Design, Methodology and Cohort Profile. Spinal Cord (2023) 61(3):194–203. 10.1038/s41393-022-00850-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Middleton JW, Arora M, Kifley A, Clark J, Borg SJ, Tran Y, et al. Australian Arm of the International Spinal Cord Injury (Aus-InSCI) Community Survey: 2. Understanding the Lived Experience in People With Spinal Cord Injury. Spinal Cord (2022) 60(12):1069–79. 10.1038/s41393-022-00817-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The Physical Activity Scale for Individuals With Physical Disabilities: Development and Evaluation. Arch Phys Med Rehabil (2002) 83(2):193–200. 10.1053/apmr.2002.27467 [DOI] [PubMed] [Google Scholar]
- 35. van den Berg-Emons RJ, L'Ortye AA, Buffart LM, Nieuwenhuijsen C, Nooijen CF, Bergen MP, et al. Validation of the Physical Activity Scale for Individuals With Physical Disabilities. Arch Phys Med Rehabil (2011) 92(6):923–8. 10.1016/j.apmr.2010.12.006 [DOI] [PubMed] [Google Scholar]
- 36. Buchholz AC, Ginis KAM, Bray SR, Craven BC, Hicks AL, Hayes KC, et al. Greater Daily Leisure Time Physical Activity Is Associated With Lower Chronic Disease Risk in Adults With Spinal Cord Injury. Appl Physiol Nutr Metab (2009) 34(4):640–7. 10.1139/H09-050 [DOI] [PubMed] [Google Scholar]
- 37. de Groot S, Dallmeijer AJ, Post MWM, Angenot ELD, van der Woude LHV. The Longitudinal Relationship Between Lipid Profile and Physical Capacity in Persons With a Recent Spinal Cord Injury. Spinal Cord (2008) 46(5):344–51. 10.1038/sj.sc.3102147 [DOI] [PubMed] [Google Scholar]
- 38. Kwak SK, Kim JH. Statistical Data Preparation: Management of Missing Values and Outliers. Korean J Anesthesiol (2017) 70(4):407–11. 10.4097/kjae.2017.70.4.407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Banks E, Jorm L, Rogers K, Clements M, Bauman A. Screen-Time, Obesity, Ageing and Disability: Findings From 91 266 Participants in the 45 and up Study. Public Health Nutr (2011) 14(1):34–43. 10.1017/S1368980010000674 [DOI] [PubMed] [Google Scholar]
- 40. Buuren SV, Groothuis-Oudshoorn K. MICE: Multivariate Imputation by Chained Equations in R (2010). [Google Scholar]
- 41. Lee JH, Huber JC. Evaluation of Multiple Imputation With Large Proportions of Missing Data: How Much Is Too Much? Iran J Public Health (2021) 50(7):1372–80. 10.18502/ijph.v50i7.6626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Marshall A, Altman DG, Holder RL, Royston P. Combining Estimates of Interest in Prognostic Modelling Studies After Multiple Imputation: Current Practice and Guidelines. BMC Med Res Methodol (2009) 9:57. 10.1186/1471-2288-9-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Harrell JFE. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2nd ed. Cham: Springer Nature; (2015). [Google Scholar]
- 44. Watson PK, Arora M, Middleton JW, Quel de Oliveira C, Heard R, Nunn A, et al. Leisure-Time Physical Activity in People With Spinal Cord Injury—Predictors of Exercise Guideline Adherence. Int J Public Health (2022) 67:1605235. 10.3389/ijph.2022.1605235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Roberton T, Bucks R, Skinner T, Allison G, Dunlop S. Barriers to Physical Activity in Individuals With Spinal Cord Injury: A Western Australian Study. Aust J Rehabil Couns (2011) 17(2):74–88. 10.1375/jrc.17.2.74 [DOI] [Google Scholar]
- 46. Bauman A, Lee K, Ding D, Phongsavan P. Physical Activity Research in the First 15 Years of the “45 and up” Cohort Study: A Narrative Review and Citation Analysis. Public Health Res Pract (2022) 32:3242234. 10.17061/phrp3242234 [DOI] [PubMed] [Google Scholar]
- 47. Eitivipart AC, Arora M, Quel de Oliveira C, Heard R, Middleton JW, Davis GM. Assessing Physical Activity and Health-Related Quality of Life in Individuals With Spinal Cord Injury: A National Survey in Thailand. Disabil Rehabil (2022) 44(23):7048–58. 10.1080/09638288.2021.1979665 [DOI] [PubMed] [Google Scholar]
- 48. Itodo OA, Flueck JL, Raguindin PF, Stojic S, Brach M, Perret C, et al. Physical Activity and Cardiometabolic Risk Factors in Individuals With Spinal Cord Injury: A Systematic Review and Meta-Analysis. Eur J Epidemiol (2022) 37(4):335–65. 10.1007/s10654-022-00859-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Jörgensen S, Costa Andersson MV, Lexell J. Changes in Health-Related Quality of Life Among Older Adults Aging With Long-Term Spinal Cord Injury. Spinal Cord (2021) 59(7):769–76. 10.1038/s41393-020-00579-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hicks AL, Martin Ginis KA, Pelletier CA, Ditor DS, Foulon B, Wolfe DL. The Effects of Exercise Training on Physical Capacity, Strength, Body Composition and Functional Performance Among Adults With Spinal Cord Injury: A Systematic Review. Spinal Cord (2011) 49(11):1103–27. 10.1038/sc.2011.62 [DOI] [PubMed] [Google Scholar]
- 51. Ginis KAM, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, et al. Leisure Time Physical Activity in a Population-Based Sample of People With Spinal Cord Injury Part I: Demographic and Injury-Related Correlates. Arch Phys Med Rehabil (2010) 91(5):722–8. 10.1016/j.apmr.2009.12.027 [DOI] [PubMed] [Google Scholar]
- 52. Sweis R, Biller J. Systemic Complications of Spinal Cord Injury. Curr Neurol Neurosci Rep (2017) 17(2):8. 10.1007/s11910-017-0715-4 [DOI] [PubMed] [Google Scholar]
- 53. Jörgensen S, Ginis KA, Iwarsson S, Lexell J. Depressive Symptoms Among Older Adults With Long-Term Spinal Cord Injury: Associations With Secondary Health Conditions, Sense of Coherence, Coping Strategies and Physical Activity. J Rehabil Med (2017) 49(8):644–51. 10.2340/16501977-2259 [DOI] [PubMed] [Google Scholar]
- 54. Battalio SL, Huffman SE, Jensen MP. Longitudinal Associations Between Physical Activity, Anxiety, an Depression in Adults With Long-Term Physical Disabilities. Health Psychol (2020) 39(6):529–38. 10.1037/hea0000848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Walsh K, Scharf T, Keating N. Social Exclusion of Older Persons: A Scoping Review and Conceptual Framework. Eur J Ageing (2017) 14(1):81–98. 10.1007/s10433-016-0398-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Collaborative TASCIR. Australian Government Treasury (2022). Available from: https://treasury.gov.au/sites/default/files/2021-05/171663_the_australian_spinal_cord_injury_research_collaborative_supporting_document_3pdf (Accessed November 10, 2023). [Google Scholar]
- 57. Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A Comparison of Direct Versus Self-Report Measures for Assessing Physical Activity in Adults: A Systematic Review. Int J Behav Nutr Phys Activity (2008) 5(1):56. 10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Marco-Ahulló A, Montesinos-Magraner L, González L-M, Morales J, Bernabéu-García JA, García-Massó X. Impact of COVID-19 on the Self-Reported Physical Activity of People With Complete Thoracic Spinal Cord Injury Full-Time Manual Wheelchair Users. J spinal cord Med (2022) 45(5):755–9. 10.1080/10790268.2020.1857490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. LaVela SL, Wu J, Nevedal AL, Harris AHS, Frayne SM, Arnow KD, et al. The Impact of the COVID-19 Pandemic on Individuals Living With Spinal Cord Injury: A Qualitative Study. Rehabil Psychol (2023) 68(1):12–24. 10.1037/rep0000469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Holm NJ, Møller T, Adamsen L, Dalsgaard LT, Biering-Sorensen F, Schou LH. Health Promotion and Cardiovascular Risk Reduction in People With Spinal Cord Injury: Physical Activity, Healthy Diet and Maintenance After Discharge-Protocol for a Prospective National Cohort Study and a Preintervention-Postintervention Study. BMJ Open (2019) 9(12):e030310. 10.1136/bmjopen-2019-030310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Chemtob K, Rocchi M, Arbour-Nicitopoulos K, Kairy D, Fillion B, Sweet SN. Using Tele-Health to Enhance Motivation, Leisure Time Physical Activity, and Quality of Life in Adults With Spinal Cord Injury: A Self-Determination Theory-Based Pilot Randomized Control Trial. Psychol Sport Exerc (2019) 43:243–52. 10.1016/j.psychsport.2019.03.008 [DOI] [Google Scholar]
- 62. Fekete C, Post MWM, Bickenbach J, Middleton J, Prodinger B, Selb M, et al. A Structured Approach to Capture the Lived Experience of Spinal Cord Injury: Data Model and Questionnaire of the International Spinal Cord Injury Community Survey. Am J Phys Med Rehabil (2017) 96(2):S5–S16. 10.1097/PHM.0000000000000622 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.