Problem based learning is used in many medical schools in the United Kingdom and worldwide. This article describes this method of learning and teaching in small groups and explains why it has had an important impact on medical education.
What is problem based learning?
In problem based learning (PBL) students use “triggers” from the problem case or scenario to define their own learning objectives. Subsequently they do independent, self directed study before returning to the group to discuss and refine their acquired knowledge. Thus, PBL is not about problem solving per se, but rather it uses appropriate problems to increase knowledge and understanding. The process is clearly defined, and the several variations that exist all follow a similar series of steps.
Generic skills and attitudes
| • Teamwork | • Critical evaluation of literature |
| • Chairing a group | • Self directed learning and use of resources |
| • Listening | • Presentation skills |
| • Recording | |
| • Cooperation | |
| • Respect for colleagues' views | |
Group learning facilitates not only the acquisition of knowledge but also several other desirable attributes, such as communication skills, teamwork, problem solving, independent responsibility for learning, sharing information, and respect for others. PBL can therefore be thought of as a small group teaching method that combines the acquisition of knowledge with the development of generic skills and attitudes. Presentation of clinical material as the stimulus for learning enables students to understand the relevance of underlying scientific knowledge and principles in clinical practice.
However, when PBL is introduced into a curriculum, several other issues for curriculum design and implementation need to be tackled. PBL is generally introduced in the context of a defined core curriculum and integration of basic and clinical sciences. It has implications for staffing and learning resources and demands a different approach to timetabling, workload, and assessment. PBL is often used to deliver core material in non-clinical parts of the curriculum. Paper based PBL scenarios form the basis of the core curriculum and ensure that all students are exposed to the same problems. Recently, modified PBL techniques have been introduced into clinical education, with “real” patients being used as the stimulus for learning. Despite the essential ad hoc nature of learning clinical medicine, a “key cases” approach can enable PBL to be used to deliver the core clinical curriculum.
What happens in a PBL tutorial?
PBL tutorials are conducted in several ways. In this article, the examples are modelled on the Maastricht “seven jump” process, but its format of seven steps may be shortened.
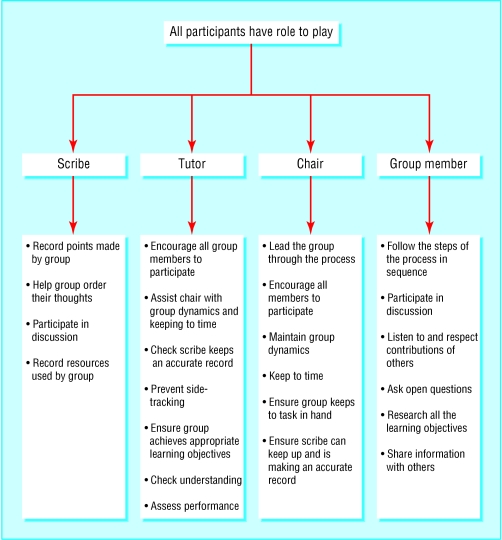
A typical PBL tutorial consists of a group of students (usually eight to 10) and a tutor, who facilitates the session. The length of time (number of sessions) that a group stays together with each other and with individual tutors varies between institutions. A group needs to be together long enough to allow good group dynamics to develop but may need to be changed occasionally if personality clashes or other dysfunctional behaviour emerges.
Students elect a chair for each PBL scenario and a “scribe” to record the discussion. The roles are rotated for each scenario. Suitable flip charts or a whiteboard should be used for recording the proceedings. At the start of the session, depending on the trigger material, either the student chair reads out the scenario or all students study the material. If the trigger is a real patient in a ward, clinic, or surgery then a student may be asked to take a clinical history or identify an abnormal physical sign before the group moves to a tutorial room. For each module, students may be given a handbook containing the problem scenarios, and suggested learning resources or learning materials may be handed out at appropriate times as the tutorials progress.
Examples of trigger material for PBL scenarios
Paper based clinical scenarios
Experimental or clinical laboratory data
Photographs
Video clips
Newspaper articles
All or part of an article from a scientific journal
A real or simulated patient
A family tree showing an inherited disorder
PBL tutorial process
Step 1—Identify and clarify unfamiliar terms presented in the scenario; scribe lists those that remain unexplained after discussion
Step 2—Define the problem or problems to be discussed; students may have different views on the issues, but all should be considered; scribe records a list of agreed problems
Step 3—“Brainstorming” session to discuss the problem(s), suggesting possible explanations on basis of prior knowledge; students draw on each other's knowledge and identify areas of incomplete knowledge; scribe records all discussion
Step 4—Review steps 2 and 3 and arrange explanations into tentative solutions; scribe organises the explanations and restructures if necessary
Step 5—Formulate learning objectives; group reaches consensus on the learning objectives; tutor ensures learning objectives are focused, achievable, comprehensive, and appropriate
Step 6—Private study (all students gather information related to each learning objective)
Step 7—Group shares results of private study (students identify their learning resources and share their results); tutor checks learning and may assess the group
The role of the tutor is to facilitate the proceedings (helping the chair to maintain group dynamics and moving the group through the task) and to ensure that the group achieves appropriate learning objectives in line with those set by the curriculum design team. The tutor may need to take a more active role in step 7 of the process to ensure that all the students have done the appropriate work and to help the chair to suggest a suitable format for group members to use to present the results of their private study. The tutor should encourage students to check their understanding of the material. He or she can do this by encouraging the students to ask open questions and ask each other to explain topics in their own words or by the use of drawings and diagrams.
PBL in curriculum design
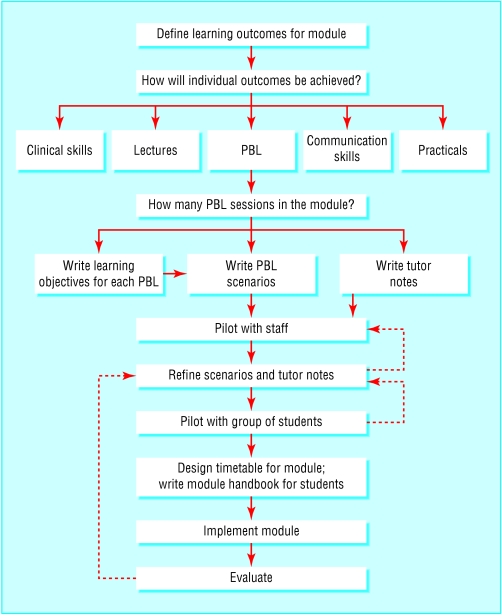
PBL may be used either as the mainstay of an entire curriculum or for the delivery of individual courses. In practice, PBL is usually part of an integrated curriculum using a systems based approach, with non-clinical material delivered in the context of clinical practice. A module or short course can be designed to include mixed teaching methods (including PBL) to achieve the learning outcomes in knowledge, skills, and attitudes. A small number of lectures may be desirable to introduce topics or provide an overview of difficult subject material in conjunction with the PBL scenarios. Sufficient time should be allowed each week for students to do the self directed learning required for PBL.
Writing PBL scenarios
PBL is successful only if the scenarios are of high quality. In most undergraduate PBL curriculums the faculty identifies learning objectives in advance. The scenario should lead students to a particular area of study to achieve those learning objectives.
How to create effective PBL scenarios*
Learning objectives likely to be defined by the students after studying the scenario should be consistent with the faculty learning objectives
Problems should be appropriate to the stage of the curriculum and the level of the students' understanding
Scenarios should have sufficient intrinsic interest for the students or relevance to future practice
Basic science should be presented in the context of a clinical scenario to encourage integration of knowledge
Scenarios should contain cues to stimulate discussion and encourage students to seek explanations for the issues presented
The problem should be sufficiently open, so that discussion is not curtailed too early in the process
Scenarios should promote participation by the students in seeking information from various learning resources
*Adapted from Dolmans et al. Med Teacher 1997;19:185-9
Staff development
Introducing PBL into a course makes new demands on tutors, requiring them to function as facilitators for small group learning rather than acting as providers of information. Staff development is essential and should focus on enabling the PBL tutors to acquire skills in facilitation and in management of group dynamics (including dysfunctional groups).
Tutors should be also given information about the institution's educational strategy and curriculum programme so that they can help students to understand the learning objectives of individual modules in the context of the curriculum as a whole. Methods of assessment and evaluation should be described, and time should be available to discuss anxieties.
Advantages and disadvantages of PBL
| Advantages of PBL | Disadvantages of PBL |
|---|---|
| Student centred PBL—It fosters | Tutors who can't “teach”—Tutors |
| active learning, improved understanding, and retention and development of lifelong learning skills | enjoy passing on their own knowledge and understanding so may find PBL facilitation difficult and frustrating |
| Generic competencies—PBL allows | Human resources—More staff |
| students to develop generic skills and attitudes desirable in their future practice | have to take part in the tutoring process |
| Integration—PBL facilitates an | Other resources—Large numbers |
| integrated core curriculum | of students need access to the same library and computer resources simultaneously |
| Motivation—PBL is fun for students | Role models—Students may be |
| and tutors, and the process requires all students to be engaged in the learning process | deprived access to a particular inspirational teacher who in a traditional curriculum would deliver lectures to a large group |
| “Deep” learning—PBL fosters deep | Informationoverload—Students |
| learning (students interact with learning materials, relate concepts to everyday activities, and improve their understanding) | may be unsure how much self directed study to do and what information is relevant and useful |
| Constructivist approach—Students | |
| activate prior knowledge and build on existing conceptual knowledge frameworks |
Staff may feel uncertain about facilitating a PBL tutorial for a subject in which they do not themselves specialise. Subject specialists may, however, be poor PBL facilitators as they are more likely to interrupt the process and revert to lecturing. None the less, students value expertise, and the best tutors are subject specialists who understand the curriculum and have excellent facilitation skills. However, enthusiastic non-specialist tutors who are trained in facilitation, know the curriculum, and have adequate tutor notes, are good PBL tutors.
Assessment of PBL
Student learning is influenced greatly by the assessment methods used. If assessment methods rely solely on factual recall then PBL is unlikely to succeed in the curriculum. All assessment schedules should follow the basic principles of testing the student in relation to the curriculum outcomes and should use an appropriate range of assessment methods.
Further reading
Davis MH, Harden RM. AMEE medical education guide number 15: problem-based learning: a practical guide. Med Teacher 1999;21:130-40
Norman GR, Schmidt HG. Effectiveness of problem-based learning curricula: theory, practice and paper darts. Med Educ 2000;34:721-8
Albanese M. Problem based learning: why curricula are likely to show little effect on knowledge and clinical skills. Med Educ 2000;34:729-38
Assessment of students' activities in their PBL groups is advisable. Tutors should give feedback or use formative or summative assessment procedures as dictated by the faculty assessment schedule. It is also helpful to consider assessment of the group as a whole. The group should be encouraged to reflect on its PBL performance including its adherence to the process, communication skills, respect for others, and individual contributions. Peer pressure in the group reduces the likelihood of students failing to keep up with workload, and the award of a group mark—added to each individual's assessment schedule— encourages students to achieve the generic goals associated with PBL.
Conclusion
PBL is an effective way of delivering medical education in a coherent, integrated programme and offers several advantages over traditional teaching methods. It is based on principles of adult learning theory, including motivating the students, encouraging them to set their own learning goals, and giving them a role in decisions that affect their own learning.
Predictably, however, PBL does not offer a universal panacea for teaching and learning in medicine, and it has several well recognised disadvantages. Traditional knowledge based assessments of curriculum outcomes have shown little or no difference in students graduating from PBL or traditional curriculums. Importantly, though, students from PBL curriculums seem to have better knowledge retention. PBL also generates a more stimulating and challenging educational environment, and the beneficial effects from the generic attributes acquired through PBL should not be underestimated.
Figure.
The group learning process: acquiring desirable learning skills
Figure.
Roles of participants in a PBL tutorial
Figure.
Designing and implementing a curriculum module using PBL supported by other teaching methods
Figure.

A dysfunctional group: a dominant character may make it difficult for other students to be heard
Acknowledgments
Christ and St John with Angels by Peter Paul Rubens is from the collection of the Earl of Pembroke/BAL.The Mad Hatter's Tea Party is by John Tenniel.
Footnotes
The ABC of learning and teaching in medicine is edited by Peter Cantillon, senior lecturer in medical informatics and medical education, National University of Ireland, Galway, Republic of Ireland; Linda Hutchinson, director of education and workforce development and consultant paediatrician, University Hospital Lewisham; and Diana F Wood, deputy dean for education and consultant endocrinologist, Barts and the London, Queen Mary's School of Medicine and Dentistry, Queen Mary, University of London. The series will be published as a book in late spring.