Abstract
目的
测量健康人椎旁肌影像学参数,阐明椎旁肌特点及变化规律,探究椎旁肌退变的影响因素。
方法
2020年2月—11月前瞻性招募82名健康志愿者,男36名,女46名;年龄21~75岁,平均48.0岁。身高150~183 cm,平均165.6 cm;体质量43~100 kg,平均65.4 kg;身体质量指数(body mass index,BMI) 16.7~32.4 kg/m2,平均23.7 kg/m2。采用MRI测量L3、L4、L5 3个层面椎旁肌(多裂肌、竖脊肌和腰大肌)影像学参数,包括相对总横截面积(relative total cross-sectional area,rtCSA)、相对脂肪横截面积(relative fatty cross-sectional area,rfCSA)、相对信号强度(relative signal intensity,rSI)及脂肪浸润比(fatty infiltration,FI)。比较不同性别以及不同测量层面椎旁肌参数差异;通过Pearson或Spearman相关分析探究椎旁肌参数与年龄、身高、体质量、BMI之间的关系。
结果
从L3至L5层面,多裂肌、腰大肌rtCSA、rfCSA及竖脊肌rfCSA逐渐增加,竖脊肌rtCSA逐渐减小;各椎旁肌的FI、rSI均逐渐增加。L4、L5层面各椎旁肌各参数与L3层面比较差异均有统计学意义(P<0.05);而L4层面与L5层面比较,多裂肌rtCSA、rfCSA,竖脊肌rtCSA、FI、rSI,以及腰大肌rtCSA、rfCSA、FI差异有统计学意义(P<0.05)。女性各腰椎层面多裂肌rfCSA和FI、竖脊肌FI、腰大肌FI高于男性,腰大肌rtCSA低于男性(P<0.05)。年龄与各椎旁肌rtCSA成负相关(P<0.05),与各椎旁肌FI及多裂肌和竖脊肌rfCSA、rSI成正相关(P<0.05)。身高与各椎旁肌rfCSA、FI成负相关(P<0.05)。
结论
沿脊柱轴线从头端至尾端,椎旁肌退变程度逐渐增加;椎旁肌退变和年龄、身高、性别相关,体质量、BMI和椎旁肌退变关系需要进一步研究。
Keywords: 多裂肌, 竖脊肌, 腰大肌, 椎旁肌退变, 健康人
Abstract
Objective
To measure the paraspinal muscle parameters, explore the characteristics of paraspinal muscles, and investigate the influence factors of paraspinal muscle degeneration in healthy people.
Methods
Eighty-two healthy Chinese people were prospectively recruited between February 2020 and November 2020, including 36 males and 46 females. The age ranged from 21 to 75 years, with a mean of 48.0 years. The height ranged from 150 to 183 cm, with a mean of 165.6 cm. The body mass ranged from 43 to 100 kg, with a mean of 65.4 kg. The body mass index (BMI) ranged from 16.7 to 32.4 kg/m2, with a mean of 23.7 kg/m2. Parameters of the paraspinal muscles (multifidus muscle, erector spinae muscle, and psoas major muscle) at L3, L4, and L5 levels were measured by MRI, including the relative total cross-sectional area (rtCSA), relative fatty cross-sectional area (rfCSA), relative signal intensity (rSI), and fatty infiltration (FI). The differences of paraspinal muscle parameters at different genders and different measurement levels were compared; Pearson or Spearman correlation analysis was used to explore the relationship between paraspinal muscle parameters and age, height, body mass, BMI.
Results
From L3 to L5 level, the rtCSA and rfCSA of multifidus muscle and psoas major muscle as well as the rfCSA of erector spinae muscle increased, while rtCSA of erector spinae muscle decreased. The FI and rSI of paraspinal muscles increased gradually. The parameters of paraspinal muscles at L4 and L5 levels were significantly different from those at L3 levels (P<0.05). There were significant differences in rtCSA and rfCSA of multifidus muscle, rtCSA, FI, and rSI of erector spinae muscle as well as rtCSA, rfCSA, and FI of psoas major muscle between L4 and L5 levels (P<0.05). Compared with males, the rfCSA and FI of multifidus muscle, FI of erector spinae muscle, and FI of psoas major muscle were significantly higher in females, while the rtCSA of psoas major muscle was significantly lower (P<0.05). Age was significantly negatively correlated with rtCSA of paraspinal muscles (P<0.05), but significantly positively correlated with FI of paraspinal muscles, rfCSA and rSI of multifidus and erector spinae muscles (P<0.05). Height was significantly negatively correlated with rfCSA and FI of paraspinal muscles (P<0.05).
Conclusion
The degree of paraspinal muscle degeneration increases gradually along the spine axis from head to tail. Paraspinal muscle degeneration is related to age, height, and gender. The relationship between the body mass, BMI and paraspinal muscle degeneration needs further study.
Keywords: Multifidus muscle, erector spinae muscle, psoas major muscle, paraspinal muscle degeneration, healthy people
脊柱的稳定性依赖于主动亚系统、被动亚系统和神经亚系统的整体调节[1]。作为主动亚系统的组成成分,椎旁肌肉在维持脊柱稳定性中的作用不容忽视。近年来,很多研究结果表明椎旁肌肉量减少、脂肪含量增加和多种腰椎疾病发生密切相关[2-6]。Wan等[7]发现慢性腰背痛患者患侧多裂肌及竖脊肌横截面积与健侧相比明显减小;Danneels等[8]比较了慢性腰背痛患者和健康人椎旁肌CT表现,发现前者L4水平多裂肌横截面积明显较小。在腰椎间盘突出症等退变性疾病的研究中,椎旁肌退变程度与其症状、预后也紧密相关[9-11]。
椎旁肌的作用受到越来越多学者关注,但仅有少数研究报道健康人椎旁肌的特点及变化规律。Crawford等[12]通过分析80名健康人资料,发现椎旁肌脂肪浸润程度随年龄增长而增加,女性及下腰椎水平椎旁肌受影响程度最大。但是其研究纳入人群最大年龄为62岁,缺少老年人相关资料,而老年人恰恰是腰椎退变性疾病的好发人群。Dahlqvist等[13]分析了53名志愿者颈、胸、腰椎旁肌和大腿肌肉情况,也发现年龄及性别会影响腰椎旁肌的脂肪浸润程度。目前健康人椎旁肌研究主要以白种人为主,而关于中国健康人椎旁肌特点及变化规律的研究很少。种族差异可能会导致椎旁肌特点存在差异,因此探究中国健康人椎旁肌特点和变化规律具有重要参考价值。
近年有研究采用定量CT方法测量我国女性人群的椎旁肌参数,发现椎旁肌脂肪浸润率和年龄及身体质量指数(body mass index,BMI)相关[14],但缺乏我国男性人群数据。也有研究[15]通过MRI测量椎旁肌脂肪浸润比,发现其受年龄、性别等因素影响;但并未测量椎旁肌横截面积等参数,对椎旁肌评估不够全面。影像学方法评估椎旁肌的退变情况,主要表现为椎旁肌横截面积减小、密度下降或脂肪浸润程度增加[16-19]。目前尚缺乏全面评估中国健康人椎旁肌特点的研究。
鉴于此,本研究通过全面测量健康人椎旁肌影像学参数,总结椎旁肌的特点及各腰椎层面椎旁肌参数变化规律,探究椎旁肌退变的影响因素,为开展国人椎旁肌退变相关研究提供参考。
1. 资料与方法
1.1. 研究对象
本研究为横断面研究,2020年2月—11月于北京地区前瞻性招募健康志愿者。纳入标准:① 年龄18~80岁;② 无脊柱疾病史;③ 无脊柱手术史;④ 过去3个月无腰背痛、腰背部外伤史等。排除标准:① 伴有神经肌肉疾病。② 有MRI相关禁忌证。③ 无法完成腰背部肌肉耐力测试,该测试要求志愿者俯卧于检查床上,在下腹部放置一无弹性垫子或枕头,高度10 cm左右;志愿者需将胸部或上半身尽量抬高,双上肢和身体轴线保持平行,双下肢保持伸直,而颈部处于水平位置[20]。
共82名健康志愿者符合选择标准纳入研究。其中男36名,女46名;年龄21~75岁,平均48.0岁。身高150~183 cm,平均165.6 cm;体质量43~100 kg,平均65.4 kg;BMI 16.7~32.4 kg/m2,平均23.7 kg/m2。18人有规律锻炼习惯,64人无规律锻炼习惯。男性志愿者身高、体质量及BMI显著大于女性志愿者,差异有统计学意义(P<0.05);而年龄及是否规律锻炼男女性之间比较差异无统计学意义(P>0.05)。见表1。
表 1.
Comparison of general condition of male and female healthy volunteers
男女性健康志愿者一般情况比较
| 指标 Indicator |
男性(n=36) Male (n=36) |
女性(n=46) Female (n=46) |
统计量 Statistical value |
P值 P value |
| 年龄(x±s,岁) | 47.3±17.1 | 48.5±17.5 | t=−0.310 | 0.757 |
| 身高(x±s,cm) | 173.2±6.6 | 159.6±5.4 | t=10.282 | <0.001 |
| 体质量(x±s,kg) | 75.1±12.2 | 57.8±8.7 | t=7.504 | <0.001 |
| BMI(x±s,kg/m2) | 25.0±3.2 | 22.7±3.5 | t=2.964 | 0.004 |
| 规律锻炼(有/无,例) | 6/30 | 12/34 | χ2=1.046 | 0.422 |
1.2. 椎旁肌参数及测量方法
所有志愿者均进行腰椎MRI检查,检查时嘱志愿者保持仰卧位,双下肢伸直,腰椎处于自然中立位,检查过程中身体保持平静状态。检查仪器为美国GE公司的Signa HDxt 3.0T,测试序列包括T2加权像(重复时间2 500~4 000 ms,回波时间 80~120 ms),层厚3 mm,每个层面间隙3 mm;扫描及测量层面(以L3~L5层面为主)平行于腰椎椎体下终板,每个志愿者均测量L3、L4、L5 3个层面的影像学参数。
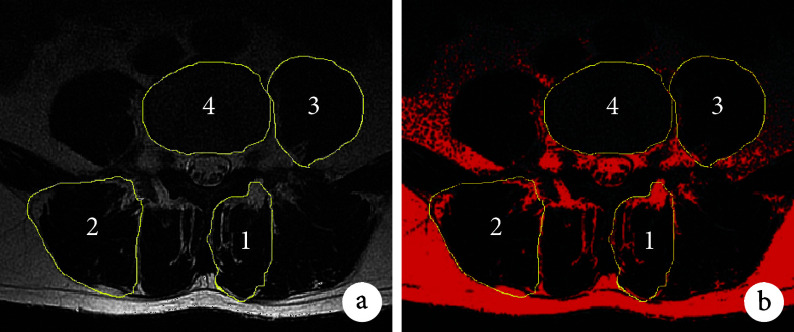
应用Image J软件测量腰椎MRI T2加权像上椎旁肌,包括多裂肌、竖脊肌及腰大肌的相关参数(各肌肉均进行双侧测量)。测量参数:① 肌肉总横截面积(total cross-sectional area,tCSA):横断面上肌肉的总面积;② 脂肪横截面积(fatty cross-sectional area,fCSA):横断面上除纯肌肉以外的面积,通过阈值技术测量(图1);③ 脂肪浸润比(fatty infiltration,FI):横断面上脂肪面积与总面积的比值(fCSA/tCSA);④ 肌肉信号强度(signal intensity,SI):MRI上肌肉的平均信号值;⑤ 相应层面皮下脂肪SI。为了减小个体身高、体质量、体型对椎旁肌参数的影响,采用肌肉相对总横截面积(relative total cross-sectional area,rtCSA;tCSA与相应层面椎体面积的比值)、相对脂肪横截面积(relative fatty cross-sectional area,rfCSA;fCSA与相应层面椎体面积的比值)以及相对信号强度(relative signal intensity,rSI;肌肉SI与相应层面皮下脂肪SI的比值)进行分析。
图 1.
Measurements of paraspinal muscle parameters
椎旁肌相关参数测量示意图
1:多裂肌 2:竖脊肌 3:腰大肌 4:椎体 a. 肌肉总横截面积;b. 脂肪横截面积(红色部分示脂肪)
1: Multifidus muscle 2: Erector spinae muscle 3: Psoas major muscle 4: Vertebrae a. Total cross-sectional area of paraspinal muscle; b. Fatty cross-sectional area of paraspinal muscle (the red part indicated fat area)
1.3. 统计学方法
采用SPSS24.0统计软件进行分析。计量资料经Kolmogorov-Smirnov正态性检验,符合正态分布的数据以均数±标准差表示,不同腰椎层面间各参数比较采用单因素方差分析,两两比较采用LSD检验;不同性别之间各参数比较采用独立样本t检验。不符合正态分布的数据以M(Q1,Q3)表示,不同腰椎层面间各参数比较采用Kruskal-Wallis检验,两两比较采用Mann-Whitney U检验;不同性别之间各参数比较采用Mann-Whitney U检验。通过Pearson或Spearman相关分析椎旁肌参数与年龄、身高、体质量、BMI之间的关系;检验水准取双侧α=0.05。
2. 结果
2.1. 不同腰椎层面椎旁肌参数比较
从L3至L5层面,多裂肌、腰大肌rtCSA、rfCSA及竖脊肌rfCSA逐渐增加,竖脊肌rtCSA逐渐减小;各椎旁肌的FI、rSI均逐渐增加,说明越接近脊柱轴线尾端,椎旁肌退变程度越重。L4、L5层面各椎旁肌各参数与L3层面比较差异均有统计学意义(P<0.05)。而L4层面与L5层面比较,多裂肌rtCSA、rfCSA,竖脊肌rtCSA、FI、rSI,以及腰大肌rtCSA、rfCSA、FI差异均有统计学意义(P<0.05);其余参数差异无统计学意义(P>0.05)。见表2、3。
表 2.
Comparison of paraspinal muscle parameters at different lumbar levels(n=82)
不同腰椎层面椎旁肌参数比较(n=82)
| 指标 Indicator |
L3 | L4 | L5 |
P值 P value |
| 多裂肌 | ||||
| rtCSA [M(Q1,Q3)] | 0.98(0.84,1.13) | 1.36(1.16,1.59) | 1.60(1.40,1.92) | <0.001 |
| rfCSA [M(Q1,Q3)] | 0.19(0.13,0.27) | 0.31(0.23,0.45) | 0.44(0.31,0.52) | <0.001 |
| FI [M(Q1,Q3)] | 0.21(0.14,0.27) | 0.25(0.18,0.31) | 0.25(0.20,0.32) | 0.001 |
| rSI(x±s) | 0.38±0.09 | 0.42±0.12 | 0.44±0.11 | 0.001 |
| 竖脊肌 | ||||
| rtCSA(x±s) | 2.74±0.45 | 2.46±0.41 | 1.71±0.56 | <0.001 |
| rfCSA [M(Q1,Q3)] | 0.44(0.31,0.58) | 0.55(0.44,0.74) | 0.57(0.45,0.70) | <0.001 |
| FI [M(Q1,Q3)] | 0.16(0.13,0.22) | 0.24(0.17,0.31) | 0.35(0.26,0.42) | <0.001 |
| rSI [M(Q1,Q3)] | 0.34(0.31,0.41) | 0.40(0.36,0.47) | 0.48(0.43,0.55) | <0.001 |
| 腰大肌 | ||||
| rtCSA [M(Q1,Q3)] | 1.42(1.16,1.71) | 2.11(1.70,2.41) | 2.25(1.85,2.71) | <0.001 |
| rfCSA [M(Q1,Q3)] | 0.15(0.10,0.19) | 0.23(0.18,0.31) | 0.35(0.27,0.42) | <0.001 |
| FI [M(Q1,Q3)] | 0.10(0.07,0.13) | 0.12(0.09,0.16) | 0.15(0.12,0.18) | <0.001 |
| rSI [M(Q1,Q3)] | 0.29(0.24,0.34) | 0.32(0.25,0.37) | 0.33(0.27,0.38) | 0.005 |
表 3.
Pairwise comparison of paraspinal muscle parameters at different lumbar levels
不同腰椎层面椎旁肌参数两两比较
| 指标 Indicator |
L3 vs L4 | L4 vs L5 | L3 vs L5 | |||||
| 效应值(95%CI) Effect value (95%CI) |
P值 P value |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
|||
| 多裂肌 | ||||||||
| rtCSA | MD=−0.384(−0.475,−0.293) | <0.001 | MD=−0.301(−0.430,−0.171) | <0.001 | MD=−0.685(−0.804,−0.566) | <0.001 | ||
| rfCSA | MD=−0.132(−0.190,−0.075) | <0.001 | MD=−0.101(−0.172,−0.030) | <0.001 | MD=−0.234(−0.298,−0.170) | <0.001 | ||
| FI | MD=−0.036(−0.069,−0.004) | 0.013 | MD=−0.014(−0.053,0.026) | 0.281 | MD=−0.050(−0.083,−0.018) | <0.001 | ||
| rSI | MD=−0.041(−0.073,−0.009) | 0.013 | MD=−0.023(−0.055,0.010) | 0.168 | MD=−0.064(−0.096,−0.031) | <0.001 | ||
| 竖脊肌 | ||||||||
| rtCSA | MD=0.282(0.119,0.444) | <0.001 | MD=0.744(0.559,0.929) | <0.001 | MD=1.026(0.836,1.216) | <0.001 | ||
| rfCSA | MD=−0.130(−0.204,−0.056) | 0.001 | MD=0.003(−0.071,0.077) | 0.552 | MD=−0.127(−0.201,−0.053) | <0.001 | ||
| FI | MD=−0.073(−0.110,−0.036) | <0.001 | MD=−0.109(−0.151,−0.067) | <0.001 | MD=−0.182(−0.219,−0.146) | <0.001 | ||
| rSI | MD=−0.058(−0.086,−0.029) | <0.001 | MD=−0.076(−0.105,−0.048) | <0.001 | MD=−0.134(−0.163,−0.105) | <0.001 | ||
| 腰大肌 | ||||||||
| rtCSA | MD=−0.623(−0.823,−0.423) | <0.001 | MD=−0.218(−0.450,−0.013) | 0.024 | MD=−0.841(−1.049,−0.634) | <0.001 | ||
| rfCSA | MD=−0.103(−0.140,−0.065) | <0.001 | MD=−0.093(−0.139,−0.047) | <0.001 | MD=−0.195(−0.235,−0.156) | <0.001 | ||
| FI | MD=−0.018(−0.034,−0.002) | 0.023 | MD=−0.027(−0.043,−0.011) | <0.001 | MD=−0.045(−0.061,−0.029) | 0.001 | ||
| rSI | MD=−0.046(−0.086,−0.006) | 0.036 | MD=0.002(−0.038,0.042) | 0.296 | MD=−0.044(−0.084,−0.004) | <0.001 | ||
2.2. 不同性别椎旁肌参数比较
不同腰椎层面椎旁肌参数比较示,女性各腰椎层面的多裂肌rfCSA和FI、竖脊肌FI、腰大肌FI高于男性,腰大肌rtCSA低于男性;此外,女性L3层面多裂肌rSI、L5层面竖脊肌rfCSA、rSI高于男性,L3层面竖脊肌rtCSA低于男性;上述差异均有统计学意义(P<0.05)。其余各腰椎层面各椎旁肌参数男女性之间比较差异均无统计学意义(P>0.05)。见表4。
表 4.
Comparison of paraspinal muscle parameters between males and females on different lumbar levels
各腰椎层面椎旁肌参数在不同性别间比较
| 指标 Indicator |
L3 | |||
| 男性(n=36) Males (n=36) |
女性(n=46) Females (n=46) |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
|
| 多裂肌 | ||||
| rtCSA | 1.00±0.21 | 0.98±0.19 | MD=–0.013(–0.075,0.101) | 0.768 |
| rfCSA | 0.16(0.12,0.21) | 0.22(0.14,0.30) | MD=−0.079(−0.133,−0.024) | 0.006 |
| FI | 0.17(0.12,0.24) | 0.25(0.16,0.30) | MD=−0.074(−0.120,−0.029) | 0.003 |
| rSI | 0.35±0.07 | 0.40±0.10 | MD=−0.047(−0.085,−0.009) | 0.016 |
| 竖脊肌 | ||||
| rtCSA | 2.95±0.44 | 2.57±0.38 | MD=0.379(0.198,0.559) | <0.001 |
| rfCSA | 0.43±0.15 | 0.50±0.24 | MD=−0.065(−0.155,0.025) | 0.154 |
| FI | 0.15(0.11,0.19) | 0.18(0.13,0.23) | MD=−0.044(−0.078,−0.010) | 0.043 |
| rSI | 0.34(0.30,0.40) | 0.35(0.31,0.43) | MD=−0.020(−0.056,0.157) | 0.350 |
| 腰大肌 | ||||
| rtCSA | 1.56(1.35,1.83) | 1.34(1.04,1.53) | MD=0.300(0.109,0.490) | 0.005 |
| rfCSA | 0.13(0.09,0.18) | 0.17(0.10,0.20) | MD=−0.028(−0.061,0.005) | 0.096 |
| FI | 0.08(0.07,0.11) | 0.11(0.09,0.17) | MD=−0.042(−0.064,−0.021) | 0.001 |
| rSI | 0.28±0.06 | 0.30±0.08 | MD=−0.016(−0.047,−0.015) | 0.337 |
| 指标 Indicator |
L4 | |||
| 男性(n=36) Males (n=36) |
女性(n=46) Females (n=46) |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
|
| 多裂肌 | ||||
| rtCSA | 1.34±0.25 | 1.40±0.29 | MD=−0.064(−0.187,0.058) | 0.298 |
| rfCSA | 0.28(0.20,0.37) | 0.35(0.26,0.49) | MD=−0.099(−0.172,−0.025) | 0.009 |
| FI | 0.22±0.08 | 0.28±0.12 | MD=−0.062(−0.109,−0.015) | 0.011 |
| rSI | 0.40±0.10 | 0.44±0.13 | MD=−0.042(−0.091,0.007) | 0.090 |
| 竖脊肌 | ||||
| rtCSA | 2.55±0.47 | 2.38±0.36 | MD=0.174(−0.007,0.354) | 0.059 |
| rfCSA | 0.54(0.39,0.60) | 0.56(0.45,0.81) | MD=−0.116(−0.236,0.003) | 0.130 |
| FI | 0.21(0.16,0.25) | 0.25(0.18,0.33) | MD=−0.064(−0.113,−0.015) | 0.012 |
| rSI | 0.39±0.09 | 0.43±0.11 | MD=−0.034(−0.079,0.109) | 0.135 |
| 腰大肌 | ||||
| rtCSA | 2.32±0.64 | 1.90±0.49 | MD=0.420(0.172,0.669) | 0.002 |
| rfCSA | 0.22(0.17,0.29) | 0.24(0.19,0.33) | MD=−0.034(−0.086,0.019) | 0.204 |
| FI | 0.10(0.07,0.13) | 0.14(0.11,0.18) | MD=−0.040(−0.063,−0.017) | <0.001 |
| rSI | 0.31(0.24,0.36) | 0.33(0.25,0.37) | MD=−0.030(−0.068,0.127) | 0.531 |
| 指标 Indicator |
L5 | |||
| 男性(n=36) Males (n=36) |
女性(n=46) Females (n=46) |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
|
| 多裂肌 | ||||
| rtCSA | 1.58(1.31,1.80) | 1.63(1.44,2.02) | MD=−0.102(−0.277,0.072) | 0.201 |
| rfCSA | 0.33(0.26,0.45) | 0.47(0.36,0.61) | MD=−0.151(−0.231,−0.071) | <0.001 |
| FI | 0.23±0.07 | 0.30±0.11 | MD=−0.076(−0.117,−0.035) | <0.001 |
| rSI | 0.42±0.09 | 0.46±0.12 | MD=−0.045(−0.091,0.001) | 0.054 |
| 竖脊肌 | ||||
| rtCSA | 1.60±0.57 | 1.80±0.54 | MD=−0.198(−0.442,0.046) | 0.110 |
| rfCSA | 0.48(0.39,0.63) | 0.64(0.54,0.76) | MD=−0.193(−0.290,−0.096) | <0.001 |
| FI | 0.32±0.10 | 0.39±0.11 | MD=−0.063(−0.111,−0.016) | 0.009 |
| rSI | 0.46±0.08 | 0.51±0.11 | MD=−0.044(−0.086,−0.003) | 0.036 |
| 腰大肌 | ||||
| rtCSA | 2.59±0.65 | 2.08±0.53 | MD=0.505(0.246,0.765) | <0.001 |
| rfCSA | 0.34±0.12 | 0.35±0.13 | MD=−0.009(−0.064,0.047) | 0.756 |
| FI | 0.14±0.04 | 0.17±0.05 | MD=−0.035(−0.056,−0.015) | 0.001 |
| rSI | 0.33±0.07 | 0.34±0.10 | MD=−0.011(−0.050,0.028) | 0.589 |
考虑到单一层面椎旁肌参数可能无法全面反映椎旁肌整体情况,遂采用各腰椎层面椎旁肌参数均值来反映椎旁肌整体情况,并比较了不同性别间椎旁肌参数的差异。结果显示,女性多裂肌rfCSA、FI和rSI,竖脊肌rfCSA和FI,以及腰大肌FI高于男性,腰大肌rtCSA低于男性,差异均有统计学意义(P<0.05);其余各椎旁肌参数男女性之间比较差异均无统计学意义(P>0.05)。见表5。
表 5.
Comparison of mean value of paraspinal muscle parameters of each lumbar level between males and females
各腰椎层面椎旁肌参数均值在不同性别间比较
| 指标 Indicator |
总体 Total |
男性(n=36) Males (n=36) |
女性(n=46) Females (n=46) |
效应值(95%CI) Effect value (95%CI) |
P值 P value |
| 多裂肌 | |||||
| rtCSA | 1.35±0.27 | 1.32±0.26 | 1.37±0.27 | MD=−0.005(−0.169,0.067) | 0.389 |
| rfCSA | 0.32(0.24,0.38) | 0.27(0.19,0.34) | 0.35(0.26,0.45) | MD=−0.110(−0.174,−0.045) | 0.001 |
| FI | 0.24(0.18,0.29) | 0.21(0.15,0.27) | 0.26(0.20,0.32) | MD=−0.071(−0.112,−0.029) | 0.003 |
| rSI | 0.41±0.10 | 0.39±0.08 | 0.43±0.11 | MD=−0.045(−0.087,−0.003) | 0.037 |
| 竖脊肌 | |||||
| rtCSA | 2.30±0.39 | 2.37±0.43 | 2.25±0.35 | MD=0.118(−0.053,0.289) | 0.174 |
| rfCSA | 0.51(00.43,0.67) | 0.45(0.40,0.60) | 0.56(0.45,0.71) | MD=−0.125(−0.207,−0.043) | 0.007 |
| FI | 0.25(0.21,0.29) | 0.22(0.18,0.26) | 0.27(0.23,0.32) | MD=−0.057(−0.094,−0.020) | 0.003 |
| rSI | 0.42±0.09 | 0.40±0.07 | 0.43±0.09 | MD=−0.033(−0.070,0.005) | 0.087 |
| 腰大肌 | |||||
| rtCSA | 1.89(1.60,2.27) | 2.15(1.77,2.49) | 1.69(1.41,2.20) | MD=0.303(0.024,0.630) | 0.001 |
| rfCSA | 0.24(0.20,0.30) | 0.23(0.18,0.29) | 0.25(0.21,0.31) | MD=−0.024(−0.064,0.017) | 0.313 |
| FI | 0.12(0.10,0.16) | 0.10(0.08,0.12) | 0.14(0.12,0.18) | MD=−0.038(−0.058,−0.018) | <0.001 |
| rSI | 0.31(0.26,0.36) | 0.31(0.26,0.36) | 0.32(0.27,0.37) | MD=0.001(−0.042,0.045) | 0.550 |
2.3. 椎旁肌参数与年龄等因素的关系
年龄与各椎旁肌rtCSA成负相关(P<0.05),与各椎旁肌FI以及多裂肌和竖脊肌rfCSA、rSI成正相关(P<0.05);但与腰大肌rfCSA和rSI无相关性(P>0.05)。
身高与各椎旁肌的rfCSA、FI以及多裂肌和竖脊肌rSI成负相关(P<0.05),与竖脊肌和腰大肌rtCSA成正相关(P<0.05);但与多裂肌rtCSA和腰大肌rSI无相关性(P>0.05)。体质量与竖脊肌和腰大肌rtCSA成正相关(P<0.05),与腰大肌FI成负相关(P<0.05),与其余指标无相关性(P>0.05)。BMI除了与竖脊肌rfCSA和rSI成正相关(P<0.05)外,与其余指标无相关性(P>0.05)。见表6。
表 6.
Correlation analysis of paraspinal muscle parameters with age and other factors
椎旁肌参数与年龄等因素的相关性分析
| 指标 Indicator |
年龄 Age |
身高 Height |
体质量 Body mass |
BMI |
| 多裂肌 | ||||
| rtCSA | r=−0.464,P<0.001 | r=−0.010,P=0.926 | r=0.008,P=0.943 | r=0.024,P=0.832 |
| rfCSA | r=0.409,P<0.001 | r=−0.480,P<0.001 | r=−0.141,P=0.207 | r=0.135,P=0.227 |
| FI | r=0.725,P<0.001 | r=−0.490,P<0.001 | r=−0.137,P=0.218 | r=0.138,P=0.215 |
| rSI | r=0.436,P<0.001 | r=−0.342,P=0.002 | r=−0.037,P=0.740 | r=0.208,P=0.061 |
| 竖脊肌 | ||||
| rtCSA | r=−0.324,P=0.003 | r=0.234,P=0.035 | r=0.272,P=0.013 | r=0.203,P=0.067 |
| rfCSA | r=0.367,P=0.001 | r=−0.355,P=0.001 | r=−0.012,P=0.911 | r=0.246,P=0.026 |
| FI | r=0.530,P<0.001 | r=−0.449,P<0.001 | r=−0.132,P=0.237 | r=0.140,P=0.211 |
| rSI | r=0.406,P<0.001 | r=−0.329,P=0.003 | r=−0.008,P=0.943 | r=0.229,P=0.038 |
| 腰大肌 | ||||
| rtCSA | r=−0.504,P<0.001 | r=0.261,P=0.018 | r=0.295,P=0.007 | r=0.199,P=0.073 |
| rfCSA | r=0.182,P=0.102 | r=−0.249,P=0.024 | r=−0.108,P=0.335 | r=0.015,P=0.896 |
| FI | r=0.590,P<0.001 | r=−0.446,P<0.001 | r=−0.358,P=0.001 | r=−0.151,P=0.175 |
| rSI | r=0.120,P=0.284 | r=−0.156,P=0.160 | r=0.023,P=0.838 | r=0.150,P=0.179 |
3. 讨论
椎旁肌是维持脊柱稳定性的重要结构,其退变在腰椎疾病中的作用受到许多研究者关注[2,4,21]。但既往研究主要集中于欧美人群,关于中国健康人椎旁肌特点的研究较少。仅有的一些研究也因研究对象年龄及性别限制、影像学参数单一而无法全面体现椎旁肌特点。鉴于此,本研究详细描述了不同腰椎水平及整体椎旁肌参数,比较不同性别之间椎旁肌参数差异,探究年龄等因素对椎旁肌退变的影响,为进一步研究健康国人椎旁肌退变提供了一定参考。
3.1. 椎旁肌影像学参数特点及变化规律
本研究通过腰椎MRI检查收集并分析了82名健康国人椎旁肌影像学参数,发现椎旁肌存在一定变化规律。按照脊柱轴线从头端至尾端,多裂肌及腰大肌的rtCSA逐渐增加,而竖脊肌rtCSA逐渐减小。Menezes-Reis等[22]前瞻性招募了93名志愿者,年龄为20~40岁,通过分析其椎旁肌参数,发现从头端至尾端多裂肌横截面积逐渐增加,而竖脊肌横截面积逐渐减小,本研究结果与其一致。Hyun等[23]在研究退变性腰椎后凸患者椎旁肌参数时纳入了20名健康志愿者,其中19名为女性,研究了多裂肌及竖脊肌相对横截面积的变化情况,本研究结果与其相似。尽管本研究纳入人群年龄分布、性别比例与上述研究存在较大差异,但不同层面椎旁肌横截面积变化规律展示出一定相似性。
此外,多裂肌、竖脊肌和腰大肌的FI及rSI从头端至尾端逐渐增加。相较于L3层面,L4、L5层面多裂肌、竖脊肌及腰大肌的FI及rSI均存在显著性差异;而L4层面与L5层面相比,竖脊肌的FI以及rSI也明显不同。这可能与既往研究提出的“悬臂假说”相关[24]。脊柱是固定在骶骨骨盆上的悬臂,越接近骶骨骨盆所承受的负荷越大[25],超出生理承受范围负荷会导致肌肉脂肪化。Menezes-Reis等[22]的研究也发现竖脊肌的脂肪比例从L3至L5层面逐渐增加,多裂肌L5层面的脂肪比例明显高于L3和L4层面,但其并未发现L3与L4层面多裂肌脂肪比例存在明显差异。我们的研究结果与之相比存在一定差异,究其原因可能与纳入人群年龄、测量方法不同相关。本研究纳入人群年龄高于Menezes-Reis等的研究,而既往研究显示40~60岁人群椎旁肌FI会显著增加[15],纳入人群年龄差异可能导致退变程度存在差异;测量方法上,本研究选取MRI T2加权像进行测量,而Menezes-Reis等采用T1加权像,测量选取的层面也略有差异。但值得注意的是,椎旁肌的FI及rSI整体呈现出较为一致的变化规律,即头端至尾端椎旁肌的FI及rSI增加,椎旁肌脂肪化逐渐加重,从侧面反映出椎旁肌退变程度逐渐加重。
尽管不同研究纳入人群的人种、性别、年龄及测量方法可能存在差异,但是椎旁肌参数沿脊柱轴线方向的变化规律是一致的,多裂肌及腰大肌rtCSA逐渐增加,而竖脊肌rtCSA逐渐减小,多裂肌、竖脊肌及腰大肌的rfCSA、FI以及rSI均逐渐增加。
本研究及既往文献[2,16-17,21,24]均表明,不同测量平面的椎旁肌参数存在显著差异。对于测量平面的选择,目前暂无统一标准,多数以L3至L5层面为主。我们以L3至L5层面测量椎旁肌参数,保证了研究数据的可比性,能够为后续研究提供更加可靠详细的参考。采用单一层面数据能够准确反映局部椎旁肌情况,而采用L3至L5层面椎旁肌参数均值进行分析,能够体现整体椎旁肌情况。研究者需综合考虑,选取合适的测量方法和测量指标。
3.2. 年龄等因素与椎旁肌退变的关系
既往研究发现年龄[12-13]、性别[16,26]、慢性腰痛[27-28]等因素会影响肌肉组织变化,但是关于健康国人椎旁肌退变的影响因素研究很少。有研究发现椎旁肌FI和年龄及BMI相关[14],但是其研究对象均为女性,并未对男性国人椎旁肌特点进行研究;其仅测量整块椎旁肌参数,而未单独分析多裂肌及竖脊肌的变化情况。为了进一步详细探究椎旁肌退变情况,本研究对正常人椎旁肌退变的影响因素进行分析,发现年龄、性别、BMI等因素和椎旁肌退变存在一定相关性。
年龄和多裂肌及竖脊肌的rtCSA成显著负相关,与多裂肌及竖脊肌的rfCSA、FI及rSI成明显正相关。说明随着年龄增长,多裂肌及竖脊肌肌肉含量明显下降,功能面积减少,脂肪化加重,椎旁肌退变程度增加。Lee等[24]发现,和年轻人相比,中老年人的多裂肌和竖脊肌肌肉密度明显下降;Crawford等[12]研究结果显示多裂肌及竖脊肌的脂肪信号比例和年龄相关,随着年龄增长,多裂肌及竖脊肌的脂肪信号比例逐渐增加,但是多裂肌及竖脊肌的体积和年龄无关。对于腰大肌,本研究发现年龄与其FI成显著正相关,但与其rtCSA成显著负相关,表明随着年龄增长,腰大肌含量下降,脂肪化加重,退变程度增加。Dallaway等[29]通过比较12对老年男性和青年男性发现,老年男性的腰大肌FI显著较高,但是两组肌肉体积无显著差异。尽管不同研究关于年龄和椎旁肌参数关系的结果存在一些差异,但均表明年龄和椎旁肌退变相关,并且随着年龄增长,椎旁肌FI增加,椎旁肌退变程度加重。
此外,我们对不同性别健康人的椎旁肌参数进行分析,结果显示不同性别之间椎旁肌参数存在显著差异。和男性相比,女性的腰大肌rtCSA较小,表明女性腰大肌含量更低;而女性的多裂肌及竖脊肌rfCSA,多裂肌、竖脊肌及腰大肌FI和多裂肌rSI显著较大,提示女性的椎旁肌质量更低、退变程度更重。这与既往研究结果相符。Shahidi等[16]发现女性椎旁肌横截面积比男性小;Schlaeger等[26]通过分析26名青年志愿者资料也发现了相同结果,女性椎旁肌横截面积比男性小,脂肪分数比男性高。这些研究结果提示女性椎旁肌退变程度较男性更加显著。
BMI也是一个潜在影响椎旁肌退变的因素。有研究发现椎旁肌横截面积与BMI成明显正相关[6,26]。我们的研究结果显示BMI与竖脊肌的rfCSA及rSI成显著正相关,而与椎旁肌的rtCSA虽然无显著相关,但也呈现出正相关趋势,与前述研究结果相近。本研究还发现身高与竖脊肌的rtCSA成显著正相关,而Boissière等[30]通过测量整体椎旁肌体积,发现椎旁肌体积和身高相关。尽管测量方法不同,但是结果都反映出身高可能影响椎旁肌含量。身高还与椎旁肌的FI以及rSI成显著负相关,提示身高较高者椎旁肌退变程度可能较低。我们的研究结果还发现,体质量与竖脊肌及腰大肌的rtCSA成显著正相关,体质量较大者椎旁肌含量也较高。为了进一步探究身高、体质量、BMI等因素的影响,需要更大样本量的试验验证本研究结果。
健康志愿者锻炼情况可能影响椎旁肌退变程度。我们根据其是否规律锻炼进行分组比较,结果显示在年龄、性别、身高、体质量、BMI无显著差异的情况下,椎旁肌参数也无显著差异。如何客观统一地量化评价锻炼强度、制定合理有效的锻炼计划有待进一步研究。此外,近来研究发现椎旁肌退变与骨密度相关,Yang等[31]的研究结果显示骨密度与椎旁肌的FI独立相关,而非椎旁肌横截面积;而Han等[32]的研究也发现骨质疏松患者的FI更高。肌肉与骨骼是相辅相成的两部分,对于椎旁肌退变严重者,需注意是否合并骨质疏松;二者之间的关系仍需要深入研究。
3.3. 本研究优势及不足
本研究通过前瞻性招募健康志愿者,分析其椎旁肌影像学参数,全面阐述了健康国人椎旁肌变化特点及影响因素,为进一步开展中国人群椎旁肌相关研究提供了参考。但本研究也存在一些局限和不足。第一,本研究招募人群以北京地区常住人口为主,研究结果可能会受到地域、环境及生活习惯等因素的影响;第二,本研究相较于既往研究样本量已有所扩大,但仍有限,需要进一步扩大样本量验证结果,但;第三,椎旁肌影像学参数均通过手动测量,有一定主观性,但本研究采用方法的一致性已得到相关研究证实,较为可靠[33-35],未来可采用深度学习方法,有望简化椎旁肌参数测量方法;第四,尽管本研究参照既往研究及自身特点制定纳入排除标准,但可能存在未知因素会影响研究结果。
综上述,健康人椎旁肌影像学参数沿脊柱轴线从头端至尾端呈现一定变化规律,多裂肌及腰大肌rtCSA逐渐增加,竖脊肌rtCSA逐渐减小,而多裂肌、竖脊肌和腰大肌的rfCSA、FI以及rSI逐渐增加;沿脊柱轴线从头端至尾端,椎旁肌退变程度逐渐增加;年龄、身高、性别与椎旁肌退变相关,而体质量、BMI和椎旁肌退变的关系需要进一步研究。
利益冲突 在课题研究和文章撰写过程中不存在利益冲突
伦理声明 研究方案经北京大学第三医院医学科学研究伦理委员会批准(M2019400);志愿者均签署知情同意书
作者贡献声明 李危石:提供研究资料,对文章内容作批评性审阅及修改;王伟:研究设计、数据收集整理、统计分析及文章撰写
References
- 1.Panjabi MM The stabilizing system of the spine. Part Ⅰ. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5(4):383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Sun D, Liu P, Cheng J, et al Correlation between intervertebral disc degeneration, paraspinal muscle atrophy, and lumbar facet joints degeneration in patients with lumbar disc herniation. BMC Musculoskelet Disord. 2017;18(1):167. doi: 10.1186/s12891-017-1522-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shafaq N, Suzuki A, Matsumura A, et al Asymmetric degeneration of paravertebral muscles in patients with degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2012;37(16):1398–1406. doi: 10.1097/BRS.0b013e31824c767e. [DOI] [PubMed] [Google Scholar]
- 4.Zotti MGT, Boas FV, Clifton T, et al. Does pre-operative magnetic resonance imaging of the lumbar multifidus muscle predict clinical outcomes following lumbar spinal decompression for symptomatic spinal stenosis? Eur Spine J, 2017, 26(10): 2589-2597.
- 5.Hyun SJ, Kim YJ, Rhim SC Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016;16(9):1095–1101. doi: 10.1016/j.spinee.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Kalichman L, Hodges P, Li L, et al Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur Spine J. 2010;19(7):1136–1144. doi: 10.1007/s00586-009-1257-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wan Q, Lin C, Li X, et al MRI assessment of paraspinal muscles in patients with acute and chronic unilateral low back pain. Br J Radiol. 2015;88(1053):20140546. doi: 10.1259/bjr.20140546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danneels LA, Vanderstraeten GG, Cambier DC, et al CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9(4):266–272. doi: 10.1007/s005860000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gengyu H, Jinyue D, Chunjie G, et al The predictive value of preoperative paraspinal muscle morphometry on complications after lumbar surgery: a systematic review. Eur Spine J. 2022;31(2):364–379. doi: 10.1007/s00586-021-07052-3. [DOI] [PubMed] [Google Scholar]
- 10.Cheng Z, Li Y, Li M, et al Correlation between posterior paraspinal muscle atrophy and lumbar intervertebral disc degeneration in patients with chronic low back pain. Int Orthop. 2023;47(3):793–801. doi: 10.1007/s00264-022-05621-9. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Yuan L, Zeng Y, et al The Difference in paraspinal muscle parameters and the correlation with health-related quality of life among healthy individuals, patients with degenerative lumbar scoliosis and lumbar spinal stenosis. J Pers Med. 2023;13(10):1438. doi: 10.3390/jpm13101438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crawford RJ, Filli L, Elliott JM, et al Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol. 2016;37(4):742–748. doi: 10.3174/ajnr.A4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dahlqvist JR, Vissing CR, Hedermann G, et al Fat replacement of paraspinal muscles with aging in healthy adults. Med Sci Sports Exerc. 2017;49(3):595–601. doi: 10.1249/MSS.0000000000001119. [DOI] [PubMed] [Google Scholar]
- 14.Peng X, Li X, Xu Z, et al Age-related fatty infiltration of lumbar paraspinal muscles: a normative reference database study in 516 Chinese females. Quant Imaging Med Surg. 2020;10(8):1590–1601. doi: 10.21037/qims-19-835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Si F, Wang T, Zang L, et al Characteristics of paraspinal muscle fat infiltration in asymptomatic Chinese adults: a cross-sectional study. Quant Imaging Med Surg. 2023;13(7):4526–4539. doi: 10.21037/qims-22-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahidi B, Parra CL, Berry DB, et al Contribution of lumbar spine pathology and age to paraspinal muscle size and fatty infiltration. Spine (Phila Pa 1976) 2017;42(8):616–623. doi: 10.1097/BRS.0000000000001848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yagi M, Hosogane N, Watanabe K, et al The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J. 2016;16(4):451–458. doi: 10.1016/j.spinee.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 18.Urrutia J, Besa P, Lobos D, et al. Is a single-level measurement of paraspinal muscle fat infiltration and cross-sectional area representative of the entire lumbar spine? Skeletal Radiol, 2018, 47(7): 939-945.
- 19.袁磊, 陈萧霖, 曾岩, 等 退变性腰椎侧凸患者椎旁肌退变与术后近端交界性后凸的相关性研究. 中国脊柱脊髓杂志. 2018;28(5):425–433. [Google Scholar]
- 20.Han G, Wang W, Yue L, et al Age-dependent differences of paraspinal muscle endurance and morphology in chinese community population without chronic low back pain. Global Spine J. 2024;14(1):235–243. doi: 10.1177/21925682221103507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miki T, Naoki F, Takashima H, et al Associations between paraspinal muscle morphology, disc degeneration, and clinical features in patients with lumbar spinal stenosis. Prog Rehabil Med. 2020;5:20200015. doi: 10.2490/prm.20200015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menezes-Reis R, Bonugli GP, Salmon CEG, et al Relationship of spinal alignment with muscular volume and fat infiltration of lumbar trunk muscles. PLoS One. 2018;13(7):e0200198. doi: 10.1371/journal.pone.0200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hyun SJ, Bae CW, Lee SH, et al Fatty degeneration of the paraspinal muscle in patients with degenerative lumbar kyphosis: A new evaluation method of quantitative digital analysis using MRI and CT scan. Clin Spine Surg. 2016;29(10):441–447. doi: 10.1097/BSD.0b013e3182aa28b0. [DOI] [PubMed] [Google Scholar]
- 24.Lee SH, Park SW, Kim YB, et al The fatty degeneration of lumbar paraspinal muscles on computed tomography scan according to age and disc level. Spine J. 2017;17(1):81–87. doi: 10.1016/j.spinee.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Sander D, Tian Z, Kirschner J Cantilever measurements of surface stress, surface reconstruction, film stress and magnetoelastic stress of monolayers. Sensors (Basel) 2008;8(7):4466–4486. doi: 10.3390/s8074466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schlaeger S, Inhuber S, Rohrmeier A, et al Association of paraspinal muscle water-fat MRI-based measurements with isometric strength measurements. Eur Radiol. 2019;29(2):599–608. doi: 10.1007/s00330-018-5631-8. [DOI] [PubMed] [Google Scholar]
- 27.Teichtahl AJ, Urquhart DM, Wang Y, et al Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J. 2015;15(7):1593–1601. doi: 10.1016/j.spinee.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 28.Kjaer P, Bendix T, Sorensen JS, et al. Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med, 2007, 5: 2.
- 29.Dallaway A, Hattersley J, Diokno M, et al Age-related degeneration of lumbar muscle morphology in healthy younger versus older men. Aging Male. 2020;23(5):1583–1597. doi: 10.1080/13685538.2021.1878130. [DOI] [PubMed] [Google Scholar]
- 30.Boissière L, Moal B, Gille O, et al Lumbar spinal muscles and spinal canal study by MRI three-dimensional reconstruction in adult lumbar spinal stenosis. Orthop Traumatol Surg Res. 2017;103(2):279–283. doi: 10.1016/j.otsr.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 31.Yang Q, Yan D, Wang L, et al Muscle fat infiltration but not muscle cross-sectional area is independently associated with bone mineral density at the lumbar spine. Br J Radiol. 2022;95(1134):20210371. doi: 10.1259/bjr.20210371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han G, Zou D, Liu Z, et al Paraspinal muscle characteristics on MRI in degenerative lumbar spine with normal bone density, osteopenia and osteoporosis: a case-control study. BMC Musculoskelet Disord. 2022;23(1):73. doi: 10.1186/s12891-022-05036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu ZJ, He J, Zhao FD, et al An assessment of the intra- and inter-reliability of the lumbar paraspinal muscle parameters using CT scan and magnetic resonance imaging. Spine (Phila Pa 1976) 2011;36(13):E868–E874. doi: 10.1097/BRS.0b013e3181ef6b51. [DOI] [PubMed] [Google Scholar]
- 34.Fan S, Hu Z, Zhao F, et al Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J. 2010;19(2):316–324. doi: 10.1007/s00586-009-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leng J, Han G, Zeng Y, et al The effect of paraspinal muscle degeneration on distal pedicle screw loosening following corrective surgery for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2020;45(9):590–598. doi: 10.1097/BRS.0000000000003336. [DOI] [PubMed] [Google Scholar]