Abstract
Abstract
Purpose
The Obesity and Disease Development Sweden (ODDS) study was designed to create a large cohort to study body mass index (BMI), waist circumference (WC) and changes in weight and WC, in relation to morbidity and mortality.
Participants
ODDS includes 4 295 859 individuals, 2 165 048 men and 2 130 811 women, in Swedish cohorts and national registers with information on weight assessed once (2 555 098 individuals) or more (1 740 761 individuals), in total constituting 7 733 901 weight assessments at the age of 17–103 years in 1963–2020 (recalled weight as of 1911). Information on WC is available in 152 089 men and 212 658 women, out of whom 108 795 have repeated information on WC (in total 512 273 assessments). Information on morbidity and mortality was retrieved from national registers, with follow-up until the end of 2019–2021, varying between the registers.
Findings to date
Among all weight assessments (of which 85% are objectively measured), the median year, age and BMI (IQR) is 1985 (1977–1994) in men and 2001 (1991–2010) in women, age 19 (18–40) years in men and 30 (26–36) years in women and BMI 22.9 (20.9–25.4) kg/m2 in men and 23.2 (21.2–26.1) kg/m2 in women. Normal weight (BMI 18.5–24.9 kg/m2) is present in 67% of assessments in men and 64% in women and obesity (BMI≥30 kg/m2) in 5% of assessments in men and 10% in women. The median (IQR) follow-up time from the first objectively measured or self-reported current weight assessment until emigration, death or end of follow-up is 31.4 (21.8–40.8) years in men and 19.6 (9.3–29.0) years in women. During follow-up, 283 244 men and 123 457 women died.
Future plans
The large sample size and long follow-up of the ODDS Study will provide robust results on anthropometric measures in relation to risk of common diseases and causes of deaths, and novel findings in subgroups and rarer outcomes.
Keywords: Body Mass Index, EPIDEMIOLOGY, Obesity, Weight Gain
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The Obesity and Disease Development Sweden (ODDS) study is a large, pooled cohort of men and women in Sweden with information on weight, height and waist circumference (WC) assessed once or more between 1963 and 2020.
The unique personal identity number of inhabitants of Sweden enables tracking of individuals across ODDS cohorts, thus identifying a large number of individuals with repeated assessments from one or more cohort/s, used to compute changes of weight and WC in adulthood.
The large sample size and long follow-up in national registers for information on morbidity and mortality outcomes ensure high statistical power and enable the investigation of anthropometric measures in relation to rarer outcomes.
Additional important information retrieved from national registers include sociodemographic characteristics, comorbidities and prescribed drugs.
Limitations are incomplete information on smoking habits and no information on dietary intake, physical activity and other potential disease-specific confounders.
Introduction
The prevalence of obesity has risen to pandemic proportions during the last decades, reaching an estimated global prevalence of around 14% in men and 18% in women in 20201 (projected from NCD-RisC),2 generally with a higher prevalence in high-income countries but with an accelerating prevalence in low-income and middle-income countries.2 The negative impact of obesity on public health is large, for example, with disability-adjusted life years, that is, years lost in full health, due to obesity projected to increase by 40% from 2020 to 2030.3 The large negative public health impact of obesity is both attributed to its high prevalence and to the established association of obesity with many common diseases, including cardiovascular diseases (CVD)4 and several cancers,5 as well as with all-cause mortality and cause-specific death due to CVD and cancer.6 Less is known about the association of obesity with rarer diseases, which, in a prospective cohort setting, requires a larger population size and/or a longer follow-up for investigation. Furthermore, body size including obesity has mostly been assessed using a one-time measure of body mass index (BMI, kg/m2) in relation to disease risk. Studies based on measures of central obesity, such as waist circumference (WC), and of changes in body size across life on the risk of morbidity and mortality have been much fewer and smaller.5 7 For example, to our knowledge, the largest study to date on BMI and mortality had 367 512 deaths during follow-up,6 whereas recent meta-analyses of studies on weight changes in middle age8 and older age9 included 34 038 and 69 255 deaths, respectively, for all studies combined. Moreover, most studies of weight changes on outcomes were based on only two weight assessments prone to measurement error. To explore whether particular ages of weight gain rather than cumulative life-time exposure to obesity poses a particularly high risk, different ages of weight assessments are needed in the studied population to enable prediction of age-specific individual weight changes.10 Such sensitive ages to obesity have been shown important, for example, for the development of hypertension and breast cancer.11 Last, weight fluctuations, that is, large variation in weight, are commonly believed to, but not concluded to, result in negative physiological changes, such as less muscle mass and a lower metabolic rate.12 The association of weight fluctuations on disease risk and mortality has been studied to some extent, but large studies with many repeated weight assessments are limited.13
The long history, high coverage and good quality of many Swedish nationwide registers, together with the unique personal identity number of inhabitants of Sweden enabling individual linkage to national healthcare registers,14 is a major advantage for epidemiological research in the country.15 For example, the Swedish Cause of Death Register16 and the Cancer Register17 18 are based on mandatory reporting of deaths and cancer diagnoses of the population since 1952 and 1958, respectively, enabling long and close to complete tracking of individuals for epidemiological studies. The personal identity number further facilitates cross-identification of individuals between different cohorts in pooled studies, which avoids duplicate contribution of an individual included in more than one cohort. It also enables the use of repeated individual assessments between cohorts to enlarge the sample size for the investigation of factors such as longitudinal changes of anthropometrics.
The pooled Obesity and Disease Development Sweden (ODDS) study was created to form a large population to investigate the association of anthropometric measures (BMI, WC and changes in weight and WC) with the risk of morbidity and mortality. The large sample size and long follow-up ensure high statistical power in investigations. Here, we describe the ODDS study population and provide an overview of the information retrieved from national registers linked to individuals in ODDS.
Cohort description
Study population
Swedish cohorts for research and national registers with individual-level information on weight and height were identified for inclusion in ODDS. The included registers with weight and height information are hereafter denoted ‘cohorts’ when referring to the study population. We included individuals with a weight assessment at a minimum age of 17 years, which was the lower age limit of the largest male cohort (military conscripts). We further required a recorded date for the assessment (year as a minimum, with any missing month and/or day replaced with June and/or day 15), and a valid personal identification number in the Swedish Total Population Register. Information on date, weight, and if available, height, WC and smoking habits were included from each assessment. The availability of height was not used as an inclusion criterion for each individual assessment as it could often be derived from repeated assessments, and because other factors, such as sociodemographic factors, were regarded to be equally important as height in studies of changes in weight and WC. Hence, completeness of these factors as potential inclusion criteria was left for later decision according to relevance for individual studies.
The characteristics of the included cohorts forming the ODDS Study population of 4 295 859 unique individuals with 7 733 901 weight assessments are described in table 1. Each cohort is presented separately in the table so individuals participating in more than one cohort are counted in each of these cohorts. Weight in the cohorts was assessed between 1963 and 2020, at an age of 17–103 years. The two largest cohorts are the Swedish Military Conscription Register and the Medical Birth Register, both nationwide and further described below. Other cohorts have local, regional or nationwide coverage of included individuals (table 1). Some of them were designed for research purposes and others were designed as general or disease-specific health check-ups, from which the information was later made available for research.19,42
Table 1. Characteristics of cohorts of the Obesity and Disease Development Sweden (ODDS) Study*.
| Cohort | Description | Individuals, n (% male) | Assessments, n (% male) | Year, median (range) | Age in years, median (range) | N (%) individuals with at least one assessment of: | ||
| Objectively measured weight | Smoking status | Waist circumference | ||||||
| Swedish Medical Birth Register19 | Includes ~98% of all births in Sweden. The mother’s weight is measured at the first antenatal care visit, commonly at 8–10 gestational weeks. Since 1992, weight is missing for <15% | 1 855 606 (0) | 3 208 127 (0) | 2003 (1982–2019) | 29 (17–54) | 1 855 606 (100) | 94 555 (5) | 0 (0) |
| Swedish Military Conscription Register20 | In Sweden, conscription was mandatory for men aged ~18 years until 2010 and was then voluntary until 2017. The male birth cohorts of 1951–1988 cover 90% of the target population, with ≤5% missing weight before 2000 | 1 790 751 (99) | 1 799 609 (99) | 1987 (1969–2014) | 18 (17–58) | 1 790 751 (100) | 190 197 (11) | 0 (0) |
| Construction Workers Cohort21 | Construction workers were invited on a regular basis to a health check-up through a collective agreement that concerned almost all construction workers in Sweden. Attendance: ≥80% | 387 545 (95) | 1 149 722 (96) | 1981 (1971–1993) | 37 (17–82) | 387 545 (100) | 333 100 (86) | 0 (0) |
| NSHDS22 | Population-based cohorts in the northernmost counties of Sweden: Norrbotten and Västerbotten | 138 379 (47) | 254 441 (40) | 2002 (1985–2020) | 50 (18–82) | 132 369 (96) | 131 734 (95) | 97 061 (70) |
| VIP23 | All residents of Västerbotten county are invited to a health check-up at 40, 50 and 60 years of age (and 30 years until 1996). Attendance: 48%–67% | 124 200 (49) | 194 650 (49) | 2005 (1985–2020) | 49 (19–70) | 124 200 (100) | 123 216 (99) | 87 538 (70) |
| MONICA24 | Seven health screenings aimed for research were performed in random selections (within specific ages) of residents of Norrbotten and Västerbotten counties. Attendance: 67%–81% in 1986–2009 | 12 260 (49) | 16 097 (49) | 1999 (1986–2014) | 51 (24–79) | 12 260 (100) | 12 245 (>99) | 12 235 (>99) |
| MSP25 | A questionnaire aimed for research was filled in connection with mammography screening offered every 2–3 years to women aged ~50–70 years in Västerbotten county. Attendance: ~85% | 25 836 (0) | 43 694 (0) | 1999 (1995–2006) | 58 (18–82) | 0 (0) | 20 026 (78) | 0 (0) |
| SIMPLER26 | Population-based cohorts in counties of southeastern Sweden: Uppsala, Västmanland and Örebro | 106 391 (43) | 237 966 (39) | 1997 (1987–2019) | 64 (38–103) | 0 (0) | 89 598 (84) | 81 462 (77) |
| SMC | All women born 1914/1917–1948, residing in Västmanland and Uppsala counties were invited to mammography screening that included a questionnaire aimed for research, with subsequent follow-ups. Attendance at baseline: 70% | 60 709 (0) | 145 234 (0) | 1997 (1987–2019) | 62 (38–103) | 0 (0) | 44 121 (73) | 40 338 (66) |
| COSM | All men born 1918–1952 residing in Västmanland and Örebro counties were invited to fill in a research-based questionnaire, with subsequent follow-ups. Attendance at baseline: 49% | 45 682 (100) | 92 732 (100) | 2008 (1997–2019) | 67 (42–101) | 0 (0) | 45 477 (>99) | 41 124 (90) |
| Swedish Twin Registry27 28 | Research-based register on mono and dizygotic twins across all of Sweden | 97 533 (46) | 154 666 (45) | 1999 (1963–2014) | 48 (17–99) | 12 360 (13) | 90 182 (92) | 12 328 (13) |
| Q63, 67, 70 | All same-sex twins born 1886–1925 were invited to fill in a questionnaire (not including weight) in 1960. Follow-up questionnaires were sent out three times during the subsequent 10 years (Q63, 67 and 70) | 20 312 (44) | 42 347 (41) | 1967 (1963–1970) | 53 (37–84) | 0 (0) | 17 986 (89) | 0 (0) |
| Q73 | All same-sex twins born 1926–1958 were invited to fill in a questionnaire in 1973. Attendance: ~83% | 27 595 (48) | 27 595 (48) | 1973 (1973–1973) | 29 (17–47) | 0 (0) | 27 507 (>99) | 0 (0) |
| SALT | All twins born 1944–58 were invited to a phone interview. Attendance: ~65% | 42 754 (47) | 42 754 (47) | 2000 (1998–2003) | 56 (41–99) | (0) | 42 234 (99) | 0 (0) |
| TwinGene | Twin pairs in SALT were invited to a follow-up investigation. Attendance: ~65% | 12 360 (45) | 12 360 (45) | 2006 (2002–2009) | 64 (47–93) | 12 360 (100) | 12 237 (99) | 12 328 (>99) |
| STAGE | All twin pairs born 1958–1985 were invited to a web-based survey. Attendance: ~60% | 23 448 (44) | 23 448 (44) | 2005 (2004–2006) | 34 (19–47) | 0 (0) | 23 230 (99) | 0 (0) |
| YATSS | All twin pairs born 1986–1992 were invited to a web-based survey. Attendance: ~42% | 6162 (40) | 6162 (40) | 2013 (2013–2014) | 24 (20–28) | 0 (0) | 1988 (32) | 0 (0) |
| Malmö cohorts | Population-based cohorts in Malmö city in southern Sweden (MPP and MDCS) and offspring of MDCS participants (MOS) | 54 876 (53) | 124 442 (54) | 1995 (1974–2019) | 56 (18–85) | 54 860 (>99) | 48 392 (88) | 36 170 (66) |
| MPP29 30 | All residents of Malmö city, born in certain years, 1921–1949, were invited for screening for CVD and alcohol abuse, with subsequent follow-ups of all or a selected population. Attendance at baseline: ~71% | 33 337 (67) | 59 427 (70) | 1983 (1974–2006) | 53 (26–85) | 33 337 (100) | 28 294 (85) | 4506 (14) |
| MDCS31 | All residents of Malmö city, born in certain years, 1926–1950, were invited to a health examination aimed for research on diet and cancer, with subsequent follow-ups of all or a selected population. Attendance at baseline: ~41% | 30 415 (40) | 60 792 (39) | 1997 (1991–2012) | 61 (44–85) | 30 390 (>99) | 29 280 (96) | 30 373 (>99) |
| MOS32 | Children and grandchildren of a random sample of MDCS participants were invited to a health examination for research purposes | 4223 (48) | 4223 (48) | 2016 (2013–2019) | 44 (18–73) | 4223 (100) | 3799 (90) | 4202 (>99) |
| Women’s Lifestyle and Health33 | Randomly selected women born 1943–1962 residing in Uppsala county were invited to fill in a questionnaire aimed for research on lifestyle and cancer and CVD, and to one subsequent follow-up. Attendance at baseline: 51% | 48 720 (0) | 82 140 (0) | 1992 (1991–2004) | 44 (27–61) | 0 (0) | 40 840 (84) | 43 132 (89) |
| Swedish National March Cohort34 | In 1997, a fund-raising event for the Swedish Cancer Society took place in ~3600 places across Sweden. Participants were requested to fill in a questionnaire aimed for research on lifestyle and chronic diseases | 41 710 (36) | 41 710 (36) | 1997 (1997–1997) | 52 (17–93) | 0 (0) | 35 801 (86) | 31 893 (76) |
| West Sweden Asthma Study35 | In 2008 and 2016, random selections of residents of western Sweden were invited to fill in a questionnaire aimed for research on asthma and respiratory diseases. Attendance: 62% and 50%, respectively | 41 276 (46) | 53 231 (45) | 2016 (2008–2016) | 51 (17–83) | 0 (0) | 40 506 (98) | 0 (0) |
| WICTORY36 | Residents of Västmanland county, born 1940–1959, were invited to a health check-up at age ~40 or 50 years, aimed for CVD prevention. Attendance: ~60% | 33 892 (48) | 33 892 (48) | 1994 (1989–2000) | 49 (35–55) | 33 892 (100) | 33 579 (99) | 33 860 (>99) |
| LifeGene37 | Residents across Sweden were invited through randomisation (~44%), or in other ways, for example, shared household with the one invited, or volunteering, to a health examination and a web-based survey for research purposes | 30 039 (41) | 30 039 (41) | 2011 (2009–2018) | 33 (17–96) | 28 861 (96) | 16 407 (55) | 28 861 (96) |
| EpiHealth38 39 | Randomly selected ~45–75-year-old residents of Uppsala and Malmö city were invited to a health examination and a web-based survey for research on gene–diet interactions and diseases. Attendance: ~20% | 25 337 (44) | 25 337 (44) | 2014 (2011–2018) | 61 (35–78) | 25 337 (100) | 18 416 (73) | 25 337 (100) |
| Melanoma in Southern Sweden40 | Randomly selected women with no prior cancer, ~25–64 years, residing in Southern Sweden, were in 1990–1992 invited to fill in a questionnaire (not including weight) aimed for research on malignant melanoma and female cancers. A follow-up questionnaire included weight. Attendance at baseline: 74% | 22 974 (0) | 22 974 (0) | 2001 (1999–2004) | 54 (35–76) | 0 (0) | 2399 (10) | 0 (0) |
| Obstructive Lung Disease in Northern Sweden41 42 | In separate surveys (five in ODDS), randomly selected adults of specific ages, residing in Norrbotten county, were invited to a health examination and follow-ups, or to fill in a questionnaire (2016), aimed for research on asthma and respiratory diseases. Attendance at baseline: 66%–91% | 12 395 (49) | 15 386 (49) | 2004 (1986–2016) | 53 (19–85) | 5853 (47) | 12 241 (99) | 0 (0) |
The numbers include overlap of individuals between cohorts, and only objectively measured or self-reported current weight. Recalled weight is available in 225 331 individuals with 500 219 recalled weights in: SIMPLER, Swedish Twin Registry (Q67 and Q70), MDCS, MOS, Women’s Lifestyle and Health, Swedish National March Cohort, EpiHealth, and Melanoma in Southern Sweden, included in table 3.
COSM, Cohort of Swedish Men; CVD, cardiovascular disease; MDCS, Malmö Diet and Cancer Study; MONICA, Monitoring of Trends of Cardiovascular disease study in Northern Sweden; MOS, Malmö Offspring Study; MPP, Malmö Preventive Project; MSP, Mammography Screening Project; NSHDS, Northern Sweden Health and Disease Study; SALT, Screening Across the Lifespan Twin Study; SIMPLER, Swedish Infrastructure for Medical Population-Based Life-Course and Environmental Research; SMC, Swedish Mammography Cohort; STAGE, Study of Twin Adults: Genes and Environment; VIP, Västerbotten Intervention Programme; WICTORY, Westmannia Cardiovascular Risk Factors StudyYATSS, Young Adult Twins in Sweden Study
Weight assessments, completeness and population coverage of the two largest cohorts
Data from military conscripts make up the majority of the male population (1 771 429 men with 1 779 681 weight assessments) and the Medical Birth Register makes up the majority of the female population (1 855 606 women with 3 208 127 weight assessments). In Sweden, conscription, that is, enrolment for military service, was mandatory for men at around 18 years of age until 30 June 2010, and was thereafter voluntary until 2017.20 For young women, conscription has been voluntary since the 1980s. The coverage in the Military Conscription Register of the Swedish male birth cohorts of 1951–1988 (corresponding to conscription between 1969 and 2006) is 90%. Weight is missing for at most 5% of conscript examinations before year 2000. No information on WC is available in the Military Conscription Register.
The Medical Birth Register includes information on around 98% of all births in Sweden. Since 1982, information is recorded at the first antenatal visit of pregnancy, generally taking place between 8 and 10 weeks of gestation.19 A large population-based study in Sweden showed that weight gain in pregnancy was minimal during the first 15 weeks of gestation, for example, with a median weight gain in normal weight women of 0.7 kg between gestational week 6 and 10.43 Weight of pregnant women were recorded in the Medical Birth Register in 1982–1989 and from 1992 onwards and has a coverage of more than 85% since 1992. In 1982–1989, early pregnancy weight was estimated by subtracting pregnancy weight gain from weight at delivery, and since 1992, weight was measured at the first antenatal visit. Due to this change in weight recording, weight in 1982–1989 was much lower than expected compared with measurements from 1992 onwards, as also observed in other studies.44 45 Therefore, we corrected weight assessments in 1982–1989 in the Medical Birth Register using a linear regression model of weight and calendar year from 1992 onwards. For illustration purposes, we let j represent the calendar years 1982–1989 for an individual i. We first regressed weight (Wi) on the year (Yi) at baseline examination (ie, first antenatal care visit) to obtain the average weight change over time (constant, b0) and slope (b1). Using these coefficients, we predicted the average weight for each calendar year j (1982–1989) as Wj=b0 + b1 × Yj. We then obtained the difference of the observed average weight from the predicted average weight between 1982–1989, then added this factor to the original weight value and obtained a more linear weight change, as also reported elsewhere.44 These corrected weights were used in the pooled analysis presented here and will be used in original ODDS studies. Additionally, pregnancy will be accounted for in all pooled analyses by inclusion of a binary variable (Medical Birth Register, yes/no) in the statistical regression or other models. No information on WC is available in the Medical Birth Register.
Weight and WC assessments in other cohorts
Other cohorts than the two largest include 972 974 individuals with 2 225 946 objectively measured or self-reported current weight assessments, of which objectively measured or self-reported WC is available in 364 747 individuals with 512 273 assessments. Self-reported current weight has shown very high validity in western populations with a correlation coefficient with objectively measured weight of over 0.95.46 47 High validity has also been shown for self-reported WC in western populations, showing correlation coefficients with objectively measured WC of over 0.85 when instructions were provided on how to measure WC,46 47 and only slightly lower when no instructions were provided.48 In ODDS, the SIMPLER cohorts and the National March Cohort collected self-reported WC information from questionnaires without further instructions, and in Women’s Lifestyle and Health, a picture indicated where to place the tape measure. WC in the other cohorts were objectively measured. In several cohorts, information on recalled weight was collected simultaneously with that of current weight (see footnote of table 1). A total of 225 331 individuals reported 500 219 recalled weights, mostly for age 20 years (139 936 (28%) of assessments), but also for 18, 25, 30, 40, 50, 60, 70 and 80 years of age, from the year 1911 or later. These assessments will primarily be used in ODDS studies of weight changes, and a sensitivity analysis excluding these measures will always be performed. In the pooled ODDS study population, recalled weight is counted as a distinct weight assessment with the date set to that of the age for the recalled weight.
Smoking information
The questions asked regarding smoking habits and the completeness of smoking information varies considerably between ODDS cohorts. To increase the completeness of smoking status in individuals with repeated weight assessments with missing and non-missing smoking information, we performed single imputation by carrying information forwards or backwards within and between cohorts, prioritising previous records over later records for never/former/current smoking status, but not for current smoking (yes/no). After imputation, never/former/current smoking information is available in 2 856 160 (37%) assessments, and current smoking (yes/no) information in 5 061 903 (65%) assessments. In total 828 763 individuals (19%) have at least one weight assessment with never/former/current smoking information available, and the proportion is larger for individuals with WC assessments (330 775 individuals, 91%). To increase the coverage of smoking information, multiple imputation49 based on all available data may be considered in single ODDS studies. Furthermore, studies dependent on the coverage of registers with a later start, such as the Patient Register (for information on CVD and Charlson comorbidity index50) or the Swedish Social Insurance Agency for studies on sick leave, will include only later years’ measurements of weight, which have a markedly higher coverage of smoking information.
Register linkages
By use of the unique personal identity number assigned to each resident of Sweden, individuals in ODDS were linked to a range of Swedish national registers from inception to the last possible follow-up date, varying between 2019 and 2021 depending on the specific register. Birth date was retrieved from the Total Population Register; however, due to Swedish legislation protecting individual integrity, date of birth was obtained only for the year and quarter of the year, so we imputed the missing date by the mean value of possible dates, for example, 15 February for the first quarter of the year.
Table 2 gives an overview of the registers and the type of information retrieved.16,18 51,60 This includes information on outcomes: all-cause and cause-specific mortality by use of the Cause of Death Register; specific cancers in the Cancer Register; prostate cancer in detailed diagnostic risk categories by use of information from the National Prostate Cancer Register; CVD, hypertension and type 2 diabetes by use of the Patient Register and National Diabetes Register; and sick leave by use of information from the Swedish Social Insurance Agency. Sociodemographic information of relevance for all ODDS studies, such as education, income, marital status and birth country, was retrieved from several national registers.
Table 2. Information on Swedish national registers with linkage to the Obesity and Disease Development Sweden (ODDS) study population.
| Swedish register | Description | Type of information retrieved | Years covered in ODDS | Coverage of target population |
| The Cancer Register17 18 | Contains information on histologically, cytologically or clinically diagnosed, or by autopsy verified (excluding death certificate only) malignant tumours, and certain benign, premalignant and borderline tumours, in Sweden | Date and type of cancer diagnosis, including International Classification of Diseases topography code, histopathology (Swedish SNOMED and PAD codes), and TNM status (recorded since 2004) | 1958–2019 | 96% in the year 1998,17 which appears to be stable over time |
| The Cause of Death Register16 | Contains information on deaths and death causes in Sweden, in electronic form since 1952. The death cause is usually determined by the treating physician or the physician last seeing the patient before death | Date of death and underlying and contributing death causes according to International Classification of Diseases codes | 1952–2020 | >99% and 96% of the underlying cause of death (>99% of deaths in ODDS) |
| The Longitudinal Integration Database for Health Insurance and Labour Market Studies (LISA)51 | Contains information from a range of sources on education, occupation, income and employment in all residents of Sweden aged ≥16 years (≥15 years since 2010) | Highest attained education. Occupation, income and main source of income (recorded since 1993) | 1990–2019 | >99% overall, 98% for education in 25–64-year-old individuals |
| The National Diabetes Register52 53 | Contains information on diabetes diagnoses (all types) and other information, such as complications and treatment, of diabetes patients aged ≥18 years in outpatient specialist clinics and in primary healthcare in Sweden | Date and type of diabetes diagnosis and treatment | 1996–2020 | Increased coverage over time; ~90% of Swedish adults with diabetes in 2015 |
| The National Prostate Cancer Register54 55 | Contains information on biopsy-confirmed prostate cancer diagnoses, tumour characteristics, and primary treatment of prostate cancer patients in Sweden | Date, TNM status, prostate-specific antigen level, and Gleason score at diagnosis, and the main reason for detection (recorded since 2004). Primary treatment, date of radical prostatectomy (recorded since 2007) and T status, Gleason score and positive margins (yes/no) after radical prostatectomy | 1998–2021 (June) | 98% of prostate cancer diagnoses in the National Cancer Register in 1998–2012 |
| The Patient Register56 57 | Contains information on diagnoses of inpatient care in Sweden, recorded since 1987, and of specialist outpatient care, recorded since 1997 for surgical care and since 2001 for other outpatient care | Date and type of diagnosis according to the Swedish International Classification of Diseases codes in inpatient and outpatient care. Information was obtained for cardiovascular diseases, hypertension, diabetes and diagnoses of the Charlson Comorbidity index50 | 1987–2020 | Since 1987, >99% of inpatient care and in 2001–2006, 71% of outpatient somatic care |
| The Population and Housing Census51 | Contains sociodemographic information through self-reported questionnaires mailed to the full Swedish population aged ≥16 years, with mandatory response | Highest attained education, county of residence and marital status | Every 5 years in 1960–1990 | ≥99% in 1960–1985, 97.5% in 1990* |
| The Prescribed Drug Register58 | Contains information on all prescribed drugs dispensed at pharmacies in Sweden. Excludes over-the-counter drugs | Date of prescribing and dispensing, type of drug (eg, ATC code and product name), dispensed amount and dosage, of antidiabetic, antihypertensive and antilipidemic drugs | 2005 (July)−2021 | >95% of all used drugs in Sweden, excluding over-the-counter drugs |
| The Total Population Register59 | Contains basic demographic information on all residents of Sweden | Birth date (year and quarter of year), country of birth for the individual and parents (four categories, see table 3), county of residence, marital status and date/s of immigration and emigration | 1968–2020 | >99% of births and deaths, 95% of immigrations, 91% of emigrations, resulting in a slight over-coverage |
| The Swedish Social Insurance Agency60 | Contains information on sick leave for periods exceeding 14 days, and of disability pension, for individuals in Sweden with income from work or unemployment benefits, which qualify and apply for sickness absence or disability pension benefits. The first 14 days of sick leave is compensated by the employer and is not recorded by the Social Insurance Agency | Date, length and type of sick leave according to International Classification of Diseases codes, for periods lasting more than 14 days and of disability pension | 1994–2021 (June) | No data available† |
Personal communication with Beatrice Kalnins, Statistics, Sweden.
Personal communication with Charlotte Limé, the Swedish Social Insurance Agency.
ATCAnatomical Therapeutic ChemicalPADPathologic-Anatomic DiagnosisSNOMEDSystematized Nomenclature of MedicineTNMTumour, Nodes, and Metastases
Patient and public involvement
Study participants and/or the public were not involved in the planning, design or conduct of the study.
Findings to date
Characteristics of all weight and WC assessments
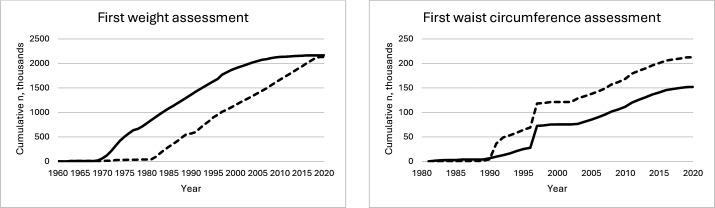
The characteristics of all 7 733 901 weight assessments in the 4 295 859 individuals in ODDS is shown in table 3 and the cumulative number of ODDS participants by year of assessment of the first recorded current weight and WC, respectively, is shown in figure 1. Most weight assessments were objectively measured (85%), and 4 066 876 individuals (95%) have information from at least one objectively measured weight assessment. The median (IQR) year and age of weight assessment is lower in men than in women; year 1985 (1977–1994) vs 2001 (1991–2010) and 19 (18–40) vs 30 (26–36) years of age. Normal weight (BMI 18.5–24.9 kg/m2) is present in 67% of assessments in men and 64% in women, and obesity (BMI≥30 kg/m2) in 5% of assessments in men and 10% in women. The low proportion of obesity in men is likely due to the, on average, young age and early calendar year at weight assessment. Information on WC is available in 152 089 men with 209473 WC assessments and in 212 658 women with 302 800 WC assessments; 52% of these were objectively measured and 63% of individuals have at least one objectively measured WC assessment. The median (IQR) year of the 512 273 WC assessments is later than that of weight, year 2007 (1997–2012) for men and 2003 (1997–2010) for women and the median age is higher, 57 (49–66) years in men and 51 (43–62) years in women.61 62
Table 3. Characteristics of all assessments in the Obesity and Disease Development Sweden (ODDS) Study, in a total of 4 295 859 unique individuals and separately in 2 165 048 men and 2 130 811 women.
| Characteristic | Total(assessments, n=7 733 901) | Men(assessments, n=3 530 952) | Women(assessments, n=4 202 949) |
| Assessments, median no. (IQR) | 1 (1–2) | 1 (1–1) | 2 (1–2) |
| Year | |||
| Median (IQR) | 1993 (1983–2005) | 1985 (1977–1994) | 2001 (1991–2010) |
| N (%) | |||
| 1911–1959* | 102 331 (1) | 49 817 (1) | 52 514 (1) |
| 1960–1969 | 159 059 (2) | 70 493 (2) | 88 566 (2) |
| 1970–1979 | 1 118 503 (15) | 1 011 194 (29) | 107 309 (2) |
| 1980–1989 | 1 866 055 (24) | 1 128 163 (32) | 737 892 (18) |
| 1990–1999 | 1 775 421 (23) | 780 028 (22) | 995 393 (24) |
| 2000–2009 | 1 470 566 (19) | 365 475 (10) | 1 105 091 (26) |
| ≥2010 | 1 241 966 (16) | 125 782 (4) | 1 116 184 (27) |
| Age (years) | |||
| Median (IQR) | 28 (19–37) | 19 (18–40) | 30 (26–36) |
| N (%) | |||
| 17–19 | 1 941 872 (25) | 1 780 928 (50) | 160 944 (4) |
| 20–29 | 2 222 093 (29) | 417 774 (12) | 1 804 319 (43) |
| 30–39 | 1 858 853 (24) | 373 384 (11) | 1 485 469 (35) |
| 40–49 | 661 048 (9) | 375 880 (11) | 285 168 (7) |
| 50–59 | 570 068 (7) | 337 970 (9) | 232 098 (5) |
| 60–69 | 324 381 (4) | 174 004 (5) | 150 377 (4) |
| ≥70 | 155 586 (2) | 71 012 (2) | 84 574 (2) |
| Weight (kg), median (IQR) | 68 (61–77) | 73 (66–81) | 64 (58–72) |
| Form of weight assessment, n (%) | |||
| Objectively measured | 6 579 779 (85) | 3 097 486 (88) | 3 482 293 (83) |
| Self-reported current weight | 653 903 (8) | 207 579 (6) | 446 324 (11) |
| Self-reported recalled weight | 500 219 (7) | 225 887 (6) | 274 332 (6) |
| Height (cm), median (IQR) | 171 (165–178) | 178 (174–183) | 166 (162–170) |
| Body mass index (kg/m2) | |||
| Median (IQR) | 23.1 (21.0–25.7) | 22.9 (20.9–25.4) | 23.2 (21.2–26.1) |
| N (%)† | |||
| Underweight (<18.5) | 305 069 (4) | 160 666 (5) | 144 403 (3) |
| Normal weight (18.5–24.9) | 5 040 375 (65) | 2 378 070 (67) | 2 662 305 (63) |
| Overweight (25–29.9) | 1 792 975 (23) | 826 610 (23) | 966 365 (23) |
| Obesity class I (30–34.9) | 429 028 (6) | 137 401 (4) | 291 627 (7) |
| Obesity class II and III (≥35) | 129 392 (2) | 23 465 (1) | 105 927 (3) |
| Missing | 37 062 (<1) | 4740 (<1) | 32 322 (1) |
| Waist circumference (cm) | |||
| Median (IQR) | 88 (79–97) | 96 (89–103) | 82 (75–90) |
| N (%)† | |||
| Low (men, <94; women, <80) | 210 489 (3) | 86 426 (2) | 124 063 (3) |
| Medium (men, 94–101.9; women, 80–87.9) | 143 891 (2) | 64 225 (2) | 79 666 (2) |
| High (men, ≥102; women, ≥88) | 157 893 (2) | 58 822 (2) | 99 071 (2) |
| Missing | 7 221 628 (93) | 3 321 479 (94) | 3 900 149 (93) |
| Smoking status, n (%) | |||
| Never | 1 334 569 (17) | 794 267 (23) | 540 302 (13) |
| Former | 679 222 (9) | 432 751 (12) | 246 471 (6) |
| Current | 842 369 (11) | 613 139 (17) | 229 230 (5) |
| Missing | 4 877 741 (63) | 1 690 795 (48) | 3 186 946 (76) |
| Marital status, n (%)‡ | |||
| Unmarried | 4 092 269 (53) | 2 297 106 (65) | 1 795 163 (43) |
| Married | 3 102 435 (40) | 1 048 593 (30) | 2 053 842 (49) |
| Divorced | 349 667 (5) | 117 091 (3) | 232 576 (5) |
| Widow/er | 88 954 (1) | 23 535 (1) | 65 419 (2) |
| Missing | 100 576 (1) | 44 627 (1) | 55 949 (1) |
| County of residence, n (%)‡ | |||
| Stockholm | 1 253 881 (16) | 481 693 (14) | 772 188 (18) |
| Västra Götaland | 1 136 238 (15) | 521 656 (15) | 614 582 (15) |
| Skåne | 993 581 (13) | 451 103 (13) | 542 478 (13) |
| Västmanland | 467 638 (6) | 219 591 (6) | 248 047 (6) |
| Västerbotten | 439 512 (5) | 203 544 (6) | 235 968 (6) |
| Uppsala | 382 360 (5) | 102 044 (3) | 280 316 (7) |
| Other counties | 3 060 691 (39) | 1 502 928 (42) | 1 449 729 (34) |
| Missing | 108 034 (1) | 48 393 (1) | 59 641 (1) |
| Highest achieved education (one assessment per individual), n (%)§ | |||
| Pre-upper secondary school<9 years | 280 244 (7) | 167 940 (8) | 112 304 (5) |
| Pre-upper secondary school 9 years | 366 211 (9) | 215 953 (10) | 150 258 (7) |
| Upper secondary school max. 2 years | 1 030 829 (24) | 578 620 (27) | 452 209 (21) |
| Upper secondary school 3 years | 880 747 (20) | 455 344 (21) | 425 403 (20) |
| Post-upper secondary school<3 years | 613 421 (14) | 299 872 (14) | 313 549 (15) |
| Post-upper secondary school≥3 years | 1 020 461 (24) | 393 934 (18) | 626 527 (30) |
| PhD degree | 52 219 (1) | 28 056 (1) | 24 163 (1) |
| Missing | 51 727 (1) | 25 329 (1) | 26 398 (1) |
| Country of birth (one assessment per individual), n (%)¶ | |||
| Born in Sweden, both parents born in Sweden | 3 367 487 (78) | 1 842 225 (85) | 1 525 262 (72) |
| Born in Sweden, one parent born in Sweden | 295 156 (7) | 156 744 (7) | 138 412 (6) |
| Born in Sweden, both parents born abroad | 121 237 (3) | 58 840 (3) | 62 397 (3) |
| Born abroad | 511 469 (12) | 107 147 (5) | 404 322 (19) |
| Missing | 510 (<1) | 92 (<1) | 418 (<1) |
Includes only recalled weight assessments.
Categories according to the World Health OrganizationWHO.61 62
From the Population and Housing Census in 1960 and 1965 and and from the Register of the Total Population in 1968 onwards. Married, divorced and widow/-er also include registered partners, recorded as of 1998. Fifteen15 ‘other counties’ each made up <5% of the total.
Highest achieved education through follow-up, retrieved from the Population and Housing Census in 1970, and from the Longitudinal Integration Database for Health Insurance and Labour Market Studies in 1990 onwards.
From the Register of the Total Population.
Figure 1. Cumulative number (n) of men (solid line) and women (dotted line) per calendar year, at the first objectively measured or self-reported current weight (1963–2020) or waist circumference (1981–2020), in the Obesity and Diseases Development Sweden (ODDS) study.
Characteristics of repeated weight and WC assessments
Individuals with two or more assessments of weight or WC, respectively, will be eligible for inclusion in studies of change of these factors, on outcomes. In these studies, we will use all assessments in an individual, that is, allowing assessments to take place in different cohorts. For each assessment, age, form of assessment (objectively measured/self-reported current/self-reported recalled) and, in women, a pregnancy indicator (Medical Birth Register, yes/no) will be included as predictor variables to model weight and WC trajectories in mixed effects models.10
Out of 477 705 men and 1 263 056 women with 2 or more weight assessments, totalling 1 843 609 assessments in men and 3 335 194 in women, the median number of assessments is 3 (IQR 2–5) in men and 2 (IQR 2–3) in women. The much smaller number of assessments in men than in women is due to the lack of repeated weight assessments in the Military Conscription Register as opposed to the many assessments in the Medical Birth Register. In individuals with two or more weight assessments, the by far largest number of assessments in men originate from the Construction Workers Cohort (n=1 036 968) followed by the Cohort of Swedish Men (n=268 408) and the Military Conscription Register (n=216 585), and the by far most assessments in women are from the Medical Birth Register (n=2 435 226) followed by the Swedish Mammography Cohort (n=273 717) and Women’s Lifestyle and Health (n=127 384). Out of 41 669 men and 67 126 women with 2 or more WC assessments, totalling 99 053 assessments in men and 157 268 in women, the median number of assessments is 2 (IQR 2–3) in men and 2 (IQR 2–2) in women. Of these, the largest number of WC assessments in men originate from the Cohort of Swedish Men (n=59 863) and the Västerbotten Intervention Programme (n=19 549) and in women from the Swedish Mammography Cohort (n=56 222) and Women’s Lifestyle and Health (n=51 696).
Follow-up time and events
The follow-up time from the first recorded current weight until emigration, death or end of follow-up for death (31 December 2020) is up to 58 years, with a median (IQR) of 31.4 (21.8–40.8) years in men and 19.6 (9.3–29.0) years in women, and a median (IQR) from the first WC assessment of 13.4 (8.0–23.2) years in men and 17.1 (9.6–25.0) years in women. The total time at risk for mortality is 66.3 million person-years for men and 42.0 million person-years for women, during which 280 537 men and 121 635 women died. Among morbidity outcomes, cancer is of main focus in the ODDS working group. Information on the number of deaths (all-cause and cause-specific) and incident cancers (all and some site-specific) during follow-up in the full ODDS population, in individuals with two or more weight assessments for studies of weight change, and in individuals with one and two or more WC assessments, respectively, is shown in table 4.
Table 4. Number of individuals, deaths and incident cancers during follow-up according to anthropometric measure in the Obesity and Disease Development Sweden (ODDS) study.
| Anthropometric measure | Individuals, n | Deaths, n | Incident cancers, n | |||
| Men | Women | Men | Women | Men | Women | |
| Weight (full population) | 2 165 048 | 2 130 811 | 280 537 all-cause98 796 CVD78 178 cancer15 325 respiratory system | 121 635 all-cause35 198 CVD45 744 cancer7174 respiratory system | 197 168 all cancer62 027 prostate11 448 colon993 small intestine658 penis | 144 413 all cancer50 732 breast7920 colon530 small intestine742 vulva |
| ≥2 weight assessments | 477 705 | 1 263 056 | 133 073 all-cause | 62 245 all-cause | 84 205 all cancer | 70 697 all cancer |
| Waist circumference | 152 089 | 212 658 | 37 155 all-cause | 35 951 all-cause | 26 619 all cancer | 28 296 all cancer |
| ≥2 waist circumference assessments | 41 669 | 67 126 | 9890 all-cause | 8664 all-cause | 6407 all cancer | 7321 all cancer |
CVD, cardiovascular diseases
Ongoing and planned studies
Several ODDS studies are ongoing or planned to start shortly on BMI, WC and changes in weight and WC, in relation to the risk of outcomes (currently mortality and cancer). Changes in weight and WC include the investigation of changes across adulthood and in age spans of young, middle and late adulthood. We further plan to investigate: (1) weight fluctuations in individuals with many repeated weight assessments in relation to outcomes, (2) anthropometric measures in interaction with, and mediated through, cardiometabolic diseases (CVD, hypertension and type 2 diabetes) on non-CVD outcomes, (3) anthropometric measures jointly with prescribed drugs (using retrieved data and after additional register linkages) on outcomes and (4) anthropometric measures in relation to specific cancers with detailed diagnostic information, after additional linkages to national quality registers of cancer. ODDS enables a range of further possible investigations to be done in the obesity field, based on already collected data or after additional register linkages. Further information about ODDS can be found at the https://odds.blogg.lu.sehttps://odds.blogg.lu.se webpage.
Strengths and limitations
The ODDS study has several strengths. First, the population is very large and has a nationwide coverage of Swedish cohorts, which, although not completely population-based, generally have a high representativeness of their background population. Furthermore, the unique personal identity number of Swedish inhabitants enables cross identification of individuals between ODDS cohorts as well as tracking of individuals in Swedish nationwide registers. Loss to follow-up is negligible in those registers, and the objective, harmonised information on outcomes as well as on sociodemographic factors by use of national registers, is an additional major strength. The combination of anthropometric measures in the pooled population with, for example, cardiometabolic diseases and medications retrieved from national registers, enables the investigation of various risk factors jointly with anthropometrics. At last, the long follow-up time together with the large sample size has accumulated many events, resulting in overall high statistical power and the possibility to investigate subgroups and rarer outcomes.
The study also has some limitations. Because repeated weight measurements were not performed in military conscripts, which make up the largest male cohort in ODDS, only 22% of men have repeated measurements on weight. By contrast, almost 60% of women have two or more weight measurements. Furthermore, the large heterogeneity of the study population in terms of geographical region, age and year of weight assessment, enforces subgroup investigation, to examine whether associations differ between subgroups. The study is further limited in that information on smoking habits, an important confounder for mortality and many diseases, is missing in a large part of the population and, apart from sociodemographic information, the ODDS database has no information on potential confounders such as diet, physical activity and other disease-specific confounders.
Acknowledgements
We thank all participants, founders, data managers and funders of ODDS cohorts. We thank the Biobank Research Unit at Umeå University, Västerbotten Intervention Programme, the Northern Sweden MONICA study and the County Council of Västerbotten for providing data and acknowledge the contribution from Biobank Sweden, supported by the Swedish Research Council (VR 2017-00650). We acknowledge the Swedish Twin Registry for access to data. The Swedish Twin Registry is managed by Karolinska Institutet and receives funding through the Swedish Research Council under the grant no 2021-00180. We further acknowledge Anders Dahlin, database manager of the Malmö cohorts, and support of the Malmö cohorts in the form of a Lund University Infrastructure grant (STYR 2019/2046). The health examination and data collection in WICTORY were supported by the Regional Council of Västmanland and the Regional Research Council Uppsala-Örebro, Sweden. In OLIN, we acknowledge professor Eva Rönmark and the late professor Bo Lundbäck.
Footnotes
Funding: The ODDS Study has so far been funded by the Swedish Research Council (no. 2021-01934), the Swedish Cancer Society (230633 SIA and 232767 Pj), Mrs. Berta Kamprad’s Cancer Foundation (FBKS-2021-12-343), the Crafoord foundation (20210628, 20220572 and 20230547) and the Cancer Research Foundation at the Department of Oncology, Malmö University Hospital.
Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-084836).
Data availability free text: All data are located on Statistics Sweden’s Microdata Online Access (MONA) server and may only be accessed from countries in the European Union or the European Economic Area. Data access for questions covered by the ethical approval will be considered in agreement with the principal investigator of ODDS, TS and on approval from relevant register holders and steering committees of ODDS cohorts.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants. This study was approved by the Swedish Ethical Review Authority (no: 2020-03846). Some of the included cohorts collected informed consent from participants, others did not, and the two largest cohorts are individuals in national registers (military conscripts and women giving birth) for which informed consent was not collected. It is unfeasible to collect this information for a study of this size. All data are pseudonymised and located on a safe server at Statistics Sweden, without possibility to extract any data.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Collaborators: The ODDS collaboration conducts research in accordance with the ethical approval of the ODDS cohort as well as approvals from the steering committee of each subcohort. New research ideas will require new approvals. Researchers interested in collaboration can contact the ODDS principal investigator, TS, for further information and discussion.
Contributor Information
Marisa da Silva, Email: marisa.da_silva@med.lu.se.
Josef Fritz, Email: josef.fritz@med.lu.se.
Innocent B Mboya, Email: innocent.mboya@med.lu.se.
Ming Sun, Email: ming.sun@med.lu.se.
Jens Wahlström, Email: jens.wahlstrom@umu.se.
Bethany van Guelpen, Email: bethany.vanguelpen@umu.se.
Karl Michaëlsson, Email: karl.michaelsson@surgsci.uu.se.
Patrik K E Magnusson, Email: patrik.magnusson@ki.se.
Olle Melander, Email: Olle.Melander@med.lu.se.
Sven Sandin, Email: Sven.Sandin@ki.se.
Weiyao Yin, Email: weiyao.yin.2@ki.se.
Ylva Trolle Lagerros, Email: Ylva.Trolle@ki.se.
Bright Nwaru, Email: bright.nwaru@gu.se.
Jerzy Leppert, Email: jerzy.leppert@regionvastmanland.se.
Abbas Chabok, Email: Abbas.Chabok@regionvastmanland.se.
Nancy L Pedersen, Email: Nancy.Pedersen@ki.se.
Sölve Elmståhl, Email: solve.elmstahl@med.lu.se.
Karolin Isaksson, Email: karolin.isaksson@med.lu.se.
Christian Ingvar, Email: christian.ingvar@med.lu.se.
Linnea Hedman, Email: linnea.hedman@norrbotten.se.
Helena Backman, Email: helena.backman@norrbotten.se.
Christel Häggström, Email: christel.haggstrom@umu.se.
Tanja Stocks, Email: tanja.stocks@med.lu.se.
Data availability statement
Data may be obtained from a third party and are not publicly available.
References
- 1.World Obesity Federation World obesity Atlas. 2023. https://data.worldobesity.org/publications/?cat=19 Available.
- 2.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chong B, Jayabaskaran J, Kong G, et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the global burden of disease study 2019. E Clin Med. 2023;57:101850. doi: 10.1016/j.eclinm.2023.101850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;143:e984–1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kyrgiou M, Kalliala I, Markozannes G, et al. Adiposity and cancer at major anatomical sites: umbrella review of the literature. BMJ. 2017;356:j477. doi: 10.1136/bmj.j477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhaskaran K, Dos-Santos-Silva I, Leon DA, et al. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53. doi: 10.1016/S2213-8587(18)30288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen C, Ye Y, Zhang Y, et al. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ. 2019;367:l5584. doi: 10.1136/bmj.l5584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karahalios A, English DR, Simpson JA. Change in body size and mortality: a systematic review and meta-analysis. Int J Epidemiol. 2017;46:526–46. doi: 10.1093/ije/dyw246. [DOI] [PubMed] [Google Scholar]
- 9.Alharbi TA, Paudel S, Gasevic D, et al. The association of weight change and all-cause mortality in older adults: a systematic review and meta-analysis. Age Ageing. 2021;50:697–704. doi: 10.1093/ageing/afaa231. [DOI] [PubMed] [Google Scholar]
- 10.Cheng Y-J, Chen Z-G, Wu S-H, et al. Body mass index trajectories during mid to late life and risks of mortality and cardiovascular outcomes: results from four prospective cohorts. E Clin Med. 2021;33:100790. doi: 10.1016/j.eclinm.2021.100790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagner C, Carmeli C, Jackisch J, et al. Life course epidemiology and public health. Lancet Public Health. 2024;9:e261–9. doi: 10.1016/S2468-2667(24)00018-5. [DOI] [PubMed] [Google Scholar]
- 12.Sanaya N, Janusaite M, Dalamaga M, et al. The physiological effects of weight-cycling: a review of current evidence. Curr Obes Rep. 2024;13:35–50. doi: 10.1007/s13679-023-00539-8. [DOI] [PubMed] [Google Scholar]
- 13.Zou H, Yin P, Liu L, et al. Body-weight fluctuation was associated with increased risk for cardiovascular disease, all-cause and cardiovascular mortality: a systematic review and meta-analysis. Front Endocrinol (Lausanne) 2019;10:728. doi: 10.3389/fendo.2019.00728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, et al. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–67. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laugesen K, Ludvigsson JF, Schmidt M, et al. Nordic health registry-based research: a review of health care systems and key registries. Clin Epidemiol. 2021;13:533–54. doi: 10.2147/CLEP.S314959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brooke HL, Talbäck M, Hörnblad J, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32:765–73. doi: 10.1007/s10654-017-0316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barlow L, Westergren K, Holmberg L, et al. The completeness of the Swedish cancer register - a sample survey for year 1998. Acta Oncol. 2009;48:27–33. doi: 10.1080/02841860802247664. [DOI] [PubMed] [Google Scholar]
- 18.Pukkala E, Engholm G, Højsgaard Schmidt LK, et al. Nordic cancer registries - an overview of their procedures and data comparability. Acta Oncol. 2018;57:440–55. doi: 10.1080/0284186X.2017.1407039. [DOI] [PubMed] [Google Scholar]
- 19.Cnattingius S, Källén K, Sandström A, et al. The Swedish medical birth register during five decades: documentation of the content and quality of the register. Eur J Epidemiol. 2023;38:109–20. doi: 10.1007/s10654-022-00947-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ludvigsson JF, Berglind D, Sundquist K, et al. The Swedish military conscription register: opportunities for its use in medical research. Eur J Epidemiol. 2022;37:767–77. doi: 10.1007/s10654-022-00887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Järvholm B, Lewold S, Malchau H, et al. Age, bodyweight, smoking habits and the risk of severe osteoarthritis in the hip and knee in men. Eur J Epidemiol. 2005;20:537–42. doi: 10.1007/s10654-005-4263-x. [DOI] [PubMed] [Google Scholar]
- 22.Hallmans G, Ågren Å, Johansson G, et al. Cardiovascular disease and diabetes in the northern Sweden health and disease study cohort - evaluation of risk factors and their interactions. Scand J Public Health. 2003;31:18–24. doi: 10.1080/14034950310001432. [DOI] [PubMed] [Google Scholar]
- 23.Winkvist A, Klingberg S, Nilsson LM, et al. Longitudinal 10-year changes in dietary intake and associations with cardio-metabolic risk factors in the northern Sweden health and disease study. Nutr J. 2017;16:20. doi: 10.1186/s12937-017-0241-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eriksson M, Holmgren L, Janlert U, et al. Large improvements in major cardiovascular risk factors in the population of northern Sweden: the MONICA study 1986-2009. J Intern Med. 2011;269:219–31. doi: 10.1111/j.1365-2796.2010.02312.x. [DOI] [PubMed] [Google Scholar]
- 25.Van Guelpen B, Hultdin J, Johansson I, et al. Low folate levels may protect against colorectal cancer. Gut. 2006;55:1461–6. doi: 10.1136/gut.2005.085480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris H, Hkansson N, Olofsson C, et al. The Swedish mammography cohort and the cohort of Swedish men: study design and characteristics of two population-based longitudinal cohorts. OA Epidemiol. 2013;1:16. doi: 10.13172/2053-079X-1-2-943. [DOI] [Google Scholar]
- 27.Zagai U, Lichtenstein P, Pedersen NL, et al. The Swedish twin registry: content and management as a research infrastructure. Twin Res Hum Genet. 2019;22:672–80. doi: 10.1017/thg.2019.99. [DOI] [PubMed] [Google Scholar]
- 28.Lichtenstein P, De Faire U, Floderus B, et al. The Swedish twin registry: a unique resource for clinical, epidemiological and genetic studies. J Intern Med. 2002;252:184–205. doi: 10.1046/j.1365-2796.2002.01032.x. [DOI] [PubMed] [Google Scholar]
- 29.Johansen D, Borgström A, Lindkvist B, et al. Different markers of alcohol consumption, smoking and body mass index in relation to risk of pancreatic cancer. A prospective cohort study within the Malmo preventive project. Pancreatology. 2009;9:677–86. doi: 10.1159/000212088. [DOI] [PubMed] [Google Scholar]
- 30.Fava C, Sjögren M, Montagnana M, et al. Prediction of blood pressure changes over time and incidence of hypertension by a genetic risk score in Swedes. Hypertension. 2013;61:319–26. doi: 10.1161/HYPERTENSIONAHA.112.202655. [DOI] [PubMed] [Google Scholar]
- 31.Rukh G, Ahmad S, Ericson U, et al. Inverse relationship between a genetic risk score of 31 BMI Loci and weight change before and after reaching middle age. Int J Obes (Lond) 2016;40:252–9. doi: 10.1038/ijo.2015.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brunkwall L, Jönsson D, Ericson U, et al. The Malmo offspring study (MOS): design, methods and first results. Eur J Epidemiol. 2021;36:103–16. doi: 10.1007/s10654-020-00695-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roswall N, Sandin S, Adami H-O, et al. Cohort profile: the Swedish women’s lifestyle and health cohort. Int J Epidemiol. 2017;46:e8. doi: 10.1093/ije/dyv089. [DOI] [PubMed] [Google Scholar]
- 34.Trolle Lagerros Y, Hantikainen E, Mariosa D, et al. Cohort profile: the Swedish national march cohort. Int J Epidemiol. 2017;46:795–795e. doi: 10.1093/ije/dyw193. [DOI] [PubMed] [Google Scholar]
- 35.Nwaru BI, Ekerljung L, Rådinger M, et al. Cohort profile: the West Sweden asthma study (WSAS): a multidisciplinary population-based longitudinal study of asthma, allergy and respiratory conditions in adults. BMJ Open. 2019;9:e027808. doi: 10.1136/bmjopen-2018-027808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenblad A, Nilsson G, Leppert J. Intelligence level in late adolescence is inversely associated with BMI change during 22 years of follow-up: results from the WICTORY study. Eur J Epidemiol. 2012;27:647–55. doi: 10.1007/s10654-012-9713-7. [DOI] [PubMed] [Google Scholar]
- 37.Rissanen R. A snapshot of an eCohort: a comparison of the lifegene population at baseline with the Swedish general population. Scand J Public Health. 2022;50:930–4. doi: 10.1177/14034948211047776. [DOI] [PubMed] [Google Scholar]
- 38.Dunder L, Salihovic S, Lind PM, et al. Plasma levels of Per- and polyfluoroalkyl substances (PFAS) are associated with altered levels of proteins previously linked to inflammation, metabolism and cardiovascular disease. Environ Int. 2023;177:107979. doi: 10.1016/j.envint.2023.107979. [DOI] [PubMed] [Google Scholar]
- 39.Lind L, Elmståhl S, Bergman E, et al. Epihealth: a large population-based cohort study for investigation of gene-lifestyle interactions in the pathogenesis of common diseases. Eur J Epidemiol. 2013;28:189–97. doi: 10.1007/s10654-013-9787-x. [DOI] [PubMed] [Google Scholar]
- 40.Lindqvist PG, Landin-Olsson M, Olsson H. Low sun exposure habits is associated with a dose-dependent increased risk of hypertension: a report from the large MISS cohort. Photochem Photobiol Sci. 2021;20:285–92. doi: 10.1007/s43630-021-00017-x. [DOI] [PubMed] [Google Scholar]
- 41.Backman H, Hedman L, Stridsman C, et al. A population-based cohort of adults with asthma: mortality and participation in a long-term follow-up. Eur Clin Respir J. 2017;4:1334508. doi: 10.1080/20018525.2017.1334508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schyllert C, Lindberg A, Hedman L, et al. Socioeconomic inequalities in asthma and respiratory symptoms in a high-income country: changes from 1996 to 2016. J Asthma. 2023;60:185–94. doi: 10.1080/02770903.2022.2039937. [DOI] [PubMed] [Google Scholar]
- 43.Johansson K, Hutcheon JA, Stephansson O, et al. Pregnancy weight gain by gestational age and BMI in Sweden: a population-based cohort study. Am J Clin Nutr. 2016;103:1278–84. doi: 10.3945/ajcn.115.110197. [DOI] [PubMed] [Google Scholar]
- 44.Robertson J, Lindgren M, Schaufelberger M, et al. Body mass index in young women and risk of cardiomyopathy: a long-term follow-up study in Sweden. Circulation. 2020;141:520–9. doi: 10.1161/CIRCULATIONAHA.119.044056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Persson CE, Adiels M, Björck L, et al. Young women, body size and risk of atrial fibrillation. Eur J Prev Cardiol. 2018;25:173–80. doi: 10.1177/2047487317740644. [DOI] [PubMed] [Google Scholar]
- 46.Tuomela J, Kaprio J, Sipilä PN, et al. Accuracy of self-reported anthropometric measures - findings from the finnish twin study. Obes Res Clin Pract. 2019;13:522–8. doi: 10.1016/j.orcp.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–73. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 48.Spencer EA, Roddam AW, Key TJ. Accuracy of self-reported waist and hip measurements in 4492 EPIC-Oxford participants. Public Health Nutr. 2004;7:723–7. doi: 10.1079/phn2004600. [DOI] [PubMed] [Google Scholar]
- 49.Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 51.Ludvigsson JF, Svedberg P, Olén O, et al. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;34:423–37. doi: 10.1007/s10654-019-00511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gudbjörnsdottir S, Cederholm J, Nilsson PM, et al. The national diabetes register in Sweden: an implementation of the St. Vincent declaration for quality improvement in diabetes care. Diabetes Care. 2003;26:1270–6. doi: 10.2337/diacare.26.4.1270. [DOI] [PubMed] [Google Scholar]
- 53.Swedish National Diabetes Register 20 years of successful improvements. 2016. https://www.ndr.nu/pdfs/20%20years%20of%20successful%20improvements_lowres_singelpage.pdf Available.
- 54.Van Hemelrijck M, Wigertz A, Sandin F, et al. Cohort profile: the national prostate cancer register of Sweden and prostate cancer data base Sweden 2.0. Int J Epidemiol. 2013;42:956–67. doi: 10.1093/ije/dys068. [DOI] [PubMed] [Google Scholar]
- 55.Tomic K, Sandin F, Wigertz A, et al. Evaluation of data quality in the national prostate cancer register of Sweden. Eur J Cancer. 2015;51:101–11. doi: 10.1016/j.ejca.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 56.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Forsberg LR, Jacobsson A, Nyqvist K, et al. Kvalitet och Innehåll I Patientregistret. Utskrivningar Från Slutenvården 1964-2007 och Besök I Specialiserad Öppenvård (exklusive primärvårdsbesök) 1997-2007. 2009. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2009-125-15_200912515_rev2.pdf Available.
- 58.Wettermark B, Hammar N, Fored CM, et al. The new Swedish prescribed drug register--opportunities for Pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16:726–35. doi: 10.1002/pds.1294. [DOI] [PubMed] [Google Scholar]
- 59.Ludvigsson JF, Almqvist C, Bonamy A-KE, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31:125–36. doi: 10.1007/s10654-016-0117-y. [DOI] [PubMed] [Google Scholar]
- 60.Swedish Social Insurance Agency Sjukpenning och Rehabiliteringspenning Midas, version 1.02. 2024. http://www.forsakringskassan.se Available.
- 61.World Health Organization . Geneva: 2000. Obesity: preventing and managing the global epidemic. report of a WHO consultation. part 1: the problem of overweight and obesity. [PubMed] [Google Scholar]
- 62.World Health Organisation . Geneva: 2008. Waist circumference and waist-hip ratio: report of a WHO expert consultation. [Google Scholar]