Abstract
Background
Antimicrobial use (AMU) in livestock contributes to antimicrobial resistance (AMR) among zoonotic pathogens, such as non-typhoid Salmonella (NTS). Since 2009, the Netherlands has made substantial efforts to reduce AMU in livestock.
Objectives
To assess the association between AMU in livestock and AMR in NTS human isolates. Additionally, associations between AMU in broilers/pigs and AMR in NTS broiler/pig isolates, and between AMR in broilers/pigs and in human NTS isolates were assessed. The focus was on Salmonella Enteritidis (SE) and Salmonella Typhimurium including its monophasic variant (ST/STM).
Methods
A national population registry-based study was conducted in the Netherlands from 2008 to 2019. Multivariable logistic regression models were used to assess the associations between livestock AMU and NTS resistance proportion in humans and broilers/pigs, overall as well as per class-specific antimicrobials. Correlation analysis was performed to relate AMR proportions between human and broiler/pig NTS isolates.
Results
For SE, only a positive association between penicillins use in broilers and resistance to ampicillin among human isolates was significant. For ST/STM, most associations between AMU in livestock and AMR among human isolates were significantly positive, overall and per class-specific antimicrobials, namely for penicillins-ampicillin, tetracyclines-tetracycline and sulfonamides/trimethoprim-sulfamethoxazole/trimethoprim. Significantly positive associations between AMU in broilers/pigs and AMR in broiler/pig ST/STM isolates were also observed, but not between broiler/pig and human AMR levels.
Conclusions
Significant associations were generally found between livestock AMU and AMR in human and broiler/pig ST/STM isolates. However, confounding factors, such as imported meat and travel are of concern. To fully comprehend the impact of livestock AMU on resistance in human NTS isolates, it is imperative to enhance AMR surveillance of NTS.
Keywords: Antimicrobial use, Livestock, Drug resistance, Salmonellosis
1. Introduction
Non-typhoid Salmonella (NTS) is one of the leading zoonotic pathogens in the European Union (EU) [1]. In the Netherlands, an estimated ∼20,000 symptomatic NTS infections occur yearly [2], mainly caused by serotypes Enteritidis (SE) and Typhimurium (ST), including its monophasic variant (STM) [[3], [4], [5]]. While SE is a poultry-adapted serotype, ST/STM has a wide range of animal hosts, such as pigs, cattle, and poultry [3,4]. NTS infection can be acquired through consumption of contaminated food, direct contact with animals, the environment, and, to a limited extent, via person-to-person transmission [6]. Although most NTS infections usually cause self-limited mild diarrheal symptoms, the pathogen can sometimes cause invasive infections that can become life-threatening, requiring hospitalization and antimicrobial treatment [7].
Antimicrobial resistance (AMR) plays part in the ecological success of NTS in animal reservoirs, thereby indirectly affecting the magnitude of human exposure to NTS [8]. Antimicrobial use (AMU) in livestock can lead to AMR emergence and spread among NTS isolates in these animals, which can then be transmitted to humans, primarily via the consumption of contaminated food of animal origin [9,10]. In addition to preventive and therapeutic use, antimicrobials have also been used as growth promoters for livestock in the EU until their ban in 2006 due to increasing evidence and concerns about the public health impact of such AMU [11,12]. Despite the ban, the Netherlands still ranked as the highest antimicrobial consumer per biomass unit of animal production in 2007, possibly due to the loss of prophylactic benefits from antimicrobials used as growth promoters, resulting in increased therapeutic use [13]. This led to the enforcement of an ambitious policy to reduce AMU in livestock by 20%, 50% and 70% in 2011, 2013, and 2015, respectively, compared with 2009 [11]. As a result, a 77% AMU reduction was achieved by 2022 [14] through more transparency in prescriptions, increased vaccination, among other interventions [11].
Thanks to the AMU reduction in livestock, resistance levels in ubiquitous microorganisms, such as commensal Escherichia coli, have decreased in livestock during 2009–2014 [15,16]. However, it is largely unknown if the observed reduction in AMU has affected the AMR levels in human infections caused by zoonotic pathogens such as NTS. Evaluating such impact is challenging, as it would require conducting interventional studies for a more accurate assessment. However, observing a link between AMU in animals and AMR in humans through monitoring human food intake until infection with a resistant strain of animal origin occurs, would be impractical and ethically questionable. Therefore, using national surveillance data for the two most common NTS serotypes reported in the Netherlands (SE and ST/STM) from 2008 to 2019, we assessed the temporal association between AMU in major livestock sectors (i.e., broiler, pigs, and cattle) and the occurrence of resistance to clinically relevant antimicrobials among human NTS isolates. Furthermore, we assessed the temporal association between AMU and AMR in broilers/pigs, as well as between AMR in broiler/pig and human NTS isolates.
2. Material and methods
2.1. Antimicrobial use and resistance data
Data sources and collection can be found in Supplementary material: Data sources and collection. Data on the annual AMU from broiler, dairy cattle, veal calf, and pig farming sectors and the corresponding pharmacotherapeutic groups were obtained from Wageningen Economic Research between 2008 and 2011, expressed as Defined Daily Dose per Animal per Year (DDDA/Y). From 2012 to 2019, data were collected from the Netherlands Veterinary Medicine Authority, expressed as the Defined Daily Dose per livestock farm per year (DDDAnat). Antimicrobial groups were selected homologous to the ones used in humans: penicillins, amphenicols, fluoroquinolones, quinolones, first-second-generation cephalosporines, third-fourth-generation cephalosporins, aminoglycosides, tetracyclines, and sulfonamides/trimethoprim. The total annual AMU per livestock sector, including those antimicrobials not used in humans, was also included.
Because NTS is not a commensal in humans (i.e., humans are not a reservoir for NTS), and as in countries like the Netherlands most NTS isolates in humans originate from animals [[3], [4], [5]], AMU in humans was not considered.
SE and ST/STM isolates from humans and livestock with available AMR profiling between January 2008 and December 2019 were retrieved from the Dutch national surveillance programme. Repeated isolates with the same serotype from the same patient were excluded if samples were taken within 90 days from each other [17]. Patients with reported travel history outside the Netherlands were also excluded. For livestock isolates, only isolates from broilers/pigs were selected, as isolates from the cattle sector were not reported in consecutive years during the study period. Gathering data on isolates from imported livestock and their products was not possible in this study. Minimum inhibitory concentration values were used to classify the isolates as resistant or susceptible based on the epidemiological cut-offs set by the European Committee on Antimicrobial Susceptibility Testing. Only antimicrobials tested consistently over the study period in both human and broiler/pig isolates were considered. This panel of antimicrobials consisted of ampicillin (AMP), ceftazidime (CAZ), ciprofloxacin (CIP), chloramphenicol (CHL), cefotaxime (CTX), gentamicin (GEN), nalidixic-acid (NAL), sulfamethoxazole (SMX), tetracycline (TET), trimethoprim (TMP). Annual proportion of resistance per each antimicrobial was determined as the number of resistance isolates to a specific antimicrobial divided by the total number isolates tested for that specific antimicrobial per serotype. Resistance proportion to ≥1 antimicrobial (R ≥ 1 AM) was defined as the total annual number of isolates resistant to at least one tested antimicrobial divided by the total annual number of isolates with that serotype tested for AMR per serotype.
2.2. Statistical analysis
AMR data were described as resistance percentages and AMU as medians with corresponding interquartile range (IQR) per livestock sector for the whole study period. To assess significance of inter-annual trends in AMR in humans, logistic regression models were used, with the explanatory variable being the sampling year and the annual resistance proportion as the response variable.
Referring to Fig. 1, the following analyses were performed: (A) To assess the association of AMU in livestock with AMR in NTS human isolates, per homologous antimicrobials or Total AMU – R ≥ 1 AM, logistic regression models were used, with the explanatory variable being the annual AMU and the annual resistance proportion as the outcome variable. Assuming a delayed effect of AMU in livestock on AMR in humans, a temporal lag of one year ( was included in the model. Only for the analyses per homologous antimicrobials, the use of other antimicrobials than the one under study was controlled for potential (co-)selection effects. Associations were expressed as Odds Ratios (ORs) with their 95% Confidence Intervals (CIs) and visualized using forest plots. (B) To assess the association of AMU in broilers/pigs with AMR in in broiler/pig isolates, per homologous antimicrobials or Total AMU – R ≥ 1 AM, logistic regression models were used, with the annual AMU being the explanatory variable and the annual resistance proportion as the outcome variable. For the analyses per homologous antimicrobials, the use of other antimicrobials than the one under study was also included in the models. No temporal lags were included here and ORs with their 95% CIs were obtained. (C) To assess the correlation between resistance proportion in NTS broiler/pig and human isolates per homologous antimicrobials or R ≥ 1 AM, Kendall-rank based correlation test was used, as linearity of the correlation could not be assumed [18]. A temporal lag of one year on the annual AMR prevalence in humans was used as the outcome variable. Coefficient (τ) estimates with their p values between antimicrobials and R ≥ 1 AM were acquired.
Fig. 1.
Schematic overview of the associations assessed in this study: (A) antimicrobial use (AMU) in livestock – antimicrobial resistance (AMR) in human non-typhoid Salmonella (NTS) isolates, (B) AMU in broilers/pigs – AMR in NTS broiler/pig isolates, (C) AMR in NTS broiler/pig isolates – AMR in NTS human isolates. AMR in human NTS isolates related to travel outside the Netherlands were excluded. However, this is not always reported in the Dutch surveillance system. In this study, it was not possible to adjust for imported food of animal origin.
Because poultry is the primary animal reservoir for SE, and poultry, cattle, and pigs for STM, analyses were conducted as follows (Fig. 1): A) association between AMU in broilers and AMR in human SE infections; association between AMU in broilers/cattle/pigs and AMR in human ST/STM infections; B) association between AMU in broilers/pigs and AMR in broiler/pig SE-ST/STM isolates, C) correlations between AMR in broiler/pig SE-ST/STM isolates and human SE-ST/STM isolates. Only antimicrobials with at least 5 resistant counts per year, serotype, or livestock sector in the AMR data, and antimicrobial groups with DDDA/Y-DDDAnat > 0.5 in all years in the AMU data across livestock sectors were modelled to allow for model convergence and reliable estimates. Multicollinearity was tested using the variance inflator factor (VIF) and predictors with VIF > 4 were excluded. A Bonferroni correction for multiple testing was applied to analyses between homologous antimicrobials. Unless stated otherwise, the p values were set to 0.05. All analyses were performed using the statistical R software, version 4.30.
3. Results
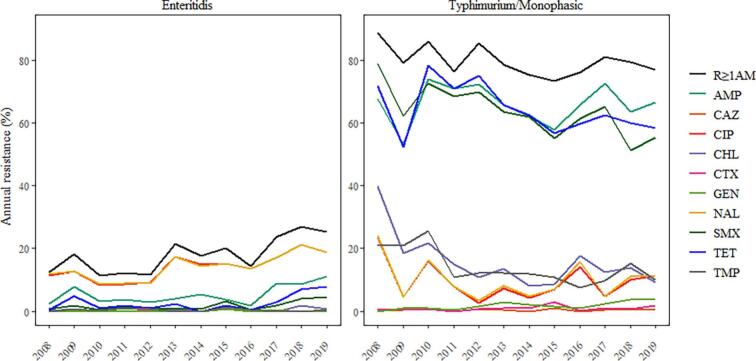
Fig. 2 depicts the annual AMR in humans by serotype in the Netherlands from 2008 to 2019. In total, 7390 human NTS isolates were tested for antimicrobial susceptibility from January 2008 to December 2019. Of these, 2947 were SE and 4443 were ST/STM isolates, with generally higher AMR levels among ST/STM isolates. Among SE isolates, the highest resistance percentages were observed for CIP and NAL (both 13%), whereas among ST/STM isolates, the highest resistant percentage were observed for AMP (67%). Supplementary material: Appendix A: Descriptive results: Table A.1. Description of the resistance patterns in NTS broiler/pig isolates can be found in Supplementary material: Appendix A: Descriptive results: Table A.2 & Fig. A.1.
Fig. 2.
Annual antimicrobial resistance (AMR) percentages in non-typhoid Salmonella (NTS) human isolates by serotype in the Netherlands (2008–2019). Resistance to ≥1 antimicrobial (R ≥ 1 AM) percentage per serotype was calculated using the total annual number of isolates resistant to at least one the following tested antimicrobials: ampicillin (AMP), ceftazidime (CAZ), ciprofloxacin (CIP), chloramphenicol (CHL), cefotaxime (CTX), gentamicin (GEN), nalidixic-acid (NAL), sulfamethoxazole (SMX), tetracycline (TET), trimethoprim (TMP), divided by the total annual number of isolates with that serotype tested for antimicrobial susceptibility per serotype.
Fig. 3 shows the annual AMU by livestock sector in the Netherlands from 2008 to 2019. Among all livestock sectors, the highest total AMU was reported in veal calves (median values: 21.8). Meanwhile, the lowest total use was observed in dairy cattle (median values: 3.7). Supplementary material: Appendix A: Descriptive results: Table A.3. Between 2008 and 2019, broilers (−73%) and pigs (−60%) experienced the largest decline in AMU, followed by dairy cattle (−55%) and veal calves (−46%).
Fig. 3.
Annual antimicrobial use (AMU) by livestock sector in the Netherlands (2008–2019). Total AMU also includes groups of antimicrobials not used in humans. *DDDA/Y: 2008–2011, DDDAnat: 2012–2019.
3.1. Long-term trends of AMR in SE and ST/STM human isolates
Overall, R ≥ 1 AM among human SE isolates increased significantly by 8% every year. Contrary to SE, R ≥ 1 AM among human ST/STM isolates decreased significantly by 5% every year. Supplementary material: Appendix A: Descriptive results: Table A.4.
3.2. Associations between AMU in livestock and AMR in NTS human isolates
Fig. 4 shows the adjusted ORs with 95%CIs for the associations between AMU in livestock and AMR in human NTS isolates.
Fig. 4.
Associations between antimicrobial use (AMU) in livestock and antimicrobial resistance (AMR) in human non-typhoid Salmonella infections in the Netherlands (2008–2019). Analyses for Typhimurium/Monophasic isolates were assessed in poultry, cattle (veal calf and dairy cattle), and pigs, whereas in Enteritidis isolates only in poultry. Adjusted for a lag of one year prior of AMR and the use of other antimicrobials. Analysis per homologous antimicrobials: number of tests 4–5; Bonferroni correction: 0.05/4–5 = 0.01 for Enteritidis & Broilers, Typhimurium/Monophasic & Broilers, Typhimurium/Monophasic & Veal calves, and Typhimurium/Monophasic & Pigs; not applicable for Typhimurium/Monophasic & Dairy cattle. Resistance to ≥1 antimicrobial (R ≥ 1 AM) proportion per serotype was calculated using the total annual number of isolates resistant to at least one the following tested antimicrobials: ampicillin(AMP), ceftazidime(CAZ), ciprofloxacin(CIP), chloramphenicol(CHL), cefotaxime(CTX), gentamicin(GEN), nalidixic-acid(NAL), sulfamethoxazole(SMX), tetracycline(TET), trimethoprim(TMP), divided by the total annual number of isolates with that serotype tested for antimicrobial susceptibility per serotype and/or animal sector. Total AMU in animals also included antimicrobials not used for humans.
Total AMU in broiler, dairy cattle, veal calf, and pig livestock sectors showed significantly positive associations over the years with R ≥ 1 AM in ST/STM human isolates only, i.e., the odds for a ST/STM human isolate to be resistant decreased as the AMU in livestock decreased as well.
Per homologous antimicrobials (Bonferroni correction: p value = 0.01), only a significant positive association was observed for SE human isolates whose odds of resistance to AMP decreased as penicillins use in broiler decreased (OR: 1.17, 95%CI: 1.07–1.27). Similarly, among ST/STM human isolates, the odds of resistance to NAL (OR: 1.17, 95%CI:1.13–1.21), TET (OR: 1.09, 95%CI:1.05–1.14), TMP (OR: 1.37, 95%CI:1.24–1.51), and SMX (OR: 1.54, 95%CI:1.36–1.74] decreased as the use of their homologous antimicrobials in broilers decreased. An exception was found for penicillins use in broilers and resistance to AMP in ST/STM human isolates, where a significant negative association was found (OR: 0.90, 95%CI: 0.88–0.93).
In addition, the odds for a human ST/STM isolate to be resistant to AMP (OR: 1.62, 95%CI: 1.28–2.06), TET (OR: 1.06, 95%CI: 1.02–1.10,), TMP (OR: 1.63, 95%CI: 1.36–1.97), and SMX (OR: 1.59, 95%CI: 1.40–1.80) decreased as the use of their homologous antimicrobials decreased in veal calves. Conversely, a significant negative association was observed between the use of amphenicols in veal calves and resistance to CHL among human ST/STM isolates (OR: 0.41, 95% CI: 0.33–0.51). Finally, the odds for a ST/STM human isolate to be resistant to TET (OR: 1.05, 95%CI: 1.02–1.07), TMP (OR: 1.41, 95%CI: 1.28–1.56), and SMX (OR: 1.20, 95%CI: 1.09–1.33) decreased as the use of their homologous antimicrobials. Supplementary material: Appendix B: Main and secondary results: Table B.1.
3.3. Associations between AMU in broilers/pigs and AMR in NTS from broiler/pig isolates
Due to lower resistant counts per year in SE isolates from broilers, AMU in broilers and AMR in broiler SE isolates was not assessed. Total AMU in broilers was significantly positive associated with R ≥ 1 AM in broiler ST/STM isolates over the study years, whereas this was not observed in broiler SE isolates. At the homologous-antimicrobials level (Bonferroni correction: p values = 0.01 for AMU-AMR in broilers and 0.02 for AMU-AMR in pigs), the odds of resistance to SMX among broiler ST/STM isolates decreased as the use of sulfonamides/trimethoprim in broilers decreased (OR: 1.66, 95%CI: 1.15–2.40, p = 0.007). Similarly, the odds of resistance to AMP among pig ST/STM isolates declined as the use of penicillins in pigs declined (OR: 2.93, 95%CI: 1.74–4.91, p < 0.001). Supplementary material: Appendix B: Main and secondary results: Table B.2.
3.4. Correlations between AMR in ST/STM isolates from broilers/pigs and ST/STM human isolates
Due to lower resistant counts per year in SE isolates from broilers, AMR in SE isolates was not assessed. Non-significant correlations were found overall as well as per antimicrobial. Supplementary material: Appendix B: Main and secondary results: Table B.3.
4. Discussion
For SE, only a significant and positive association could only be observed between penicillins use in broilers and AMP resistance in human SE isolates. Moreover, while the AMR levels among human SE isolates increased over the years, they remained considerably lower than for ST/STM. Several factors may explain the limited associations observed for SE. First, the primary livestock reservoir of SE is laying hens (mainly transmitting infection to humans via eggs) and less often broilers [3,4]. In our study, AMU in laying hens were too low to allow for analysis. Second, in the Netherlands, AMR in SE is more likely to be acquired abroad than ST/STM [19]. Thus, even though we excluded cases with known travel history, a number of cases with unknown travel history might have been travel-related and therefore included in the analysis, as this is optional to fill in on the laboratory form. Lastly, SE outbreaks have increasingly been linked to imported eggs [[20], [21], [22]]. This may suggest that SE transmission is more likely to occur through imported food and/or increased travel behavior. Therefore, the reduction of AMU in the Dutch broiler sector did not significantly change AMR in SE isolates.
As for ST/STM, in general, significant and positive associations between AMU in broiler, cattle, and pig sectors and AMR in human ST/STM isolates were observed, overall as well as per homologous antimicrobials, such as penicillins-AMP, tetracyclines-TET, trimethoprim/sulfonamides-TMP, and trimethoprim/sulfonamides-SMX. In addition, there was a marked decrease in the overall levels of resistance among human ST/STM isolates. Nevertheless, few (positive) associations of AMU in broilers/pigs with AMR in ST/STM isolates from broilers/pigs were observed, such as sulfonamides/trimethoprim-SMX, and penicillins-AMP. ST/STM has a broader range of animal reservoirs compared to SE [3,4] and it is more prevalent in the Netherlands [19]. As such, changes in AMR were more evident in ST/STM than SE.
The recent JIACRA report, which assessed similar associations to the ones studied here but at the European level [23], found significant associations between the use of aminopenicillins and aminopenicillins resistance in Salmonella isolates from food-producing animals. This is consistent with our results, although the associations were borderline significant for broilers. They also found a relation between fluoroquinolone use and CIP resistance in Salmonella from poultry, while only quinolone use in broilers was associated with NAL resistance in human ST/STM isolates in our study.
AMU in humans was not considered in the analyses. Firstly, NTS is not a naturally occurring microorganism in the human gut microflora. Furthermore, humans are considered a ‘dead-end’ host for NTS, which means that the microorganism cannot maintain a population in humans. This limited biological plausibility makes it unlikely for NTS to evolve and develop AMR upon exposure to AMU in humans [24]. Secondly, the primary source of human SE and ST/STM infections in the Netherlands is mostly via contaminated food of animal origin, whereas human-to-human transmission is rare [[3], [4], [5]]. As such, NTS strains in humans would generally be resistant or susceptible to antimicrobials from the selection pressure exerted in the livestock reservoirs, with very restrained selective pressure from the antimicrobials used in humans.
The limited associations with AMR in the broiler/pig sector may also be due to limited representativeness of these data. The NTS isolates from broiler/pigs were collected by various veterinary/food safety organizations and private laboratories in the country, which used different sampling and monitoring methods. Thus, it is unknown to which extent the samples were taken from diseased or healthy animals or to which extent these samplings cover the total presence of NTS among livestock. This could result in under/overestimation of AMR and selection bias in the monitoring of animal isolates. Since 2021, there have been significant improvements in AMR monitoring and reporting for cattle, pigs and poultry in the new European legislation [25]. For instance, the isolation of NTS from cecal samples of veal calves and pigs collected at slaughterhouses has been included to increase the number of NTS isolates from livestock. Hence, it is recommended to use this more representative data within both animal and human populations over an extended period for future assessment.
Although most associations were significantly positive, meaning that as AMU decreases, so does AMR, there were a few instances where significantly negative associations were observed. This can be due to the ecological nature of our study, where the unit of analysis was at the (annual) national level of AMU/AMR (at the population level), whereas several other unmeasured factors at the individual level related to AMU or AMR in both humans and animals were not possible to take into account. Moreover, the absence of fine-scale temporality to detect monthly shifts in AMU and AMR, did not allow us to capture seasonal patterns, especially relevant given the seasonal exposure of human NTS in the Netherlands, where the incidence is higher during warmer seasons. Additionally, it was not possible to account for variation in the pathways involved between AMU and AMR in humans and animals, the amount of imported and consumed animal-food and geographical differences within the country [26]. Ultimately, while our findings offer insights into potential associations, they do not establish causality.
5. Conclusions
AMU in livestock was significantly associated with AMR in human NTS isolates, especially for ST/STM. To a lesser extent, significantly positive associations between AMU in broilers/pigs and AMR in ST/STM isolates from broilers/pigs were also observed, whereas no significant correlations between AMR in ST/STM from broilers/pigs and humans were found. However, concerns remain that a number of human infections result from imported meat and foreign travel. A more comprehensive evaluation of these associations using data that is more representative of NTS isolates from livestock over a longer time period is needed to gather further evidence of livestock contribution to the burden of AMR in NTS. It is also advisable to compare these findings with forthcoming similar studies in countries that serve as primary trading partners for livestock, as well as animal product markets, between the Netherlands and other regions.
Funding
This study was supported by the research project “Effects of decreaSing AntiBiotic use in animaLs on antibiotic reSistance in Human infections” (EStABLiSH) funded through the Netherlands Organization for Health Research and Development (ZonMw) (Grant number: 541003002).
Ethics
The present study was performed on deidentified surveillance and annual reported data collected for public health surveillance, thus no ethics approval was required.
CRediT authorship contribution statement
Linda E. Chanamé Pinedo: Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Anouk P. Meijs: Formal analysis, Investigation, Methodology, Writing – review & editing. Huifang Deng: Conceptualization, Formal analysis, Investigation, Writing – review & editing. Sabine C. de Greeff: Conceptualization, Methodology, Writing – review & editing. Engeline van Duijkeren: Conceptualization, Funding acquisition, Investigation, Methodology, Writing – original draft. Cindy M. Dierikx: Funding acquisition, Investigation, Methodology, Writing – review & editing. Kees T. Veldman: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing. Pim Sanders: Data curation, Methodology, Resources, Writing – review & editing. Maaike J.C. van den Beld: Data curation, Investigation, Methodology, Resources, Writing – review & editing. Bart Wullings: Conceptualization, Funding acquisition, Investigation, Resources, Writing – review & editing. Eelco Franz: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. Roan Pijnacker: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Supervision, Writing – review & editing. Lapo Mughini-Gras: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft.
Declaration of competing interest
The authors of the present study declare no competing interests.
Acknowledgments
We wish to thank the Netherlands Organization for Health Research and Development (ZonMw) for funding this study. Also, thanks to Wageningen Economic Research (formerly known as the Agricultural Economic Institute (LEI) Wageningen UR) and the Veterinary Medicine Authority (SDa), who kindly provided the antimicrobial use data in livestock animals in the Netherlands. Also, thanks to all medical and veterinary laboratories for submitting their Salmonella isolates.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2024.100844.
Appendix A. Supplementary data
Supplementary material: Data sources and collection; Appendix A: Descriptive result; Appendix B: Main and secondary results
Data availability
Data will be made available upon formal request and supervision by the RIVM.
References
- 1.European Centre for Disease Prevention and Control (ECDC) and European Food Safety Authority (EFSA). The European Union One Health 2019 Zoonoses Report. EFSA J. 2020;19:06406. doi: 10.2903/j.efsa.2021.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Public Health and the Environment (RIVM) Disease burden of food-related pathogens in the Netherlands. 2021. http://hdl.handle.net/10029/626297
- 3.Mughini-Gras L., Enserink R., Friesema I., Heck M., van Duynhoven Y., van Pelt W. Risk factors for human salmonellosis originating from pigs, cattle, broiler chickens and egg laying hens: a combined case-control and source attribution analysis. PloS One. 2014;9:87933. doi: 10.1371/journal.pone.0087933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mughini-Gras L., Smid J., Enserink R., Franz E., Schouls L., Heck M., van Pelt W. Tracing the sources of human salmonellosis: a multi-model comparison of phenotyping and genotyping methods. Infect. Genet. Evol. 2014;28:251–260. doi: 10.1016/j.meegid.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 5.National Institute for Public Health and the Environment (RIVM) State of Zoonoses 2020. 2021. http://hdl.handle.net/10029/625375
- 6.Dekker J.P., Frank K.M. Salmonella, Shigella, and yersinia. Clin. Lab. Med. 2015;35:225–246. doi: 10.1016/j.cll.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acheson D., Hohmann E.L. Nontyphoidal Salmonellosis. Clin. Infect. Dis. 2011;32:263–269. doi: 10.1086/318457. [DOI] [PubMed] [Google Scholar]
- 8.Barza M., Travers K. Excess infections due to antimicrobial resistance: the “attributable fraction”. Clin. Infect. Dis. 2002;34:126–130. doi: 10.1086/340250. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization (WHO) 2006. Antimicrobial use in aquaculture and antimicrobial resistance: report of a joint FAO/OIE/WHO expert consultation on antimicrobial use in aquaculture and antimicrobial resistance.https://www.fao.org/3/bq500e/bq500e.pdf [Google Scholar]
- 10.Aarestrup F.M. Veterinary drug usage and antimicrobial resistance in bacteria of animal origin. Basic Clin. Pharmacol. Toxicol. 2005;96:271–281. doi: 10.1111/j.1742-7843.2005.pto960401.x. [DOI] [PubMed] [Google Scholar]
- 11.Speksnijder D.C., Mevius D.J., Bruschke C.J., Wagenaar J.A. Reduction of veterinary antimicrobial use in the Netherlands. The Dutch success model. Zoonoses Public Health. 2015;62:79–87. doi: 10.1111/zph.12167. [DOI] [PubMed] [Google Scholar]
- 12.European Union Commission . 2005. Ban on antibiotics as growth promoters in animal feed enters into effect.https://ec.europa.eu/commission/presscorner/detail/en/IP_05_1687 [Google Scholar]
- 13.Grave K., Torren-Edo J., Mackay D. Comparison of the sales of veterinary antibacterial agents between 10 European countries. J. Antimicrob. Chemother. 2010;65:2037–2040. doi: 10.1093/jac/dkq247. [DOI] [PubMed] [Google Scholar]
- 14.The Netherlands Veterinary Medicine Authority (SDa) 2023. Usage of antibiotics in agricultural livestock in 2022.https://cdn.i-pulse.nl/autoriteitdiergeneesmiddelen/userfiles/sda%20jaarrapporten%20ab-gebruik/AB-rapport%202022/def-sda-rapport-met-brief---het-gebruik-van-antibiotica-bij-landbouwhuisdieren-in-2022-erratum20230912(1).pdf [Google Scholar]
- 15.Dorado-García A., Mevius D.J., Jacobs J.J., Van Geijlswijk I.M., Mouton J.W., Wagenaar J.A., Heederik D.J. Quantitative assessment of antimicrobial resistance in livestock during the course of a nationwide antimicrobial use reduction in the Netherlands. J. Antimicrob. Chemother. 2016;71:3607–3619. doi: 10.1093/jac/dkw308. [DOI] [PubMed] [Google Scholar]
- 16.Hesp A., Veldman K., van der Goot J., Mevius D., van Schaik G. Monitoring antimicrobial resistance trends in commensal Escherichia coli from livestock, the Netherlands, 1998 to 2016. Euro Surveill. 2019;24:1800438. doi: 10.2807/1560-7917.ES.2019.24.25.1800438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mughini-Gras L., Pijnacker R., Duijster J., Heck M., Wit B., Veldman K., Franz E. Changing epidemiology of invasive non-typhoid Salmonella infection: a nationwide population-based registry study. Clin. Microbiol. Infect. 2020;26:941. doi: 10.1016/j.cmi.2019.11.015. [DOI] [PubMed] [Google Scholar]
- 18.Puth M.-T., Neuhäuser M., Ruxton G.D. Effective use of Spearman’s and Kendall’s correlation coefficients for association between two measured traits. Anim. Behav. 2015;102:77–84. doi: 10.1016/j.anbehav.2015.01.010. [DOI] [Google Scholar]
- 19.Chaname-Pinedo L., Franz E., Beld M., Veldman K., Pijnacker R., Mughini-Gras L. Increased antimicrobial resistance among non-typhoidal Salmonella infections in international travellers returning to the Netherlands. J. Travel Med. 2023;30:1–4. doi: 10.1093/jtm/taad079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaname Pinedo L., Franz E., van den Beld M., Van Goethem N., Mattheus W., Veldman K., et al. Changing epidemiology of Salmonella Enteritidis human infections in the Netherlands and Belgium, 2006 to 2019: a registry-based population study. Euro Surveill. 2022;27:2101174. doi: 10.2807/1560-7917.ES.2022.27.38.2101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.European Centre for Disease Prevention and Control (ECDC) and European Food Safety Authority (EFSA) 2020. Multi-country outbreak of Salmonella Enteritidis infections linked to eggs, third update – 6 February 2020.https://www.ecdc.europa.eu/sites/default/files/documents/salmonella-enteritidis-infections-multi-country-outbreak-eggs-third-update.pdf [Google Scholar]
- 22.Pijnacker R., Dallman T.J., Tijsma A.S.L., Hawkins G., Larkin L., Kotila S.M., et al. An international outbreak of Salmonella enterica serotype Enteritidis linked to eggs from Poland: a microbiological and epidemiological study. Lancet Infect. Dis. 2019;19:778–786. doi: 10.1016/S1473-3099(19)30047-7. [DOI] [PubMed] [Google Scholar]
- 23.European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), and European Medicines Agency (EMA), Third joint inter-agency report on integrated analysis of consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals in the EU/EEA, JIACRA III (2016–2018), 19, 6 23-164, 10.2903/j.efsa.2021.6712. [DOI] [PMC free article] [PubMed]
- 24.Ahmer B.M., Gunn J.S. Interaction of Salmonella spp. with the intestinal microbiota. Front. Microbiol. 2011;2:101. doi: 10.3389/fmicb.2011.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.European Union. Commission Implementing Decision (EU) 2020. 2020/1729 of 17 November 2020 on the monitoring and reporting of antimicrobial resistance in zoonotic and commensal bacteria and repealing Implementing Decision 2013/652/EU.https://eur-lex.europa.eu/eli/dec_impl/2020/1729/oj [Google Scholar]
- 26.Allel K., Day L., Hamilton A., Lin L., Furuya-Kanamori L., Moore C.E., et al. Global antimicrobial-resistance drivers: an ecological country-level study at the human-animal interface. Lancet Planet Health. 2023;7:291–303. doi: 10.1016/S2542-5196(23)00026-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: Data sources and collection; Appendix A: Descriptive result; Appendix B: Main and secondary results
Data Availability Statement
Data will be made available upon formal request and supervision by the RIVM.