Scalp ringworm is reaching epidemic proportions in parts of Britain's cities. Prompt diagnosis is needed to stop it spreading from child to child, but the varied presentation makes it easy to miss
Scalp ringworm, or tinea capitis, largely disappeared in Great Britain after oral griseofulvin was introduced in the late 1950s.1 Over the past few years, however, dermatology departments in London, Bristol, and Birmingham have seen a large increase in cases, with rates of positive scalp isolates up to 20 times higher than previous baseline rates.2–4 A community point prevalence study from London suggested a disease prevalence of about 2.5% with a carriage rate of between 12% and 47% among schoolchildren.5 AfroCaribbean children seem to be particularly vulnerable to infection.3 Scalp ringworm is also increasing in Europe and North America.6,7 We discuss the current epidemic, illustrate the clinical presentations of the disease, and describe the methods for diagnosis and management.
Summary points
Scalp ringworm is common among innercity children in the United Kingdom
Diagnosis is difficult because of the wide range of clinical presentations
Systemic therapy is required to clear scalp ringworm
The diagnosis should be confirmed by mycological analysis before starting treatment
Antifungal shampoos may reduce the risk of transmission
Methods
We based this review on our extensive clinical experience in managing patients in a dedicated tinea capitis clinic at a teaching hospital. It also draws on information derived from a study assessing the impact of the problem on the local community and a detailed review of English language publications.
Source of infection
Scalp ringworm is caused by the dermatophyte group of fungi. The fungi are classified into three groups according to where they are normally found. Geophilic organisms live in soil, zoophilic organisms on animals, and anthropophilic organisms on humans. Most cases of childhood ringworm in the past 20 years have been due to the zoophilic organisms Microsporum canis (after exposure to an infected puppy or kitten) or Trichophyton verrucosum (from cattle). Recently, however, the predominant organism has changed to an anthropophilic one, T tonsurans, which spreads directly from child to child at home, school, or the hairdresser. This organism is now responsible for most scalp ringworm in Britain's larger cities.3,5 The reason for the change is unclear, but the United Kingdom seems to be repeating a trend observed in the United States 20 years ago.8
Clinical appearances of scalp ringworm
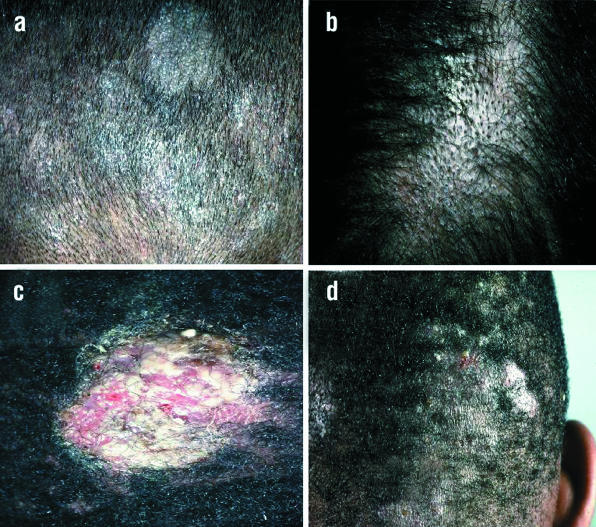
Clinical diagnosis of scalp infection with T tonsurans can be difficult as presentations are wide ranging and variable. It is thus easy for inexperienced clinicians to overlook the diagnosis.9 The presenting features can be divided into six main patterns.
Grey type
—Circular patches of alopecia with marked scaling (fig 1a).
Figure 1.
Four types of scalp ringworm: (a) grey type, (b) black dot, (c) kerion, and (d) diffuse pustules
Black dot
—Swollen stubs of broken off hairs are visible within the patch of alopecia (fig 1b). The dermatophytes invade the inside of the hair shaft, making it fragile and vulnerable to fracture.
Kerion
—Boggy, localised swelling occurs due to an aggressive inflammatory response to the organism (fig 1c). Patients often also have cervical lymphadenopathy (fig 2).
Figure 2.
Painful occipital lymphadenopathy associated with kerion scalp ringworm
Diffuse scale
—This form looks like dandruff, with widespread scale throughout scalp that can be masked with hair oils.
Moth eaten
—Hair loss is patchy, and the underlying scalp may be generally scaly.
Diffuse pustular pattern
—Widespread scattered pustules are seen on the scalp (fig 1d). The inflammatory response is brisk but there is only scanty growth of organisms. There may be associated painful lymphadenopathy.
The pustular type is most difficult to diagnose. Pus usually occurs in bacterial infections, and diffuse pustular tinea capitis is often incorrectly treated with antibiotics. Although there may also be bacterial colonisation, the main pathogen is the dermatophyte.
Confirming the diagnosis
The Wood's light, which was traditionally used to diagnose scalp ringworm, can detect infection with only Microsporum sp. The greenish fluorescence seen under the light is due to an ectothrix infection of hairs, in which fungal spores form a sheath on the outside of the hair. T tonsurans causes an endothrix infection with the spores inside the hair shaft, and there is no fluorescence.
Diagnosis therefore relies on mycological analysis of scalp scale and broken off infected hairs. Samples for analysis can be obtained by scraping the affected area with the blunt side of a scalpel (to avoid slicing through the infected hairs) on to a piece of paper. This technique requires some practice.
Sampling using a soft plastic brush has been shown to be equally effective.10 The friction from massaging the bristles around the affected areas makes the bristles negatively charged so that they pick up hairs and scalp scales. The brush is then sent to the laboratory and used to innoculate an agar plate. Travel toothbrushes are cheap and ideal for this. If possible, both techniques should be used so that samples can be analysed by both microscopy and culture.11
Management
Tinea capitis requires systemic treatment because antifungal creams are unable to penetrate the hair shaft sufficiently to clear the infection.12 Furthermore, the use of topical antifungal treatment alone may contribute to the creation of carriers. The concept of carriers is controversial but describes patients whose symptoms and clinical signs are minimal but who are still mycologically positive and presumed capable of transmitting infection.
The only licensed treatment is oral griseofulvin. It is usually given at a dose of 10 mg/kg for six to eight weeks. However, T tonsurans seems resistant in some cases, and longer treatment may be required at doses of up to 20-25 mg/kg.12 Because treatment takes a long time, it is essential to have a positive mycology result before starting. However, patients with the more aggressive clinical variants, pustular tinea capitis and kerion, should use antifungal creams or shampoos to reduce the risk of progression while waiting for the mycology results.13 The results of microscopy can take a week and culture up to four weeks, and these variants can be painful.
The newer fungicidal drugs such as oral terbinafine and itraconazole are effective in tinea capitis.14,15 Because of their fungicidal action, they require shorter treatments than griseofulvin. However, these drugs are unlicensed for use in children in the United Kingdom.
Patients sometimes develop papules after starting treatment, particularly around the ears and face (fig 3). This is an identity reaction and not an adverse drug reaction. An identity reaction is one that occurs away from the primary lesion and is usually due to an immunological reaction to the causative agent—in this case, the dermatophyte. The treatment should not be stopped.
Figure 3.
Identity reaction showing papules around the ears
Adjuvant therapy
A small randomised trial found that antifungal shampoo (selenium sulphide) increases the rate of eradication, which may reduce the transmissibility of the organism.13 Our experience supports this, and we recommend that children use topical treatments as well as oral drugs.15,16 It is not clear at what stage during treatment a child is free from spores. However, current advice states that once children are receiving adequate treatment (oral and topical) it is safe for them to return to school.16
Conclusion
Scalp ringworm seems to be increasing in the United Kingdom and is reaching epidemic proportions in some areas. T tonsurans is responsible for most of these cases. Doctors should consider scalp ringworm in any child with a scaly scalp in whom a diagnosis of dandruff or scalp eczema has been suspected.16
Additional educational resources
British Association of Dermatology (www.bad.org.uk)
Contains clinical guidelines for management
The Skin Site (www.skinsite.com)
The site contains information sheets for patients
Acknowledgments
We thank the British Society of Paediatric Dermatology for funding the study that provided some of the information for this review, Roderick Hay for help and encouragement, and Claire P Lloyd for comments on the manuscript.
Footnotes
Competing interests: The authors' tinea capitis clinic is funded by Novartis.
References
- 1.Williams DI, Marten RH, Sarkany I. Oral treatment of ringworm with griseofulvin. Lancet. 1958;ii:1212–1213. doi: 10.1016/s0140-6736(58)92363-8. [DOI] [PubMed] [Google Scholar]
- 2.Leeming JG, Elliott TSJ. The emergence of Trichophyton tonsurans tinea capitis in Birmingham, UK. Br J Dermatol. 1995;133:929–931. doi: 10.1111/j.1365-2133.1995.tb06928.x. [DOI] [PubMed] [Google Scholar]
- 3.Fuller LC, Child FC, Higgins EM. Tinea capitis in south east London: an outbreak of Trichophyton tonsurans infection. Br J Dermatol. 1997;136:139. doi: 10.1111/j.1365-2133.1997.tb08771.x. [DOI] [PubMed] [Google Scholar]
- 4.Buckley DM, Moss C, Austin G, Armer J, Leeming JG. Trichophyton tonsurans infection in Birmingham. Br J Dermatol. 1996;135(suppl 47):21. [Google Scholar]
- 5.Hay RJ, Clayton YM, de Silva N, Midgley G, Rosser E. Tinea capitis in south east London—a new pattern of infection with public health implication. Br J Dermatol. 1996;135:955–958. doi: 10.1046/j.1365-2133.1996.d01-1101.x. [DOI] [PubMed] [Google Scholar]
- 6.Elewski BE. Tinea capitis: a current perspective. J Am Acad Dermatol. 2000;42:1–24. doi: 10.1016/s0190-9622(00)90001-x. [DOI] [PubMed] [Google Scholar]
- 7.Hay RJ, Robles W, Midgley D, Moore MK. Tinea capitis in Europe: new perspective on an old problem. J Eur Acad Derm Venerol. 2001;15:229–233. doi: 10.1046/j.1468-3083.2001.00214.x. [DOI] [PubMed] [Google Scholar]
- 8.Bronson DM, Desai DR, Barskey S. An epidemic of infection with Trichophyton tonsurans revealed in a twenty year survey of fungal pathogens in Chicago. J Am Acad Dermatol. 1983;8:322–330. doi: 10.1016/s0190-9622(83)70034-4. [DOI] [PubMed] [Google Scholar]
- 9.Gibbon KL, Goldsmith P, Salisbury JA, Bewley AP. Unnecessary surgical treatment of fungal kerions in children. BMJ. 2000;320:696–697. doi: 10.1136/bmj.320.7236.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fuller LC, Child FC, Midgley G, Hay RJ, Higgins EM. Practical method for the diagnosis of scalp ringworm; validation of the toothbrush technique. J Eur Acad Derm Venerol. 1997;9(suppl 1):209. [Google Scholar]
- 11.Hay RJ, Roberts SOB, McKenzie DWR. Mycology. In: Champion RH, Burton JL, Ebling FJG, editors. Textbook of dermatology. 5th ed. Vol. 2. Oxford: Blackwell; 1998. p. 1151. [Google Scholar]
- 12.Elewski BE. Cutaneous mycoses in children. Br J Dermatol. 1996;134(suppl 46):7–11. doi: 10.1111/j.1365-2133.1996.tb15651.x. [DOI] [PubMed] [Google Scholar]
- 13.Allen HB, Honig PJ, Leyden JJ, McGInley KJ. Selenium sulfide: adjunctive therapy for tinea capitis. Pediatrics. 1982;69:81–83. [PubMed] [Google Scholar]
- 14.Jones TC. Overview of the use of terbinafine (Lamisil) in children. Br J Dermatol. 1995;132:683–689. doi: 10.1111/j.1365-2133.1995.tb00711.x. [DOI] [PubMed] [Google Scholar]
- 15.Fuller LC, Smith CH, Cerio R, Marsden RA, Midgley G, Beard AL, et al. A randomised comparison of four weeks of terbinafine versus eight weeks of griseofulvin for the treatment of tinea capitis—advantages of a shorter treatment schedule. Br J Dermatol. 2001;144:321–327. doi: 10.1046/j.1365-2133.2001.04022.x. [DOI] [PubMed] [Google Scholar]
- 16.Higgins EM, Fuller LC, Smith CE. Guidelines for management of tinea capitis in UK. Br J Dermatol. 2000;143:53–58. doi: 10.1046/j.1365-2133.2000.03530.x. [DOI] [PubMed] [Google Scholar]