ABSTRACT
Public health centers (PHCs, hokenjo in Japanese) are local government authorities responsible for public health in Japan. As of 2010, 494 centers were operating under the Ministry of Health, Labour and Welfare of Japan. While the general rule is that one PHC covers 300,000 inhabitants, several centers cover a population of more than 1 million. The roles of PHCs described in the Community Health Act include 1) propagation and improvement of information on community health, 2) vital statistics and other statistics on community health, 3) improvement of dietary conditions and food sanitation, 4) environmental sanitation including housing, water supply, sewage, waste disposal and public cleaning, 5) medical and pharmaceutical affairs, 6) matters involving public health nurses, 7) promotion and improvement of public medical services, 8) maternal, child, and elderly health, 9) dental health, 10) psychiatric health, 11) health of patients under long-term care due to incurable diseases, 12) prevention of infectious diseases, 13) laboratory tests on sanitation/environment, and 14) other functions needed to maintain/promote health in the community. Among those many roles, infectious disease controls are one of the most important. Concerning tuberculosis control, PHCs are responsible for the isolation of patients, health check-ups of those in close contact with infectious TB patients, and public subsidy of medical expenses for tuberculosis treatments. Food poisoning controls are also an important responsibility of PHCs, as are the conduct of surveys to trace suspicious foods and laboratory testing of samples from patients. To make these many measures effective, sufficient numbers of public health professionals are required.
Key Words: Public health center, Community Health Act, Infectious disease control, Food poisoning
INTRODUCTION
Although information on the public health administration of the Japanese national government is accessible in English through the homepage of the Ministry of Health, Labour and Welfare (http://www.mhlw.go.jp/english/index.html), information on public health centers (PHCs, hokenjo in Japanese), which are the responsibility of local authorities executing the public health administration of the Japanese government, is rather scarce in English. In addition, the structures and roles of PHCs in Japan have rarely been published in English language journals.1) Accordingly, the usefulness and effectiveness of the services provided to the community by PHCs do not seem to be well-known among researchers in health services outside Japan.
This article simply summarizes the structures and roles of PHCs responsible for providing the fundamentals of community health in Japan.
HISTORY OF PUBLIC HEALTH CENTERS
The first Public Health Center Act (Hokenjo Hou in Japanese) was enacted in 1937, and in the following year, a Ministry of Health and Welfare was established by the national government of Japan. After Japan’s defeat in the Second World War, a new Public Health Center Act was established in 1947, which covered the appropriate administrative roles in medical and pharmaceutical affairs, food sanitation, and environmental health. Through the steady development of social structures, the needs of communities for PHCs have become greatly diversified. To meet those diversified demands, the Public Health Center Act was amended to the Community Health Act (Chiiki Hoken Hou in Japanese) in 1994. It clearly specified the roles of prefectural governments and municipal/town/village local governments in community health. The Act incorporated municipal/town/village health centers (HCs, hoken senta in Japanese) as the proxies of PHCs. The Ministry of Health and Welfare and the Ministry of Labour were combined to establish the Ministry of Health, Labour and Welfare in 2001.2)
After such the disasters as the Hanshin-Awaji earthquake on January 17, 1995, and the sarin gas crime on March 20, 1995, PHCs were also expected to assume the additional role of administrative centers for health crisis management.2,3)
STRUCTURE OF HEALTH ADMINISTRATION
Health administration in Japan is basically structured along the line of the Ministry of Health, Labour and Welfare to prefectures, PHCs, and cities/towns/villages. In cities designated by the Ordinance of Community Health Act and special wards of Tokyo, the organizational line runs from the Ministry of Health, Labour and Welfare to the designated cities or the special wards, and finally to PHCs, as shown in Fig. 1. The prefectural PHCs cover several cities/towns/villages, while the PHCs of the designated cities and wards cover their own area. The roles of PHCs in designated cities and special wards are the same as those of prefectures.
Fig. 1.
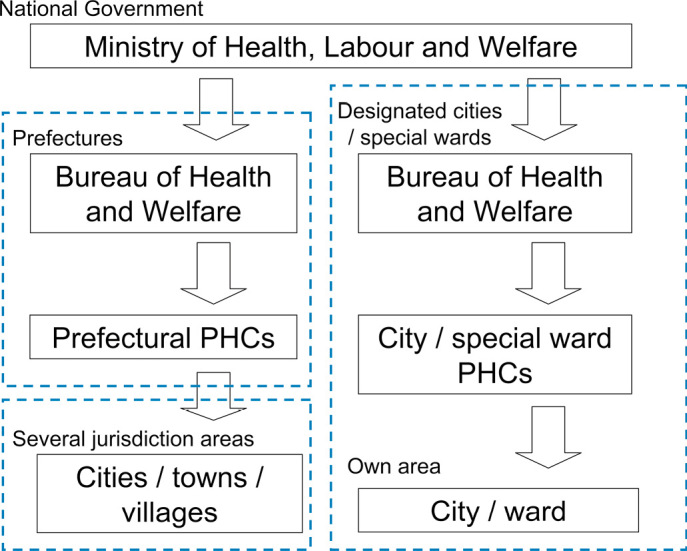
Basic structure of health administration in Japan.
The Ministry of Health, Labour and Welfare is responsible for public health pursuant to an Act determining the national standards. Prefectural governments establish the necessary criteria/conditions on public health by prefectural ordinance. PHCs constitute an administrative agency empowered to execute that responsibility. All administrative units in Japan defined by city, ward, town, and village are under the jurisdiction of their respective PHCs.
NUMBER OF PUBLIC HEALTH CENTERS
After the stock market collapse of 1993–1994, the government subsidies for PHCs started to decrease and were almost completely abolished by March, 2006, being replaced with the budgets of local governments.4) The Community Health Act was revised in 1994 and came into effect in 1997 to promote the unification of PHCs covering a small population. That Act included a policy5) whereby (1) PHCs have roles designed to improve and promote community health, (2) Prefectural PHCs are recommended to cover jurisdiction area with populations of about 300,000, (3) while cities with population over 300,000 are recommended to establish a PHC from their own budget.
According to this policy, prefectural PHCs with a small population have been integrated into a neighboring PHC, or are transferred to a municipal government with a population over 300,000.
The total number of PHCs in 1966 was 826, a figure maintained at approximately 850 until 1996.5) However, a decreasing trend has been observed since 1997 when the Community Health Act came into effect.
Table 1 shows the number of PHCs based on the level of local governments in 19965) and 2010.2) Prefectural PHCs have been steadily decreasing from 623 in 1996 to 374 in 2010. Cities owning at least one PHC increased from 35 to 66, while PHCs owned by cities decreased from 169 to 97. In 2010, the only cities with two or more PHCs were Sendai, Kawasaki, Nagoya and Fukuoka. The PHCs of Tokyo’s 23 special wards decreased from 53 to 23 between 1996 and 2010. While the general rule is that one PHC serves 300,000 inhabitants, PHCs in Sapporo, Saitama, Kyoto, Osaka, Kobe, and Hiroshima each account for a population of over 1 million, while the PHC of Yokohama covers 3.6 million people.1,3) The number of medical doctors working in PHCs has been decreasing along with the number of PHCs, from 1,173 in 19976) to 840 in 2008.7)
Table 1.
Number of public health centers (PHCs) in 1996 and 2010a)
| Level of government | 1996 | 2010 | ||||
| N | PHC | N | PHC | |||
| Prefectures | 47 | 623 | 47 | 374 | ||
| Designated cities | 35 | 169 | 66 | 97 | ||
| Special wards of Tokyo | 23 | 53 | 23 | 23 | ||
| Total | 105 | 845 | 136 | 494 | ||
a) A current list of PHCs is available at the homepage of the Japanese Association of Public Health Center Directors (http://www.phcd.jp/HClist/HClist-top.html in Japanese)
STRUCTURE OF PUBLIC HEALTH CENTERS
Since the population covered by one PHC varies from 10 thousand to over three million, the number of PHC staff also varies greatly. However, the structure of PHCs remains basically unchanged.
The director of a PHC must be a certified medical doctor. There are three divisions in a PHC under the director. The General Affairs Division (Soumu-ka in Japanese) has the responsibility for collecting vital statistical data and reporting them to the Ministry of Health, Labour, and Welfare. The supervision and auditing of medical facilities are also among the jobs of this division. The responsibility of the Life Environment Division (Seikatsu Kankyo-ka in Japanese) involves food safety assurance, sanitation of restaurants, hotels, performance halls, barber shops, beauty parlors, laundries, dry cleaners, public baths and pools. Supervision and auditing pharmaceutical facilities are also included in the responsibility.
The Health and Prevention Division (Hoken Yobou-ka in Japanese) covers such areas as infectious disease control, nutritional improvement, health check-ups and elderly care services.
PHC staff numbers vary depending on the size of the population. According to 2008 statistics (http://www.e-stat.go.jp/ in Japanese),7) those numbers averaged 53.9 personnel per one PHC, including public health professionals such as 1.6 medical doctors, 0.2 dentists, 4.1 veterinarians, 5.3 pharmacists, 15.0 public health nurses, 0.1 midwives, 0.5 nurses, 2.3 dieticians, 1.6 laboratory technicians and 2.2 others.
ROLES OF PUBLIC HEALTH CENTER DEFINED BY COMMUNITY HEALTH ACT
The roles of PHCs are set forth in the Community Health Act as follows.2)
1. Propagation and improvement of information on community health
2. Vital statistics and other statistics on community health
3. Improvement of dietary conditions and food sanitation
4. Environmental sanitation of housing, water supply, sewage, waste disposal and public cleaning
5. Medical and pharmaceutical affairs
6. Matters concerning public health nurses
7. Promotion and improvement of public medical services
8. Maternal, child, and elderly health
9. Dental health
10. Psychiatric health
11. Health of patients under long-term care due to incurable diseases
12. Prevention of diseases including acquired immune deficiency syndrome (AIDS), tuberculosis (TB), sexually transmitted diseases (STD), and other infectious diseases
13. Laboratory testing of sanitation/environment
14. Other measures to maintain/promote health in the community
Additionally, PHCs are empowered to conduct the following.
1. Collection, summarization, and use of available information on community health
2. Surveys and studies on community health
3. Treatment of dental and other diseases designated by the Minister of Health, Labour and Welfare
4. Laboratory tests, and permission for doctors to conduct such tests in PHCs
Additionally, prefectural PHCs are responsible for improvement of communication among and technical support for local governments (city, town, and village).
AUTHORIZED ENFORCEMENTS
Acts concerning public health empower local governments to conduct licensing and inspection of industries such as restaurants and food manufacturers, public facilities such as public bath houses, inns, hotels, cinemas, theaters, performance halls, barber shops, and beauty salons, laundries, and medical, dental and pharmaceutical facilities such as hospitals, clinics, dental offices, and pharmacies. To conduct licensing and inspections, PHCs employ various public health and medical professionals.
The Ministry of Health, Labour and Welfare determines (or indicates the standard models of) inspection checkpoints. For example, the size of inpatient rooms, width of corridors, numbers of hired medical staff (doctors, nurses, pharmacists, and so on) per patient, facilities and equipment to prevent the transmission of infectious diseases are checkpoints for medical facility inspection.8) In Japan, a hospital is defined by the Medical Service Act (Iryou Hou in Japanese) as a medical facility with more than 20 beds for inpatient care which is subject to on-site inspections by a PHC inspector, including a medical doctor.
For restaurants, the checklist includes a separate area for preparing meals, prescribed materials for floors and walls of cooking areas, a refrigerated facility, a hand-washing station with running water, a toilet also equipped with a hand-washing station with running water, equipment for the cleaning and disinfection of utensils, a disinfected water supply and drainage, a locker room for cooks, etc. Restaurants must designate one person as a food- sanitation supervisor, who has to attend a one-day lecture executed by PHC as a condition for the extension of the restaurant’s business license. Such a business license is usually effective for 6 or 7 years.
The water of public bath houses must be disinfected with chlorine and replaced once a day. From 1998 to 2003 in Japan, 388 patrons, including 16 who died, were diagnosed with legionella, having been infected at public baths with a circulating water system.9) Thus PHCs are required to inspect the chloride concentration of bath water to determine whether legionella are not detected to measure for legionellosis.9-11)
TUBERCULOSIS CONTROLS
PHCs play a key role in anti-TB measures. TB used to be the leading cause of death as late as 1950, but it dropped to as low as 27th in rank by 2007.12) The incidence of TB cases in Japan decreased dramatically from 383,773 (402.2 per 100,000) in 1962 to 24,170 (19.0 per 100,000) in 2009,13) which was still high compared with other developed countries. Accordingly, TB remains one of the most important infectious diseases in Japan. The Tuberculosis Prevention Act (Kekkaku Yobou Hou in Japanese) was incorporated into the Infectious Disease Act (Kansensyo Hou in Japanese) in April, 2007, with TB being classified into a type 2 disease in the Act.14)
The Infectious Disease Act classifies targeted infectious diseases into five types according to the severity, infectivity and their transmission route. Type 1 is a group with the most serious infectious diseases such as Ebola hemorrhagic fever. Patients infected with type 1 or 2 infectious disease must be admitted to an isolation ward.14) In Japan, no type 1 or 2 diseases except TB have been reported. The isolation procedures are almost the same for all type 1 and 2 diseases.
Measures for TB mandated by the Infectious Disease Act are as follows. (1) Isolation of infectious TB patients and in-patient treatments until verified non-infectious. (2) Health check-ups of those in close contact with infectious TB patients to prevent an outbreak. (3) Additional public subsidy of medical expense of TB to ensure the complete course of medical treatments. (4) Consultation with public health nurses regarding medical treatment as well as other TB issues. (5) An Infectious Disease Advisory Committee to protect patient’s rights and to recommend treatments that meet the standard regime.
Signs of TB outbreaks trigger clinicians’ notification to a nearby PHC. Public health nurses visit patients to collect information and to scrutinize those in contact with TB patients. The nurses provide information not only on medical treatment but also on associated matters such as financial support from the government.
A sputum smear is a very important test to assess a patient’s infectiousness. In case of a positive TB bacilli sputum smear, the PHC staff recommends that the patient be admitted to a hospital with a TB isolation ward. Almost all patients voluntarily accept such a recommendation, although PHCs can order a maximum hospitalization of 72 hours for patients who refuse to cooperate, with any admission fees basically covered by a public subsidy. For a hospitalization exceeding 72 hours, permission of the Infectious Disease Advisory Committee is needed in advance for every 30 days of further hospitalization. Local governments must form an Infectious Disease Advisory Committee for any area governed by several PHCs. The committee includes medical doctors, lawyers and experts on human rights. Most patients become non-infectious verified by culture within 2–4 months after starting treatment.
To confirm a patient’s continued medication to prevent a TB relapse and the emergence of multidrug resistance, WHO recommends they take their medication in the presence of a medical worker for 6 to 9 months (DOTS: directly observed treatment, short course), which is shorter than the one- to two-year course in a previous TB treatment.15,16) Sputum smear-positive patients are isolated and receive medication under the direct observation of nurses in the isolation ward. Public health nurses in PHCs also help and advise outpatients to continue taking their drugs.
PHCs investigate a patient’s family, as well as other contacts in his/her school, workplace, and other locales, by administering a chest radiographs, tuberculin skin tests (TST), and/or Quantiferon TB (QFT), if necessary. In case patient’s contacts prove TST/QFT-positive and chest radiographs negative, they are diagnosed as a case of latent TB infection, and PHCs recommend they receive a course of medication for 6 months to prevent symptomatic TB.17) Since most Japanese are routinely vaccinated several times during such programs, a positive TST without TB infection is quite common.18) Accordingly, QFT would prove more useful than a TST to diagnose TB infection.19,20)
FOOD POISONING CONTROLS
The work of the food safety administration (http://www.mhlw.go.jp/english/topics/foodsafety/index.html) is based on the Food Sanitation Act (Shokuhin Eisei Hou in Japanese) http://www.japaneselawtranslation.go.jp/?re=02) and other related Acts. The national government establishes the standards/specifications for food, food additives, and food labelling, having the authority to prohibit the sale of foods when they fail to meet the standards. In addition, the national government is in charge of the supervision and instructions for imported food. Food sanitation inspectors of each quarantine station carry out document examinations and inspections to verify whether the imported foods/products comply with the Food Sanitation Act. Prefectural governments establish the mandatory criteria/conditions on hygiene management for facilities serving foods, in accordance with prefectural ordinances.
PHCs grant licenses to restaurants or other businesses according to the prefectural ordinances, and are empowered to suspend licensed businesses if they violate the criteria/conditions of hygiene management defined by prefectural ordinances, and can order the disposal of foods that fail to meet the standards set by the national government. Food sanitation inspectors of PHCs visit grocery stores and food manufacturers to inspect the handling, labelling, and storage of foods. They collect food samples, and test them for contamination from bacteria, toxins, additives, artificial food coloring, genetically modified foods, antibiotics, and insecticides to verify whether they meet the standards. The cadre of food sanitation inspectors must include a medical doctor, a dentist, a pharmacist, a veterinarian, a certified dietitian, or university graduates who have majored in fishery science or agricultural chemistry.
Article 58 of the Food Sanitation Act requires that clinicians must notify the director of a PHC within 24 hours, once they have diagnosed anyone suspected of suffering from food poisoning. When notified by clinicians or restaurant customers, the PHC (1) conducts epidemiological investigations to trace suspicious foods, (2) collects samples from feces, urine, or vomitus of poisoned patients, conducts stool examination of food handlers21) and swabs of cooking facilities as well as food collections to test for possible causes including bacteria, viruses, chemical substances, toxins (shell fish, fish, and mushrooms), parasites (cryptosporisium and anisakis), etc.22,23)
It is to be expected that the identification of food poisoning only through the reports by clinicians will be incomplete. In 2009, 3,878 patients infected with Enterohemorrhagic Escherichia coli (EHEC) infection were notified thanks to the PHCs’ disease reporting system, while those reported merely as possible food poisoning cases numbered only 181.24) Although the difference in the reported numbers between the food poisoning reporting system and the disease reporting system might be due to cases spread randomly by a person-to-person infection route,25) it appears likely that there were many unreported patients with sporadic food poisoning. At the time of notification to PHCs through the disease reporting system, suspicious food had been usually abandoned due to 3–5 days latent period of the EHEC and so PHCs cannot collect suspicious food samples.
For school lunches and hospital food, preservation of samples for at least two weeks became mandatory after a massive outbreak of EHEC among schoolchildren in 1996.26)
In recent years, pulsed-field gel electrophoresis (PFGE) has become available to identify sporadic cases of diffuse food-borne outbreaks, including EHEC cases.27,28) A diffuse outbreak is a kind of food-borne dissemination, which occurs in separate regions or at different times when foods are stocked below freezing and widely distributed.29) In 2009, there were three diffuse outbreaks affecting geographically wide areas; two were caused through beefsteak restaurant chains spreading nationwide and one through a yakiniku (grilled sliced meat) restaurant chain in a metropolitan area.24)
According to the government’s 2008 food poisoning reports, causes were identified for 93.4% of the 1,369 food poisoning outbreaks. Among those identified, 60.9% were bacterial in origin, mainly campylobacter and salmonella, while viruses (mainly the norovirus), caused 23.8% of the outbreaks and 50.5% of the cause-identified cases.30)
HEALTH CENTERS
The HCs (hoken senta in Japanese) comprise sections of city/town/village levels of the local governments. Their roles are also described in the Community Health Act and they co-ordinate with PHCs for community health. Table 2 shows the differences between PHCs and HCs. Main medical staff in HCs includes public health nurses and dieticians, while PHCs employ various medical professionals including medical doctors. Maternal and child health are the main focus of HCs, which include health check-ups of children, vaccinations of polio and BCG for children and a mother-child handbook which is distributed free to pregnant women when they report their pregnancy to HCs. In 2008, 2,726 HCs with 26,129 personnel including 16,525 public health nurses and 2,357 dieticians were administered by cities/towns/villages throughout Japan.31)
Table 2.
Characteristics of public health centers (PHCs) and health centers (HCs) run by city/town/village governments
| PHC | HC | ||
| Government level | Prefecture, major city, and special wards of Tokyo | City, town, and village | |
| Director | Certified medical doctor | No medical qualification | |
| Medical professional | Medical doctor, dentist, pharmacist, veterinarian, public health nurse, dietician, etc | Public health nurse and dietician | |
| Legal authority | Supervision, audit, licensing, and suspension of restaurants, medical facilities, etc | None | |
| Health check-up | For those in close contact with infectious disease patients | For children | |
| Vaccination a) |
None | Oral polio and BCG | |
| Treatment b) |
Dental diseases and designated diseases | No |
a) The Ministry of Health, Labour and Welfare recommends vaccination programs not at HCs, but at clinics or hospitals.
b) Although Okinawa prefectural PHC treated tuberculosis in the past, no other PHCs have conducted such treatments to date.
CONCLUSIONS
It is widely recognized that prompt and appropriate measures against crises threatening health are essential in any community; PHCs play key roles in taking such measures. As described in this article, the responsibilities of PHCs extend into many fields. To ensure those measures are effective, sufficient numbers of public health professionals, especially medical doctors, are needed in PHCs. Public health researchers are responsible for advocating the maintenance and extension of the PHC system. This article has described in English the outline of the structure and roles of PHCs, which will facilitate the exchange of information among their counterparts in other countries.
REFERENCES
- 1).Hayasaka S, Murata C, Shibata Y, Noda T, Ojima T. Decreasing number of public health centres (hokenjyo) in Japan. Public Health, 2009; 123: 194–195. [DOI] [PubMed]
- 2).Health and Welfare Statistics Association. Outline of health administration activities. J HealthWelf Stat, 2010 (in Japanese); 57: 16–26.
- 3).Fujimoto S. Organization of Public Health Centers for health crisis management. J HealthWelf Stat, 2009 (in Japanese); 56: 10–19.
- 4).Health and Welfare Statistics Association. Finance of Public Health. J HealthWelf Stat, 2006 (in Japanese); 53: 14–15.
- 5).Otuki K. Public health centers: numbers and activities of public health centers. Jpn J Public Health, 2010 (in Japanese); 57:561–570. [PubMed]
- 6).Department of statistics and information of Ministry of Health, Labour and Welfare. Numbers of full-time employees of Public Health Centers. Report on Community Health and Health Services 1997, pp.454–455, 1999, (in Japanese), Health and Welfare Statistics Association, Tokyo.
- 7).Department of statistics and information of Ministry of Health, Labour and Welfare. Numbers of full-time employees of Public Health Centers, Report on Community Health and Health Services 2008 (volume1), pp.418–425, 2010, (in Japanese), Health and Welfare Statistics Association, Tokyo.
- 8).Tanaka T, Takahashi H, Kobayashi JM, Ohyama T, Okabe N. A nosocomial outbreak of febrile bloodstream infection caused by heparinized-saline contaminated with Serratia marcescens, Tokyo, 2002. Jpn J Infect Dis, 2004; 57: 189–192. [PubMed]
- 9).Ogawa M. Measures for circulating bath infection. Handbook of Legionnaires’ disease, edited by Saitou A. pp.231–241, 2003, (in Japanese) Japanese Medical Journal, Tokyo.
- 10).Nakamura H, Yagyu H, Kishi K, Tsuchida F, Oh-Ishi S, Yamaguchi K, Matsuoka T. A large outbreak of Legionnaires’ disease due to an inadequate circulating and filtration system for bath water epidemiologic manifestations. Intern Med, 2003; 42: 806–811. [DOI] [PubMed]
- 11). Kuroki T, Ishihara T, Ito K, Kura F. Bathwater-associated cases of legionellosis in Japan, with a special focus on Legionella concentrations in water. Jpn J Infect Dis, 2009; 62: 201–205. [PubMed]
- 12).Japan Anti-Tuberculosis Association. Trend of death cause ranking in Japan. STATISTICS OF TB 2010, p.24, 2010, Anti-Tuberculosis Association, Tokyo (in Japanese).
- 13).Japan Anti-Tuberculosis Association. Trend of incidence rate of tuberculosis in Japan. STATISTICS OF TB 2010, p.24, 2010, Japan Anti-Tuberculosis Association, Tokyo (in Japanese).
- 14).National Institute of Infectious Diseases. Amendment of the Infectious Diseases Control Law. IASR, 28: pp.185–188, 2007, National Institute of Infectious Diseases, Tokyo.
- 15).WHO publication on tuberculosis. Pursue high-quality DOTS expansion and enhancement, Stop TB strategy 2006, pp.9–11, 2006, WHO, Geneva.
- 16).Narita T, Kobayashi N. Development and perspectives of community DOTS. Kekkaku, 2009; 84: 187–201 (in Japanese). [PubMed]
- 17).The National Tuberculosis Controllers Association and CDC. Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep, 2005; 54(RR-15): 1–47. [PubMed]
- 18).Yamamoto S, Yamamoto T. Historical review of BCG vaccine in Japan. Jpn J Infect Dis, 2007; 60: 331–336. [PubMed]
- 19).Yoshiyama T, Harada N, Higuchi K, Sekiya Y, Uchimura K. Use of the QuantiFERON®-TB Gold test for screening tuberculosis contacts and predicting active disease. Int J Tuberc Lung Dis, 2010; 14: 819–827. [PubMed]
- 20).Mazurek GH, Jereb J, Lobue P, Iademarco MF, Metchock B, Vernon A. Guidelines for using the QuantiFERON®-TB Gold Test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep, 2005; 54(RR15); 49–55. Erratum in MMWR Morb Mortal Wkly Rep, 2005; 54: 1288. [PubMed]
- 21). Ozawa K, Oka T, Takeda N, Hansman GS. Norovirus infections in symptomatic and asymptomatic food handlers in Japan. J Clin Microbiol, 2007; 45: 3996–4005. [DOI] [PMC free article] [PubMed]
- 22).Yoshida H, Matsuo M, Miyoshi T, Uchino K, Nakaguchi H, Fukumoto T, Teranaka Y, Tanaka T. An outbreak of cryptosporidiosis suspected to be related to contaminated food, October 2006, Sakai City, Japan. Jpn J Infect Dis, 2007: 60: 405–407. [PubMed]
- 23).Kitamoto M, Kito K, Niimi Y, Shoda S, Takamura A, Hiramatsu T, Akashi T, Yokoi Y, Hirano H, Hosokawa M, Yamamoto A, Agata N, Hamajima N. Food poisoning by Staphyloccocus aureus at a university festival. Jpn J Infect Dis, 2009; 62: 242–243. [PubMed]
- 24).National Institute of Infectious Diseases. Enterohemorrhagic Escherichia coli infection in Japan as of May 2010, IASR, 31, pp.152–153, 2010, National Institute of Infectious Diseases, Tokyo.
- 25).Kanazawa Y, Ishikawa T, Shimizu K, Inaba S. Enterohemorrhagic Escherichia coli outbreaks in nursery and primary schools. Jpn J Infect Dis, 2007; 60: 326–327. [PubMed]
- 26).Michino H, Araki K, Minami S, Takaya S, Sakai N, Miyazaki M, Ono A, Yanagawa H. Massive outbreak of Escherichia coli O157:H7 infection in schoolchildren in Sakai City, Japan, associated with consumption of white radish sprouts. Am J Epidemiol, 1999; 150: 787–796. [DOI] [PubMed]
- 27).Kawamori F, Hiroi M, Harada T, Ohata K, Sugiyama K, Masuda T, Ohashi N. Molecular typing of Japanese Escherichia coli O157 : H7 isolates from clinical specimens by multilocus variable-number tandem repeat analysis and PFGE. J Med Microbiol, 2008; 57(Pt 1): 58–63. [DOI] [PubMed]
- 28).Terajima J, Izumiya H, Iyoda S, Mitobe J, Miura M, Watanabe H. Effectiveness of pulsed-field gel electrophoresis for the early detection of diffuse outbreaks due to Shiga toxin-producing Escherichia coli in Japan. Foodborne Pathog Dis, 2006; 3: 68–73. [DOI] [PubMed]
- 29).Watanabe H, Terajima J, Izumiya H, Iyoda S, Tamura K. PulseNet Japan: surveillance system for the early detection of diffuse outbreak based on the molecular epidemiological method. Kansenshogaku Zasshi, 2002; 76: 842–848 (in Japanese). [DOI] [PubMed]
- 30).Health and Welfare Statistics Association. 8) Food poisoning. J HealthWelf Stat, 2009; 56: 293-295 (in Japanese).
- 31).Department of Statistics and Information of Ministry of Health, Labour and Welfare. Numbers of full-time employees of cities/wards/towns/villages related health services. Report on Community Health and Health Services 2008 (volume 1), pp. 668-675, 2010(in Japanese), Health and Welfare Statistics Association, Tokyo.


