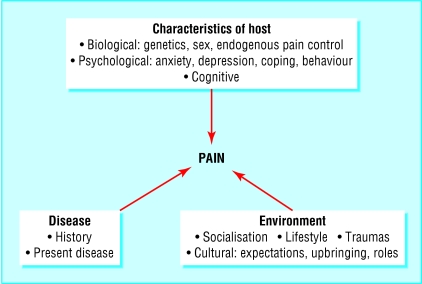
The management of pain differs if pain is self limiting or persistent; for example, if pain is prolonged then treatment will be managed by a multidisciplinary team in a pain clinic. Pain is not just from physical disorders but also from combinations of physiological, pathological, emotional, psychological, cognitive, environmental, and social factors (fig 1). The keys to successful pain control are the mechanisms that initiate and maintain pain. Major advances in neurobiology, from molecular studies to imaging the cortex of the brain, show the complex integration of nerve cell activity and have generated a fundamental change in attitude and expectation about the control of pain.1 Now, the public and health professionals expect to control pain by using preventive and active strategies, including drugs and physical and psychosocial interventions.
Figure 1.
Biopsychosocial factors that interact and modulate the experience of pain
Methods
The topics we have chosen result from discussions with all grades of staff involved in the management of acute and chronic pain and range from new drug development based on scientific evidence that may impact on future pain management to a holistic approach to patient care. Our searches focused on the key words “pain,” “systematic review,” “management,” and “neuropathic.” We searched Medline, the Cochrane Library, and Health Technology Assessments, and we scrutinised the BMJ and the National Institutes of Health websites as well as professionally based websites for pain, such as that of the International Association for the Study of Pain and scientific websites such as that of the National Academy of Sciences. We identified systematic reviews from the past three years from these sources and leading scientific papers.
Recent developments
A major change in pain management is a move from empirical therapies to a mechanism based approach
New drug developments are targeting specific receptor subtypes
Pain assessment includes qualitative sensory affective and quantitative sensory testing to improve subgroup analysis and evidence based treatment of heterogeneous disease states
Care is individualised, holistic, and organised through a multidisciplinary approach
What is being managed in pain control?
A simple to complex phenomenon
When pain is experienced, this sensation has reached the cerebrum through complex and dynamic interactions. Heat on the skin, for example, results in chemical and electrical signals being sent through peripheral sensory nerves to the dorsal horn of the spinal cord. Whether this stimulus becomes painful depends on many factors. Higher centres may block or enhance the message wholly or partly through behavioural, cognitive, psychological (for example, anxiety), biological (for example, sex hormones), or pharmacological activities. When the stimulus becomes unpleasant the normal responses are to recognise the sensation as pain, to withdraw, and to avoid the activity. These responses can be expressed as sensory, motor, cognitive, motivational, and attentional consequences of the stimulus. A picture thus emerges of differences in sensory awareness and after effects, so that although the stimulus may be the same temperature, modulation of the sensory process occurs at all levels of neural activity from the periphery through the spinal cord to the cortex. Consequently the perception of a stimulus and initiated responses vary. In addition, the scenario could be set in the situation of no tissue damage, such as a volunteer study, or of tissue injury, which can be either intentional or unintentional. By changing the context—for example, the sex of a researcher—extra interactive factors may increase the variability of response (see fig 1).
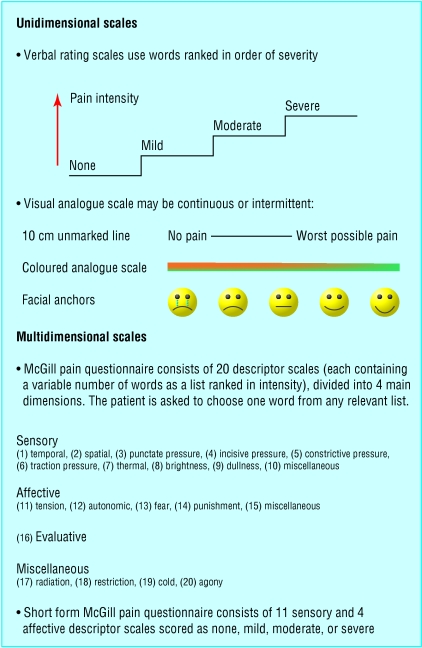
Verbal limitations on descriptions of pain
As pain is essentially subjective and the measurement of quality is based on verbal concepts, a definition of pain sensation in humans has been sought to standardise its measurement and management (fig 2). Over the years concepts have changed from a hard wired neuroanatomical approach, through a more flexible gating control system in the spinal cord, to widespread modulation and neuroplasticity, the patterns and interactions of which are the focus of current research. The debate is still evolving on the concept of pain. Definitions that arose in the 1990s to describe unpleasant sensory and emotional experiences associated with actual or potential tissue damage are changing to recognise that tissue damage may be lacking and that there is a component of unpleasantness that has a cognitive base.2–4 Both ideas can be illustrated by the heat stimulus scenario described above. For example, repetitive non-noxious stimulation can increase a volunteers' sensitivity to pain; in the intention to harm scenario, the emotive response to the situation may be unpleasant as well as the stimulus.
Figure 2.
Subjective measures of pain based on word descriptors
Clinical examples
Through recognition of these new ideas, approaches can be made to control both pain in the absence of tissue damage and pain inappropriately large for the stimulus. One important example based on clinical evidence is back pain where therapies have changed from bed rest to active movement.5 Following recognition that the cause was not tissue damage but altered sensation to pain and that rest did not reduce tissue trauma, activity and analgesics became the key to restoring normal sensation (box B1). Another example is the management of pain in children undergoing venepuncture where, in addition to pharmacological measures, teaching cognitive and behavioural strategies can help to reduce distress.6 Thus definitions of pain and fundamental clinical assumptions are changing, leading to more rapid recovery of mobility in patients with back pain and reduced stress during painful interventions.
Box 1.
Evidenced based management plan for conservative treatment of acute and chronic low back pain5
- Recommended for short term relief of symptoms
- Potential harmful side effects
- Choice not limited by type but side effects
- Leads to less chronic disability
- Exercise therapy strongly recommended for chronic low back pain
- Helps patients return to work
- Evidenced based treatment for acute back pain rather than bed rest
- Includes education, active exercises, relaxation, behaviour therapy
- Improves long term outcomes measured by function, pain, and time at work
The role of different mechanisms
Clinically, pain management is moving towards a mechanism based approach through the reorganisation of taxonomy and the design of molecularly targeted pharmacological therapies. Thus queries should concern which nerve cells and neurochemicals are involved with the pain and what psychosocial mechanisms are maintaining it rather than just the location of the pain.7,8
Age and sex
Although anatomical classifications are considered artificial and of limited therapeutic value, they have been used in epidemiology to elucidate differences between the sexes in perception of pain. A US study analysed data on pain lasting more than a day within a six month period and found that women reported pain in the back, head, chest, abdomen, and face more often than men at all ages, although the difference decreased with age.9 This pattern of reporting pain has raised several theories: a greater biological sensitivity to painful stimuli in women; a cognitive psychological difference such that women label stimuli as painful at different thresholds from men; and social and cultural factors that influence reporting of pain differently in men and women. Consequences for improving analgesia not only include reducing the higher frequency of reporting of pain in women but also addressing the potential problem of under-reporting in men.
Neuropathic pain
Diagnosis of pain by site, duration, and cause can limit therapeutic specificity. Neuropathic pain is a clinically important example of a diagnostic tag failing to predict therapeutic outcome. The pain is “initiated or caused by a primary lesion or dysfunction in the nervous system,” and yet its cause is heterogeneous and commonly may be inflammatory (for example, post herpetic neuralgia), metabolic, or ischaemic.2 Thus a new classification has been proposed. The main approach is to divide peripheral neuropathic pain into stimulus evoked pain or stimulus independent pain (spontaneous pain).10 Spontaneous pain mainly arises by spontaneous activity in primary sensory neurones, and drugs that diminish neuronal activity in ion channels are prime targets for research. In contrast, stimulus evoked pain can be precisely measured by quantitative sensory testing (see bmj.com): heightened reaction to a painful stimulus evoked by brushing or pressure (dynamic or static hyperalgesia) and tactile pain to an innocuous stimulus (allodynia). If these tests could be used to select patients for specific treatment, then the result would be a more rational basis for pain management. The present challenge is to establish the validity of these tests.
Specific drugs to control neuropathic pain are being developed on the basis of sodium channel blockers.11 Drugs presently available act on sodium channels sensitive to tetrodotoxin and thus have widespread side effects in the heart and central nervous system. The future direction of research is to identify agents that block sodium channels insensitive to tetrodotoxin and thus restrict their effects to sensory nerves (table).
Additional educational resources
Transcutaneous electrical nerve stimulation (TENS)
Carroll D, Moore RA, McQuay HJ, Fairman F, Tramèr M, Leijon G. Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Library. Issue 1. Oxford: Update Software, 2002.
Proctor ML, Smith CA, Farquhar CM, Stones RW. Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev 2002;(1):CD002123.
Acupuncture
Acupuncture. National Institutes of Health consensus statement No 107. 1997;Nov 3-5,15:1-34.
Organisation reports
NHS Health Technology Assessment (www.hta.nhsweb.nhs.uk)
Systematic review of out-patient services for chronic pain control. London: NHS Executive, 1997. [Includes multiple reports on treatments for back pain]
NHS Centre for Reviews and Dissemination. Acute and chronic low back pain. Effective Health Care 2000;6(5). (www.york.ac.uk/)
Royal College of Anaesthetists (www.rcoa.ac.uk/). Guidelines for the use of non-steroidal anti-inflammatory drugs in the perioperative period, 1998
Pain Society (www.painsociety.org). Desirable criteria for pain management programmes, 1997
The Association of Anaesthetists of Great Britain and Ireland and the Pain Society (www.aagbi.org). Provision of pain services, 1997
World Health Organization (www.who.int/). Cancer pain relief and cancer pain relief and palliative care in children, 1996
Royal College of Nursing (www.rcn.org.uk/). The recognition and assessment of acute pain in children. Implementation guide, 2001
College of Physicians and Surgeons of Ontario (www.cpso.on.ca). Evidence based recommendations for medical management of chronic non-malignant pain. Reference guide for clinicians, 2000
General information (for the public and professionals)
International Association for the Study of Pain (www.iasp-pain.org)
This has a general website with links to special interest groups such as systematic reviews in pain relief (www.jr2.ox.ac.uk/bandolier/booth/painpag or www.ebandolier.com) and sympathetically mediated pain. There are other interesting links to journals and international developments as well as IASP publications. The IASP supports task forces to investigate specific issues such as the desirable characteristics for facilities for the treatment of pain
The National Academy of Sciences and the Institute of Medicine (www.nationalacademies.org/)
The National Academy of Sciences includes the Institute of Medicine. It is an independent body that advises the US government on science and medicine. Selected back issues of the Proceedings of the National Academy of Sciences are available free online and titles can be found in the references to this paper. Books such as Exploring the Biological Contributions to Human Health: Does Sex Matter? edited by Theresa M Wizemann and Mary-Lou Pardue, 2001, are also freely available online and include references to pain
The National Institutes of Health (www.nih.gov/)
This website has several public and medical programmes and statements on sex and systematic reviews, including acupuncture, chiropractic methods, temporomandibular disorders, and complimentary and alternative medicines
The National Institute for Clinical Excellence (www.nice.org.uk/)
The National Institute for Clinical Excellence is part of the NHS and produces guidance on medications and treatment. Guidelines are available for the management of low back pain, including advice on referrals. The site is easy to negotiate
The National Health and Medical Research Council of Australia (www.painmgmt.usyd.edu.au/acutepain.html)
The Department of Anaesthesia and Pain Management at the Royal North Shore Hospital has developed this website for patients and professionals. The site supports research and professional training as well as access to patients. The National Health and Medical Research Council of Australia has released three documents that can be downloaded, including Acute pain: scientific evidence, 1998
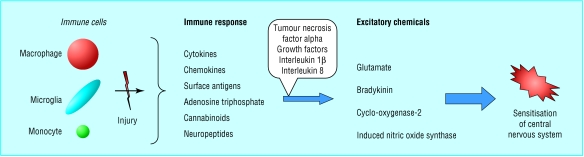
Although this approach is an advance, its scope is still limited. Evidence is emerging that inhibitory, immune, hormonal (sex and stress), and inflammatory systems may enhance or inhibit neuronal activity in the peripheral or central nervous systems.12,13 Figure 3 shows one schematic cascade of responses that may mediate neuropathic pain. This complexity illustrates fundamental diversity and plasticity in an organism—that is, the state of an individual determines the present pain. Interestingly, individual differences may be explained and visualised not only through molecular processes but also through brain imaging. When positron emission tomography and functional magnetic resonance imaging have been used to investigate painful stimuli, a cortical network has been observed that reorganises after injury. In neuropathic pain this includes spatial and temporal restructuring.14 When the sensation is particularly unpleasant, the anterior cingulate cortex shows activation.15 Brain imaging is not yet a routine diagnostic tool but represents a revolution in pain management, because it has confirmed the role of many of the pain modulators (see fig 1).
Figure 3.
Sensitisation of central nervous system develops from a cascade of neuroimmune activation events in tissues, peripheral nervous system, or central nervous system
Multidisciplinary pain clinics
To identify factors that initiate and maintain pain, a pain clinic usually has facilities for medical, psychological, physiotherapy, and pharmaceutical interventions provided by various health professionals. Consultations occur serially or in parallel, depending on the facilities and choice of the patient or health professional. Consultations occur either on the ward or in outpatient facilities. Conferences on cases are usually held early to assess and plan all aspects of management. Pain clinics may develop a particular medical referral basis, but the staff are usually similar as conventional physical interventions and medical treatments can fail. For example, there is little rationale for the choice of drugs or physical treatments for neuropathic pain, and the solution is by consideration of the psychosocial factors.16 Evidence is accumulating for a major effect of cognitive behavioural therapy, and in the future mechanism based research studies are planned.17
The future for opioids
Opioids are recognised as the standard drug for pain relief in severe postoperative and cancer related pains. Recognition of their limitations has, however, enabled a broad reappraisal of the indications for opioid therapy. Box B2 summarises the evidence based guidelines for appropriate use of opioids in non-malignant pain.18 These have been accepted as a tool in the prevention of addiction and should reduce the unmet needs of patients for opioids.
Box 2.
Guide to prescription of opioids for chronic non-malignant pain
- One prescriber
- Amount to be dispensed
- No additional prescriptions
- Consequences of breaking contract
- Titration of doses
- Use of short acting opioids
- Use of injectable opioids at home
- Prescription of more than one opioid
- Assessment at intervals of 6-9 weeks
- Alcohol problems
- Drug problems
- Other treatments not tried first
- If in doubt
- Focus on improved function not pain relief
- Use of long acting opioids
- Make prescriptions tamper proof
Opioids can be classified into either μ or κ depending on the receptor subtype at which they exert their action. Clinically, μ opioid receptor agonists such as morphine are used more often than κ agonists because they are full rather than partial agonists. In a systematic evaluation of κ opioid agonists (buprenorphine, nalbuphine, and pentazocine), however, women obtained significantly better analgesia from these drugs than men, a difference not explained by altered pharmacokinetics.19 Further evidence for sex differences in opioid effects comes from sexual dimorphism in imaging studies of binding of opioids in brain receptors, greater opioid use in men, greater potency and more adverse effects of μ opioids in women, and experimental pain studies of κ opioids.20 As a result of these and similar studies, a reappraisal of analgesic use in well defined groups of patients is considered the way forward to providing better control of analgesia.
The need to reduce the side effects of opioids has encouraged many different approaches. One is the rotation of opioids.21 As a result, pharmaceutical companies have produced alternative opioids such as oxycodone, hydromorphone, fentanyl, methadone, and tramadol. Because fentanyl is highly fat soluble, it can be given by the transmucosal route for breakthrough cancer pain and by transdermal patches for long term delivery. Another approach is using drugs to antagonise the peripheral effects of opioids so that bowel dysfunction is reversed, speeding discharge from hospital.22 Combination therapies, using an opioid with another analgesic acting by different mechanisms, may offer an effective solution to adverse effects.
Supplementary Material
Table.
Approach to management of neuropathic pain based on diagnostic tests and mechanism based classification. Italics represent neurotransmitter at receptor
| Mechanism
|
Diagnostic features
|
Molecular target
|
Drugs
|
|---|---|---|---|
| General sodium channels: redistribution or altered expression | Spontaneous pain, paraesthesia | Sodium channels sensitive to tetrodotoxin | Local anaesthetics, antiepileptics, antiarrhythmics (for example, mexilitine), tricyclic antidepressants |
| Specific sodium channels | Spontaneous pain | Sodium channels resistant to tetrodotoxin | Selective blockers* |
| Central sensitisation | Hyperalgesia (in response to tests using touch, cold, pin prick) | N-methyl d-aspartate receptor (glutamate, glycine); neurokinin 1 receptor (bradykinin); neuronal nitric oxide synthase; protein kinase | N-methyl d-aspartate antagonist* (for example, ketamine, dextromethorphan, memantine), glycine site antagonists*; neurokinin 1 receptor antagonist*; neuronal nitric oxide synthase inhibitors*; protein kinase inhibitors* |
| Peripheral sensitisation | Hyperalgesia in response to pressure | Vanilloid receptor | Capsaicin, cannabinoids* |
| Hyperalgesia in response to thermal stimuli | Neurokinin 1 receptor | Neurokinin 1 receptor antagonist* | |
| Neurogenic inflammation | Nerve growth factor | Nerve growth factor antagonists* | |
| Sympathetic activity | Spontaneous pain | Adrenergic receptors (α adrenergic), nerve growth factor or trKA | Phentolamine, guanethidine, clonidine, nerve growth factor antagonists* |
| Reduced inhibition | Hyperalgesia | Opioid receptors, γ-aminobutyric acid transaminase, neurokinin 1, adenosine, purine, kainite, cholecystokinin, acetyl choline (nicotinic) | Morphine, gabapentin |
Drugs under development.
Footnotes
Competing interests: None declared.
A description of quantitative sensory testing and additional tables appear on bmj.com
References
- 1.Dubner R, Gold M. The neurobiology of pain. Proc Natl Acad Sci. 1999;96:7627–7630. doi: 10.1073/pnas.96.14.7627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merskey H, Bogduk N. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. 2nd ed. Seattle: International Association for the Study of Pain; 1994. [PubMed] [Google Scholar]
- 3.Fields HL. Pain: an unpleasant topic. Pain. 1999;suppl 6:61–9S. doi: 10.1016/S0304-3959(99)00139-6. [DOI] [PubMed] [Google Scholar]
- 4.Petrovic P, Ingvar M. Imaging cognitive modulation of pain processing. Pain. 2002;95:1–5. doi: 10.1016/s0304-3959(01)00467-5. [DOI] [PubMed] [Google Scholar]
- 5. NHS Centre for Reviews and Dissemination. Acute and chronic low back pain. Effective Health Care 2000;6(5).
- 6.Kolk AM, van Hoof R, Fieldeldij Dop MJC. Preparing children for venepuncture. The effects of an integrated intervention on distress before and during venepuncture. Child: Care, Health Dev. 2000;26:251–260. doi: 10.1046/j.1365-2214.2000.00145.x. [DOI] [PubMed] [Google Scholar]
- 7.Woolf CJ, Bennett GJ, Doherty M, Dubner R, Kidd B, Koltzenburg M, et al. Towards a mechanisms-based classification of pain? Pain. 1998;77:227–229. doi: 10.1016/S0304-3959(98)00099-2. [DOI] [PubMed] [Google Scholar]
- 8.Woolf CJ, Decosterd I. Implications of recent advances in the understanding of pain pathophysiology for the assessment of pain in patients. Pain. 1999;6:141–17S. doi: 10.1016/S0304-3959(99)00148-7. [DOI] [PubMed] [Google Scholar]
- 9.LeResche L. Epidemiological perspectives on sex differences in pain. In: Fillingim R, editor. Sex, gender and pain. Progress in pain research and management. Vol. 17. Seattle: International Association for the Study of Pain Press; 2000. [Google Scholar]
- 10.Woolf CJ, Mannion RJ. Pain: neuropathic pain: aetiology, symptoms, mechanisms and management. Lancet. 1999;353:1959–1964. doi: 10.1016/S0140-6736(99)01307-0. [DOI] [PubMed] [Google Scholar]
- 11.Dickinson AH, Matthews EA, Suzuki R. Neurobiology of neuropathic pain: mode of action of anticonvulsants. Eur J Pain. 2002;6(suppl A):51–60. doi: 10.1053/eujp.2001.0323. [DOI] [PubMed] [Google Scholar]
- 12.Watkins LR, Maier SF. Implications of immune-to-brain communication for sickness and pain. Proc Natl Acad Sci. 1999;96:7710–7713. doi: 10.1073/pnas.96.14.7710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeLeo JA, Yezierski RP. The role of neuroinflammation and neuroimmine activation in persistent pain. Pain. 2001;90:1–6. doi: 10.1016/s0304-3959(00)00490-5. [DOI] [PubMed] [Google Scholar]
- 14.Casey KL. Concepts of pain mechanisms: the contribution of functional imaging of the human brain. Prog Brain Res. 2000;129:277–287. doi: 10.1016/S0079-6123(00)29020-1. [DOI] [PubMed] [Google Scholar]
- 15.Hofbauer RK, Rainville P, Duncan GH, Bushnell MC. Cortical representation of the sensory dimension of pain. J Neurophysiol. 2001;86:402–411. doi: 10.1152/jn.2001.86.1.402. [DOI] [PubMed] [Google Scholar]
- 16.Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80:1–13. doi: 10.1016/s0304-3959(98)00255-3. [DOI] [PubMed] [Google Scholar]
- 17.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 18.College of Physicians and Surgeons of Ontario. Evidence-based recommendations for medical management of chronic non-malignant pain. Reference guide for clinicians. Ontario: CPSO; 2000. [Google Scholar]
- 19.Gear RW, Miaskowski C, Gordon NC, Paul SM, Heller PH, Levine JD. The kappa opioid nalbuphine produces gender- and dose-dependent analgesia and antianalgesia in patients with postoperative pain. Pain. 1999;83:339–345. doi: 10.1016/s0304-3959(99)00119-0. [DOI] [PubMed] [Google Scholar]
- 20.Fillingim RB. Sex differences in analgesic responses: evidence from experimental pain models. Eur J Anaesthesiol. 2002;19(suppl 26):6–24. doi: 10.1097/00003643-200219261-00004. [DOI] [PubMed] [Google Scholar]
- 21.De Stoutz ND, Bruera E, Suarez-Almazor M. Opioid rotation for toxicity reduction in terminal cancer patients. J Pain Symptom Manage. 1995;10:378–384. doi: 10.1016/0885-3924(95)90924-c. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt WK. Alvimopan(ADL 8-2698) is a novel peripheral opioid antagonist. Am J Surg. 2001;182:27–38S. doi: 10.1016/s0002-9610(01)00784-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.