Preventing malaria in travellers is difficult because of the widespread emergence of drug resistance and the increasing popularity of travel to endemic locations. Mefloquine is the most effective recommended antimalarial, but doxycycline (a tetracycline derivative) is being increasingly used in areas where there is resistance to mefloquine or in patients who have side effects to this drug.1
Intracranial hypertension is a well recognised side effect of tetracyclines and has been associated with the medium to long term use of minocycline for acne vulgaris.2–6 We report on two patients with acute onset of severe intracranial hypertension associated with doxycycline, in one instance causing permanent loss of most vision.
Case reports
Case 1—A 21 year old Afro-Caribbean woman who had been on holiday in Uganda for three weeks complained of headaches and blurred vision. She had been taking doxycycline 100 mg once daily for malaria prophylaxis throughout this period. Her vision was 6/9 in the right eye and 6/5 in the left. She had severe papilloedema with associated haemorrhages and cotton wool spots, more so in the right eye. A magnetic resonance imaging scan of the brain was normal. A lumbar puncture had an opening pressure of 52.5 cm H2O. All other investigations were normal. Intracranial hypertension was diagnosed and the doxycycline stopped. Oral acetazolamide 250 mg four times daily was started. Her visual fields were normal. Symptoms gradually improved, and the lumbar puncture was repeated after three weeks. The opening pressure was still high at 40 cm H2O. Cerebrospinal fluid was drained. Her vision was recorded as 6/5 in both eyes. The papilloedema subsequently resolved. The acetazolamide was continued for a further two months, after which it was gradually reduced. During this period and after cessation of the acetazolamide she remained asymptomatic and had normal optic discs.
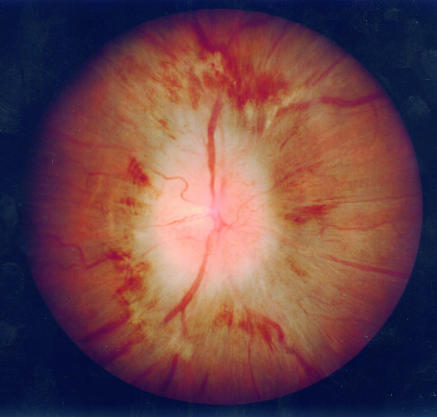
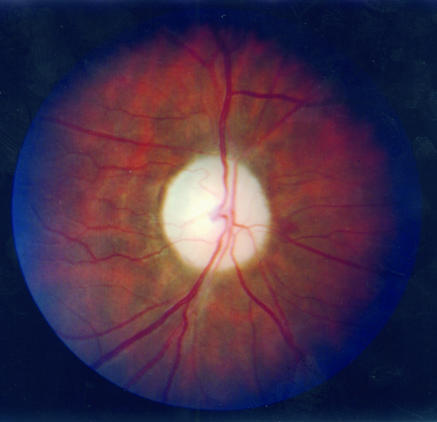
Case 2—A 19 year old white woman who had been teaching in West Africa for four months began vomiting spontaneously. She had had mild and transient headaches the week before. The vomiting continued for three weeks, and then she developed blurred vision in both eyes. She had been taking doxycycline 100 mg once daily for malaria prophylaxis throughout her stay. A computed tomogram of the head was normal. She returned to the United Kingdom where her vision was recorded as 6/5 in the right eye and 6/12 in the left. She had reduced colour vision in both eyes (zero score with Ishihara plates). Examination of her fundi showed bilateral gross papilloedema with associated haemorrhages and cotton wool spots (fig 1). Both visual fields were severely constricted, more so on the left. A magnetic resonance imaging scan of the brain was normal. Lumbar puncture showed an increased cerebrospinal fluid pressure of >40 cm H2O with normal cerebrospinal fluid composition. All other investigations were normal. Intracranial hypertension was diagnosed and oral acetazolamide 250 mg four times daily started. The doxycycline was stopped. Over the next two weeks the vomiting became less frequent but her vision continued to deteriorate to 6/24 in the right eye and 6/36 in the left. Two further lumbar punctures were performed over this period, with opening pressures of 18 cm H2O and 36 cm H2O. Her symptoms stabilised, and over the next few days her vision improved to 6/12 in the right eye and 6/18 in the left. A repeat lumbar puncture showed a normal opening pressure of 9 cm H2O. The acetazolamide was tailed off over one month. The disc swelling resolved rapidly, but consecutive optic atrophy developed (fig 2). Despite reasonable recovery of central acuity her colour vision and visual fields remained poor, with an estimated 70% loss of vision.
Figure 1.
Swelling of left optic disc
Figure 2.
Left consecutive atrophy of optic disc
Discussion
Primary idiopathic intracranial hypertension occurs predominantly in obese women in their 30s and 40s. It has been referred to as benign intracranial hypertension. The diagnostic criteria consist of symptoms and signs of raised intracranial pressure, no other neurological signs, measured increase in intracranial pressure, normal cerebrospinal fluid composition, and normal imaging studies.7 Typically, primary idiopathic intracranial hypertension is a chronic disease with a major long term risk to vision requiring regular monitoring.8,9 Treatment includes weight loss, carbonic anhydrase inhibitors, and occasionally surgery to lower the intracranial pressure and to protect the optic nerve. Intracranial hypertension may also occur secondary to several drugs, including tetracyclines, steroids, nalidixic acid, and amiodarone.3 Several other drug associations have been reported. The mechanism of these reactions is unknown.5 Stopping the culprit drug leads to resolution of the intracranial hypertension usually over 2-4 weeks. The disorder presents in a similar way in both the primary and the secondary cases, with symptoms and signs of increased cerebrospinal fluid pressure including headaches, visual obscurations, and occasional double vision due to paresis of the sixth nerve.
Although the patients described here were slightly overweight neither was morbidly obese, having a body mass index below 30 kg/m2. In idiopathic intracranial hypertension associated with poor visual outcome, the body mass index is usually over 40 kg/m2.10 Investigation in both cases did not reveal an underlying disorder associated with the hypertension. The symptoms of raised intracranial pressure began one and three months after starting doxycycline. The cerebrospinal fluid pressure was substantially increased and with appropriate treatment and withdrawal of the drug fell to normal. The evidence that doxycycline was responsible is therefore compelling.
The unusual feature in the first case was the extent of the increased intracranial pressure (52.5 cm H2O). The mean intracranial pressure in acute idiopathic intracranial hyerptension is around 34 (SD 8) cm H2O.11 Severe acute papilloedema was present with signs of axonal compromise (haemorrhages and cotton wool spots) not typically seen in idiopathic intracranial hypertension. Overall vision was, however, maintained and the patient remained asymptomatic after stopping treatment at six months.
In the second case, the intracranial pressure was increased to the extent usually measured in idiopathic intracranial hypertension, but symptoms had been present for six weeks before the first lumbar puncture was undertaken and while doxycycline treatment continued. When the patient was first examined at our institute her vision was severely reduced, with optic nerve signs indicative of major axonal compromise (see fig 1). Intracranial pressure returned to normal within three weeks of starting treatment, but despite some improvement in vision, the optic discs became atrophic. The resulting visual field defects make this patient eligible for partial sight registration and leave her outside the minimum driving requirement.
Intracranial hypertension as a side effect of doxycycline has not been previously reported. As trends change in the prescribing of antimalarials, and doxycycline is more widely used, it is important that prescribers make patients aware of the symptoms associated with intracranial hypertension—headaches, visual obscurations, blurred vision, diplopia, back and neck pain, although occasionally these can be less specific, as in case 2. If symptoms occur, medical advice should be sought. Visual acuities should be measured and the optic discs examined. The successful management of this condition follows cessation of the drug. Individuals who have had this idiosyncratic response to doxycycline should probably avoid all tetracyclines.
Doxycycline should be prescribed with caution to women of childbearing age who are overweight or have a history of idiopathic intracranial hypertension. Awareness of this side effect is essential among travellers. Prompt cessation of the drug along with appropriate medical therapy can curtail an attack of secondary intracranial hypertension, hence any permanent threat to vision.
Doxycycline prescribed for malaria prophylaxis may cause intracranial hypertension that threatens sight
Footnotes
Editorial by Digre
Funding: None.
Competing interests: None declared.
References
- 1.Juckett G. Malaria prevention in travelers. Am Fam Phys. 1999;59:2523–2530. , 2535-6. [PubMed] [Google Scholar]
- 2.Goulden V, Glass D, Cunliffe WJ. Safety of long term high-dose minocycline in the treatment of acne. Br J Dermatol. 1996;134:693–695. doi: 10.1111/j.1365-2133.1996.tb06972.x. [DOI] [PubMed] [Google Scholar]
- 3.Lander CM. Minocycline induced BIH. Clin Exp Neurol. 1989;26:161–167. [PubMed] [Google Scholar]
- 4.Monaco F, Agnetti V, Mutani R. Benign intracranial hypertension after minocycline therapy. Eur Neurol. 1978;17:48–49. doi: 10.1159/000114921. [DOI] [PubMed] [Google Scholar]
- 5.Stuart BH, Litt IF. Benign intracranial hypertension with tetracycline therapy. J Paediatr. 1978;93:901. doi: 10.1016/s0022-3476(78)81136-6. [DOI] [PubMed] [Google Scholar]
- 6.Nagarajan L, Lam GC. Tetracycline-induced benign intracranial hypertension. J Paediatr Child Health. 2000;36:82–83. doi: 10.1046/j.1440-1754.2000.00430.x. [DOI] [PubMed] [Google Scholar]
- 7.Johnston I, Paterson A. Benign intracranial hypertension II. CSF pressure and circulation. Brain. 1974;97:301–312. doi: 10.1093/brain/97.1.301. [DOI] [PubMed] [Google Scholar]
- 8.Corbett JJ, Savino PJ, Thompson S, Kansu T, Schatz NJ, Orr LS, et al. Visual loss in pseudotumour verebri. Arch Neurol. 1982;39:461–474. doi: 10.1001/archneur.1982.00510200003001. [DOI] [PubMed] [Google Scholar]
- 9.Orcutt JC, Page NG. Factors affecting visual loss in BIH. Ophthalmology. 1984;91:1303–1312. doi: 10.1016/s0161-6420(84)34149-5. [DOI] [PubMed] [Google Scholar]
- 10.Rowe FJ, Sarkies NJ. The relationship between obesity and idiopathic intracranial hypertension. Int J Obes Relat Metab Disord. 1999;23:54–59. doi: 10.1038/sj.ijo.0800758. [DOI] [PubMed] [Google Scholar]
- 11.Corbett JJ. Problems in the diagnosis and treatment of pseudotumour cerebri. Can J Neurol Sci. 1983;10:221. doi: 10.1017/s0317167100045042. [DOI] [PubMed] [Google Scholar]