Abstract
A vast amount of knowledge has been acquired through human activities such as farming, hunting, and fishing. Throughout history, humans have utilized living creatures for disease treatment, relying on the natural world's healing powers. The special “healers” may be able to treat patients via the power of nature. However, there was no systematic introduction or summary of these treatments. Therefore, we conducted a literature review based on PubMed, Google Scholar, Web of Science, Scopus, CNKI and WanFang DATA. Here, we defined this unique method as “animal healer” and six common kinds of animal healers were reviewed. These are fish therapy, pet therapy, worm therapy, leech therapy, maggot therapy, and bee therapy. According to the different characteristics of healers, treatment methods mainly included bite, parasitism, contact and communication. With the advantages of green and effectiveness, animal healers have great therapy potential against a variety of refractory diseases. The main purpose of this review is to draw people's attention to animal healer, promote it to become a possible clinical treatment strategy, and make further exploration in species cultivation, mechanism research, animal welfare, standard setting, safety evaluation and other aspects. In the future, animal healers will play an increasingly important role in medicine and hopefully solve more medical problems and dilemmas.
Keywords: Living creatures, Animal healer, Nature, Refractory diseases, Therapy
Graphical abstract

1. Introduction
In many fairy tales, characters who possess extraordinary longevity and live secluded lives in mountains and forests are a recurring motif. These characters may not be entirely fictional. Beyond the pristine natural environment, living creatures play a crucial role in maintaining the health and longevity of centenarians (Fig. 1). Nowadays, with the rapid development of medicine, most of diseases can be alleviated or even cured and the average life expectancy of human is constantly increasing [1]. However, there are still certain diseases that cannot get satisfactory results through conventional therapies. Alongside the development of new medical technologies and new drugs, the explorations of many ancient and miraculous drugs hold promise. Herein, we discussed animal as the panacea, which may have great potential against the refractory diseases.
Fig. 1.
Six representative animal healers were conceived in the same context: The seriously ill old man is being treated by animal healers.
The animal healers are defined as natural animals that have direct or indirect therapeutic effects on diseases by acting directly on the patients through various means (including bite, parasitism, contact, communication, etc.). Currently, maggot therapy [2], helminth therapy [3], leech therapy [4], fish therapy [5], bee therapy [6] and pet therapy [7] are known animal treatment providing medical assistance. Among them, leech therapy, maggot therapy and pet therapy are more widely used in clinical practice and have been undergone extensive study. Unlike conventional biotherapy, which often relies on the biological characteristics of organisms to treat diseases, animal healers leverage direct interactions such as biting, parasitism, contact, and communication to offer treatment. For example, in the treatment of infectious wound, use of antibiotics often needs to consider the patient's systemic state, drug metabolism and drug resistance. There is no such concern with maggot therapy because it works directly on the wound to treat bacterial infections and promote healing [8]. Another example, leech therapy, eliminates shortcomings of traditional puncture and blood drawing methods. Its procedure is minimally invasive and has a significant analgesic effect [9]. However, there is not any article to introduce this method or summarize its research status. In this article, we propose the concept of animal healer and introduce six representative healers, currently including fish, pet, worm, leech, maggot and bee (Table 1).
Table 1.
Overview of animal healers.
| Name | Main selected species | Indications | Appropriate crowd | Usage | Mechanism of treatment | Side effects | Main existing problem |
|---|---|---|---|---|---|---|---|
| Fish therapy | Cyprinion macrostomus; Garra rufa | Skin diseases (psoriasis) | Patients who are no taboos about bathing; people with healthy immune systems | Patients and fishes bathe together | Gently exfoliating the skin | Cross contamination | How to enhance the effectiveness of fish therapy |
| Pet therapy | Dog; cat; dolphin; others | Mental and emotional disorders; pain; low quality of life | Patients with malignant tumors or mental illness | Pets are assigned to accompanied with patients | Emotional sustenance; kill time; attention diversion | Accidental injury; parasitic disease; allergy; bite | There is no standard measurement, pet type, and treatment plan |
| Worm therapy | Tapeworm; nematode; whipworm; blood fluke | Inflammatory bowel disease; encephalomyelitis; multiple sclerosis; type I diabetes; rheumatoid arthritis | Unknown | Patients are artificially parasitized with worms | Regulation of immune response; inhibition inflammatory process | Pruritus; enteropathy; eosinophilia | How to prevent worms from escaping; How to enhance the safety |
| Leech therapy | Hirudo nipponica | Venous congestive disease; knee osteoarthritis; chronic complex regional pain syndrome; diabetic foot; revascularization | Unknown | Place the leech in the lesion area of patients | Removal of the hematoma; release the effective substances | Infection; skin itching; secondary bleeding; anemia | How to promote infection prevention |
| Maggot therapy | Larvae of Calliphoridae | Infectious or refractory wounds | Patients who have no fear and psychological resistance | Place the larvae in the wound of patients | Debridement; anti-infection; healing promotion | Crawling feeling; pain; unpleasant odor | How to achieve standardized production and application |
| Bee therapy | Honey bee | Knee osteoarthritis; nerve-root type cervical spondylosis; peripheral vascular diseases | Patients who are negative response to bee venom | Clamp the bee and stab the bee venom into the patient's skin | Expansion and congest of local blood vessels; meridian stimulation | Intoxication; allergy | How to reduce toxic and side effects |
Due to limited treatment options for refractory diseases, a comprehensive and in-depth understanding of animal healers is imperative. Additionally, although many articles about animal healers have been published, there is still a lack of systematic combing and summary about efficacy, side effects, suitable population, disadvantages, and so on. Therefore, starting with classification, this review highlights the progress made so far in research involving animal healers, and it provides in-depth introduction to the currently known therapeutic mechanism, as well as those of animal healers that have already been applied to the treatment of different refractory diseases. This review also seeks to provide treatment optimization, determination of indications, improvement and species range expansion for subsequent scrutiny of animal healers, find new breakthroughs aimed at expanding the application of animal healers against refractory diseases and provide new suggestions for developing treatment strategies in the future.
2. Method
A search was conducted mainly applying the following key words: “fish therapy” “Ichthyotherapy”, “pet therapy”, “animal assisted therapy”, “worm therapy”, “helminthic therapy”, “leech therapy”, “hirudinization”, “maggot therapy”, “biological debridement therapy”, “bee therapy”, “bee-sting therapy”, “apitherapy”, “refractory disease”, “traditional Chinese medicine”, “Persian medicine”, “Ayurveda”, “Unani” and assorted combinations of these terms, in scholarly electronic databases, including PubMed, Google Scholar, Web of Science, Scopus, CNKI and WanFang DATA. The literature obtained via this means was reviewed for aggregating information on different types of treatment, as well as for developing the concept of “animal healer”. Relevant studies until March 2024 were selected. Regarding the treatment of animal healer, relevant literature from 2000 to March 2024 on the subject was selected, as was a small portion of earlier literature to ensure the integrity of the review and provide support.
The inclusion criteria of the generated literature were as follows: (1) Clinical and preclinical studies with all types of animal healer; (2) Studies of other species receiving animal healers.
The exclusion criteria were as follows: (1) Studies that have no relevance for disease treatment; (2) Studies on animal damage to humans during non-disease treatments.
3. Different treatment methods of animal healers
3.1. Fish therapy (Ichthyotherapy)
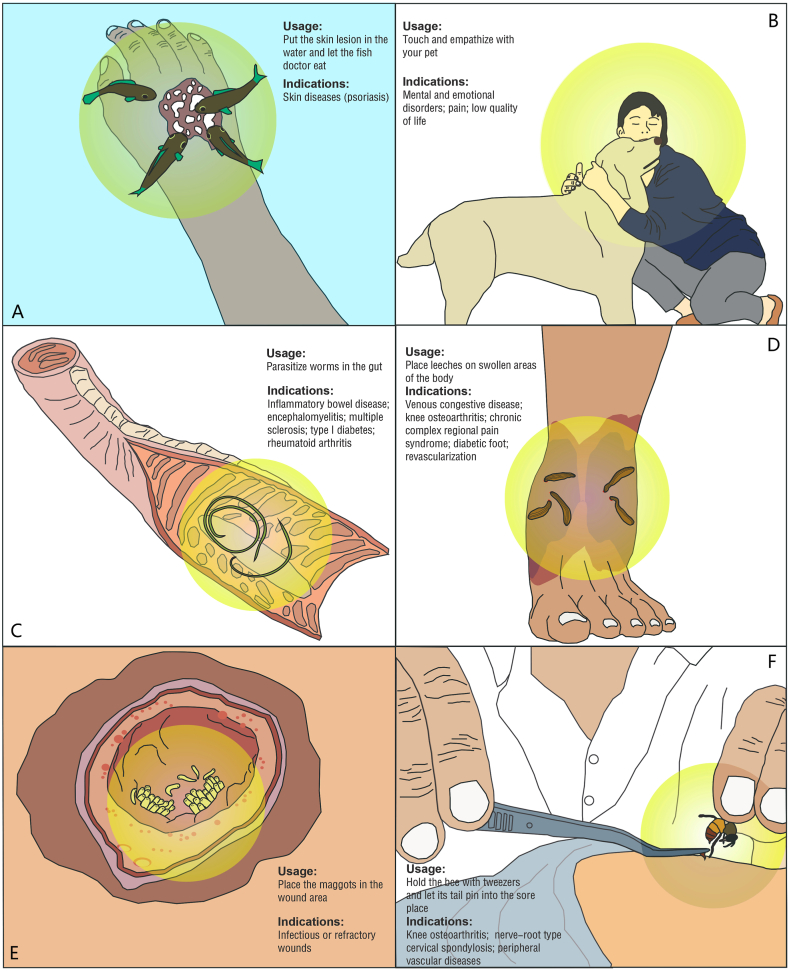
With recreational nature, fish therapy originated in Turkey and widely used around the world. It is regarded as a method to relieve fatigue and treat skin diseases with a simple and comfortable process. During bathing, fishes could chew and clean the dead epidermis and diseased skin (Fig. 2A). As a chronic inflammatory skin disease, psoriasis had a long course of disease and a tendency of recurrence. However, there was no specific therapy for psoriasis and some patients suffer from psoriasis for the whole life. Fish therapy may provide a promising method for remission and treatment of psoriasis.
Fig. 2.
Usage and indications of six animal healers: fish therapy(A), pet therapy (B), worm treatment (C), leech treatment (D), maggot treatment (E) and apitherapy (F).
Cyprinion macrostomus and Garra rufa are two species from Kangal hot spring in Turkey and were often used for fish therapy. Garra rufa is considered to be more effective. In the natural state, these healers feed on plankton rather than skin necrosis of mammals. Once adapted for therapeutic purposes, they have become beneficial to humans. Fish therapy was first reported in Lancet in 1989, showing that compared with the patients treated with corticosteroids, the remission period of psoriasis patients treated with fish therapy was significantly extended [10]. The short-term fish therapy, lasting four to 8 h, has a good effect on the relief of psoriasis. The therapeutic effect of fish therapy on psoriasis is probably related to the reverse Koebner phenomenon. Haemorrhagic lesion following fish attack may cause this special phenomenon to promote the skin recovery [11]. Between 2002 and 2004, Grassberger conducted a study treating psoriasis patients with fish therapy for three weeks [12]. The patients received fish therapy for 2 h in a separate bathtub at a suitable temperature every day and the results proved that fish therapy had a good effect on the treatment of psoriasis. In addition, the stronger natural ultraviolet radiation, higher selenium content and jacuzzi effect may play a positive role in improving the therapeutic effect of fish [12].
Currently, it is recognized that fish therapy could prolong the remission period of psoriasis patients and repair the damaged skin. However, it is noted that patients should be careful to avoid sunburn when performing fish therapy outdoors. Despite these benefits, current research faces several challenges, including the absence of control cases and a limited number of patient samples. More researches on the therapeutic mechanism are needed to advance its use and maximize its therapeutic effect. Furthermore, there is no conclusive evidence on whether fish therapy increases the risk of contracting diseases. Compared with conventional treatment, fish therapy has the advantages of acceptance and fewer side effects. In future, fish therapy may be expected to become an important method to treat skin diseases.
3.2. Pet therapy (Animal assisted therapy)
Pet therapy, recognized as a means to alleviate stress and improve the psychological state of patients, operates through the interaction between pets and their human companions. It is often performed to assist psychological counseling of terminal stage patients or mental patients (Fig. 2B). The main purpose of this treatment is diverting patients' attention and enriching patients' lives through the communication and interaction between patients and pets. The concept of using pet dogs or other animals as cooperative therapists dates back to the 1960s and was proposed by psychiatrist Boris M. Levinson, who described pets as "emotional mediators" and "catalysts" for socialization [13]. Many kinds of animals can be used in pet therapy, such as dogs, cats, dolphins, etc [14]. However, due to the limitation of funding, regions and other reasons, most studies used the pet dog as a treatment medium to explore the therapeutic effect of pet therapy on specific diseases.
The anesthetic effect of pet therapy on children's negative emotions is very significant. Pet dogs can significantly reduce children's physical pain and emotional distress [15]. Moreover, the psychological pressure of both parents and children could be significantly relieved [16]. Pet therapy could be used to help children suffering from malignant tumors for improving emotion, appetite, social engagement and participation of activity [17,18]. Pets can also entertain, reduce fear and anxiety, and bring children sense of safety [17]. For children with terminal cancer, pet therapy can improve their quality of life [18]. Furthermore, pet therapy is also used to assist in the treatment of attention deficit hyperactivity disorder [18]. Elderly patients are another vulnerable group that should be cared for. They often face psychological and physical problems. Pet therapy is the ideal auxiliary solution for these patients, as well [19]. Pet therapy could significantly improve the depression and quality of life of patients with severe dementia. But there was no effect on restlessness [19]. Pets could also improve patients' social and communication skill via the enhanced language and body language, which could improve happiness, self-esteem and optimistic attitude [20]. Pet therapy was considered to enhance the social and cardiovascular functions of the elderly in the community [21] and improve the symptoms of the elderly psychiatric patients [22]. It has also shown excellent efficacy on other types of patients, such as enhancing the feeling of well-being, reducing anxiety [23], reducing pressure [24,25], and creating a better treatment environment [26]. Other studies have found that pets can also be used to treat pregnant women with psychological disorder and the intellectual disabled with communication difficulty [27,28].
Pet therapy can be used as an auxiliary therapy of conventional treatment scheme, which affects the hormone level in patients, and then reduce anxiety and excitement of sympathetic nervous system [29]. However, there was a different viewpoint from Thodberg et al. that the pet therapy does not affect the long-term mental state of patients, and the effect on sleep time and other aspects still remains to be studied [30]. Although some studies have set up a control group, it is still not sure that pet therapy is more effective than other interventions. There are still some deficiencies in researches clinic about pet therapy, including the measurement standard, pet type, side effect, and treatment plan. In terms of side effects, accidental injury and transmission of parasites are problems that need to be addressed in pet treatment. By standardization and improvement, the healers will be the partners living together with the patients as well as the great complement in therapeutic process.
3.3. Worm therapy (Helminthic therapy)
Worm therapy refers to the treatment or adjuvant therapy for some diseases by artificially placing or ingesting worms into patient's digestive tract (Fig. 2C). Medical parasitology divides worms into nematodes, acanthocephalans, flukes and tapeworms. Nematodes include ascaris, hookworm, filariasis and trichinella. Except harm to the human body, their parasitics in the digestive tract have some unexpected positive effects.
Research has indicated that worms can easily parasitize in our body, increasing the metabolism of intestinal epithelial cells and promoting the recovery of normal intestinal function [31,32]. These organisms can trigger the type 2 immune response of the host and alternately activate macrophages and mast cells. This activation promotes the proliferation of goblet cells and the production of mucous [33]. Numerous studies have confirmed that worm therapy has a significant effect on inflammatory bowel disease [[34], [35], [36], [37], [38]]. Worms induce strong Th2 cell-mediated immune response as well as inhibit Th1 cell-mediated immune response to mucosa, and then possibly inhibit inflammatory bowel disease [35]. Schistosome eggs could reduce colitis and protect the intestine of mice from fatal inflammation [36]. It was worth noting that tapeworm was better than dexamethasone in the prevention of colitis in mice, and it would not lead to the side effects of collagen deposition [37]. Moreover, the larvae of the nematode heligmosomoides polygyrus can inhibit the symptoms of colitis induced by dextran sodium sulfate (DSS). Its mechanism was not only increasing the expression of inflammation-associated cytokines in the small intestine, but also inhibiting of the expression of these factors in the colon [38]. The eggs of swine whipworm were safe and effective in the treatment of active colitis [39]. For refractory diseases, worm therapy will be a new choice. For example, infection with schistosoma japonicum may decrease the incidence of encephalomyelitis by reducing the production of proinflammatory cytokines and improving the inflammation in the central nervous system [40]. Parasite infection significantly prolonged the deterioration times of patients with multiple sclerosis. It may be related to the protective effect of some cytokines induced by parasite [41]. Another research showed that worm infection can significantly inhibit type I diabetes in mice through the mechanism of independent CD25 and IL-10 [42]. It was also reported that schistosoma japonicum might be useful for rheumatoid arthritis [43]. Evaluation of the safety and effectiveness of worm therapy have been done in allergic rhinitis patients. Unfortunately, they proposed that there was not enough evidence to prove the effectiveness of worm therapy in the treatment of allergic rhinitis [44]. There are a series of reports about the mechanism of immunotherapy about worms, focus on the regulation of inflammatory response and the improvement of immune system [45,46].
Despite its potential, worm therapy faces several challenges, including the possibility of affecting drug efficacy through immune response regulation and increasing infection risks in immunocompromised hosts due to parasite implantation [47]. To a certain extent, the emergence of side effects such as pruritus, enteropathy and eosinophilia also restricted the application of worm therapy. Another stumbling block is the cost that involved production and application. In addition, it is also very difficult to prevent worm escape while treating [48]. In future, the focus of research will be the reasonable selection of species and state of worms, improvement of the safety, and the formulation of standardized methods.
3.4. Leech therapy (Hirudinization)
In nature, leeches attach to the surface of the host body and pierce the skin through mouthparts to feed on blood, similar to mosquitoes. While this may seem harmful to humans, leech therapy has significant therapeutic value for certain diseases (Fig. 2D). Dating back to ancient Rome 3500 years ago, leech therapy experienced a revival in the second half of the 20th century [49]. Ancient Ayurveda and Unani have accumulated rich experience in the use of leech therapy. They are good at using leeches for removing hematoma and prmoting the healing of skin and soft tissue diseases [[50], [51], [52]]. Leech therapy is also an important component in the development of treating varicose veins in Persian medicine [53]. The hirudin contained in leech's body is known as the most effective natural coagulant inhibitor. Because of the blood-sucking habit, Hirudo nipponica was most commonly used.
The properties of leeches to absorb blood has been used in studies to improve blood circulation, showing significant effect in the treatment of venous congestive diseases [54,55]. Lee et al. placed the leeches on the open incision line in the dark position of fingers. After the leeches fall off by themselves, the wound is wiped with gauze stained with heparin solution to facilitate blood outflow. The result showed that leech therapy could help patients with severed fingers to reconstruct blood circulation and to provide the success rate of plantation surgery [56]. Moreover, the effectiveness of leech therapy has been found in the treatment of chronic musculoskeletal diseases. Michalsen et al. placed four to six medicinal leeches on the soft tissue around the knee, until the leeches and the patient's skin were separated [57]. After that, the pain and symptoms of knee osteoarthritis were significantly relieved, suggesting long-term treatment value for chronic conditions [57]. Kulbida et al. applied leech therapy to chronic complex regional pain syndrome, the symptoms of pain intensity in patients were alleviated rapidly, and the active and passive degree of affected limbs was also improved significantly [58]. Hohmann et al. conducted the first randomized controlled trial of leech therapy for chronic low back pain, demonstrating that leech therapy was effective in lowering the intensity of pain and improving the quality of life [59]. Furthermore, the end measure of gangrene in diabetic foot patients is often debridement and amputation. Leech therapy can also be used for the complications treatment of diabetic foot to alleviate the progression of gangrene [60]. In addition, leech therapy may also be effective in some special diseases, such as priapism [61], promoting skin flap survival after long-term ischemia [62]. It was also played an important role in the field of plastic surgery [63]. The saliva of leeches consists of anesthetic components, anticoagulant components and vasodilator components, which can not only mask the pain of the host, but also effectively prevent the wound healing after blood coagulation [64].
Despite its benefits, the main complication of leech therapy is infection, including cellulitis, perianal abscess, and keratitis, with infection rates reported between 2 % and 36 % [[65], [66], [67], [68]]. Additionally, the bites of leech can cause mild skin itching, which can last for hours to three days [63]. Due to the saliva of leeches contains anticoagulant and vasodilator components, secondary bleeding and anaemia after leech treatment also occurs sometimes [67,68]. Even so, the potential of this animal healer in medical field has attracted wide attention, including pain syndrome, inflammatory conditions, reconstructive surgeries, dentistry, and ophthalmological and ear nose throat disorders.
3.5. Maggot therapy (Biological debridement therapy)
Maggot therapy is an ancient animal healer, using medical maggots to clear the necrotic tissue in the wound, kill bacteria, promote the growth of granulation (Fig. 2E). The larvae of Calliphoridae, such as Lucilia sericata, Chrysomyia megacephala and Lucilia cuprina, have been regarded as the mediums for this treatment. In China, as a part of traditional Chinese medicine (TCM), maggot has a long history. The ancient Chinese regarded maggot as the panacea for both wound and dyspepsia. Ayurveda considered that the therapeutic process of maggots accorded with Krimi Utpattikara Chikitsa. And debridement and disinfection are two significant effects in maggots’ promoting wound healing [69]. The observation of confocal microscopy showed that maggots could phagocytize and kill E.coli by its midgut [70]. With the continuous development of researches, maggots have been proved to have the ability of anti-biofilm, anti-inflammatory, healing wound and can also enhance tissue proliferation and repair [71,72]. Via crawling, maggots can stimulate the wounded surface to accelerating healing [73]. The secretions and excretions of maggots contain deoxyribonuclease, growth promoting factors, serine enzyme and non-proteolytic auxiliary factors, which initiate the mechanisms of wound repair [[74], [75], [76]]. Recently, maggots have been used to work in synergy with antibiotics aiming at exploring the potential mechanism of combined antibacterial [[77], [78], [79]].
Maggot therapy is recognized as a safe and effective wound treatment method, offering lots of advantages, such as effectively reducing the use of antibiotics, wide indications, shortening the length of stay, auxiliary debridement and lightning the workload of doctors [80]. At the same time, it is cost-effective for the patient and healthcare providers from both an economic and a medical perspective [81]. In the last century, researchers began to treat osteomyelitis by maggots and found the necrotic and deactivated tissue in the wound can be removed rapidly, forming healthy granulation tissue, and accelerating the healing of the wound [82]. The strong anti-infective ability of maggot therapy was soon aroused attention of the lancet [83]. For debridement effect, maggot therapy has obvious and efficient ability. In a study on refractory wounds, researchers placed a certain amount of maggots on the wounds and found that the superficial wounds can be cleaned quickly [84]. A retrospective study was done to compare the changes of necrotic area of chronic wound under maggot therapy and standard treatment [85]. The result showed that maggot therapy had better effect in promoting the healing of lower limb ulcer. Maggot therapy could play a remarkably effective role on promoting wound healing [85]. Dumville et al. carried out a study on maggots in the treatment of leg ulcers, which illustrated that Maggot therapy shortened the time to heal leg ulcers compared with hydrogels [86]. Moreover, the curative effect of maggot therapy in pressure sore cases was also cheerful [87]. Seven different types of hard-to-heal wounds were successfully cured by the combined application of maggot treatment and moist burn ointment, including scar ulcer, pressure ulcer, skin necrotic wound, iatrogenic incision, diabetic foot ulcer, traumatic skin ulcer, and infective skin ulcer [8]. Additionally, maggot therapy seems to be an effective way to cure malodorous and infectious cancer wounds [88]. Some secretions of maggots can help control cancer by inhibiting proliferation and migration [89]. Maggot therapy have been used to treat equine sarcoid with the satisfactory effect [90]. Based on the findings, we believe that it is a promising way to promote tissue repair.
However, it is undeniable that there are still many practical problems to be solved in maggot therapy. For medical maggots, the problems mainly focus on maggot acquisition, use time and treatment plan. For patients whom received treatment, shortcomings like potential psychological resistance, possible pain symptoms and occasional anaphylaxis can not be ignored. In the future, the primary research directions of Maggot therapy focus on the standardized cultivation, transportation and preservation of medical maggots, improvement of treatment methods, collaborative application with other drugs and other aspects.
3.6. Bee therapy (Apitherapy)
Bee therapy has a long history in TCM, with the ancient Chinese medical text "Huang Di Nei Jing Su Wen" documenting the concept of "attacking poison with poison. Approximately 2500 years ago, Hippocrates utilized bee therapy to treat his patients [91]. It has also been reported that this therapeutic modality in use since at least the second century BC in Eastern Asia [92]. The discovery of this treatment is closely related to the honey gathering activities of ancient humans in the wild. In term of the concept of bee therapy, factitious bee sting was applied to the meridians and acupoint to generate mechanical stimulation and had the mixed effect of acupuncture, medicine and warming moxibustion (Fig. 2F). From the perspective of TCM, the theory of this animal healer does not seem complicated. Bee acupuncture was similar to acupuncture and the venom were the main factors. It has the advantages of economical, simple, fast and effective. The pharmacological effect of bee venom on the body could promote the local blood vessels to expand and congest, which promote warming meridians and collaterals, activating blood circulation, and reducing pain [93]. Additionally, bee therapy alleviated RA effects and all rheumatoid factor markers were significantly reduced [92].
Among the studies, researchers used needle of honeybee to stab the acupoint at knee joints, and then the bee needle was carefully put out via forceps [94]. The later clinical observation results indicated that bee therapy had a definite effect on knee osteoarthritis, which is superior to conventional acupuncture therapy in both pain relief and long-term effect [94]. Nerve-root type cervical spondylosis often follows intractable pain and persistent numbness and lack effective conservative treatment. Pan et al. performed a study including seventeen nerve-root type cervical spondylosis patients and inserted bee needle into the cervical acupoint [95]. It was proved that bee therapy had significant effect on the improvement of symptoms, and most of the patients did not recur after one year [95]. To clarify the efficacy of bee therapy on appendicitis, one bee therapy study of patients with appendicitis was performed [96]. In the process of treatment, patients regularly took 10 ml bee product mixture such as honey and royal jelly. After 1–3 courses of bee therapy, all patients were cured without recurrence in the next six months [96]. In addition, the team found that a similar combination of bee therapy could treat cervical lymph tuberculosis and inhibit tumor progression [97]. Another study was applied to the treatment to relieve cancer pain and the result showed analgesic effect of bee therapy was not only better than that of conventional therapy, but also had a certain inhibitory effect on tumor growth [98]. Bee therapy was also believed to have effect on reducing the symptoms in patients with peripheral vascular diseases and improving the quality of their lives [99,100]. In addition, bee therapy also has a good therapeutic effect on gynecopathy such as hyperplasia of mammary gland [101,102].
Most of the researches on bee therapy have positive results. But xiong et al. searched 589 literature reports and found a relatively low level of evidence for bee-related treatments [103]. There are also some side-effects in this therapy. After bee sting, patients may develop three main symptoms like systemic reactions, local allergic reactions, and digestive discomfort [104]. In order to reduce adverse reactions, researchers have made many attempts. Kwon and Hwang tried to change the therapy method by needle dipping in bee venom instead of living bees, which could control the amount of bee venom entering the body [105,106]. TCM painless bee therapy has been introduced, including focus on improved breeding, manipulation techniques, and acupoint selection to eliminate pain [107]. Allergic reactions and infections remain the most common side effects of apitherapy. ddressing these challenges, the development of apitherapy relies on solving a series of problems, mainly including improving the quality of clinical research and achieving treatment without side effects. There still are reasons to believe that the application prospect and scientific value of bee therapy in solving various stubbornt diseases are worth looking forward to.
3.7. Others
In recent years, more and more creatures are being used as animal healers. Although no formal studies provide reliable data for reference and verification, some animal healers still caused widespread concern in the medical community. For example, Baldness is known as a refractory skin disease, which has long plagued many male patients. There seems no effective treatment in cases where medication is largely ineffective. According to the records of TCM “Thousand Golden Prescriptions”, cattle lick is able to cure baldness. Researchers found that this method could actually help hair to regenerate, because saliva contained many enzymes and growth-promoting proteins [108]. From the perspective of TCM, licking may play a role of massage to promote local blood circulation and hair growth. Similar treatments could also be found in other ancient medicine [109]. Additionally, it was found that the symptoms like weight loss, bloody diarrhea, colon shortening and damage of colon tissue were significantly improved in these mice after trichinella papuae therapy, which gave the possibility for single-celled organisms to work as animal healer [110]. While encouraging, we cannot ignore the side effects of these emerging animal healers. The selection of animal healers for treatment also requires sufficient preliminary research, good standards, and the established plan to deal with side effects.
4. Discussion
It is well known that animals are human's best companions. The relationship, especially the doctor-patient relationship between humans and animals, could not be ignored. The pace of medical development will never stop, and the advanced development of drugs and technologies has cured a vast number of patients. Unfortunately, for refractory diseases including chronic wounds, autoimmune diseases, psoriasis and depressive disorders, as well as some rare diseases, traditional treatment seems to struggle to get satisfied results. In primitive society, dangers from nature were everywhere. The outdoor collection and farming experience of the ancient time brought the new inspiration of medical development. Therefore, we present the opinion of animal healer and believe that it will play an increasingly inestimable role in the field of medicine.
4.1. Categories of animal healers
According to the mode of action, animal healers can mainly be divided into four categories: parasitism, bite, contact and communication. Leech therapy, maggot therapy, and worm therapy can be considered as a kind of therapy based on parasitism. The host provides the nutrition for parasites, and the creatures can delay, inhibit, or even reverse the development of the host's disease. Additionally, some creatures can use special structure to pierce the skin of patients, or use their biological functions and secretions to affect the progress of the diseases. The last therapy works by touching. Pet therapy, as a classic example, also achieves results through physical contact and interaction with patients.
Based on the habits of living creatures, animal healers can be divided into two different categories. The first category is the creatures attach to body surface and easy to be detected. Leeches fed on blood and indirectly improve blood circulation of the host. With the increase of blood intaking, the size of leeches will increase at the same time. Maggots clean up the necrotic tissue rapidly with high efficiency. There are changes not only in body size but also at instars of the maggots, which can even be captured by the naked eye. Pet healers also express their happy emotions through behaviors and actions that can be found by both patients and doctors. The second category involves therapies that cannot be judged through simple observation. It is often found that the diseases improve unconsciously after the patients contact with the creatures. The process of bee acupuncture is fast, but it takes a long time to work in vivo. Therefore, the curative effect may not be judged by observation of the bee used.
4.2. Social economics, welfare and ethics
The current status of animal healers indicates significant economic benefits from this treatment method, despite it not being widely applied yet. Maggots, fishes, leeches, pets, and bees have already seen their services priced or included on regional price lists. The sources of costs involved capture, breeding, feeding, training, disinfection, vaccination, transportation, and final treatment. Treatment is charged in two forms: by quantity or by course of treatment. Maggot is the most standardized and clear type of charge at present. Medical maggot was approved by the Food and Drug Administration (FDA) as a medical device in 2004 [111]. Subsequently, the American Medical Association and Centers for Medicare and Medicaid approved reimbursement coding guidelines for maggot therapy [112]. In Poland, one hundred medical maggots cost about 26–44 EUR [113]. Soares et al. found the average cost of maggot therapy was 1696–1833 GBP through the clinical data research of 267 leg ulcers [114].
Fish therapy actually evolved from a fee-based spa program. At present, Turkish Ministry of Health has designated the Kangal Spring as a certified health center to offer a 21-day treatment for worldwide patients with psoriasis [115]. In 2004, the FDA also approved leeches for clinical use as medical devices at a recommended price of 7–10 USD each [116].
Pet therapy appears to be the most widely used treatment. Pets may play a therapeutic role in several ways since they establish a close relationship with their owners. This is an expensive treatment. Using guide dog pricing as a reference, the average total cost per dog during his or her work cycle was 40,598 USD. And the average cost of dog guide ownership per year over the working life of the animal was 2379 USD [117]. Bee therapy seems mainly used in China, outpatient clinics featuring bee therapy have made use of this particular method to solve difficult conditions. It has been included in China medical service price item specification sincec 2007, but the price of the treatment remains unclear [118]. However, it may take a long time before worm therapy to be both commoditized and charged. And no report on economics has been found.
As the relationship between humans and animals grows closer, the research interest in evaluating the influence of human proximity behavior towards animals on animal welfare has increased [119]. The potential harm to animal healers also deserve extensive attention. The welfare of therapy dog is studied more deeply and its definition includes absence of stress and positive emotions [120]. Handler are the principal person responsible for their dog welfare who can recognize the signs of stress to get them out of the uncomfortable situation. Guidelines to handlers should be established based on applied ethology [120]. Additionally, because to lack of animal welfare, fish therapy is not allowed in many parts of the US, Canada, and Europe [121]. Welfare studies for other animal healers are still unknown. The ethics of treatment for animal healers have not been described in detail. All available is approval from the ethics committee of the medical institution where the treatment was performed.
4.3. Management and optimization
Although there was no special criteria and conception for animal healing in the past, this therapy method still had made great progress. It is mainly reflected in the optimization of treatment methods and expansion of indications. Creatures that can be used as healers are mostly wild. Similar to domesticated livestock and insect, animal healers are also need to be specially treated, bred or domesticated. Almost all animal healers need to go through artificial process. Because side effects can not be ignored (Table 1). Fish therapy seems to be the safest but there is still a risk of cross infection. Ensuring cleanliness of both water and treatment area is a reasonable coping approach. The patient with acute exacerbation of severe skin diseases is not suitable for treatment with fish therapy. Accidental injury, parasitic disease, allergy and bite are main side effects of pet therapy. Trained pets often improve the safety of pet therapy after regular vaccination. Pet therapy is not a good option for patients who are susceptible to allergies. Worms are mainly used to treat autoimmune diseases, so its main complication is directly related to the immune dysregulation. This treatment may be more appropriate for the adult population, provided worms are well disinfected. Bacteria in the salivary glands and digestive tract of leeches may cause infection and pruritus. This is very important for the quality control of medical leeches. After the method of leech treatment is standardized, the incident of secondary bleeding and anemia will also significantly decrease. This treatment is not recommended for patients with abnormal coagulation function and anemia. As a commonly used animal healer in clinical practice, the side effects of maggot treatment are highlighted by crawling feeling, pain and unpleasant odor. The maggots confined in container or mesh bag provides a great help in reducing the crawling feeling during treatment. Painkillers can be administered to patients during maggot therapy. Maintaining ventilation in the room is a good way to change the undesirable odor caused by the treatment. Patients with psychological illness or mental disorder should not use this method. The essence of bee therapy is to pierce the venom into the body of the patient, so it is also a relatively dangerous treatment. Intoxication and allergy are the most significant complications. Artificial breeding of bees to reduce both toxicity and sensitization is an urgent problem to be solved. This treatment is not suitable to use in people who are susceptible to allergies. However, adding allergen testing before formal treatment is beneficial to exclude maladaptive populations.
To improve the safety, convenience and efficacy, many efforts of both research and clinic experts have been done to promote the development and application of animal healers. Combined with selenium-rich hot spring and modest ultraviolet, fish therapy may achieve better therapeutic effect [11]. Active maggots prefer to constantly wandering and cause patients to have crawling feeling. This always leads to develop patients' fears for maggot therapy. On the premise of ensuring vitality and ability, maggots could be enclosed in biological packs that were made of special materials [8]. By this indirect contact, patient's discomfort and fear could be dramatically reduced. Bee venom contains lots of toxic substance that is the main cause of side effects, so bee therapy must be modified for much safe. Now, bee therapy is advocated for some new methods, needles with appropriate bee venom and bee therapy combined with special acupuncture methods of TCM [122,123]. This measure greatly protects the treatment safety of patients. Leech therapy was very popular in Europe, but its main causes of side effects were the hemorrhagic shock and infection. Studies have shown that about 20 % patients suffering from wound infection [124]. To prevent infection, researchers found 0.02 % chlorhexidine solution could effectively kill aeromonas hydrophilus in the intestinal tract of leech. Results indicated the risk of infection was dramatically reduced by pre-use disinfection [125]. Moreover, pets that directly contact with the patient usually need to be immunized with vaccines. Most of them should receive special training for supplying with more help to the patients.
4.4. Advantages and limitations
A relatively convenient method of use and a wide range of indications are the significant advantages of animal healers. It is emphasized to make full use of the natural relationship between human and creature for treatment, such as the accompanying relationship between human and pets, the parasitic relationship between worms and human beings, and the stress relationship after bee venom enters the human body. The impact of this natural relationship on human body is more in line with human psychophysiology, so people are more likely to accept this kind of therapy. In the long term, both the medical institutions and the patients will reap greater benefits.
Despite its long history, limitations of animal healers cannot be ignored. Artificial screening and purification culture is the first hurdle. Then, strictly standardized processes and relevant laws should be developed from capture to clinical application of the animal healers. In many countries, animal healers are still seen as unconventional method, which cannot be subject to medical insurance funds and the doctors are also not interested in using the method. The data from clinical trials and number of patients have been lacking to date. More randomized controlled trials are also needed to optimize usage and indications, while exploring more compatible drugs. Although it is certain that animal healers play an important role in the process of treatment, the therapeutic mechanisms of these creatures are still veiled.
5. Conclusions and perspectives
The animal healer must be considered as an interdisciplinary subject including medicine, nursing, parasitology, zoology, health law and ethics. The development of a standard set of treatment protocols or tools can facilitate the internationalization of treatment and ethics, while enabling patients to subjectively evaluate the approaches. As animal healers become available within more countries' national health care systems, the accessibility of this approach and the demand for related products will gradually increase. The corresponding production and treatment costs will gradually decrease, thus bringing immeasurable economic benefits while improving the medical efficacy. In addition, there is a great deal of medical wealth in nature. The emergence of new animal healer species should also be adequately studied and verified.
Fish therapy cleans the diseased skin tissue by chewing. Pet therapy changes the hormone levels in patients’ body through communication and interaction. Worm therapy can stimulate the immune response. Leeches improve blood circulation through the active constituents in the body. And maggots can remove the necrotic tissue while secreting antibacterial and enzymes that promote the growth of healthy tissue. However, most mechanisms of animal healers are still unknown and need to be further explored by researchers, which is going to be a huge area of research. In the future, the emergence of new animal healers should be fully studied and validated, and artificial intelligence and bio-simulation can also be used to mimic the therapeutic effects of animal healers.
In conclusion, safety, efficiency, and lower side effects will be the rules for the development of animal healers. The animal healers will become guardians of human health.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Funding
This study was supported by the National Key R&D Program of China (2022YFA1207500), and National Natural Science Foundation of China (82072412/92048205/82204822).
CRediT authorship contribution statement
Mingzhi Song: Writing – review & editing, Writing – original draft, Validation, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Conceptualization. Changru Zhang: Writing – original draft. Simengge Yang: Writing – original draft, Formal analysis. Jialin Lu: Writing – original draft, Investigation. Tianze Sun: Writing – review & editing, Investigation. Heyue Li: Writing – original draft. Liang Tang: Writing – original draft. Kerong Dai: Writing – review & editing. Chaozong Liu: Writing – review & editing, Supervision. He Meng: Writing – review & editing, Supervision. Jinwu Wang: Writing – review & editing, Writing – original draft, Supervision, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Not applicable.
Contributor Information
Chaozong Liu, Email: chaozong.liu@ucl.ac.uk.
He Meng, Email: menghe@sjtu.edu.cn.
Jinwu Wang, Email: wangjw-team@shsmu.edu.cn.
Abbreviations
- TCM
Traditional Chinese Medicine
- FDA
Food and Drug Administration
References
- 1.United Nations World social report 2023: leaving no one behind in an ageing world. UN DESA Publications. 2023 https://desapublications.un.org/publications/world-social-report-2023-leaving-no-one-behind-ageing-world [Internet] Available from: [Google Scholar]
- 2.Chung M.M.T., Fang S.Y.J., Yeung A.P.C., et al. Hybrid approach in sacral sore management with maggot debridement therapy and flap reconstruction. JPRAS Open. 2023;39:95–100. doi: 10.1016/j.jpra.2023.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu X., Gao H., Duan S., Ding W., Yang X. A review of the clinical progress on helminths and their derivative products in autoimmune disease. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2023;39(12):1132–1140. PMID: 38140874.(Article in Chinese) [PubMed] [Google Scholar]
- 4.Mojahedi M., Alizadeh M., Kebria A.S., Parvizi M.M. Successful maintenance treatment of a patient with chronic dermatitis with leech therapy. J. Res. Med. Sci. 2023;28:60. doi: 10.4103/jrms.jrms_199_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shih T., Khan S., Shih S., Khachemoune A. Fish pedicure: review of its current dermatology applications. Cureus. 2020;12(6):e8936. doi: 10.7759/cureus.8936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weis W.A., Ripari N., Conte F.L., et al. An overview about apitherapy and its clinical applications. Phytomedicine. 2022;2(2) [Google Scholar]
- 7.Villarreal-Zegarra D., Yllescas-Panta T., Malaquias-Obregon S., Dámaso-Román A., Mayo-Puchoc N. Effectiveness of animal-assisted therapy and pet-robot interventions in reducing depressive symptoms among older adults: a systematic review and meta-analysis. Compl. Ther. Med. 2024;80 doi: 10.1016/j.ctim.2024.103023. [DOI] [PubMed] [Google Scholar]
- 8.Song M., et al. Combined application of moist exposed burn ointment and maggot therapy in wound healing. J. Wound Care. 2022;31(Sup10):S41–S52. doi: 10.12968/jowc.2022.31.Sup10.S41. [DOI] [PubMed] [Google Scholar]
- 9.Mishra V., Shindhe P.S., Killedar R.S. Protocol based pain management by Ayurveda parasurgical procedures W.S.R to musculoskeletal pain and its critical appraisal - an open labeled clinical trial. J. Ayurveda Integr. Med. 2022;13(4) doi: 10.1016/j.jaim.2022.100665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warwick D., Warwick J. Turkey the doctor FISH-A cure for psoriasis? Lancet. 1989;334(8671):1093–1094. [Google Scholar]
- 11.Ozcelik S., et al. Kangal hot spring with fish and psoriasis treatment. J. Dermatol. 2000;27(6):386–390. doi: 10.1111/j.1346-8138.2000.tb02188.x. [DOI] [PubMed] [Google Scholar]
- 12.Grassberger M., Hoch W. Ichthyotherapy as alternative treatment for patients with psoriasis: a pilot study. Evid Based Complement Alternat Med. 2006;3(4):483–488. doi: 10.1093/ecam/nel033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levinson B.M. The dog as a "co-therapist". Ment Hyg. 1962;46:59–65. [PubMed] [Google Scholar]
- 14.Kamioka H., et al. Effectiveness of animal-assisted therapy: a systematic review of randomized controlled trials. Compl. Ther. Med. 2014;22(2):371–390. doi: 10.1016/j.ctim.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Sobo E.J., Eng B., Kassity-Krich N. Canine visitation (pet) therapy: pilot data on decreases in child pain perception. J. Holist. Nurs. 2006;24(1):51–57. doi: 10.1177/0898010105280112. [DOI] [PubMed] [Google Scholar]
- 16.Gagnon J., et al. Implementing a hospital-based animal therapy program for children with cancer: a descriptive study. Can. Oncol. Nurs. J. 2004;14(4):217–222. doi: 10.5737/1181912x144217222. [DOI] [PubMed] [Google Scholar]
- 17.Urbanski B.L., Lazenby M. Distress among hospitalized pediatric cancer patients modified by pet-therapy intervention to improve quality of life. J. Pediatr. Oncol. Nurs. 2012;29(5):272–282. doi: 10.1177/1043454212455697. [DOI] [PubMed] [Google Scholar]
- 18.Schuck S.E., et al. Canine-assisted therapy for children with ADHD: preliminary findings from the positive assertive cooperative kids study. J. Atten. Disord. 2015;19(2):125–137. doi: 10.1177/1087054713502080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olsen C., et al. Effect of animal-assisted interventions on depression, agitation and quality of life in nursing home residents suffering from cognitive impairment or dementia: a cluster randomized controlled trial. Int. J. Geriatr. Psychiatr. 2016;31(12):1312–1321. doi: 10.1002/gps.4436. [DOI] [PubMed] [Google Scholar]
- 20.Peluso S., et al. Animal-assisted therapy in elderly patients: evidence and controversies in dementia and psychiatric disorders and future perspectives in other neurological diseases. J. Geriatr. Psychiatr. Neurol. 2018;31(3):149–157. doi: 10.1177/0891988718774634. [DOI] [PubMed] [Google Scholar]
- 21.Krause-Parello C.A., Kolassa J. Pet therapy: enhancing social and cardiovascular wellness in community dwelling older adults. J. Community Health Nurs. 2016;33(1):1–10. doi: 10.1080/07370016.2016.1120587. [DOI] [PubMed] [Google Scholar]
- 22.Moretti F., et al. Pet therapy in elderly patients with mental illness. Psychogeriatrics. 2011;11(2):125–129. doi: 10.1111/j.1479-8301.2010.00329.x. [DOI] [PubMed] [Google Scholar]
- 23.Petranek S., Pencek J., Dey M. The effect of pet therapy and artist interactions on quality of life in brain tumor patients: a cross-section of art and medicine in dialog. Behav. Sci. 2018;8(5):43. doi: 10.3390/bs8050043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wood E., et al. The feasibility of brief dog-assisted therapy on university students stress levels: the PAwS study. J. Ment. Health. 2017;27(3):263–268. doi: 10.1080/09638237.2017.1385737. [DOI] [PubMed] [Google Scholar]
- 25.Ein N., Li L., Vickers K. The effect of pet therapy on the physiological and subjective stress response: a meta-analysis. Stress Health. 2018;34(4):477–489. doi: 10.1002/smi.2812. [DOI] [PubMed] [Google Scholar]
- 26.Coakley A.B., Mahoney E.K. Creating a therapeutic and healing environment with a pet therapy program. Compl. Ther. Clin. Pract. 2009;15(3):141–146. doi: 10.1016/j.ctcp.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynch C.E., et al. Pet therapy program for antepartum high-risk pregnancies: a pilot study. J. Perinatol. 2014;34(11):816–818. doi: 10.1038/jp.2014.120. [DOI] [PubMed] [Google Scholar]
- 28.Scorzato I., et al. Effects of dog-assisted therapy on communication and basic social skills of adults with intellectual disabilities: a pilot study. Intellect. Dev. Disabil. 2017;55(3):125–139. doi: 10.1352/1934-9556-55.3.125. [DOI] [PubMed] [Google Scholar]
- 29.Handlin L., et al. Short-term interaction between dogs and their owners: effects on oxytocin, cortisol, insulin and heart rate—an exploratory study. Anthrozoös. 2015;24(3):301–315. [Google Scholar]
- 30.Thodberg K., et al. Therapeutic effects of dog visits in nursing homes for the elderly. Psychogeriatrics. 2016;16(5):289–297. doi: 10.1111/psyg.12159. [DOI] [PubMed] [Google Scholar]
- 31.Artis D., Grencis R.K. The intestinal epithelium: sensors to effectors in nematode infection. Mucosal Immunol. 2008;1(4):252–264. doi: 10.1038/mi.2008.21. [DOI] [PubMed] [Google Scholar]
- 32.Lindholm H.T., et al. BMP signaling in the intestinal epithelium drives a critical feedback loop to restrain IL-13-driven tuft cell hyperplasia. Sci Immunol. 2022;7(71):eabl6543. doi: 10.1126/sciimmunol.abl6543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gerbe F., et al. Intestinal epithelial tuft cells initiate type 2 mucosal immunity to helminth parasites. Nature. 2016;529(7585):226–230. doi: 10.1038/nature16527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hou X., et al. Protective effect of Schistosoma japonicum eggs on TNBS-induced colitis is associated with regulating Treg/Th17 balance and reprogramming glycolipid metabolism in mice. Front. Cell. Infect. Microbiol. 2022;12 doi: 10.3389/fcimb.2022.1028899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elliott D.E., et al. Does the failure to acquire helminthic parasites predispose to Crohn's disease? Faseb. J. 2000;14(12):1848–1855. doi: 10.1096/fj.99-0885hyp. [DOI] [PubMed] [Google Scholar]
- 36.Elliott D.E., et al. Exposure to schistosome eggs protects mice from TNBS-induced colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2003;284(3):G385–G391. doi: 10.1152/ajpgi.00049.2002. [DOI] [PubMed] [Google Scholar]
- 37.Melon A., et al. Infection with Hymenolepis diminuta is more effective than daily corticosteroids in blocking chemically induced colitis in mice. J. Biomed. Biotechnol. 2010;2010 doi: 10.1155/2010/384523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Donskow-Łysoniewska K., et al. Heligmosmoides polygyrusfourth stages induce protection against DSS-induced colitis and change opioid expression in the intestine. Parasite Immunol. 2012;34(11):536–546. doi: 10.1111/pim.12003. [DOI] [PubMed] [Google Scholar]
- 39.Summers R.W., et al. Trichuris suis therapy for active ulcerative colitis: a randomized controlled trial. Gastroenterology. 2005;128(4):825–832. doi: 10.1053/j.gastro.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 40.La Flamme A.C., Ruddenklau K., Backstrom B.T. Schistosomiasis decreases central nervous system inflammation and alters the progression of experimental autoimmune encephalomyelitis. Infect. Immun. 2003;71(9):4996–5004. doi: 10.1128/IAI.71.9.4996-5004.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Correale J., Farez M. Association between parasite infection and immune responses in multiple sclerosis. Ann. Neurol. 2007;61(2):97–108. doi: 10.1002/ana.21067. [DOI] [PubMed] [Google Scholar]
- 42.Liu Q., et al. Helminth infection can reduce insulitis and type 1 diabetes through CD25- and IL-10-independent mechanisms. Infect. Immun. 2009;77(12):5347–5358. doi: 10.1128/IAI.01170-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.He Y., et al. The inhibitory effect against collagen-induced arthritis by Schistosoma japonicum infection is infection stage-dependent. BMC Immunol. 2010;11:28. doi: 10.1186/1471-2172-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Croft A.M., Bager P., Kumar S. Helminth therapy (worms) for allergic rhinitis. Cochrane Database Syst. Rev. 2012;2012(4):CD009238. doi: 10.1002/14651858.CD009238.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang B., Gems D. Gross ways to live long: parasitic worms as an anti-inflammaging therapy? Elife. 2021;10 doi: 10.7554/eLife.65180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lothstein K.E., Gause W.C. Mining helminths for novel therapeutics. Trends Mol. Med. 2021;27(4):345–364. doi: 10.1016/j.molmed.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salgame P., Yap G.S., Gause W.C. Effect of helminth-induced immunity on infections with microbial pathogens. Nat. Immunol. 2013;14(11):1118–1126. doi: 10.1038/ni.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sobotková K., et al. Helminth therapy – from the parasite perspective. Trends Parasitol. 2019;35(7):501–515. doi: 10.1016/j.pt.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 49.Singh S.K., Rajoria K. Medical leech therapy in Ayurveda and biomedicine - a review. J. Ayurveda Integr. Med. 2020;11(4):554–564. doi: 10.1016/j.jaim.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koeppen D., Aurich M., Pasalar M., Rampp T. Medicinal leech therapy in venous congestion and various ulcer forms: perspectives of Western, Persian and Indian medicine. J Tradit Complement Med. 2019;10(2):104–109. doi: 10.1016/j.jtcme.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bopparathi S., K V.N.R. Diabetic foot ulcer with osteomyelitis, successfully treated with the holistic approach of multiple ayurvedic treatment modalities - a case report. Int J Surg Case Rep. 2023;107 doi: 10.1016/j.ijscr.2023.108315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kumar Bhatted S., Arun Shende H., Kumar Singh H., Kumar A. Ayurveda management of palmoplantar psoriasis (Vipadika) -a case report. J. Ayurveda Integr. Med. 2023;14(2) doi: 10.1016/j.jaim.2023.100704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Asadi M.H., Van Hee R., Khosravi A., et al. The historical course of varicose vein surgery in the Persian medicine. Acta Chir. Belg. 2023;123(6):589–600. doi: 10.1080/00015458.2023.2254603. [DOI] [PubMed] [Google Scholar]
- 54.Brzezinski P., et al. Case Report: positive outcome of medical leeches (hirudotherapy) for venous congestion. Malawi Med. J. 2015;27(1) doi: 10.4314/mmj.v27i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Buote N.J. The use of medical leeches for venous congestion. Vet. Comp. Orthop. Traumatol. 2017;27(3):173–178. doi: 10.3415/VCOT-13-10-0122. [DOI] [PubMed] [Google Scholar]
- 56.Lee Z.H., et al. Quantifying outcomes for leech therapy in digit revascularization and replantation. J. Hand Surg. 2019;44(4):414–418. doi: 10.1177/1753193418823595. [DOI] [PubMed] [Google Scholar]
- 57.Michalsen A., et al. Effectiveness of leech therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann. Intern. Med. 2003;139(9):724–730. doi: 10.7326/0003-4819-139-9-200311040-00006. [DOI] [PubMed] [Google Scholar]
- 58.Kulbida R., Mathes A., Loeser J. Beneficial effects of hirudotherapy in a chronic case of complex regional pain syndrome. Journal of Integrative Medicine. 2019;17(5):383–386. doi: 10.1016/j.joim.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 59.Hohmann C.D., et al. The effectiveness of leech therapy in chronic low back pain. Dtsch Arztebl Int. 2018;115(47):785–792. doi: 10.3238/arztebl.2018.0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zaidi S.M.A. Unani treatment and leech therapy saved the diabetic foot of a patient from amputation. Int. Wound J. 2016;13(2):263–264. doi: 10.1111/iwj.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Asgari S.A., Rostami S., Teimoori M. Leech therapy for treating priapism: case report. Iran. J. Public Health. 2017;46(7):985–988. [PMC free article] [PubMed] [Google Scholar]
- 62.Moosavian H.R., Mirghazanfari S.M., Moghaddam K.G. Effect of ischemia preconditioning and leech therapy on cutaneous pedicle flaps subjected to prolonged ischemia in a mouse model. Aesthetic Plast. Surg. 2014;38(5):1024–1029. doi: 10.1007/s00266-014-0399-y. [DOI] [PubMed] [Google Scholar]
- 63.Mumcuoglu K.Y. Recommendations for the use of leeches in reconstructive plastic surgery. Evid. base Compl. Alternative Med. 2014;2014:1–7. doi: 10.1155/2014/205929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ernst E. Born to suck – the return of the leech? Pain. 2008;137(2):235–236. doi: 10.1016/j.pain.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 65.Kilic M., Ak R. Orbital cellulitis due to leech therapy. Bull Emerg Trauma. 2019;7(3):335–336. doi: 10.29252/beat-0703020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mentes B.B., et al. Anal abscess due to leech therapy of hemorrhoids: mumbo jumbo is still in vogue. J. Surg. Case Rep. 2019;2019(7):rjz218. doi: 10.1093/jscr/rjz218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Özkaya D. Keratitis following leech therapy for periocular eczematous dermatitis: a case report. BMC Complement Med Ther. 2023;23(1):124. doi: 10.1186/s12906-022-03613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Green P.A., Shafritz A.B. Medicinal leech use in microsurgery. J. Hand Surg. 2010;35(6):1019–1021. doi: 10.1016/j.jhsa.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 69.Krishna N.H., Shilpa P.N., Chiranthkumar R. Maggot debridement therapy an Ayurvedic understanding. Journal of Ayurveda and Integrated Medical Sciences. 2020;5(1):118–121. [Google Scholar]
- 70.Mumcuoglu K.Y., et al. Destruction of bacteria in the digestive tract of the maggot of Lucilia sericata (Diptera: Calliphoridae) J. Med. Entomol. 2001;38(2):161–166. doi: 10.1603/0022-2585-38.2.161. [DOI] [PubMed] [Google Scholar]
- 71.Yan L., et al. Pharmacological properties of the medical maggot: a novel therapy overview. Evid. base Compl. Alternative Med. 2018;2018:1–11. doi: 10.1155/2018/4934890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sherman R.A. Mechanisms of maggot-induced wound healing: what do we know, and where do we go from here? Evid Based Complement Alternat Med. 2014;2014 doi: 10.1155/2014/592419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jarczyk G., et al. Use of Lucilia sericata blowfly maggots in the treatment of diabetic feet threatened with amputation. Acta Angiol. 2008;14(2):42–55. [Google Scholar]
- 74.Szecsi P.B., et al. A novel serine protease secreted by medicinal maggots enhances plasminogen activator-induced fibrinolysis. PLoS One. 2014;9(3) doi: 10.1371/journal.pone.0092096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Prete P.E. Growth effects of Phaenicia sericata larval extracts on fibroblasts: mechanism for wound healing by maggot therapy. Life Sci. 1997;60(8):505–510. doi: 10.1016/s0024-3205(96)00688-1. [DOI] [PubMed] [Google Scholar]
- 76.Brown A., et al. Blow fly Lucilia sericata nuclease digests DNA associated with wound slough/eschar and with Pseudomonas aeruginosa biofilm. Med. Vet. Entomol. 2012;26(4):432–439. doi: 10.1111/j.1365-2915.2012.01029.x. [DOI] [PubMed] [Google Scholar]
- 77.Cazander G., et al. Synergism between maggot excretions and antibiotics. Wound Repair Regen. 2010;18(6):637–642. doi: 10.1111/j.1524-475X.2010.00625.x. [DOI] [PubMed] [Google Scholar]
- 78.Peck G.W., Kirkup B.C. Biocompatibility of antimicrobials to maggot debridement therapy: medical maggots Lucilia sericata (Diptera: Calliphoridae) exhibit tolerance to clinical maximum doses of antimicrobials. J. Med. Entomol. 2012;49(5):1137–1143. doi: 10.1603/me12066. [DOI] [PubMed] [Google Scholar]
- 79.van der Plas M.J., et al. Combinations of maggot excretions/secretions and antibiotics are effective against Staphylococcus aureus biofilms and the bacteria derived therefrom. J. Antimicrob. Chemother. 2010;65(5):917–923. doi: 10.1093/jac/dkq042. [DOI] [PubMed] [Google Scholar]
- 80.Bazaliński D., et al. Effectiveness of chronic wound debridement with the use of larvae of Lucilia sericata. J. Clin. Med. 2019;8(11):1845. doi: 10.3390/jcm8111845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bazaliński D., et al. The use of Lucilia sericata larvae in the treatment of chronic wounds—a study of three cases. 2018;15:105–111. [Google Scholar]
- 82.Mclellan N.W. The maggot treatment of osteomyelitis. Can. Med. Assoc. J. 1932;27(3):256–260. [PMC free article] [PubMed] [Google Scholar]
- 83.Bonn D. Maggot therapy: an alternative for wound infection. Lancet. 2000;356(9236):1174. doi: 10.1016/S0140-6736(05)72870-1. [DOI] [PubMed] [Google Scholar]
- 84.Mumcuoglu K.Y., et al. Maggot therapy for the treatment of intractable wounds. Int. J. Dermatol. 1999;38(8):623–627. doi: 10.1046/j.1365-4362.1999.00770.x. [DOI] [PubMed] [Google Scholar]
- 85.Sherman R.A. Maggot therapy for treating diabetic foot ulcers unresponsive to conventional therapy. Diabetes Care. 2003;26(2):446–451. doi: 10.2337/diacare.26.2.446. [DOI] [PubMed] [Google Scholar]
- 86.Dumville J.C., et al. VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers. Health Technol. Assess. 2009;13(55):1–182. doi: 10.3310/hta13550. [DOI] [PubMed] [Google Scholar]
- 87.Sherman R.A., Wyle F., Vulpe M. Maggot therapy for treating pressure ulcers in spinal cord injury patients. The Journal of Spinal Cord Medicine. 2016;18(2):71–74. doi: 10.1080/10790268.1995.11719382. [DOI] [PubMed] [Google Scholar]
- 88.Ahmadnejad M., Rafinejad J., Tolouei M. Use of fly larva (Maggots) in Cancer Treatment: a systematic review. J Surg Trauma. 2022;10(3):95–102. [Google Scholar]
- 89.Wang D., Wang R., Cai M., et al. Maggot extract inhibits cell migration and tumor growth by targeting HSP90AB1 in ovarian cancer. J. Clin. Med. 2022;11(21):6271. doi: 10.3390/jcm11216271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ahmadnejad M., Tolouei M., Jarolmasjed S.H., et al. Evaluation of maggot therapy effects on the progression of equine sarcoid. Iran. J. Vet. Med. 2022;16(1):15–25. [Google Scholar]
- 91.Gokulakrishnaa R., Thirunavukkarasu S. Apitherapy: a valuable gift from honey bee. J Entomol Zool Stud. 2020;8(5):2317–2323. [Google Scholar]
- 92.Abdel-Rahman M., Elebiary A.S., Hafez S.S., Mohammed H.E., Abdel Moneim A.E. Therapeutic activity of bee-stings therapy in rheumatoid arthritis causes inflammation and oxidative stress in female patients. Int. J. Res. Ayurveda Pharm. 2013;4(3):316–321. [Google Scholar]
- 93.Zhang F., et al. Clinical application of bee acupuncture in recent five years. Journal of Liaoning university of TCM. 2019;21(12):220–224. doi: 10.13194/j.issn.1673-842x.2019.12.058. (Article in Chinese) [DOI] [Google Scholar]
- 94.An X., Tian Y. Clinical observation of bee acupuncture in treating 86 cases of knee osteoarthritis. Apiculture of China. 2019;70(2):23–24. CNKI:SUN:ZGYF.0.2019-02-011. (Article in Chinese) [Google Scholar]
- 95.Pan H., Chen L. Clinical observation of bee needle stinging Dazhui Point in the treatment of radiculopathy of cervical spondylosis. Apiculture of China. 2015;66(2):49–50. CNKI:SUN:ZGYF.0.2015-02-030. (Article in Chinese) [Google Scholar]
- 96.Chen Y. Clinical observation of apitherapy in 28 cases of appendicitis. Apicultural Science and Technology. 2004;(6):33–34. CNKI:SUN:YFKJ.0.2004-06-022.(Article in Chinese) [Google Scholar]
- 97.Chen Y. Experience of apitherapy for cervical lymphatic tuberculosis. Journal of bee. 1997;(1):11–12. CNKI:SUN:MFZA.0.1997-01-006.(Article in Chinese) [Google Scholar]
- 98.Peng L., et al. Clinical observation on 30 cases of cancer pain treated by apitherapy. Journal of new Chinese medicine. 2014;46(12):177–178. CNKI:SUN:REND.0.2014-12-092.(Article in Chinese) [Google Scholar]
- 99.Fang Z. Apitherapy for peripheral vascular disease. Apicultural Science and Technology. 1993;(4):26–27. (Article in Chinese) [Google Scholar]
- 100.Dai Q. 120 cases of thromboangiitis obliterans treated by apitherapy. Apiculture of China. 2008;59(9) doi: 10.3969/j.issn.0412-4367.2008.09.028. 34-34. (Article in Chinese) [DOI] [Google Scholar]
- 101.Wang D. Bee venom therapy for breast hyperplasia. Journal of bee. 2019;39(2):42–43. CNKI:SUN:MFZA.0.2019-02-026. (Article in Chinese) [Google Scholar]
- 102.Zhou F., Zhou F. Clinical observation of apitherapy combined with millimeter acupuncture in treating 127 cases of mammary hyperplasia. Apiculture of China. 2005;56(2) doi: 10.3969/j.issn.0412-4367.2005.02.025. 28-28. (Article in Chinese) [DOI] [Google Scholar]
- 103.Xiong J., et al. Based on modern literatures to explore the evidence-based grade disease spectrum of apitherapy. Chin. J. Ethnomed. Ethnopharmacy. 2022;31(21):1–6. (Article in Chinese) [Google Scholar]
- 104.Hu Y., et al. Analysis of related factors of common adverse reactions of bee-venom acupuncture therapy. Journal of new Chinese medicine. 2021;53(19):185–189. doi: 10.13457/j.cnki.jncm.2021.19.042/. (Article in Chinese) [DOI] [Google Scholar]
- 105.Kwon Y.B., et al. The analgesic efficacy of bee venom acupuncture for knee osteoarthritis: a comparative study with needle acupuncture. Am. J. Chin. Med. 2001;29(2):187–199. doi: 10.1142/S0192415X01000228. [DOI] [PubMed] [Google Scholar]
- 106.Hwang J.H., Kim K.H. Bee venom acupuncture for circumscribed morphea in a patient with systemic sclerosis: a case report. Medicine (Baltim.) 2018;97(49) doi: 10.1097/MD.0000000000013404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhong X., et al. Application of Lingnan painless apitherapy in treating non-diseased patients. Henan traditional Chinese medicine. 2017;37(6):956–957. doi: 10.16367/j.issn.1003-5028.2017.06.0336. (Article in Chinese) [DOI] [Google Scholar]
- 108.Kligman A.M., Freeman B. History of baldness. From magic to medicine. Clin. Dermatol. 1988;6(4):83–88. doi: 10.1016/0738-081x(88)90070-3. [DOI] [PubMed] [Google Scholar]
- 109.Musa R. Folk remedies for alopecia. Clin. Dermatol. 2013;31(4):498–500. doi: 10.1016/j.clindermatol.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 110.Adisakwattana P., Nuamtanong S., Kusolsuk T., Chairoj M., Yenchitsomanas P.T., Chaisri U. Non-encapsulated Trichinella spp., T. papuae, diminishes severity of DSS-induced colitis in mice. Asian Pac. J. Allergy Immunol. 2013;31(2):106–114. doi: 10.12932/AP0238.31.2.2013. [DOI] [PubMed] [Google Scholar]
- 111.FDA. 510(k) Premarket Notifification. Medical Maggots. K033391. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=K033391.
- 112.King C. Changing attitudes toward maggot debridement therapy in wound treatment: a review and discussion. J. Wound Care. 2020;29(Sup2c):S28–S34. doi: 10.12968/jowc.2020.29.Sup2c.S28. [DOI] [PubMed] [Google Scholar]
- 113.Bazaliński D., et al. The use of Lucilia sericata larvae in the treatment of chronic wounds—a study of three cases. Leczenie Ran. 2018;15:105–111. [Google Scholar]
- 114.Soares M.O. Cost effectiveness analysis of larval therapy for leg ulcers. BMJ. 2009;19(338):b825. doi: 10.1136/bmj.b825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shih T., et al. Fish pedicure: review of its current dermatology applications. Cureus. 2020;12(6):e8936. doi: 10.7759/cureus.8936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.FDA. Beyond Bloodletting: FDA Gives Leeches a Medical Makeover. Available online: https://permanent.access.gpo.gov/lps1609/www.fda.gov/fdac/features/2004/504_leech.html. [PubMed]
- 117.Wirth K.E., Rein D.B. The economic costs and benefits of dog guides for the blind. Ophthalmic Epidemiol. 2008;15(2):92–98. doi: 10.1080/09286580801939353. [DOI] [PubMed] [Google Scholar]
- 118.F X. In the new historical starting point to promote the development of traditional Chinese medicine apitherapy. Journal of bee. 2008;28(4):35–36. doi: 10.3969/j.issn.1003-9139.2008.04.030. (Article in Chinese) [DOI] [Google Scholar]
- 119.Mellor D.J., et al. The 2020 five domains model: including human–animal interactions in assessments of animal welfare. Animals. 2020;10(10):1870. doi: 10.3390/ani10101870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mignot A., et al. Handlers' representations on therapy dogs' welfare. Animals (Basel) 2022;12(5):580. doi: 10.3390/ani12050580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wildgoose W.H. A review of fish welfare and public health concerns about the use of Garra rufa in foot spas. Fish Vet J. 2012;13:3–16. [Google Scholar]
- 122.Zhou B., Lao J. Clinical observation of bee venom acupuncture combined with moxibustion with warming needle in treating neurogenic tinnitus. Journal of Guangzhou University of Traditional Chinese Medicine. 2019;36(11):1749–1752. 10. 13359/j. cnki. gzxbtcm. 2019. 11. 015. (Article in Chinese) [Google Scholar]
- 123.Du G., et al. Polymeric microneedle-mediated transdermal delivery of melittin for rheumatoid arthritis treatment. J. Contr. Release. 2021;336:537–548. doi: 10.1016/j.jconrel.2021.07.005. [DOI] [PubMed] [Google Scholar]
- 124.Mercer N.S., et al. Medical leeches as sources of wound infection. Br. Med. J. 1987;294(6577):937. doi: 10.1136/bmj.294.6577.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lucht F., Aubert G., Seguin P., Tissot-Guerraz F., Relave M. Postoperative skin-flap decongestion, leeches and Aeromonas hydrophila. J. Hosp. Infect. 1988;11(1):92–93. doi: 10.1016/0195-6701(88)90046-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.