Abstract
Maxillary skeletal expansion is considered a challenging treatment modality in adult ages. Mini-screw-assisted rapid palatal expansion (MARPE) is considered a pioneer in providing a solution for maxillary deficiency in adults away from any surgical interventions. If we consider patient cooperation and motivation, together with operator skills, as constant factors during MARPE, and exclude all hygiene and soft tissue complications that jeopardise the appliance's stability, there is a percentage of expansion failure recorded in different studies with no emphasis on what makes mid-facial diastema appear in some, rather than others. Electronic databases including PubMed, Scopus, Google Scholar, and Web of Science, were searched for literature published in English till 2023. Failure was related in some literature to different criteria, as of yet, no verifiable indicators would allow us to determine success or failure in advance. This review highlighted the most common reasons for failure discussed in different literature: Chronological Age, Mid-palatal suture maturation, Bone density, Sex, Race, Appliance design, and Expansion technique used. This study could be considered an attempt to make candidate selection for non-surgical maxillary skeletal expansion at this old age easier, time-saving, and cost less.
Keywords: Adult Orthodontics, Maxillary Expansion, Mini-implants, Skeletal Deficiency
1. Introduction
One of the most prevalent orthodontic problems is maxillary transverse deficiency, which can occasionally be associated with a unilateral cross-bite, or even a bilateral one. The most effective line of treatment for skeletally increasing the maxilla is thought to be rapid maxillary expansion (RME) (Kurol, and Berglund, 1992). Recent years have seen the development of several maxillary expansion appliances aimed at reducing the detrimental consequences of tooth-borne maxillary expansion. The force is divided by these appliances between the 2–4 mini-implants and the anchoring teeth. Wilmes (Wilmes et al., 2010), in 2007, introduced the hybrid hyrax expander using two mini-screws in the front palate and two (deciduous) molars (Fig. 1) (Wilmes, 2007, Wilmes and Drescher, 2008, Wilmes, 2008). The name “mini-screw assisted rapid palatal expansion” (MARPE) was used to designate similar hybrid expanders reported in the years that followed by Garib (Garib et al., 2008), Lee (Lee et al., 2010) and Moon (Moon et al., 2015).
Fig. 1.

The first MARPE The hybrid hyrax expander ().
Adopted from Wilmes et al., 2010
Numerous studies have shown that MARPE is preferable to tooth-borne expanders as it is associated with less anchorage tooth tipping, increased skeletal expansion, less loss of buccal bone thickness, increased nasal airway flow, and less anchorage tooth root resorption (Lin et al., 2015, Gunyuz et al., 2015, Celenk-Koca et al., 2018, Bazargani et al., 2018, Yildirim and Akin, 2019). Although skeletal borne expanders have the drawback of requiring local anaesthesia and mini-implants to be placed. However, the degree of discomfort and pain experienced during RPE therapy with a traditional Hyrax expander and a mini-screw anchored equipment did not appear to differ (Feldmann,and Bazargani, 2017).
Some clinicians preferred to use two mini-implants in the front palate (T-Zone) claiming that it is the optimal insertion site. They asserted that the area called “T-Zone” in the front palate offers the best cortical bone width and the safest insertion location for the mini-screws far from blood vessels and tooth roots. They demonstrated the effectiveness of that pure bone-born expander design in producing successful skeletal expansion (Wilmes et al., 2021).
Others used mini-implants assisted rapid palatal expansion (MARPE), which also achieved skeletal expansion at this crucial age, in which four mini-implants were inserted into the expansion screw body parallel to the mid-palatal suture and banded to two anchored teeth (Choi et al., 2016) or one anchored tooth from each side, a design of a bone-tooth-born expander (Brunetto et al., 2017, Cantarella et al., 2017).
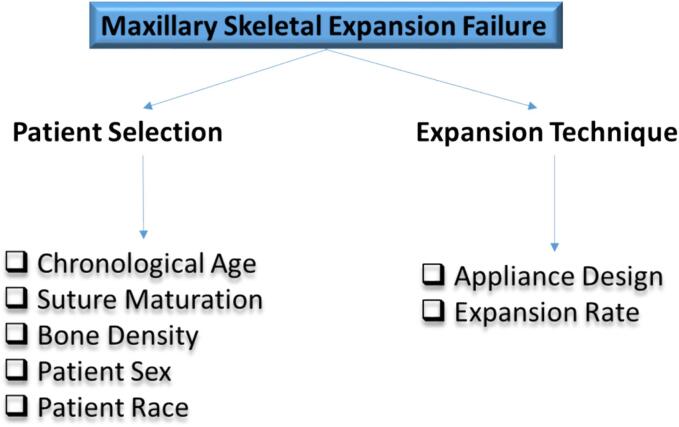
Despite the high success rate of skeletal expansion in adult ages in several studies, there is still a failure percentage that was presented in some literature. In Choi (Choi et al., 2016) and Park's studies (Park et al., 2017), among the patients treated by MARPE, a percentage exhibited failure of the mid-palatal suture opening and were excluded from the studies. It is still unclear why some MARPE cases fail. Authors claimed failure due to different causes, but until now, no study has used clinical intervention to attribute failure to evidence-based reasons. This study will highlight the most discussed expansion failure explanations in literature in an attempt to identify which of them play the major role in mid-facial expansion failure in adults (Fig. 2).
Fig. 2.
The study Flow Chart A flow chart of the factors discussed as a reason for expansion failure.
2. Search strategy
Electronic databases including PubMed, Scopus, EPSCO Host, Cochran Library, Web of Science, and Google Scholar were searched for literature. The inclusion criteria were as follows: Studies using dried human skulls or human samples of young people or late adults who are not undergoing any other treatments that could affect the mid-facial skeletal expansion therapy have been reported in English till 2023. Studies using samples from animals were not included. 58 articles were studied and analyzed by the three authors to determine the percentage of success and failure with MARPE expansion and the reasons for failure. The expansion failure reasons were ignored in most of the studies that focus on their objectives. The authors had to extract the reasons after studying the sample used and the methodology of those studies.
3. Chronological age, suture maturation, or bone density?
3.1. Chronological Age
In general, expanding the palate skeletally through the aperture of the palatal suture is more difficult when the patient gets older. This fact was discussed by Liu et al. when they analyzed skeletal expansion in their systematic review of patients ranging in age from five to twenty years (Liu et al., 2015).
The theoretical explanation of skeletal expansion in adults according to previous findings, shows that the chronological age does not correlate with the real bony obliteration of the mid-palatal suture in radiographs (Persson, and Thilander, 1977). Boryor in their article reported substantially identical histological results in Individuals aged between 10 and 30 years (Boryor et al., 2013). According to Lin's comparative study (Lin et al., 2015), bone-anchored RME produced more orthopaedic effects and fewer dentoalveolar side effects than conventional RME in patients with a mean age of 22 years, however, skeletal transverse expansion was achieved in both groups. Despite being much less in the tooth-born RME group, it was still obtained (Lin et al., 2015).
3.2. Mid-Palatal suture Maturation
Despite radiographs appearing to show complete suture ossification, a histological study (Boryor et al., 2013) found that in humans older than 70 years, only the anterior third of the suture had ossification. A low force (80 to 90 N) was required to open the fused sutures in the 73-year-old female specimen, which demonstrated the possibility of opening the inter-maxillary suture with a very low transverse force. This force similarly corresponds to that of youths with non-fused sutures during RME. In those samples, the posterior areas still had connective tissue. These investigations corroborated the idea that the constant mechanical stress placed on the mid-palatal suture renders it the sole cranial suture incapable of achieving complete ossification. (Brunetto et al., 2017).
To determine age-related morphological changes concerning the degree of obliteration (O) and mean sutural width (MSW) in the region of the mid-palatal suture, Knoup (Knoup et al., 2004) conducted his investigation on 22 human palate specimens belonging to various age groups (18–63 years). There were created two age categories (under 25 and over 26 years old). The results revealed that the younger group (those under 25 years old) had a considerably wider median sutural width than the older group. All subjects had a small percentage of ossified tissue (obliteration) over the whole suture. Ossification rates ranged from 0 % in the younger age group to roughly 3 % over 26 years. A man aged 21 had the earliest ossification ever observed. A 54-year-old man was the oldest individual who did not have ossification. These results led them to demonstrate that the higher resistance in the transverse direction experienced during RPE in younger participants (less than 25 years old) as well as in numerous elderly individuals is not a credible cause.
An alternative classification system for the assessment of each individual's mid-palatal suture morphology was presented by Angelieri (Angelieri et al., 2013). To identify the radiographic stages of mid-palatal suture maturation, 140 patients (ages, 5.6–58.4 years) underwent scans by CBCT “Cone Beam Computed Tomography”. The mid-palatal suture maturation was reported and defined in five stages: Stage A: a straight, high-density sutural line with little to no inter-digitation; Stage B: a high-density sutural line that appears scalloped; Stage C: two parallel, scalloped, high-density lines that are close to one another and are occasionally separated by small low-density spaces; stage D: palatine bone fusion that has been completed with no sign of a suture; stage E: anterior maxilla fusion. Stages A and B were generally seen in children up to the age of 13, whereas stage C was occasionally seen in younger and older age groups, it was most prevalent between 11 to 17 years. Only in girls did the mid-palatal suture fusion of the palatine (stage D) and maxillary (stage E) regions take place after 11 years. 3 of 13 (23 %) of boys between the ages of 14 and 17 only had fusion in the palatine bone (stage D). Late adolescents and young adults, believed that this new classification technique could help prevent the negative impacts of RME failure or unnecessary surgically assisted RME (Angelieri et al., 2013).
CBCT images of the mid-palatal suture were analyzed in Angelieri’s study (Angelieri et al., 2016). The five maturational phases of the mid-palatal were seen as follows: A straight, dense sutural line with little to no inter-digitation is an indicator of stage A. The high-density sutural line has a scalloped look in Stage B. Two parallel, scalloped, high-density lines that are near to one another and sometimes separated by tiny low-density areas define Stage C. Stage D is distinguished by palatine bone fusion without any indication of a suture. They reasoned that because Stage C's suture had numerous bone bridges, less skeletal reactivity than at Stages A and B would be expected. Individuals in Stages D and E would need surgically assisted RME since the mid-palatal suture has already fused, either entirely or partly. To assess the prognosis of the RME, they advised adopting this diagnostic method, particularly for late adolescents and young adults for whom this process is unpredictable clinically (Angelieri et al., 2016).
3.3. Bone Density
Angelieri (Angelieri et al., 2016), Abo Samra (Abo Samra and Hadad, 2018) conducted a study quite similar to theirs to examine the connection between the mid-palatal suture's bone densities and various stages of morphological maturity. They found that; in the maxillary area in stages D and E as well as the palatal region in stage E, there was a considerable increase in the bone density of the mid-palatal suture. It was shown that the variation in bone density of the mid-palatal suture between the morphological developmental stages was the main factor sustaining their reliability in a clinical application (Abo Samra and Hadad, 2018).
As mentioned in some studies, each individual’s ossification of the mid-palatal suture should be evaluated by CBCT before therapy to evaluate the efficacy of non-surgical skeletal expansion (Winsauer et al., 2021). In their investigation (Winsauer et al., 2021), they noted that the age varied significantly across the stages of mid-palatal suture development and was significantly linked with the mid-palatal suture opening ratio. Similar to this, they reported a substantial correlation between age and both expansion failure and complications in their study. They rendered the reason for the inter-digitation of the mid-palatal and circum-maxillary sutures that might begin to increase in late youth and become increasingly inflexible as ageing occurs, particularly around the age of thirty. (Winsauer et al., 2021).
Concerning the split of the pterygopalatine suture, on both the left and right sides (Colak et al., 2020), 84 sutures out of 100 (or 84 %) showed gaps between the medial and lateral pterygoid plates. Among the eight patients, there was a significant partial split (5 females and 3 men). Three patients only exhibited disarticulation on their right side, whereas five other patients had medial pterygoid plate splits on both pterygo-maxillary sutures. In the axial perspective, the MSE appliance performed almost parallel expansion. Surprisingly, this study demonstrates that pterygopalatine suture can split by MSE appliance without the need for surgical intervention because most patients' pterygopalatine suture disarticulation was noticeable. (Colak et al., 2020).
Maxillofacial surgeons had different opinions according to Chhatwani's study (Chhatwani et al., 2021) when considering surgical assistance as mandatory during maxillary expansion. Regarding age, gender, and the technique required for that goal, opinions diverge. After turning 16 years old, Epker and Frost (Epker, and Frost, 1965) recommended SARME “a surgically assisted rapid maxillary expansion”. Conversely, Timms and Vero assert that a standard SARME should not be performed over the age of 25 years (Timms, and Vero, 1981). However, maxillary expansion following SARME is frequently asymmetrical, according to the postoperative examination of the maxilla or biomechanical anatomic models. More than 50 % of the sample group examined by Elkenawy et al. exhibit asymmetric expansions (Elkenawy et al., 2020). Additionally, these asymmetries may also be in an oblique direction which might necessitate a second corrective operation (Elkenawy et al., 2020).
Even after relieving the mid-palatal suture and the surrounding resistance, the reason for the asymmetric expansion remains unclear. Besides other factors, differential bone densities at the sutures and the structures surrounding provided a significant explanation for these asymmetries (Elkenawy et al., 2020). According to Winsauer (Winsauer et al., 2021), a 43-year-old patient who was not included in their analysis had an asymmetrical expansion of the naso-maxillary complex and a dislocated nasal bone. According to them, different bone densities on either side of the suture or an asymmetric screw position in the maxilla were suggested as potential causes of this problem.
4. Does the patient sex or race play a role in expansion failure?
4.1. Males or Females?
According to Yuan's study (Yuan et al., 2021), if bone density is one of the primary factors resisting maxillary expansion in adults, they demonstrated a relationship between depression and bone density in adult males and females. There are several reasons why bone density may be decreased in adults and adolescents exhibiting depressive symptoms. Higher amounts of cortisol are seen in depressed individuals compared to healthy individuals, and cortisol may act as a mediator in the loss of bone mineral density (BMD) in adult depressive women. Depressed patients often lead depressing lifestyles and poor dietary habits, which are important for preserving bone mass. Significantly, obesity harms bones and has been connected to depression in adults and adolescents. According to a Yuan et al. meta-analysis published in 2021 (Yuan et al., 2021), gender has a significant impact on the evaluation of a relationship between depression and BMD. In a gender-stratified analysis, the male group did not experience a significant decline in BMD. There could be many other contributing factors behind this disparity between men and women. According to Yuan’s study, women experience depression at a rate of 2:1 more frequently than males, especially after menopause. Also hormonal factors such as; Estrogen levels, for example, may have an impact on how depression and BMD are related in both men and women (Cauley et al., 2005).
A retrospective study (Yoon et al., 2022) conducted on 265 adult patients (126 females and 130 males) revealed a suture separation success in 87.8 % of the sample. The males exhibited 61.1 % success rate, while the females showed 94.2 % success. However, the investigators did not explain the effect of sex on failure and success rates in this study. They focused on their objective which was identifying complications associated with MARPE in this adult age.
4.2. Patient’s Race
Cauley et al., 2005 investigated the relationship between the incidence of non-spinal fractures and BMD in older Black and White women to figure out if BMD predicts fracture risk in White women as well as it does in Black women. They found that Black women experience fractures at a lesser incidence than White women. The major outcome measures revealed that White women have softer bones and an increased fracture risk than Black women at every level of BMD (Cauley et al., 2005).
5. The appliance design and technique used
5.1. Appliance Position
The expander's body should be positioned as posteriorly as feasible at the junction of the hard and soft palate, according to research by Brunetto (Brunetto et al., 2017), as these sutures provide the greatest resistance to expansion (Fig. 3, Fig. 4).
Fig. 3.
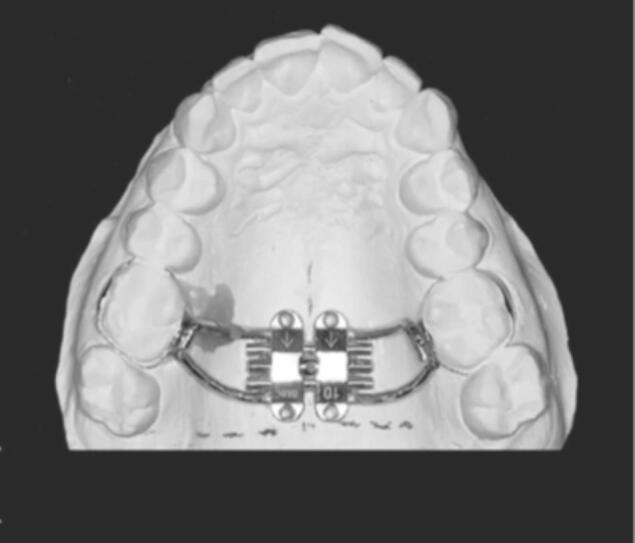
Appliance posterior position The body of the expander was designed as posteriorly as possible, close to the junction of the hard and soft palate. ().
Adopted from Brunetto et al., 2017
Fig. 4.
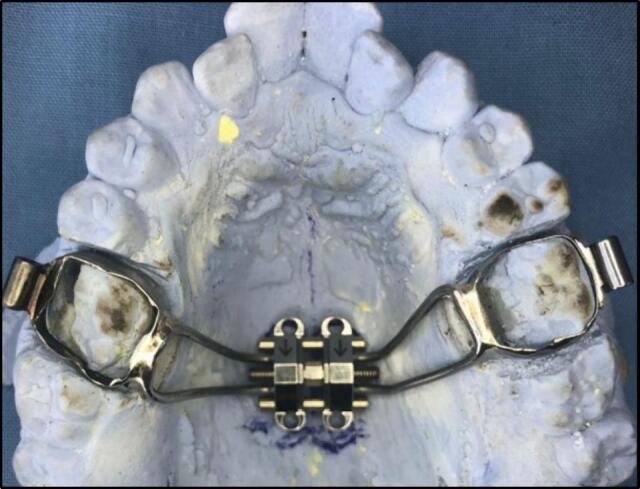
Appliance laboratory construction posteriorly.
To overcome early resistance and encourage the parallel opening of the mid-palatal suture, forces should be applied posteriorly according to Brunetto’s study. Cantarella supported this position (Cantarella et al., 2018) to improve the transfer of the device expansion force to the supporting bone structures, and four mini-implants with bi-cortical engagement were used. According to what they said, this resulted in an expansion force vector parallel to the zygomatic buttress bone. Their results also showed that significant bone bending occurred during the widening of the temporal bone's zygomatic process. This was consistent with their study's findings that all treated individuals had a split mid-palatal suture. Compared to other locations, the front palate is claimed to have a substantially reduced mini-implant failure rate of 1 %–5%. According to Wilmes (Wilmes et al., 2021). the better bone quantity and quality, along with the thinly connected mucosa and the low risk of tooth-root injuries, were assigned to the anterior palate as the cause. Additionally, they concluded that the zone immediately posterior to the palatal rugae is the optimum one with the lowest failure rates (Wilmes et al., 2021) (Fig. 5).
Fig. 5.

Appliance anterior position The body of the expander was placed immediately posterior to the palatal rugae at the anterior palate. ().
Adopted from Wilmes et al., 2021
5.2. Activation Rate
With a device expanding by 0.2 mm each quarter turn, Brunetto (Brunetto et al., 2017) produced a chart outlining possible activation rates according to age. In several investigations, including their own, the most common expansion rate was two turns each day (0.4 mm per day). Zong (Zong et al., 2019) and Oh-Heeso (Oh et al., 2019), applying different screw widths that needed four activations each day, applied the same amount of expansion. Hourfar (Hourfar et al., 2016) employed a three-turn, 0.6 mm-per-day in a rapid expansion protocol. Those studies didn't report any failure percentage, either due to the younger ages of their samples, or the objectives of the studies that focused on comparing MARPE with RPE using the regular Hyrax expander. On the other hand, a slow expansion every other day (one rotation of 0.2 mm) was utilized in studies by Lagravere (Lagravere et al., 2010) and Choi (Choi et al., 2016) to lessen tissue damage, inflammation, and pain/discomfort, though Choi et al., got 13.04 % failure. Cantarella (Cantarella et al., 2017) and Colak O (Colak et al., 2020) used 0.5 mm expansion /day till diastema appeared and then decreased the turns to 0.25 mm /day. They also didn't report the failure of expansion in their study. Wilmes (Wilmes we al., 2021) used a slower rate of expansion in an almost near-age sample and found that the failure percent was 1 %-5% which they claimed to be significantly lower than in other studies. They attributed their increased success rate to the appliance's placement in the anterior palate, not to the rate of expansion (Table 1).
Table 1.
The following table might summarize some effects of appliance designs, and activation protocols on expansion failure percentage.
| The study | Appliance position | Number and position of mini-implants | Activation protocol | Failure percentage |
|---|---|---|---|---|
| Choi et al., 2016 | Middle Palate | 4 along the mid-palatal suture, 2 anteriors in the rougeh area, and 2 posteriors between the 2nd premolar and 1st molar area | 0.5 mm/2d Slow expansion |
|
| Cantarella et al., 2018 | ||||
| Posterior palate | 4 parallel to mid-palatal suture | 0.5 mm/d Rapid expansion |
0 % | |
| Colak et al., 2020 | ||||
| Wilmes et al., 2021 | Anterior Palate | 2 parallel to mid-palatal suture | 0.2 mm/d Slow expansion |
1 %- 5 % |
| Winsauer et al., 2021 | Anterior palate | 4 between the roots of 1st − 2nd premolars anteriorly, and 2nd premolar −1st molar posteriorly. | Force-controlled polycyclic expansion protocol (FCPC) | |
| 0.5–1 mm/ d | ||||
| Brunetto et al., 2022 | Posterior palate | 4 parallel to mid-palatal suture | Rapid expansion | 15 % |
mm = millimetres d = day.
As they did nott use a rapid expansion procedure, Winsauer (Winsauer et al., 2021) investigated the failure and success rate of MAPE (not MARPE) with a unique FCPC “Force-Controlled Polycyclic Expansion Protocol” following the placement of the four mini-screws and the 12-week osseointegration latency period, the expander was installed, and the FCPC procedure was used. The new protocol of expansion, which involves the appliance opening and closing (alternate expansion and constriction, simulates oscillatory tensile and compressive strains. Winsour (Winsauer et al., 2021) adopted the hypothesis that clinical implications for a cyclic loading regimen would include new mechanical stimuli to modulate the craniofacial development of patients with dentofacial deformities and craniofacial anomalies. The circum-maxillary sutures appear to weaken as a result of the impact that was used in their investigation, permitting effective expansion even in elderly patients (Winsauer et al., 2021). In their study, 16.6 % of the samples failed to expand, and complications were seen in 18.5 % of the successful samples. The age range of the sample used for this study was 18 to 58 years. They put the failure rate and complications attributable to age, which also markedly raised the odds of complications (Winsauer et al., 2021).
Their study included important variations that might account for the high rate of success in older patients, including the rigidity of the appliance, the insertion area of the mini-screws in the anterior palate, which was preferred for the fixation of their device, and the unique 2-stage procedure. As they stated, age-related changes to the suture may require more expanding force, thus they produced the MICRO-4 appliance, a revolutionary device that, owing to its rigidity, can efficiently transmit the expansion force to the hard palate. Although it could be the reason for their study's anterior V-shaped expansion pattern, the mini-implant's more secure anchoring in the anterior palate may also account for their high success rate (Winsauer et al., 2021). This is why Brunetto, in their most recent study in 2022 (Brunetto et al., 2022), chose their favourable posterior site when assessing MARPE impacts on adult non-obese individuals with transverse maxillary deficiencies who have obstructive sleep apnea in terms of their sleep and quality of life. Though they experienced 15 % failure, they defended the hypothesis that a parallel sutural expansion and further impacts on the Oro- and Nasopharynx's measurement and airflow resistance are anticipated if the posterior portions of the maxilla expand more.
6. Conclusions
The true bony obliteration of the mid-palatal suture in radiographs does not correlate with chronological age. Differential bone density seems to be the parameter limiting conservative MARPE. The adult age group with the highest bone density was the middle age group [from 25 to ≤ 30]. Adults with depressed symptoms have lower bone density. Women were more prone to depression than men with a ratio of 2:1, a concept that correlates sex and bone density with the rate of expansion success and failure. White women have a softer bone and increased fracture risk than Black women. The appliance position, number of mini-screws or rate of expansion was not correlated to the expansion success or failure percentage in different studies.
Ethics Approval
This article did not require IRB approval because it’s a review of the literature article.
The figures adopted from other articles were all cited and referred to in the figure captions.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
Grant supported from External Agencies KPS Dental Care Team Sdn Bhd (RT 304 PPSG.6150250.K161).
Contributor Information
Amira Allam, Email: amira.hussein@ksiu.edu.eg.
Basaruddin Ahmed, Email: basaruddin@usm.my.
Norma Ab Rahman, Email: drnorma@usm.my.
References
- Abo Samra D., Hadad R. Midpalatal suture: evaluation of the morphological maturation stages via bone density. Prog. Orthod. 2018;19(1):29. doi: 10.1186/s40510-018-0232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelieri F., Cevidanes L.H., Franchi L., Gonçalves J.R., Benavides E., McNamara J.A. Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am. J. Orthod. Dentofacial Orthop. 2013;144:759–769. doi: 10.1016/j.ajodo.2013.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelieri F., Franchi L., Cevidanes L., Bueno-Silva B. The midpalatal suture on cone beam CT. Dental Press J. Orthod. 2016;21(6):115–125. doi: 10.1590/2177-6709.21.6.115-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazargani F., Magnuson A., Ludwig B. Effects on nasal airflow and resistance using two different RME appliances: a randomized controlled trial. Eur. J. Orthod. 2018;40:281–284. doi: 10.1093/ejo/cjx081. [DOI] [PubMed] [Google Scholar]
- Boryor A., Hum B., Hohmann A., Wunderlich A., Nat R., Geiger M., et al. Use of a Modified Expander During Rapid Maxillary Expansion in Adults: An in Vitro and Finite Element Study. Int. J. Oral Maxillofac Implants. 2013;28:11–16. doi: 10.11607/jomi.2078. [DOI] [PubMed] [Google Scholar]
- Brunetto DP, Sant’Anna EF, Machado AW, Moon W. Non-surgical treatment of transverse deficiency in adults using Microimplant-assisted Rapid Palatal Expansion (MARPE). Dent. Press J. Orthod. 2017;22:110-25. DOI: 10.1590/2177-6709.22.1.110-125. [DOI] [PMC free article] [PubMed]
- Brunetto D.P., Moschik C.E., Dominguez-Mompell R., Jaria E., Sant’Anna E.F., Moon W. Mini-implant assisted rapid palatal expansion (MARPE) effects on adult obstructive sleep apnea (OSA) and quality of life: a multi-center prospective controlled trial. Prog. Orthod. 2022:23:3. doi: 10.1186/s40510-021-00397-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantarella D., Dominguez-Mompell R., Mallya S.M., Moschik C., Pan H.C., Miller J., et al. Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander were analyzed with a novel 3D method based on CBCT imaging. Prog. Orthod. 2017;18(1):34. doi: 10.1186/s40510-017-0188-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauley J., Lui L.Y., Ensrud K.E., Zmuda J.M., Hochberg M.C., Cummings S.R. Bone Mineral Density and the Risk of Incident Nonspinal Fractures in Black and White Women. J. Am. Med. Assoc. (JAMA) 2005;293:2102–2218. doi: 10.1001/jama.293.17.2102. [DOI] [PubMed] [Google Scholar]
- Celenk-Koca T., Erdinc A.E., Hazar S., Harris L., English J.D., Akyalcin S. Evaluation of miniscrew-supported rapid maxillary expansion in adolescents: a prospective randomized clinical trial. Angle Orthod. 2018;88:702–709. doi: 10.2319/011518-42.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhatwani S., Schudlich K., Möhlhenrich S.C., Pugachev A., Bicsak A., Ludwig B., Hassfeld S., Danesh G., Bonitz L. Evaluation of symmetry behaviour of surgically assisted rapid maxillary expansion with simulation-driven targeted bone weakening. Clin. Oral Invest. 2021 doi: 10.1007/s00784-021-03958-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S.H., Shi K.K., Cha J.Y., Park Y.C., Lee K.J. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016;86:713–720. doi: 10.2319/101415-689.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colak O., Paredes N., Elkenawy I., Torres M., Bui J., Jahangiri S., Moon W. Tomographic assessment of palatal suture opening pattern and pterygopalatine suture disarticulation in the axial plane after midfacial skeletal expansion. Prog. Orthod. 2020;21:21. doi: 10.1186/s40510-020-00321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkenawy I., Fijany L., Colak O., Paredes N.A., Gargoum A., Abedini S., Cantarella D., Dominguez-Mompell R., Sfogliano L., Moon W. An assessment of the magnitude, parallelism, and asymmetry of micro-implant-assisted rapid maxillary expansion in nongrowing patients. Prog. Orthod. 2020;21(1):42. doi: 10.1186/s40510-020-00342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epker B.N., Frost H.M. The direction of transverse drift of actively forming osteons in the human rib cortex. J. Bone Joint Surg. Am. 1965;47:1211–1215. PMID: 14337779. [PubMed] [Google Scholar]
- Feldmann I., Bazargani F. Pain and discomfort during the first week of rapid maxillary expansion (RME) using two different RME appliances: a randomized controlled trial. Angle Orthod. 2017;87:391–396. doi: 10.2319/091216-686.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garib D.G., Navarro R., Francischone C.E., Oltramari P.V. Rapid maxillary expansion using palatal implants. J. Clin. Orthod. 2008;42:665–671. PMID: 19075382. [PubMed] [Google Scholar]
- Gunyuz T.M., Germec-Cakan D., Tozlu M. Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone borne expansion appliances. Am J Orthod Dentofacial Orthop. 2015;148:97–109. doi: 10.1016/j.ajodo.2015.02.022. [DOI] [PubMed] [Google Scholar]
- Hourfar J., Kinzinger G.S.M., Ludwig B., Spindler J., Lisson J.A. Differential treatment effects of two anchorage systems for rapid maxillary expansion: a retrospective cephalometric study. J. Orofac. Orthop. 2016;77(5):314–324. doi: 10.1007/s00056-016-0037-1. [DOI] [PubMed] [Google Scholar]
- Kurol J., Berglund L. Longitudinal study and cost-benefit analysis of the effect of early treatment of posterior cross-bites in the primary dentition. Eur. J. Orthod. 1992;14:173–179. doi: 10.1093/ejo/14.3.173. [DOI] [PubMed] [Google Scholar]
- Lee K.J., Park Y.C., Park J.Y., Hwang W.S. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am. J. Orthod. Dentofacial Orthop. 2010;137:830–839. doi: 10.1016/j.ajodo.2007.10.065. [DOI] [PubMed] [Google Scholar]
- Lin L., Ahn H.W., Kim S.J., Moon S.C., Kim S.H., Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253–262. doi: 10.2319/030514-156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S.Y., Xu T.M., Zou W. Effects of rapid maxillary expansion on the mid-palatal suture: a systematic review. Euro. J. Orthod. 2015;37:6. doi: 10.1093/ejo/cju100. [DOI] [PubMed] [Google Scholar]
- Moon W., Wu K.W., MacGinnis M., Sung J., Chu H., Youssef G., et al. The efficacy of maxillary protraction protocols with the microimplant- assisted rapid palatal expander (MARPE) and the novel N2 mini-implant-a finite element study. Prog. Orthod. 2015;16:16. doi: 10.1186/s40510-015-0083-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh H., Park J., Lagravere M.O. Comparison of traditional RPE with two types of micro-implant assisted RPE: CBCT study. Semin. Orthod. 2019;25(1):60–66. doi: 10.1053/j.sodo.2019.02.007. [DOI] [Google Scholar]
- Park J.J., Park Y.C., Lee K.J., Cha J.Y., Tahk J.H., Choi Y.J. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. Korean J. Orthod. 2017;47(2):77–86. doi: 10.4041/kjod.2017.47.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson M., Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am. J. Orthod. 1977;72:42–52. doi: 10.1016/0002-9416(77)90123-3. [DOI] [PubMed] [Google Scholar]
- Timms D.J., Vero D. The relationship of rapid maxillary expansion to surgery with special reference to mid palatal synostosis. Br. J. Oral Surg. 1981;19(3):180–196. doi: 10.1016/0007-117x(81)90003-2. [DOI] [PubMed] [Google Scholar]
- Wilmes B. In: Innovative Anchorage Concepts. Mini-Implants in Orthodontics. Ludwig B., Baumgaertel S., Bowman J., editors. Quintessenz; Berlin: 2007. Fields of application of mini-implants; pp. 89–120. [Google Scholar]
- Wilmes B. In: Innovative Anchorage Concepts. Mini-Implants in Orthodontics. Ludwig B., Baumgaertel S., Bowman J., editors. Quintessenz; Berlin: 2008. Fields of application of mini-implants; pp. 91–122. [Google Scholar]
- Wilmes B., Drescher D. A miniscrew system with interchangeable abutments. J. Clin. Orthod. 2008;42:574–580. PMID: 19075372. [PubMed] [Google Scholar]
- Wilmes B., Nienkemper M., Drescher D. Application and effectiveness of a mini-implant- and tooth-borne rapid palatal expansion device: the hybrid hyrax. World J. Orthod. 2010;11:323–330. PMID: 24018639. [PubMed] [Google Scholar]
- Wilmes B., Tarraf N., Drescher D. Treatment of maxillary transversal deficiency by using a mini-implant-borne rapid maxillary expander and aligners in combination. Am. J. Orthod. Dentofacial Orthop. 2021;160:147–154. doi: 10.1016/j.ajodo.2020.11.037. [DOI] [PubMed] [Google Scholar]
- Winsauer H., Walter A., Katsaros C., et al. Success and complication rate of miniscrew assisted non-surgical palatal expansion in adults - a consecutive study using a novel force-controlled polycyclic activation protocol. Head Face Med. 2021;17:50. doi: 10.1186/s13005-021-00301-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildirim M., Akin M. Comparison of root resorption after boneborne and tooth-borne rapid maxillary expansion evaluated with the use of microtomography. Am. J. Orthod. Dentofacial Orthop. 2019;155:182–190. doi: 10.1016/j.ajodo.2018.03.021. [DOI] [PubMed] [Google Scholar]
- Yoon A., Payne J., Suh H., Phi L., Chan A., Oh H. A retrospective analysis of the complications associated with mini screw-assisted rapid palatal expansion. Am. J. Orthod. Dentofacial Orthop. 2022;2(5):423–430. doi: 10.1016/j.xaor.2022.08.001. [DOI] [Google Scholar]
- Yuan S., Chen J., Zeng L., Zhou C., Yu S., Fang L. Association of bone mineral density and depression in different bone sites and ages: a meta-analysis. Food Sci. Nutr. 2021;9:4780–4792. doi: 10.1002/fsn3.2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zong C., Tang B., Hua F., He H., Ngan P. Skeletal and dentoalveolar changes in the transverse dimension using microimplant-assisted rapid palatal expansion (MARPE) appliances. Seminars Orthod. 2019;25(1):46–59. doi: 10.1053/j.sodo.2019.02.006. [DOI] [Google Scholar]