Abstract
Idiopathic pleuroparenchymal fibroelastosis (iPPFE) is a rare form of idiopathic interstitial pneumonia. We report a case of a patient with iPPFE in whom postural changes improved diaphragmatic excursion (DE) and exercise tolerance. Chest radiography showed a greater elevation of the diaphragm at maximum expiration in the supine position than the standing position. DE measured by ultrasonography was higher in the supine position than the standing position. The findings may suggest greater diaphragm movement in the supine position, leading to successful rehabilitation and improved exercise endurance. There is no effective treatment for iPPFE; therefore, an innovative treatment strategy is warranted.
Keywords: Pulmonary rehabilitation, Respiratory muscles, Ultrasonography, X-ray, Interstitial lung disease
1. Introduction
Pleuroparenchymal fibroelastosis (PPFE) is an interstitial lung disease characterized by dense subpleural consolidation with traction bronchiectasis, architectural distortion, and upper lobe volume loss. Idiopathic PPFE (iPPFE) was included as a rare form of idiopathic interstitial pneumonia in the official American Thoracic Society/European Respiratory Society 2013 classification, and patients with this condition often complain of severe exertional dyspnea [1]. Here, we report case of a patient with iPPFE in whom postural changes improved diaphragmatic excursion (DE) and exercise tolerance.
2. Case report/case presentation
A 64-year-old woman with severe dyspnea was diagnosed with iPPFE based on the findings of bilateral upper lobe volume loss and hilar elevation with emaciation (height, 165 cm; body weight, 34.3 kg; body mass index, 12.6 kg/m2) [2]. A pulmonary function test revealed restrictive ventilatory impairment and increased residual volume (RV) (forced vital capacity [FVC], 0.71 L [%FVC, 26.0%]; forced expiratory volume in 1 second [FEV1]/FVC, 100%; total lung capacity [TLC], 3.17 L [%TLC, 74.4%]; and RV, 2.44 L [%RV, 190.6%]). Arterial blood gas analysis showed hypoxemia and hypercapnia (PaO2, 69.9 Torr and PaCO2, 57.9 Torr in room air). Pulmonary rehabilitation was initiated for the severe dyspnea, which occurred even when the patient was just sitting and talking. Of note, her dyspnea was relieved in the supine position. Therefore, she could perform lower limb exercise effectively using an ergometer in the supine position. A constant-load exercise test (75% of the peak) was performed in the seated and supine positions. The endurance time was longer, tidal volume (VT) was higher, and respiratory rate and difference between the inspiratory and expiratory tidal volumes (VTi–VTe) were lower in the supine position than in the seated position (Table 1).
Table 1.
Results of constant exercise testing in different postures.
| Variable | Supine posture | Sitting posture |
|---|---|---|
| Endurance time | 29:27 | 3:33 |
| mBorg scale, dyspnea | 5 | 8 |
| mBorg scale, leg fatigue | 5 | 5 |
| SpO2, % | 96 | 96 |
| HR, bpm | 90 | 115 |
| Peak exercise measurements | ||
| VE, L | 17.1 | 24.7 |
| VT, mL | 533 | 459 |
| RR, times/min | 35.3 | 53.7 |
| Ti/Ttot, % | 0.60 | 0.55 |
| VTi–VTe, mL | 11 | 34 |
HR = heart rate, mBorg = modified Borg, SpO2 = percutaneous oxygen saturation, Ti/Ttot = inspiratory duty cycle, RR = respiratory rate, VE = minute ventilation, VT = tidal volume, VTi–VTe = difference between inspiratory and expiratory tidal volumes, bpm = beats per minute.
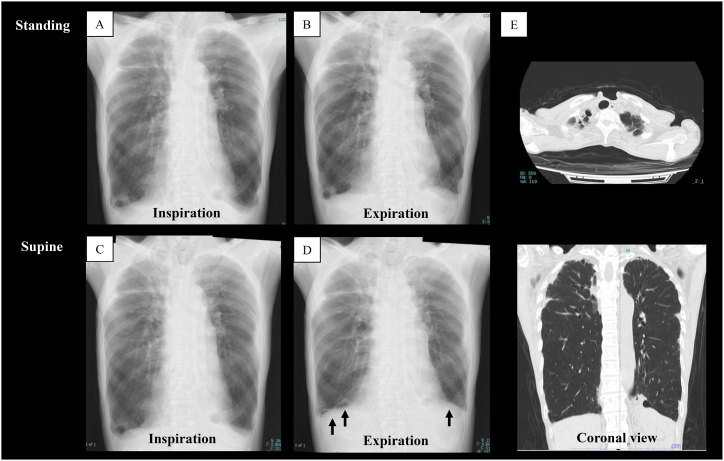
Chest radiography showed bilateral upper pleural thickening and an elevation of the hilar region of the lungs caused by upper lobe volume loss (Fig. 1A). Chest computed tomography revealed pleural thickening with subpleural fibrosis concentrated in the upper lobes, without lower lobe involvement (Fig. 1E). On chest radiography, at maximum inspiration, there was no difference in the diaphragm position between the standing and supine postures (Fig. 1A and C). However, at maximum expiration, the elevation of the diaphragm was greater in the supine position than in the standing position (Fig. 1B and D), suggesting that the diaphragm moved a greater distance in the supine position than in the standing position.
Fig. 1.
Radiography images obtained in the standing and supine positions.
(A) Inspiration and (B) expiration in the standing position. (C) Inspiration and (D) expiration in the supine position. (E) Chest computed tomography image.
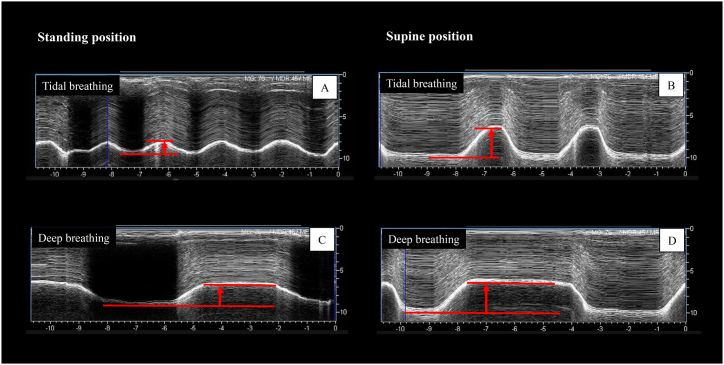
DE was measured using ultrasonography. Excursions of the right hemidiaphragm were measured using an M-mode cursor, which was rotated and placed on the axis of the diaphragmatic displacement in the stored image, followed by measurement of the displacement during each of the rest and deep breaths [3]. The DE at tidal breathing was lower in the standing position than in the supine position (13.4 mm vs. 19.2 mm; Fig. 2A and B, respectively). During deep breathing, the distance was lower in the standing position than in the supine position (20.7 mm vs. 44.5 mm; Table 2, Fig. 2C and D, respectively). Also, the lateral position was equivalent to the supine position (Table 2). The strength of the inspiratory and expiratory muscles was stronger in the supine position than in the standing position (Table 3). This case report was approved by the Ethics Committee of the Kinki University School of Medicine (Approval No. R04-44), and consent for publication of the accompanying images was obtained from the patient.
Fig. 2.
Ultrasonography images of diaphragmatic excursion.
Tidal breathing in the (A) standing position and (B) supine position. Deep breathing in the (C) standing position and (D) supine position.
Table 2.
Change in diaphragm excursion in different postures.
| Standing position | Supine position | Lateral position (left) | Lateral position (right) | |
|---|---|---|---|---|
| Tidal breathing, mm | 13.4 | 19.2 | 19.0 | 19.2 |
| Deep breathing, mm | 20.7 | 44.5 | 42.7 | 43.6 |
Table 3.
Inspiratory and expiratory muscle strength with standing in different postures.
| Standing position | Supine position | |
|---|---|---|
| PImax, cmH2O (% predicted) | 29.6 (58.7) | 42.7 (84.6) |
| PEmax, cmH2O (% predicted) | 30.6 (53.7) | 40.6 (71.3) |
PImax: maximum inspiratory pressure, PEmax: maximum expiratory pressure.
3. Discussion
iPPFE is a rare form of idiopathic interstitial pneumonia, and patients with iPPFE complain of severe exertional dyspnea. Moreover, the 6-min walk test result is significantly lower in these patients than in those with idiopathic pulmonary fibrosis, a representative form of idiopathic interstitial pneumonia [4]. In iPPFE, the lesion is predominantly located in the upper lung, causing the upper lobe to contract and elevate the entire lung while flattening the thorax, whereas the middle and lower lobes are hyperinflated [[5], [6], [7]]. Indeed, Ishii et al. reported that as the thoracic cage flattens, FVC decreases but RV/TLC increases [8]. Therefore, in the standing or sitting position, gravity may enhance the pulmonary hyperinflation in the middle and lower lobes. In contrast, in the supine position, the compensatory overdistension of the middle and lower lobes [7] is attenuated because of the absence of a gravitational effect. In our patient, at maximum inspiration, radiography showed no difference in the diaphragm position between the standing and supine postures, while at maximum expiration, the diaphragm was elevated to a greater extent in the supine position than in the standing position. Moreover, the endurance time was longer, VT was higher, and respiratory rate and VTi–VTe were lower in the supine position than in the sitting position. These results suggest that the diaphragm does not fully elevate in the antigravity position owing to expiratory limitation in patients with iPPFE, which may contribute to ventilatory limitation and dyspnea. On the other hand, the supine position was suggested to increase diaphragm movement and inspiratory and expiratory muscle strength, leading to successful rehabilitation and improved exercise endurance. Expiratory flow limitation during tidal breathing is a major determinant of dynamic hyperinflation and exercise limitation in patients with chronic obstructive pulmonary disease (COPD) [9].
Safavi et al.‘s study using magnetic resonance imaging (MRI) obeserved that diaphragmatic movement distance is decreased in the supine position in patients with severe COPD [10]. The comfortable posture for COPD patients is the “tripod position,” wherein the trunk is tilted forward while supporting the arms; this posture relieves dyspnea and improves lung function [[11], [12], [13], [14]]. The anterior tilt posture also improves the length–tension relationship and shape of the diaphragm and increases the output required for breathing [15]. In contrast, in PPFE patients, the feeling of shortness of breath does not improve even when they lean forward, which is thought to be because of the fact that PPFE patients experience expiratory restriction due to the effects of gravity. In other words, the posture that is considered comforting is different when comparing COPD patients, who have pulmonary hyperinflation, to PPFE patients in this case report.
Although the pathophysiology of iPPFE differs from that of COPD, expiratory limitation may be an important factor in exercise tolerance and dyspnea. Considering that ultrasonography can be repeated without radiation exposure, it is possible to evaluate the difference in diaphragmatic functions due to the postural changes between patients with PPFE and those with COPD.
iPPFE is a rare disease with no effective treatment; therefore, an innovative treatment strategy is warranted for this condition [16]. Ideally, pulmonary rehabilitation should be part of the standard treatment for iPPFE. Moreover, exercise in the supine position may be more effective possibly through an improvement in DE. Nevertheless, additional studies are necessary to confirm this observation.
4. Conclusions
We reported case of a patient with iPPFE in whom postural changes dramatically improved DE and exercise tolerance. This report may provide insights into the mechanisms of dyspnea reduction and may help identify more effective ways of rehabilitation in patients with iPPFE.
Statement of ethics
This case report was approved by the Ethics Committee of the Kinki University School of Medicine (Approval No. R04-44), and consent for publication of the accompanying images was obtained from the patient.
Funding sources
This work was supported by Grants-in-Aid for Scientific Research (21K17664).
Data availability statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
CRediT authorship contribution statement
Masashi Shiraishi: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Visualization, Writing – original draft. Yuji Higashimoto: Writing – review & editing, Conceptualization, Investigation, Methodology. Osamu Nishiyama: Data curation, Methodology, Writing – review & editing. Ryo Yamazaki: Data curation, Methodology, Validation. Ryuji Sugiya: Investigation, Methodology. Hiroki Mizusawa: Data curation, Visualization. Yu Takeda: Data curation, Validation, Visualization. Masaya Noguchi: Investigation, Methodology. Kengo Kanki: Validation, Visualization. Mitsuo Kuwano: Data curation, Investigation. Tamotsu Kimura: Validation, Writing – review & editing. Hisako Matsumoto: Conceptualization, Methodology, Supervision, Writing – review & editing.
Declaration of competing interest
No conflict.
Handling Editor: DR AC Amit Chopra
References
- 1.Travis W.D., Costabel U., Hansell D.M., et al. An official American thoracic society/European respiratory society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2013;188:733–748. doi: 10.1164/rccm.201308-1483st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Enomoto Y., Nakamura Y., Satake Y., et al. Clinical diagnosis of idiopathic pleuroparenchymal fibroelastosis: a retrospective multicenter study. Respir. Med. 2017;133:1–5. doi: 10.1016/j.rmed.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Shiraishi M., Higashimoto Y., Sugiya R., et al. Diaphragmatic excursion correlates with exercise capacity and dynamic hyperinflation in COPD patients. ERJ Open Res. 2020;6:589–2020. doi: 10.1183/23120541.00589-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sato N., Iwanami Y., Ebihara K., et al. Determinants of six-minute walk distance in idiopathic pulmonary fibrosis and idiopathic pleuroparenchymal fibroelastosis. Biomedicines. 2022;10:2556. doi: 10.3390/biomedicines10102556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fukada A., Suzuki Y., Mori K., et al. Idiopathic pleuroparenchymal fibroelastosis: three-dimensional computed tomography assessment of upper-lobe lung volume. Eur. Respir. J. 2022;60 doi: 10.1183/13993003.00637-2022. [DOI] [PubMed] [Google Scholar]
- 6.Ishii H., Kinoshita Y., Kushima H., et al. The similarities and differences between pleuroparenchymal fibroelastosis and idiopathic pulmonary fibrosis. Chron. Respir. Dis. 2019;16 doi: 10.1177/1479973119867945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oda T., Ogura T., Kitamura H., et al. Distinct characteristics of pleuroparenchymal fibroelastosis with usual interstitial pneumonia compared with idiopathic pulmonary fibrosis. Chest. 2014;146:1248–1255. doi: 10.1378/chest.13-2866. [DOI] [PubMed] [Google Scholar]
- 8.Ishii H., Watanabe K., Kushima H., et al. Pleuroparenchymal fibroelastosis diagnosed by multidisciplinary discussions in Japan. Respir. Med. 2018;141:190–197. doi: 10.1016/j.rmed.2018.06.022. [DOI] [PubMed] [Google Scholar]
- 9.Gagnon P., Guenette J.A., Langer D., et al. Pathogenesis of hyperinflation in chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2014;9:187–201. doi: 10.2147/COPD.S38934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Safavi S., Arthofer C., Cooper A., et al. Assessing the impact of posture on diaphragm morphology and function using an open upright MRI system-A pilot study. Eur. J. Radiol. 2020;130 doi: 10.1016/j.ejrad.2020.109196. [DOI] [PubMed] [Google Scholar]
- 11.Bott J., Blumenthal S., Buxton M., et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax. 2009;64:i1–i52. doi: 10.1136/thx.2008.110726. [DOI] [PubMed] [Google Scholar]
- 12.Ogino T., Mase K., Nozoe M., et al. Effects of arm bracing on expiratory flow limitation and lung volume in elderly COPD subjects. Respir. Care. 2015;60:1282–1287. doi: 10.4187/respcare.03945. [DOI] [PubMed] [Google Scholar]
- 13.Gosselink R. Controlled breathing and dyspnea in patients with chronic obstructive pulmonary disease (COPD) J. Rehabil. Res. Dev. 2003;40:25–33. doi: 10.1682/jrrd.2003.10.0025. [DOI] [PubMed] [Google Scholar]
- 14.O'Neill S., McCarthy D.S. Postural relief of dyspnoea in severe chronic airflow limitation: relationship to respiratory muscle strength. Thorax. 1983;38:595–600. doi: 10.1136/thx.38.8.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharp J.T., Drutz W.S., Moisan T., et al. Postural relief of dyspnea in severe chronic obstructive pulmonary disease. Am. Rev. Respir. Dis. 1980;122:201–211. doi: 10.1164/arrd.1980.122.2.201. [DOI] [PubMed] [Google Scholar]
- 16.Chua F., Desai S.R., Nicholson A.G., et al. Pleuroparenchymal fibroelastosis. A review of clinical, radiological, and pathological characteristics. Ann Am Thorac Soc. 2019;16:1351–1359. doi: 10.1513/AnnalsATS.201902-181CME. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.