Abstract
Background
Smoking and chronic kidney disease (CKD) have a disproportionately high prevalence among African American (AA) adults, but their impact on mortality among AA adults is not well known.
Methods
Given the lack of evidence in published literature on specific factors affecting the relationship between CKD and mortality among AA adults, we examined the influence of smoking on mortality among AA adults with CKD. National Health and Nutrition Examination Survey (NHANES, 1999-2010) data were analyzed with study participants prospectively followed up for mortality analysis through December 31, 2019, using National Death Index (NDI) death certificate records.
Results
A total of 6,108 AA adults were included in the study sample, with more than two-fifths (44.9%) being smokers and 6.3% having CKD. AA individuals with CKD had 2.22 (95% CI = 1.38-3.57) times the risk of cardiovascular mortality, but when stratified by smoking, AA individuals with CKD who were current smokers had 3.21 times the risk of cardiovascular mortality. Similarly, in AA with CKD, the risk of all-cause mortality was 3.53 (95% CI = 1.31-9.47), but when stratified by smoking status, AA individuals with CKD who were current smokers had 5.54 times the risk of all-cause mortality.
Conclusions
Smoking and CKD are highly prevalent in AA individuals and frequently cooccur, leading to higher rates of mortality. Smoking cessation interventions should be a priority in collaborative care models and interdisciplinary care teams for AA with CKD and current smoker status.
Keywords: Race, Mortality, Kidney disease, Smoking, Risk
Introduction
African Americans (AA) have disproportionately high rates of chronic diseases, resulting in higher mortality and lower life expectancy.1, 2, 3, 4 For example, recent estimates suggest that AA are significantly more likely to have chronic kidney disease (CKD), kidney failure, or associated mortality when the rates for several other groups are either declining or stabilizing.3, 4, 5, 6, 7 Also, in a recent comprehensive review, most studies (24 out of 36 reviewed) found a higher risk of CKD progression among AAs compared to others. However, in this review, it was also noted that for most studies (18 out of 27), there were no significant differences in survival rates and only 5 studies indicated an increased risk of mortality in AA individuals with CKD.8 It is frequently proposed that the higher rates of CKD and its progression in AA are due to lower socioeconomic status and lifestyle risk factors (e.g., diet, exercise, and smoking).4,8,9 However, regarding mortality due to CKD in AA, some studies have shown that both behavioral and sociodemographic characteristics may play a role, while a few studies found no influence of socioeconomic characteristics.3,5,8, 9, 10 Given the lack of evidence in published literature on specific factors affecting the relationship between CKD and mortality (overall and CVD) among AA individuals, we examined the influence of smoking on CKD and mortality (overall and CVD) relationship among AA individuals. Smoking was specifically examined due to its high prevalence among AA adults and the associated burden of chronic health conditions due to smoking among AA adults.
Methods
Study Sample and Measures
National Health and Nutrition Examination Survey (NHANES, 1999-2010) data were analyzed for this study.11,12 Study participants 20 years of age or above were considered for the analytic sample that was representative of noninstitutionalized African American adults across the nation. Study participants were prospectively followed up for overall mortality and cardiovascular (International Classification of Diseases, 10th revision, codes I-00 to I-99) mortality analysis through December 31, 2019, using probabilistic matching between NHANES and National Death Index (NDI) death certificate records.11, 12, 13, 14 For CKD categorization, we calculated the glomerular filtration rate (GFR) using the Cockcroft-Gault equation. Participants with a GFR < 59 mL/min/1.73 m2 were considered to have CKD.6,13,14 Smoking status was defined by dichotomizing the response to the following question: “Do you now smoke?” status. If the respondent answered “every day” or “some days” to the question, then they were considered to be positive for smoking status. However, if the respondent answered “not at all” then these individuals were to be negative for smoking status. Participant characteristics such as age, sex, education, smoking, family income, and BMI were analyzed for this study. For income, FIPR (family income to poverty ratio) was utilized. For hypertension, stroke, and diabetes history, self-reported data from NHANES survey were utilized. For hypercholesterolemia, the level of cholesterol was determined through laboratory tests and dichotomized according to previously validated standards. For this study, 240 mg/dL was determined as hypercholesterolemia. Before data collection for the NHANES, NCHS Research Ethics Review approved all protocols and procedures.
Analysis
Initially, the study variables were analyzed using descriptive statistics (e.g., frequency, percentage, and mean values). Next, a series of bivariate analyses using Chi-square tests were conducted to assess group differences between participants who currently smoked versus those who did not for sociodemographic and health-related characteristics. Finally, multiple Cox regression models were constructed to examine differences in mortality risk among those with CKD based on smoking status and hazard ratios with 95% confidence intervals (HR, 95% CI) were computed. In these models, to compute the risk of cardiovascular and all-cause mortality among individuals with CKD based on current smoking status, we adjusted for multiple sociodemographic and health-related characteristics of study participants.
Results
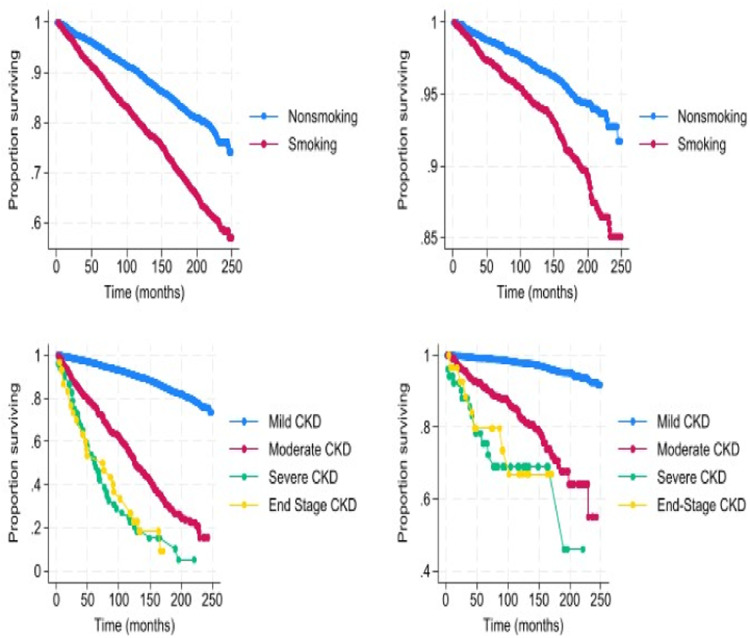
A total of 6108 AA adults were included in the study sample, with more than two-fifths (44.9%) being smokers and 6.3% having CKD. Smokers were statistically significantly more likely to be older, be males, have lower education, be below the poverty level, and have diabetes, hypertension, or hypercholesterolemia. Among smokers, there were 805 deaths compared to 542 deaths among the nonsmokers upon a mean of 8.4 years follow-up (Table 1). For overall mortality, when stratified by smoking status, the mean years of follow-up was 7.6 years among smokers and 8.1 years for nonsmokers. For cardiovascular mortality, when stratified by smoking status, the mean number of years of follow-up was 7.9 years among smokers and 8.1 years for nonsmokers. Figure 1 shows survivorship curves from life tables. There was a graded decline in the proportion of individuals surviving with increasing severity of CKD for both overall and cardiovascular mortality. Additionally, compared to nonsmokers, smokers had a greater decline in the proportion of individuals surviving for both overall and cardiovascular mortality.
Table 1.
Characteristics of sample participants stratified by smoking status
| Characteristics | Total population (n = 6108) | Smoking (+) (n = 2739) | Smoking (−) (n = 3369) |
|---|---|---|---|
| Mean age* (years, 95% CI) | 43.9 (43.4-44.5) | 47.3 (46.7-48.0) | 41.5 (40.8-42.2) |
| Female (%, 95% CI) ⁎⁎ | 55.6 (54.5-56.8) | 46.7 (44.1-49.3) | 62.1 (60.6-63.6) |
| Education level (%, 95% CI)⁎⁎ | |||
| Less than high school | 29.4 (27.1-31.7) | 36.0 (33.3-38.7) | 24.7 (22.3-27.1) |
| High school grad | 24.7 (22.9-26.4) | 25.5 (23.5-27.6) | 24.0 (21.7-26.3) |
| Some college and beyond | 45.9 (43.9-48.0) | 38.5 (36.2-40.9) | 51.3 (48.6-54.0) |
| Family Poverty Income Ratio (%) (PIR < 1)⁎⁎ | 23.3 (21.4-25.3) | 27.7 (25.4-30.0) | 20.2 (18.1-22.4) |
| Mean BMI (kg/m2) | 30.2 (30.0-30.5) | 29.4 (29.1-29.7) | 30.8 (30.4-31.2) |
| Chronic Kidney Disease (%, 95% CI)⁎ | 6.31 (5.7-7.0) | 7.4 (6.4-8.5) | 5.5 (4.8-6.4) |
| Hypertension (%, 95% CI)* | 31.3 (30.0-32.7) | 35.1 (33.2-37.1) | 28.6 (26.9-30.3) |
| Diabetes (%, 95% CI)⁎⁎ | 12.2 (11.2-13.2) | 14.4 (12.9-15.9) | 10.7 (9.4-11.9) |
| Hypercholesterolemia (%, 95% CI) (Ref: LDL < 240 mg/dL)⁎⁎ | 36.3 (34.5-38.1) | 42.9 (40.2-45.7) | 31.7 (29.7-33.7) |
| Stroke (%, 95% CI) | 3.6 (3.2-4.1) | 4.8 (4.1-5.6) | 2.8 (2.3-3.3) |
| All deaths (N)* | 1347 | 805 | 542 |
| Cardiovascular deaths⁎⁎ | 361 | 217 | 144 |
Note:
p < .05.
p < .01. Numbers with 95% CI indicate 95% confidence intervals for proportions.
Smoking + and – indicate participant report of whether they were current smokers.
Figure 1.
Survivorship curve for smoking status vs all-cause mortality (top left), smoking status vs cardiovascular mortality (top right), CKD vs all-cause mortality (bottom left), and CVD vs all-cause mortality (bottom right).
Among the total study population, AA individuals with CKD had 2.22 times the risk of cardiovascular mortality than those without CKD despite adjusting for sociodemographic and health-related factors (Table 2). However, when stratified by smoking, AA individuals with CKD who were current smokers had 3.21 times the risk of cardiovascular mortality (compared to those without CKD or smoking). Similarly, in AA individuals with CKD, the risk of all-cause mortality was 3.53 times higher. When stratified by smoking status, AA individuals with CKD who were current smokers had 5.54 times the risk of all-cause mortality (compared to those without CKD or smoking). For nonsmoking AA individuals with CKD, the risk of mortality was higher than for those without CKD, but the hazard ratios were not statistically significantly higher. The relationship between CKD and cardiovascular mortality was also moderated by age, gender, income, education, and stroke history. In contrast, the relationship between CKD and all-cause mortality was moderated by income, education, stroke history, and hypercholesterolemia (models shown in Table 2).
Table 2.
Mortality risk among African Americans based on smoking status and chronic kidney disease
| Mortality predictors | Cardiovascular mortality |
All-cause mortality |
||||
|---|---|---|---|---|---|---|
| Full population HR (95% CI) | CKD − smoking HR (95% CI) | CKD + smoking HR (95% CI) | Full population HR (95% CI) | CKD − smoking HR (95% CI) | CKD + smoking HR (95% CI) | |
| Chronic kidney disease (Ref ≥ 59 mL/min/1.73 m2) | 2.22 (1.38-3.57)⁎⁎ | 1.43 (0.78-2.60) | 3.21 (1.63-6.31)⁎⁎ | 3.53 (1.31-9.47)* | 1.89 (0.57-6.30) | 5.54 (1.45-21.3)* |
| Diabetes | 1.02 (0.69-1.50) | 0.95 (0.37-2.40) | 1.01 (0.68-1.51) | 0.90 (0.40-2.00) | 0.89 (0.14-5.61) | 0.84 (0.26-2.76) |
| Hypertension | 1.52 (0.90-2.59) | 1.40 (0.71-2.78) | 1.54 (0.85-2.81) | 1.16 (0.50-2.73) | 0.71 (0.25-2.02) | 2.01 (0.54-7.58) |
| BMI (kg/m2) | 1.00 (0.97-1.04) | 1.02 (0.96-1.08) | 0.99 (0.96-1.02) | 1.02 (0.97-1.08) | 1.06 (1.00-1.12) | 1.01 (0.93-1.10) |
| Hypercholesterolemia (Ref: LDL < 240) | 0.82 (0.58-1.16) | 0.76 (0.56-1.04) | 0.92 (0.52-1.63) | 3.04 (1.37-6.75)* | 2.59 (1.00-6.70) | 4.63 (0.90-23.80) |
| Stroke | 2.02 (1.32-3.09)⁎⁎ | 2.41 (0.98-5.92) | 1.80 (0.99-3.29) | 2.64 (1.19-5.85)* | 4.48 (0.69-28.0) | 1.79 (0.55-5.82) |
| Age | 1.06 (1.03-1.08)⁎⁎ | 1.07 (1.03-1.10)⁎⁎ | 1.05 (1.02-1.08)⁎⁎ | 1.03 (0.99-1.08) | 1.05 (1.00-1.11) | 1.03 (0.94-1.12) |
| Gender (Ref: Female) | 0.61 (0.43-0.85)⁎⁎ | 0.73 (0.45-1.17)* | 0.69 (0.42-1.11) | 0.65 (0.34-1.26) | 0.50 (0.23-1.12) | 1.08 (0.43-2.69) |
| Family Poverty to Income Ratio (Ref: PIR ≥ 1) | 1.46 (1.32-2.19)⁎⁎ | 1.24 (0.57-2.70) | 1.69 (1.02-2.80)* | 2.86 (1.74-4.71)⁎⁎ | 2.81 (0.72-10.9) | 1.99 (0.73-5.41) |
| Education level | ||||||
| Some college and beyond | Ref | Ref | Ref | Ref | Ref | Ref |
| High school graduate | 1.79 (1.15-2.76)* | 2.39 (0.94-6.08) | 1.23 (0.76-1.99) | 2.79 (1.61-4.80)⁎⁎ | 1.54 (0.42-5.61) | 5.35 (1.64-17.5)⁎⁎ |
| Less than high school | 1.46 (0.91-2.19) | 2.30 (1.02-5.19)* | 1.01 (0.59-1.73) | 1.44 (0.52-3.97) | 1.22 (0.28-5.29) | 2.61 (0.54-12.59) |
Note:
p < .05.
p < .01. HR (95% CI) indicates hazard ratios with 95% confidence intervals for the outcome (i.e., mortality).
Ref indicates the reference group among each variable for comparison with other groups.
Discussion
The results of this large nationwide study indicate that in AA adults, CKD increases the risk of cardiovascular and all-cause mortality by more than 2 and 3 times, respectively. Current smoking among AA with CKD increases the risk of cardiovascular and all-cause mortality by more than 3 and 5 times, respectively, indicating the detrimental impact of smoking. A cohort study of 7968 middle-aged adults in Taiwan found that the risk of cardiovascular mortality was 2.02 times higher among individuals with decreased GFR and 3.34 times higher among individuals who smoked and had decreased GFR (despite adjusting for cardiovascular risk factors, age, and sex).15 These findings are numerically very similar to our findings despite the stark differences in study period, region, and other sociodemographic or health-related characteristics of study participants across the two groups. In another analysis of 8 cohort studies with nearly 35,000 adults, 40-89 years old, in Japan, it was reported that after adjustment for age and major cardiovascular risk factors, among male and female current smokers with CKD, the risk was 2.26 and 1.78 times higher for all-causes of mortality, and 2.66 and 1.71 times higher for cardiovascular disease mortality, respectively.16
Given that smoking and CKD are highly prevalent in AA individuals and frequently cooccur, multiple pathways could potentially explain the higher risk of mortality among AA with CKD if they smoke (e.g., immune, inflammatory, vascular, biochemical, and metabolic pathways).3,4,14,16,17 For example, the KNOW-CKD prospective cohort study from Korea found that smoking was associated with higher risk of worsening kidney function and the risk of adverse kidney outcomes was incrementally higher as smoking pack-years increased (in contrast, smoking cessation was associated with attenuation of risk of adverse kidney outcomes).18 Interestingly, a recent analysis of the REGARDS study found that the risk of incident CKD and GFR reduction was higher among those who were older and had lower income/education, high blood pressure, high BMI, diabetes, heart disease, and current smoking. Furthermore, these risk factors accounted for higher risk of incident CKD in AA versus whites.9 These findings and our analysis indicate that preventive measures and therapeutic interventions for CKD risk factors (e.g., smoking) could be highly valuable in reducing the disproportionate burden of CKD and its associated morbidity and premature mortality among AA adults.14, 15, 16, 17, 18
The results of this study should be interpreted considering potential limitations. First, there are numerous influences on mortality risk, and we may not have accounted for all of them given the limitations of analyzing existing data. Second, we utilized cross-sectional data from NHANES which precluded the assessment of granular data (e.g., progression of CKD among individuals over time). Third, NHANES data are subject to all threats to validity and reliability inherent to survey study designs (e.g., self-reports and recall bias). Finally, longer duration of follow-up for mortality could influence the results of this study, but the analysis was limited to existing data available in NHANES and NDI. Despite these limitations, this study is one of the very few and largest studies assessing the risk of mortality among AA adults with CKD based on current smoking status. A major strength of the study was that we were able to discern that CKD not only causes increased overall mortality but also leads to increased cardiovascular mortality. This is supported by previous literature on the pathophysiological development of cardiorenal syndrome.9 Another strength was that the analysis was adjusted for several sociodemographic and health-related variables, and despite the adjustments, smoking status modified the association between CKD and all-cause and cardiovascular disease–related mortality.
CRediT authorship contribution statement
Srikanta Banerjee: Methodology, Formal analysis, Data curation. Jagdish Khubchandani: Writing – review & editing, Writing – original draft, Supervision, Formal analysis. W. Sumner Davis: Writing – review & editing, Validation, Methodology, Investigation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data Availability
All of the study data are publicly available at the U.S. Centers for Disease Control and Prevention NHANES website: https://www.cdc.gov/nchs/nhanes/index.htm.
Contributor Information
Srikanta Banerjee, Email: srikanta.banerjee2@mail.waldenu.edu.
Jagdish Khubchandani, Email: jagdish@nmsu.edu.
W. Sumner Davis, Email: sumner.davis@mail.waldenu.edu.
References
- 1.Jackman MR, Shauman KA. The toll of inequality: Excess African American deaths in the United States over the twentieth century. Du Bois Rev.: Social Science Research on Race. 2019;16(2):291–340. [Google Scholar]
- 2.Quiñones AR, Botoseneanu A, Markwardt S, Nagel CL, Newsom JT, Dorr DA, Allore HG. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLOS One. 2019;14(6) doi: 10.1371/journal.pone.0218462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehrotra R, Kermah D, Fried L, et al. Racial differences in mortality among those with CKD. J Am Soc Nephrol.: JASN. 2008;19(7):1403. doi: 10.1681/ASN.2007070747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tarver-Carr ME, Powe NR, Eberhardt MS, et al. Excess risk of chronic kidney disease among African-American versus white subjects in the United States: A population-based study of potential explanatory factors. J Am Soc Nephrol. 2002;13(9):2363–2370. doi: 10.1097/01.asn.0000026493.18542.6a. [DOI] [PubMed] [Google Scholar]
- 5.Kobo O, Abramov D, Davies S, et al. CKD-associated cardiovascular mortality in the United States: Temporal trends from 1999 to 2020. Kidney Med. 2023;5(3):100597. doi: 10.1016/j.xkme.2022.100597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bragg-Gresham J, Xhang X, Le D, et al. Prevalence of chronic kidney disease among black individuals in the US after removal of the black race coefficient from a glomerular filtration rate estimating equation. JAMA Netw Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.35636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC. Prevalence of CKD among adults. 2023. Available at: https://nccd.cdc.gov/CKD/detail.aspx?QNum=Q9.
- 8.Hounkpatin HO, Fraser SD, Honney R, Dreyer G, Brettle A, Roderick PJ. Ethnic minority disparities in progression and mortality of pre-dialysis chronic kidney disease: A systematic scoping review. BMC Nephrol. 2020;21:1–14. doi: 10.1186/s12882-020-01852-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung KL, Crews DC, Cushman M, et al. Risk factors for incident CKD in Black and White Americans: The REGARDS study. Am J Kidney Dis. 2023;;82(1):11–21. doi: 10.1053/j.ajkd.2022.11.015. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fedewa SA, et al. The association between race and income on risk of mortality in patients with moderate chronic kidney disease. BMC Nephrol. 2014;15:1–9. doi: 10.1186/1471-2369-15-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey. 2023. Available at: https://www.cdc.gov/nchs/nhanes/index.htm.
- 12.Banerjee S, Radak T, Khubchandani J, Dunn P. Food insecurity and mortality in American adults: Results from the NHANES-linked mortality study. Health Promot Pract. 2021;22(2):204–214. doi: 10.1177/1524839920945927. [DOI] [PubMed] [Google Scholar]
- 13.Rai NK, Wang Z, Drawz PE, et al. CKD progression risk and subsequent cause of death: A population-based cohort study. Kidney Med. 2023;5(4) doi: 10.1016/j.xkme.2023.100604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banerjee S, Khubchandani J, Noonan L, et al. Risk of mortality among people with rheumatoid arthritis and depression. Egypt Rheumatol. 2024;46(1):43–46. [Google Scholar]
- 15.Cheng TYD, Wen SF, Astor BC, et al. Mortality risks for all causes and cardiovascular diseases and reduced GFR in a middle-aged working population in Taiwan. Am J Kidney Dis. 2008;52(6):1051–1060. doi: 10.1053/j.ajkd.2008.05.030. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura K, Nakagawa H, Murakami Y, et al. Smoking increases the risk of all-cause and cardiovascular mortality in patients with chronic kidney disease. Kidney Int. 2015;88(5):1144–1152. doi: 10.1038/ki.2015.212. [DOI] [PubMed] [Google Scholar]
- 17.Orth SR, Hallan SI. Smoking: A risk factor for progression of chronic kidney disease and for cardiovascular morbidity and mortality in renal patients—absence of evidence or evidence of absence? Clin J Am Soc Nephrol. 2008;3(1):226–236. doi: 10.2215/CJN.03740907. [DOI] [PubMed] [Google Scholar]
- 18.Lee S, Kang S, Joo YS, et al. Smoking, smoking cessation, and progression of chronic kidney disease: Results from KNOW-CKD study. Nicotine Tob Res. 2021;23(1):92–98. doi: 10.1093/ntr/ntaa071. [DOI] [PubMed] [Google Scholar]