Abstract
Background
National Cancer Center (NCC) updated nationwide cancer statistics using population-based cancer registry data in 2015.
Methods
501 cancer registries submitted data, among which 368 registries with high quality data were included in analysis. Numbers of nationwide new cancer cases and deaths were estimated using incidence and mortality rates and corresponding national population stratified by area, sex, age group and cancer site. The world Segi's population was applied for the calculation of age-standardized rates.
Results
About 3,929,000 new cancer cases were diagnosed. The crude incidence rate was 285.83/100,000 and the age-standardized incidence rate by world standard population (ASIRW) was 186.39/100,000. ASIRW was higher in urban areas than in rural areas. South China had the highest ASIRW while Southwest China had the lowest ASIRW. Age-specific incidence rate was higher in males for population younger than 20 years or over 49 years. From 2000 to 2015, the ASIRWs for esophageal cancer, gastric cancer and liver cancer decreased significantly. The ASIRWs for colorectal cancer in whole population and for lung cancer, breast cancer, cervix cancer, uterus cancer and thyroid cancer in females increased significantly. 2,338,000 cancer deaths were reported. The crude mortality rate was 170.05/100,000 and the age standardized mortality rate by world standard population (ASMRW) was 105.84/100,000. ASMRW was higher in rural areas than in urban areas. Central China had the highest ASMRW while North China had the lowest ASMRW. Age-specific mortality rates in males were higher than that in females in every age group. From 2000 to 2015, the ASMRWs for esophageal cancer, gastric cancer, liver cancer and lung cancer decreased significantly. The ASMRWs for colorectal cancer, pancreas cancer and prostate cancer in males and for breast cancer, cervix cancer and thyroid cancer in females increased significantly.
Conclusions
Cancer has become a major life-threatening disease in China. Disease burdens differed across areas. Disease burdens for esophageal cancer, gastric cancer and liver cancer have decreased, while disease burdens for colorectal cancer, female breast cancer, cervix cancer and thyroid cancer have increased over the last 15 years. National and regional initiative for cancer prevention and control should be prioritized.
Keywords: Cancer registry, Incidence, Mortality, Epidemiology, China
Introduction
Cancer has become the leading cause of death in China. Nationwide cancer registry data can reflect the cancer disease burden in whole country. National Cancer Registration and Follow-up Program was launched by the Ministry of Health in 2008. To date, a national cancer surveillance network has been built in China and cancer registration has been carried out in all provinces. National Cancer Center (NCC) is responsible for collecting, evaluating, and publishing national cancer statistics of China. In 2015, the national cancer surveillance network has expanded to 501 cancer registries, providing cancer registry data with high quality and national representativeness.
A previous publication on Cancer statistics in China in 2015 have been published by Chen W et al.1, but the result was predicted by using data in 2009 to 2011 from 72 cancer registries and the results are high due to the most registries were in high incidence areas. But in this paper, we aim to report the estimated new cancer cases and deaths in 2015, as well as a comprehensive overview of cancer incidence and mortality. The update of nationwide cancer profiles can provide scientific evidence for health policymaking in China.
Materials and methods
Data source
By 30th August 2018, a total of 501 local cancer registries from 31 provinces submitted cancer registry data of 2015 to NCC. All cancer registries covered 387,872,825 populations, including 197,211,672 males and 190,661,153 females, accounting for 28.22% of the national population in 2015. All patients included in the statistics are invasive cases and all cancer cases were coded according to the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) and the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). Provincial cancer registry centers are responsible for collecting, evaluating, and publishing provincial cancer statistics. Local population-based cancer registries are responsible for collecting and evaluating cancer registry data within the administrative regions. All hospitals, medical and health institutions in administrative region are required to submit cancer records to local cancer registries.
Data quality control
NCC assessed the validity, reliability, completeness and comparability of all cancer registry data based on the quality control criteria of “Guideline for Chinese Cancer Registration”2 by NCC and criteria by International Agency for Research on Cancer/International Association of Cancer Registries (IARC/IACR).3,4 A series of indexes were taken into consideration, including the mortality to incidence (M/I) ratio, the percentage of cases morphologically verified (MV), the percentage of death certificate-only cases (DCO), the percentage of the diagnosis of unknown basis (UB) and the stability of cancer trends over years.
National population data sources
National Bureau of Statistics of the People's Republic of China provided national population data of 2015 stratified by area (urban/rural) and sex. We estimated the age-specific population of 2015 according to the population structure of the fifth and sixth National Population Census, which provided the whole population data of 2000 and 2010 by age group (0-, 1–4, 5–84 by 5 years and 85+ years). The change of age-specific death probabilities between the two Census data was calculated and the age-specific death probabilities of 2015 were estimated under the assumption of linear interpolation and extrapolation. We used estimated death probabilities to estimate the population age structure in 2015. We multiplied estimated age structure by national population of 2015 to calculate age-specific population.
Statistical analysis
Areas covered by population-based cancer registries were classified into urban/rural areas and seven administrative regions according to the National Bureau of Statistics of the People's Republic of China. Urban areas were defined as regions above county level and rural areas were defined as regions of county level. Seven administrative regions included North (Beijing, Tianjin, Hebei, Shanxi, Inner Mongolia), Northeast (Heilongjiang, Jilin, Liaoning), East (Shanghai, Shandong, Jiangsu, Zhejiang, Fujian, Anhui, Jiangxi), Central (Henan, Hubei, Hunan), South (Guangdong, Guangxi, Hainan), Southwest (Chongqing, Sichuan, Guizhou, Yunnan, Tibet) and Northwest (Shaanxi, Gansu, Ningxia, Qinghai, Xinjiang).
Cancer incidence and mortality rates stratified by age (0-, 1–4, 5–84 by 5 years and 85+ years), sex (male/female), area (urban/rural) and region (7 administrative regions) were calculated using data with good quality. We multiplied these incidence and mortality rates by population in each stratum and added them up to obtain the estimated numbers of new cancer cases and deaths in China. The Segi's population was used to calculate age-standardized rates for the purpose of comparison.5 We applied SAS software (Version 9.4, SAS Institute Inc., Cary, USA) for statistical analysis.
The trends for cancer incidence and mortality from 2000 to 2015 were tested by fitting Joinpoint Regression Models (https://surveillance.cancer.gov/joinpoint/). Those 22 cancer registries used for trend analysis were evaluated with qualified and continues data which established since 1990s, covered about 3.34% of the whole national population and more details about those 22 registries can be find in previous publication.1 The models used for trend analysis were restricted to a maximum of 2 joinpoints (with 3 segments) to reduce the possibility of reporting spurious changes over the period. Trends were expressed as an average annual percent change (AAPC) and the Z test was used to examine whether the change was statistically different from zero.
Results
Basic information of cancer registry data
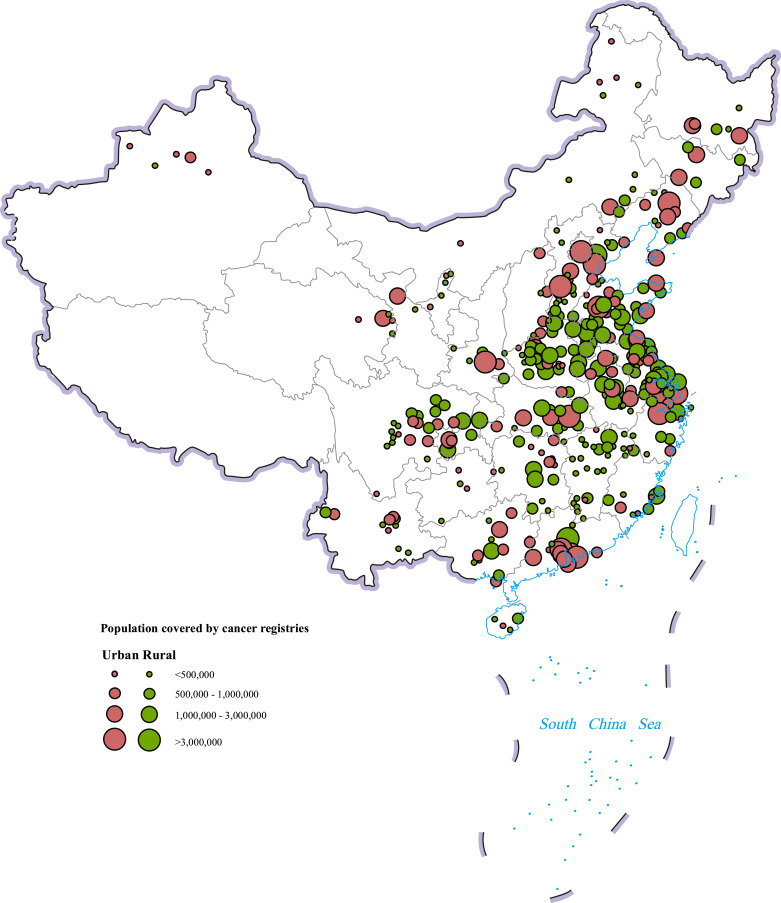
Data from 368 cancer registries met quality control criteria and were pooled together for subsequent analysis, of which 134 were in cities above the county level and 234 were in cities of the county level (Fig. 1). These registries covered 309,553,499 populations, including 156,934,140 males and 152,619,359 females, accounting for 22.52% of the national population in 2015 (Table 1).
Fig. 1.
Map of the 368 contributing cancer registries and geographic regions in China (the dots are locations of the cancer registries).
Table 1.
Registry number and population coverage in different areas.
| Areas | Registries | Population |
|---|---|---|
| Urban/rural areas | ||
| Urban areas | 134 | 148,804,626 |
| Rural areas | 234 | 160,748,873 |
| Seven administrative regions | ||
| North | 44 | 45,184,181 |
| Northeast | 25 | 23,188,244 |
| East | 134 | 123,935,648 |
| Central | 62 | 48,479,402 |
| South | 31 | 32,874,565 |
| Southwest | 44 | 23,808,099 |
| Northwest | 28 | 12,083,360 |
| All | 368 | 309,553,499 |
Estimated numbers of new cancer cases and cancer incidence rates
Table 2 displays the estimated nationwide numbers of new cancer cases, crude incidence rates and age-standardized incidence rates by world standard population (Segi's population) (ASIRWs) by cancer site and sex in 2015. About 3,929,000 new cancer cases were diagnosed in 2015, including 2,151,000 male cases and 1,778,000 female cases. The crude incidence rate was 285.83/100,000 (305.47/100,000 in males, 265.21/100,000 in females). The ASIRW was 186.39/100,000 (206.49/100,000 in males, 168.45/100,000 in females). Lung cancer (787,000 cases) was the most common cancer in whole population. Lung cancer (520,000) was the most common cancer in males and female breast cancer (304,000) was the most common cancer in females.
Table 2.
Estimated numbers of new cancer cases and incidence rates by sex in China, 2015.
| ICD-10 | Site | All |
Male |
Female |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases (× 104) | Crude incidence (× 1/105) | ASIRW (× 1/105) | Cases (× 104) | Crude incidence (× 1/105) | ASIRW (× 1/105) | Cases (× 104) | Crude incidence (× 1/105) | ASIRW (× 1/105) | ||
| C00–10, 12–14 | Lip,oral cavity & pharynx but nasopharynx | 5.2 | 3.77 | 2.49 | 3.5 | 4.92 | 3.35 | 1.7 | 2.55 | 1.63 |
| C11 | Nasopharynx | 5.1 | 3.71 | 2.53 | 3.6 | 5.14 | 3.56 | 1.5 | 2.22 | 1.48 |
| C15 | Esophagus | 24.6 | 17.87 | 11.28 | 17.7 | 25.13 | 16.75 | 6.9 | 10.25 | 5.94 |
| C16 | Stomach | 40.3 | 29.31 | 18.57 | 28.1 | 39.95 | 26.56 | 12.2 | 18.15 | 10.83 |
| C18–21 | Colorectum | 38.8 | 28.20 | 17.81 | 22.5 | 31.96 | 21.21 | 16.3 | 24.25 | 14.54 |
| C22 | Liver | 37.0 | 26.92 | 17.35 | 27.4 | 38.98 | 26.15 | 9.6 | 14.26 | 8.54 |
| C23, 24 | Gallbladder | 5.4 | 3.95 | 2.41 | 2.6 | 3.70 | 2.42 | 2.8 | 4.21 | 2.41 |
| C25 | Pancreas | 9.5 | 6.92 | 4.29 | 5.4 | 7.67 | 5.06 | 4.1 | 6.14 | 3.54 |
| C32 | Larynx | 2.5 | 1.84 | 1.19 | 2.3 | 3.20 | 2.14 | 0.3 | 0.42 | 0.25 |
| C33, 34 | Lung | 78.7 | 57.26 | 35.92 | 52.0 | 73.90 | 48.87 | 26.7 | 39.78 | 23.52 |
| C37, 38 | Other thoracic organs | 1.3 | 0.93 | 0.64 | 0.8 | 1.10 | 0.79 | 0.5 | 0.74 | 0.49 |
| C40, 41 | Bone | 2.4 | 1.77 | 1.32 | 1.4 | 1.99 | 1.52 | 1.0 | 1.53 | 1.11 |
| C43 | Melanoma of skin | 0.7 | 0.53 | 0.35 | 0.4 | 0.53 | 0.37 | 0.3 | 0.52 | 0.34 |
| C50 | Female breast | 30.4 | 45.29 | 29.56 | — | — | — | 30.4 | 45.29 | 29.56 |
| C53 | Cervix | 11.1 | 16.56 | 10.86 | — | — | — | 11.1 | 16.56 | 10.86 |
| C54, 55 | Uterus | 6.9 | 10.28 | 6.66 | — | — | — | 6.9 | 10.28 | 6.66 |
| C56 | Ovary | 5.3 | 7.88 | 5.29 | — | — | — | 5.3 | 7.88 | 5.29 |
| C61 | Prostate | 7.2 | 10.23 | 6.47 | 7.2 | 10.23 | 6.47 | — | — | — |
| C62 | Testis | 0.3 | 0.49 | 0.42 | 0.3 | 0.49 | 0.42 | — | — | — |
| C64–66, 68 | Kidney | 7.4 | 5.40 | 3.56 | 4.7 | 6.66 | 4.54 | 2.7 | 4.08 | 2.58 |
| C67 | Bladder | 8.0 | 5.80 | 3.57 | 6.2 | 8.83 | 5.76 | 1.8 | 2.61 | 1.50 |
| C70–72 | Brain,CNS | 10.6 | 7.72 | 5.56 | 5.0 | 7.04 | 5.34 | 5.7 | 8.43 | 5.77 |
| C73 | Thyroid | 20.1 | 14.60 | 10.44 | 4.9 | 7.03 | 5.12 | 15.1 | 22.56 | 15.94 |
| C81–85, 88,90,96 | Lymphoma | 9.0 | 6.52 | 4.48 | 5.2 | 7.43 | 5.29 | 3.7 | 5.56 | 3.69 |
| C91–95 | Leukaemia | 8.7 | 6.30 | 5.32 | 4.9 | 7.02 | 6.03 | 3.7 | 5.54 | 4.60 |
| A_O | All other sites | 16.4 | 11.76 | 7.89 | 9.0 | 12.10 | 8.46 | 7.5 | 11.41 | 7.36 |
| ALL | All sites | 392.9 | 285.83 | 186.39 | 215.1 | 305.47 | 206.49 | 177.8 | 265.21 | 168.45 |
ICD-10, International Statistical Classification of Diseases and Related Health Problems 10th Revision.
ASIRW, age-standardized incidence rate by world standard population (Segi's population); CNS, central nervous system.
Table 3 displays the ASIRWs of all cancers combined and selected cancer types in cancer registry areas in 2015. ASIRW for all cancers combined was higher in urban areas than in rural areas (191.5/100,000 vs. 179.3/100,000). South China had the highest ASIRW (203.6/100,000), followed by Northeast China (189.0/100,000) and East China (188.2/100,000). Southwest China (161.6/100,000) had the lowest ASIRW. ASIRWs for colorectal cancer, lung cancer, female breast cancer, prostate cancer, kidney cancer, bladder cancer, lymphoma and leukemia were higher in urban areas than in rural areas. ASIRWs for esophageal cancer, gastric cancer, liver cancer and cervical cancer were higher in rural areas than in urban areas. ASIRW for kidney cancer was highest in North China. ASIRWs for lung cancer, female breast cancer and bladder cancer were highest in Northeast China. ASIRWs for esophageal cancer and cervical cancer were highest in Central China. ASIRWs for colorectal cancer, liver cancer, prostate cancer, lymphoma and leukemia were highest in South China. ASIRW for gastric cancer was highest in Northwest China.
Table 3.
Age-standardized incidence rates by world standard population (ASIRWs) of selected cancers in areas covered by 368 cancer registries, 2015 (× 1/105).
| Geographic areas | All sites | Esophagus | Stomach | Colorectum | Liver | Lung | Female breast | Cervix | Prostate | Kidney | Bladder | Lymphoma | Leukemia |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All areas | 185.5 | 11.9 | 19.0 | 17.4 | 17.7 | 35.9 | 28.7 | 11.0 | 6.2 | 3.4 | 3.5 | 4.4 | 5.3 |
| Urban | 191.5 | 7.7 | 16.2 | 20.3 | 15.6 | 36.0 | 33.8 | 10.4 | 8.2 | 4.3 | 4.0 | 4.9 | 5.4 |
| Rural | 179.3 | 16.2 | 21.8 | 14.3 | 19.7 | 35.7 | 23.6 | 11.5 | 4.1 | 2.4 | 3.0 | 3.8 | 5.2 |
| North | 178.1 | 7.9 | 14.7 | 16.3 | 12.2 | 35.4 | 33.7 | 8.1 | 5.7 | 5.3 | 4.3 | 5.2 | 6.3 |
| Northeast | 189.0 | 4.9 | 14.4 | 21.3 | 17.3 | 41.2 | 35.4 | 10.9 | 4.9 | 5.2 | 4.9 | 3.1 | 4.2 |
| East | 188.2 | 14.6 | 23.3 | 17.0 | 17.2 | 35.3 | 27.3 | 10.5 | 7.1 | 3.1 | 3.2 | 4.3 | 5.0 |
| Central | 185.8 | 15.2 | 20.1 | 14.8 | 19.0 | 37.4 | 27.2 | 14.9 | 4.5 | 2.5 | 2.9 | 4.4 | 5.2 |
| South | 203.6 | 4.6 | 9.7 | 23.7 | 25.9 | 36.5 | 33.6 | 11.1 | 8.7 | 2.8 | 3.4 | 5.8 | 6.4 |
| Southwest | 161.6 | 13.7 | 13.4 | 16.1 | 18.9 | 34.1 | 18.1 | 11.6 | 4.3 | 1.7 | 3.0 | 3.8 | 5.1 |
| Northwest | 178.7 | 12.9 | 27.8 | 13.4 | 18.4 | 30.0 | 23.2 | 11.5 | 6.3 | 3.8 | 3.5 | 2.8 | 4.3 |
| North (Urban) | 184.1 | 4.4 | 11.1 | 19.2 | 10.7 | 34.2 | 38.9 | 7.8 | 7.6 | 6.7 | 4.8 | 6.0 | 6.3 |
| Northeast (Urban) | 195.6 | 4.5 | 14.0 | 23.3 | 15.0 | 41.6 | 40.1 | 11.9 | 5.6 | 5.9 | 5.1 | 3.4 | 4.3 |
| East (Urban) | 195.0 | 10.0 | 21.3 | 19.9 | 14.6 | 35.1 | 32.4 | 10.1 | 9.9 | 3.9 | 3.5 | 4.7 | 5.0 |
| Central (Urban) | 186.8 | 8.9 | 14.8 | 18.0 | 15.4 | 37.6 | 32.2 | 13.2 | 6.9 | 3.3 | 4.1 | 5.4 | 5.1 |
| South (Urban) | 210.5 | 4.6 | 9.2 | 25.8 | 24.1 | 37.3 | 36.8 | 10.5 | 9.8 | 3.1 | 3.6 | 6.3 | 6.8 |
| Southwest (Urban) | 157.7 | 7.4 | 9.8 | 17.3 | 15.6 | 34.5 | 20.7 | 10.8 | 5.9 | 2.3 | 3.3 | 4.7 | 5.2 |
| Northwest (Urban) | 192.5 | 13.9 | 30.8 | 15.3 | 18.8 | 31.4 | 25.7 | 11.0 | 7.3 | 4.4 | 4.0 | 3.1 | 4.5 |
| North (Rural) | 171.8 | 11.8 | 18.6 | 13.1 | 13.8 | 36.6 | 28.1 | 8.5 | 3.4 | 3.7 | 3.7 | 4.3 | 6.2 |
| Northeast (Rural) | 171.9 | 5.9 | 15.5 | 15.7 | 23.3 | 40.1 | 23.5 | 8.5 | 2.8 | 3.3 | 4.1 | 2.3 | 3.9 |
| East (Rural) | 182.9 | 18.3 | 24.9 | 14.7 | 19.3 | 35.5 | 23.3 | 10.8 | 4.8 | 2.4 | 3.0 | 4.0 | 5.0 |
| Central (Rural) | 185.1 | 19.1 | 23.2 | 12.9 | 21.2 | 37.2 | 24.2 | 16.0 | 3.0 | 1.9 | 2.2 | 3.7 | 5.2 |
| South (Rural) | 187.7 | 4.8 | 10.8 | 19.0 | 30.0 | 34.6 | 26.3 | 12.3 | 6.1 | 2.2 | 2.8 | 4.6 | 5.5 |
| Southwest (Rural) | 164.7 | 18.9 | 16.6 | 15.0 | 21.7 | 33.8 | 15.9 | 12.3 | 3.0 | 1.2 | 2.8 | 3.2 | 5.1 |
| Northwest (Rural) | 150.2 | 11.2 | 22.1 | 9.6 | 17.3 | 27.2 | 17.9 | 12.5 | 4.0 | 2.5 | 2.5 | 2.3 | 4.0 |
Estimated numbers of cancer deaths and cancer mortality rates
Table 4 displays the estimated nationwide numbers of cancer deaths, crude mortality rates and age-standardized mortality rates by world standard population (Segi's population) (ASMRWs) by cancer sites and sex in 2015. About 2,338,000 cancer deaths were reported in 2015, including 1,480,000 male deaths and 858,000 female deaths. The crude mortality rate was 170.05/100,000 (210.10/100,000 in males, 128.00/100,000 in females). The ASMRW was 105.84/100,000 (138.57/100,000 in males, 74.81/100,000 in females). Lung cancer was the most common cause of cancer deaths in both males and females.
Table 4.
Estimated cancer deaths and mortality rates by sex in China, 2015.
| ICD-10 | Site | All |
Male |
Female |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deaths (× 104) | Crude mortality (× 1/105) | ASMRW (× 1/105) | Deaths (× 104) | Crude mortality (× 1/105) | ASMRW (× 1/105) | Deaths (× 104) | Crude mortality (× 1/105) | ASMRW (× 1/105) | ||
| C00–10, 12–14 | Lip,oral cavity & pharynx but nasopharynx | 2.4 | 1.73 | 1.08 | 1.7 | 2.45 | 1.61 | 0.7 | 0.99 | 0.56 |
| C11 | Nasopharynx | 2.7 | 1.98 | 1.30 | 2.0 | 2.88 | 1.95 | 0.7 | 1.04 | 0.65 |
| C15 | Esophagus | 18.8 | 13.68 | 8.36 | 13.7 | 19.45 | 12.74 | 5.1 | 7.62 | 4.14 |
| C16 | Stomach | 29.1 | 21.16 | 12.92 | 20.1 | 28.59 | 18.61 | 9.0 | 13.37 | 7.53 |
| C18–21 | Colorectum | 18.7 | 13.61 | 8.12 | 11.0 | 15.56 | 10.01 | 7.8 | 11.58 | 6.37 |
| C22 | Liver | 32.6 | 23.72 | 15.09 | 24.2 | 34.31 | 22.88 | 8.4 | 12.60 | 7.35 |
| C23, 24 | Gallbladder | 4.1 | 2.95 | 1.75 | 1.9 | 2.72 | 1.75 | 2.1 | 3.18 | 1.75 |
| C25 | Pancreas | 8.5 | 6.16 | 3.76 | 4.8 | 6.88 | 4.49 | 3.6 | 5.41 | 3.04 |
| C32 | Larynx | 1.4 | 1.00 | 0.61 | 1.2 | 1.70 | 1.11 | 0.2 | 0.25 | 0.14 |
| C33. 34 | Lung | 63.1 | 45.87 | 28.02 | 43.3 | 61.52 | 40.11 | 19.7 | 29.43 | 16.54 |
| C37, 38 | Other thoracic organs | 0.7 | 0.49 | 0.33 | 0.4 | 0.61 | 0.43 | 0.2 | 0.36 | 0.23 |
| C40, 41 | Bone | 1.8 | 1.31 | 0.89 | 1.1 | 1.51 | 1.06 | 0.7 | 1.10 | 0.72 |
| C43 | Melanoma of skin | 0.4 | 0.27 | 0.17 | 0.2 | 0.31 | 0.20 | 0.2 | 0.24 | 0.14 |
| C50 | Female breast | 7.0 | 10.50 | 6.48 | — | — | — | 7.0 | 10.50 | 6.48 |
| C53 | Cervix | 3.4 | 5.04 | 3.15 | — | — | — | 3.4 | 5.04 | 3.15 |
| C54, 55 | Uterus | 1.6 | 2.39 | 1.47 | — | — | — | 1.6 | 2.39 | 1.47 |
| C56 | Ovary | 2.5 | 3.73 | 2.35 | — | — | — | 2.5 | 3.73 | 2.35 |
| C61 | Prostate | 3.1 | 4.36 | 2.65 | 3.1 | 4.36 | 2.65 | — | — | — |
| C62 | Testis | 0.1 | 0.11 | 0.09 | 0.1 | 0.11 | 0.09 | — | — | — |
| C64–66, 68 | Kidney | 2.7 | 1.97 | 1.21 | 1.7 | 2.40 | 1.58 | 1.0 | 1.52 | 0.87 |
| C67 | Bladder | 3.3 | 2.37 | 1.32 | 2.5 | 3.56 | 2.20 | 0.7 | 1.11 | 0.55 |
| C70–72 | Brain,CNS | 5.6 | 4.10 | 2.90 | 3.1 | 4.40 | 3.23 | 2.5 | 3.77 | 2.58 |
| C73 | Thyroid | 0.8 | 0.58 | 0.36 | 0.3 | 0.43 | 0.28 | 0.5 | 0.73 | 0.44 |
| C81–85,88,90,96 | Lymphoma | 5.0 | 3.62 | 2.36 | 3.1 | 4.38 | 2.99 | 1.9 | 2.84 | 1.74 |
| C91–95 | Leukemia | 5.4 | 3.96 | 3.07 | 3.2 | 4.51 | 3.56 | 2.3 | 3.39 | 2.59 |
| A_O | All other sites | 9.0 | 6.56 | 4.16 | 5.3 | 7.27 | 4.91 | 4.0 | 5.82 | 3.45 |
| ALL | All sites | 233.8 | 170.05 | 105.84 | 148.0 | 210.10 | 138.57 | 85.8 | 128.00 | 74.81 |
ICD-10, International Statistical Classification of Diseases and Related Health Problems 10th Revision.
ASMRW, age-standardized mortality rate by world standard population (Segi's population); CNS, central nervous system.
Table 5 displays the ASMRWs of all cancers combined and selected major cancer types in cancer registry areas in 2015. ASMRWs for all cancers combined was higher in rural areas than in urban areas (109.8/100,000 vs. 102.8/100,000). Central China had the highest cancer mortality rate (112.8/100,000), followed by Northeast China (110.2/100,000) and East China (108.4/100,000). North China (94.7/100,000) had the lowest mortality rate. ASMRWs for colorectal cancer, female breast cancer, prostate cancer, kidney cancer, bladder cancer, lymphoma and leukemia were higher in urban areas than in rural areas. ASMRWs for esophageal cancer, gastric cancer, liver cancer, lung cancer and cervix cancer were higher in rural areas than in urban areas. ASMRWs for lung cancer, female breast cancer, kidney cancer and bladder cancer were highest in Northeast China. ASMRWs for esophageal cancer and cervical cancer were highest in Central China. ASMRWs for colorectal cancer, liver cancer, prostate cancer and lymphoma were highest in South China. ASMRWs for gastric cancer was highest in Northwest China. ASMRWs for leukemia cancer was similar in different areas.
Table 5.
Age-standardized mortality rates by world standard population (ASMRWs) of selected cancers in areas covered by 368 cancer registries, 2015 (× 1/105).
| Geographic areas | All sites | Esophagus | Stomach | Colorectum | Liver | Lung | Female breast | Cervix | Prostate | Kidney | Bladder | Lymphoma | Leukemia |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All areas | 106.4 | 8.8 | 13.3 | 8.0 | 15.3 | 28.1 | 6.4 | 3.2 | 2.6 | 1.2 | 1.3 | 2.3 | 3.1 |
| Urban | 102.8 | 5.9 | 10.9 | 9.2 | 13.7 | 27.8 | 7.1 | 3.0 | 3.2 | 1.5 | 1.4 | 2.5 | 3.1 |
| Rural | 109.8 | 11.7 | 15.7 | 6.7 | 16.9 | 28.3 | 5.6 | 3.4 | 1.9 | 0.8 | 1.2 | 2.1 | 3.0 |
| North | 94.7 | 5.4 | 10.5 | 7.0 | 10.6 | 27.1 | 7.0 | 2.4 | 2.3 | 1.7 | 1.5 | 2.5 | 3.3 |
| Northeast | 110.2 | 4.0 | 10.0 | 9.8 | 15.5 | 34.1 | 7.6 | 3.3 | 2.4 | 1.8 | 1.8 | 1.8 | 2.4 |
| East | 108.4 | 10.9 | 15.9 | 7.7 | 15.2 | 27.0 | 5.8 | 2.7 | 2.7 | 1.0 | 1.2 | 2.4 | 3.0 |
| Central | 112.8 | 11.0 | 14.8 | 7.5 | 16.5 | 30.4 | 7.0 | 4.6 | 2.1 | 1.0 | 1.2 | 2.4 | 3.1 |
| South | 106.9 | 3.8 | 6.4 | 10.0 | 21.5 | 28.3 | 7.1 | 3.3 | 3.5 | 0.9 | 1.1 | 2.8 | 3.3 |
| Southwest | 102.5 | 9.8 | 10.5 | 7.9 | 16.5 | 27.7 | 4.6 | 3.9 | 2.3 | 0.6 | 1.3 | 1.9 | 3.3 |
| Northwest | 105.6 | 9.6 | 18.3 | 7.2 | 14.7 | 23.1 | 6.5 | 3.8 | 2.9 | 1.6 | 1.3 | 1.2 | 2.4 |
| North (Urban) | 91.5 | 3.5 | 7.6 | 8.2 | 9.8 | 26.3 | 8.1 | 2.2 | 2.8 | 2.1 | 1.7 | 2.9 | 3.2 |
| Northeast (Urban) | 109.1 | 3.7 | 9.5 | 10.7 | 13.3 | 33.8 | 8.2 | 3.6 | 2.7 | 2.1 | 1.8 | 2.0 | 2.3 |
| East (Urban) | 103.1 | 7.6 | 14.3 | 9.0 | 13.1 | 25.6 | 6.3 | 2.4 | 3.2 | 1.3 | 1.3 | 2.5 | 3.0 |
| Central (Urban) | 109.1 | 7.0 | 10.8 | 8.8 | 14.8 | 30.9 | 7.6 | 4.2 | 3.1 | 1.5 | 1.6 | 2.8 | 3.4 |
| South (Urban) | 104.6 | 3.6 | 5.5 | 10.4 | 19.6 | 28.2 | 7.3 | 3.1 | 3.9 | 1.0 | 1.1 | 2.9 | 3.3 |
| Southwest (Urban) | 98.3 | 5.5 | 7.2 | 8.7 | 14.0 | 29.5 | 5.2 | 3.9 | 3.2 | 0.9 | 1.3 | 2.2 | 3.9 |
| Northwest (Urban) | 110.0 | 9.9 | 19.0 | 8.1 | 14.6 | 23.8 | 7.3 | 3.8 | 3.3 | 1.8 | 1.4 | 1.3 | 2.4 |
| North (Rural) | 97.7 | 7.6 | 13.9 | 5.4 | 11.6 | 27.8 | 5.7 | 2.7 | 1.5 | 1.1 | 1.3 | 2.1 | 3.3 |
| Northeast (Rural) | 112.3 | 4.8 | 11.2 | 7.5 | 21.1 | 34.6 | 5.9 | 2.7 | 1.3 | 1.2 | 1.7 | 1.1 | 2.7 |
| East (Rural) | 112.4 | 13.5 | 17.2 | 6.7 | 16.8 | 28.0 | 5.3 | 3.0 | 2.2 | 0.8 | 1.1 | 2.3 | 3.0 |
| Central (Rural) | 115.1 | 13.5 | 17.2 | 6.8 | 17.5 | 30.1 | 6.7 | 4.8 | 1.4 | 0.8 | 1.0 | 2.2 | 3.0 |
| South (Rural) | 112.5 | 4.1 | 8.4 | 9.0 | 25.8 | 28.5 | 6.5 | 3.6 | 2.6 | 0.8 | 1.1 | 2.4 | 3.4 |
| Southwest (Rural) | 106.0 | 13.5 | 13.3 | 7.2 | 18.7 | 26.1 | 4.2 | 3.9 | 1.5 | 0.3 | 1.2 | 1.8 | 2.8 |
| Northwest (Rural) | 95.0 | 8.9 | 16.4 | 5.2 | 14.7 | 21.7 | 4.6 | 3.9 | 1.8 | 1.1 | 1.1 | 1.0 | 2.5 |
Age-specific incidence and mortality
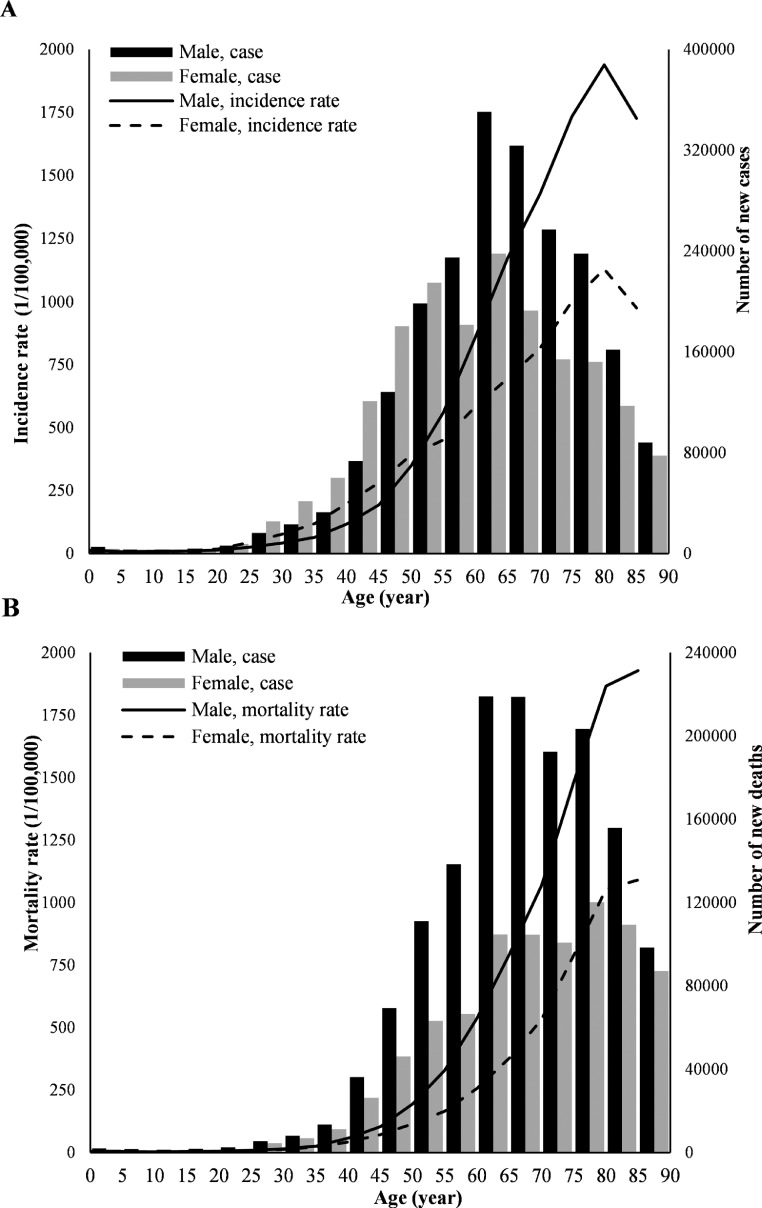
Cancer incidence rates increased with age. Cancer incidence rates in males between 0 −19 years and between 50–85+ were higher than that in females. Cancer incidence rates in females between 20 and 49 years were higher than that in males. The number of new cancer cases peaked at age group of 60–64 years both in males and females (Fig. 2A).
Fig. 2.
Age-specific cancer incidence and mortality by sex in China, 2015. (A) Age-specific cancer incidence rates and new cases by sex; (B) Age-specific cancer mortality rates and deaths by sex.
Cancer mortality rates increased with age. Cancer mortality rates in males were higher than that in females in all age groups. The number of deaths peaked at age group of 60–64 years in males and at age group of 75–79 years in females (Fig. 2B).
Trends in cancer incidence and mortality
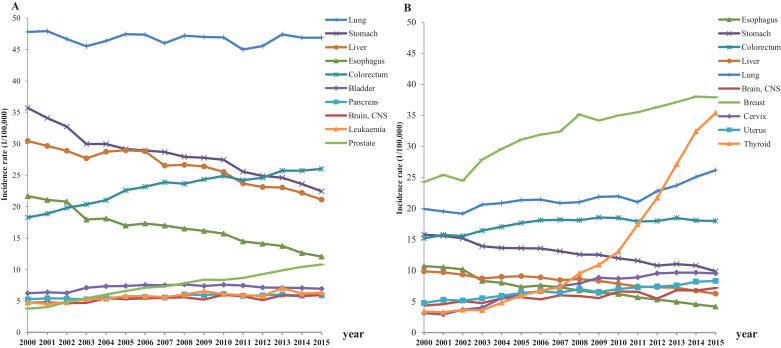
In males, the ASIRWs for esophageal cancer, gastric cancer and liver cancer decreased significantly from 2000 to 2015 (p < 0.05). The ASIRWs for colorectal cancer, pancreas cancer, prostate cancer, brain cancer and leukemia increased significantly (p < 0.05). The ASIRWs for lung cancer was stable over the years. The ASIRWs for bladder cancer increased from 2000 to 2006, but decreased from 2007 to 2015 (p < 0.05). In females, the ASIRWs for esophageal cancer, gastric cancer and liver cancer decreased significantly from 2000 to 2015 (p < 0.05). The ASIRWs for colorectal cancer, lung cancer, breast cancer, cervix cancer, uterus cancer, brain cancer and thyroid cancer increased significantly from 2000 to 2015 (p < 0.05) (Table 6, Fig. 3).
Table 6.
Trends of age-standardized incidence rates by world standard population (ASIRWs) for selected cancers in China, 2000 to 2015.
| ICD-10 | Site | Trend1 |
Trend2 |
Trend3 |
APC |
||||
|---|---|---|---|---|---|---|---|---|---|
| years | APC(95%CI) | years | APC(95%CI) | years | APC(95%CI) | 2000–2015 | 2010–2015 | ||
| Male | |||||||||
| C15 | Esophagus | 2000–2005 | −4.8*(−6.7~−2.8) | 2005–2009 | −1.2 (−5.7~3.4) | 2009–2015 | −4.9*(−6.3~−3.4) | −3.9*(−5.1~−2.6) | −4.9*(−6.3~−3.4) |
| C16 | Stomach | 2000–2003 | −5.5*(−6.9~−4.1) | 2003–2010 | −1.6*(−2.1~−1.1) | 2010–2015 | −3.6*(−4.3~−3.0) | −3.1*(−3.4~−2.7) | −3.6*(−4.3~−3.0) |
| C18–21 | Colorectum | 2000–2006 | 4.2*(3.4~5.0) | 2006–2015 | 1.2*(0.8~1.7) | – | – | 2.4*(2.1~2.8) | 1.2*(0.8~1.7) |
| C22 | Liver | 2000–2006 | −0.8 (−2.1~0.4) | 2006–2015 | −3.1*(−3.7~−2.4) | – | – | −2.2*(−2.7~−1.6) | −3.1*(−3.7~−2.4) |
| C25 | Pancreas | 2000–2015 | 0.9*(0.6~1.2) | – | – | – | – | 0.9*(0.6~1.2) | 0.9*(0.6~1.2) |
| C33-C34 | Lung | 2000–2015 | −0.1 (−0.3~0.1) | – | – | – | – | −0.1 (−0.3~0.1) | −0.1 (−0.3~0.1) |
| C61 | Prostate | 2000–2005 | 12.5*(10.7~14.3) | 2005–2015 | 4.8*(4.3~5.4) | – | – | 7.3*(6.7~7.9) | 4.8*(4.3~5.4) |
| C67 | Bladder | 2000–2006 | 3.8*(2.4~5.2) | 2006–2015 | −1.1*(−1.8~−0.4) | – | – | 0.9*(0.2~1.5) | −1.1*(−1.8~−0.4) |
| C70-C72 | Brain,CNS | 2000–2015 | 1.5*(0.9~2.1) | – | – | – | – | 1.5*(0.9~2.1) | 1.5*(0.9~2.1) |
| C91-C95 | Leukaemia | 2000–2015 | 2.2*(1.4~3.0) | – | – | – | – | 2.2*(1.4~3.0) | 2.2*(1.4~3.0) |
| Female | |||||||||
| C15 | Esophagus | 2000–2015 | −5.8*(−6.3~−5.3) | – | – | – | – | −5.8*(−6.3~−5.3) | −5.8*(−6.3~−5.3) |
| C16 | Stomach | 2000–2015 | −2.8*(−3.1~−2.6) | – | – | – | – | −2.8*(−3.1~−2.6) | −2.8*(−3.1~−2.6) |
| C18–21 | Colorectum | 2000–2006 | 3.3*(2.4~4.1) | 2006–2015 | −0.0 (−0.5~0.4) | – | – | 1.3*(0.9~1.6) | −0.0 (−0.5~0.4) |
| C22 | Liver | 2000–2009 | −1.7*(−2.5~−1.0) | 2009–2015 | −4.3*(−5.6~−2.9) | – | – | −2.7*(−3.4~−2.1) | −4.3*(−5.6~−2.9) |
| C33-C34 | Lung | 2000–2011 | 0.9*(0.5~1.4) | 2011–2015 | 4.6*(2.3~6.9) | – | – | 1.9*(1.3~2.5) | 4.6*(2.3~6.9) |
| C50 | Breast | 2000–2006 | 5.3*(3.8~6.9) | 2006–2015 | 1.9*(1.1~2.7) | – | – | 3.3*(2.6~4.0) | 1.9*(1.1~2.7) |
| C53 | Cervix | 2000–2007 | 16.0*(12.8~19.2) | 2007–2015 | 3.0*(0.7~5.4) | – | – | 8.9*(7.2~10.6) | 3.0*(0.7~5.4) |
| C54–55 | Uterus | 2000–2005 | 5.4*(2.9~7.9) | 2005–2015 | 2.7*(1.9~3.6) | – | – | 3.6*(2.7~4.5) | 2.7*(1.9~3.6) |
| C70-C72 | Brain,CNS | 2000–2015 | 2.9*(2.1~3.7) | – | – | – | – | 2.9*(2.1~3.7) | 2.9*(2.1~3.7) |
| C73 | Thyroid | 2000–2003 | 3.9 (−6.4~15.3) | 2003–2015 | 21.1*(19.6~22.6) | – | – | 17.5*(15.1~19.9) | 21.1*(19.6~22.6) |
APC, annual percentage change; CNS, central nervous system; ICD-10, International Classification of Diseases 10th revision.
The difference is statistically significant (p < 0.05).
Fig. 3.
Trends of age-standardized incidence rates by world standard population (Segi's population) for selected cancers in China, 2000 to 2015; (A) Males; (B) Females.
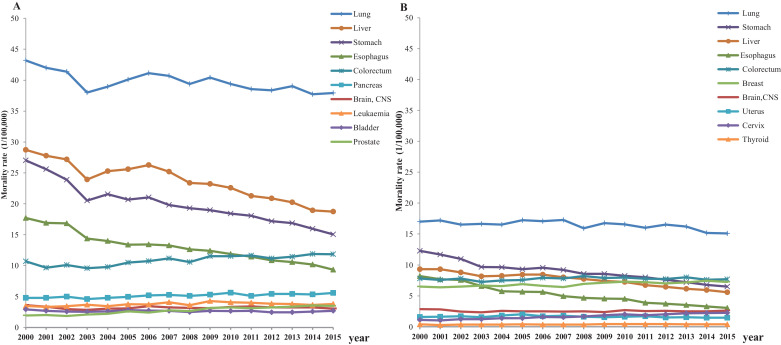
In males, the ASMRWs for esophageal cancer, gastric cancer, liver cancer and lung cancer decreased significantly from 2000 to 2015 (p < 0.05). The ASMRWs for colorectal cancer, pancreas cancer and prostate cancer increased significantly (p < 0.05). The ASMRWs for bladder cancer, brain cancer and leukemia cancer were stable over the years. In females, the ASMRWs for esophageal cancer, gastric cancer, liver cancer and lung cancer decreased significantly from 2000 to 2015 (p < 0.05). The ASMRWs for breast cancer, cervix cancer and thyroid cancer increased significantly (p < 0.05). The ASMRWs for colorectal cancer, uterus cancer and brain cancer were stable over the years (Table 7, Fig. 4).
Table 7.
Trends for age-standardized mortality rates by world standard population (ASMRWs) for selected cancers in China, 2000 to 2015.
| ICD-10 | Site | Trend1 |
Trend2 |
Trend3 |
APC |
||||
|---|---|---|---|---|---|---|---|---|---|
| years | APC(95%CI) | years | APC(95%CI) | years | APC(95%CI) | 2000–2015 | 2010–2015 | ||
| Male | |||||||||
| C15 | Esophagus | 2000–2003 | −6.2*(−9.7~−2.6) | 2003–2015 | −3.4*(−3.9~−3.0) | – | – | −4.0*(-4.7~−3.3) | −3.4*(−3.9~−3.0) |
| C16 | Stomach | 2000–2003 | −8.3*(−10.8~−5.7) | 2003–2006 | −0.6 (−5.9~5.1) | 2006–2015 | −3.3*(−3.8~−2.8) | −3.8*(−4.8~−2.7) | −3.3*(−3.8~−2.8) |
| C18–21 | Colorectum | 2000–2015 | 1.3*(0.8~1.8) | – | – | – | – | 1.3*(0.8~1.8) | 1.3*(0.8~1.8) |
| C22 | Liver | 2000–2003 | −5.4*(−7.7~−3.1) | 2003–2006 | 1.6 (−3.1~6.6) | 2006–2015 | −3.7*(−4.1~−3.2) | −3.0*(−3.9~−2.1) | −3.7*(−4.1~−3.2) |
| C25 | Pancreas | 2000–2015 | 1.1*(0.7~1.5) | – | – | – | – | 1.1*(0.7~1.5) | 1.1*(0.7~1.5) |
| C33-C34 | Lung | 2000–2003 | −4.1*(−6.1~−2.1) | 2003–2006 | 1.9 (−2.2~6.3) | 2006–2015 | −0.9*(−1.3~−0.5) | −1.0*(−1.8~−0.2) | −0.9*(−1.3~−0.5) |
| C61 | Prostate | 2000–2015 | 4.7*(4.0~5.5) | – | – | – | – | 4.7*(4.0~5.5) | 4.7*(4.0~5.5) |
| C67 | Bladder | 2000–2015 | −0.4 (−0.9~0.1) | – | – | – | – | −0.4 (−0.9~0.1) | −0.4 (−0.9~0.1) |
| C70-C72 | Brain,CNS | 2000–2003 | −7.6*(−12.2~−2.8) | 2003–2006 | 5.4 (−4.9~16.8) | 2006–2015 | −0.4 (−1.4~0.5) | −0.8 (−2.8~1.2) | −0.4 (−1.4~0.5) |
| C91-C95 | Leukaemia | 2000–2010 | 2.0*(0.8~3.1) | 2010–2015 | −2.1 (−5.2~1.2) | – | – | 0.6 (−0.6~1.8) | −2.1 (−5.2~1.2) |
| Female | |||||||||
| C15 | Esophagus | 2000–2015 | −6.3*(−6.7~−5.9) | – | – | – | – | −6.3*(−6.7~−5.9) | −6.3*(−6.7~−5.9) |
| C16 | Stomach | 2000–2003 | −7.3*(−10.1~−4.6) | 2003–2010 | −2.4*(−3.4~−1.5) | 2010–2015 | −4.9*(−6.2~−3.7) | −4.3*(−5.0~−3.6) | −4.9*(−6.2~−3.7) |
| C18–21 | Colorectum | 2000–2003 | −2.0 (−5.1~1.2) | 2003–2008 | 1.8 (−0.2~3.9) | 2008–2015 | −0.7 (−1.6~0.1) | −0.2 (−1.0~0.7) | −0.7 (−1.6~0.1) |
| C22 | Liver | 2000–2003 | −4.6*(−6.8~−2.3) | 2003–2006 | 0.8 (−3.9~5.7) | 2006–2015 | −4.4*(−4.8~−4.0) | −3.4*(−4.3~−2.5) | −4.4*(−4.8~−4.0) |
| C33-C34 | Lung | 2000–2015 | −0.6*(−1.0~−0.3) | – | – | – | – | −0.6*(−1.0~−0.3) | −0.6*(−1.0~−0.3) |
| C50 | Breast | 2000–2015 | 1.0*(0.7~1.3) | – | – | – | – | 1.0*(0.7~1.3) | 1.0*(0.7~1.3) |
| C53 | Cervix | 2000–2015 | 5.4*(4.8~6.0) | – | – | – | – | 5.4*(4.8~6.0) | 5.4*(4.8~6.0) |
| C54–55 | Uterus | 2000–2005 | 3.3*(0.3~6.4) | 2005–2015 | −2.3*(−3.3~−1.3) | – | – | −0.4 (−1.5~0.6) | −2.3*(−3.3~−1.3) |
| C70-C72 | Brain,CNS | 2000–2003 | −5.5*(−10.4~−0.2) | 2003–2015 | 0.5 (−0.1~1.1) | – | – | −0.7 (−1.8~0.3) | 0.5 (−0.1~1.1) |
| C73 | Thyroid | 2000–2015 | 1.4*(0.3~2.5) | – | – | – | – | 1.4*(0.3~2.5) | 1.4*(0.3~2.5) |
APC, annual percentage change; CNS, central nervous system; ICD-10, International Classification of Diseases 10th revision.
The difference is statistically significant (p < 0.05).
Fig. 4.
Trends of age-standardized mortality rates by world standard population (Segi's population) for Selected Cancers in China, 2000 to 2015; (A) Males; (B) Females.
Discussion
In this paper, we reported the overview of cancer burden in China in 2015 using qualified cancer registry data. Cancer incidence was higher in urban areas than in rural areas. Lung cancer and female breast cancer was the most common cancer in males and females respectively. Cancer mortality was higher in rural areas than in urban areas. Lung cancer was the most common cause of cancer deaths in both males and females. Cancer incidence and mortality showed differences in rates between urban and rural areas, across geographic areas and those differences may primarily be attributable to differences in exposures to carcinogens, lifestyle, or different health resource, and also may partially be attributable to differences in registry quality, urbanicity.6
In China, cancer has become a major public health problem. Compared with previous data in 20147, the crude incidence and mortality rates of all cancer combined in 2015 in China increased slightly. Although we observed a decrease of the incidence of infection-related and poverty-related cancers, such as stomach cancer, esophageal cancer, liver caner, et al., and the disease burden of cancers related to westernization of lifestyle kept growing rapidly, such as colorectum cancer, breast cancer, et al. Aging of the Chinese population and socioeconomic development caused by the rapid process of urbanization may be responsible for the growth of cancer disease burden and the changing cancer profile. Cancer mortality rate reflected the development of health care system. We were delighted to see decreases in mortality rates of cancers with traditionally high incidence rates and bad prognosis, such as esophageal cancer, gastric cancer, liver cancer and lung cancer. However, the mortality rates of other cancers, such as colorectal cancer, prostate cancer and breast cancer, were still rising.
GLOBOCAN 2018 estimated that 307,000 cases and 283,000 deaths of esophageal cancer occurred in China, accounting for 53.7% and 55.7% of all esophageal cancer cases and deaths in the world. About 456,000 cases and 390,000 deaths of gastric cancer occurred in China, accounting for 44.1% and 49.9% of all gastric cancer cases and deaths in the whole world.8 In the present study, the number of cases and deaths of both cancers in 2015 were lower than GLOBOCAN's estimation. Considering the decreasing trend of incidence and mortality and increasing trend of survival rate of both cancers9, the actual disease burden of upper gastrointestinal cancers will be lower than GLOBOCAN's estimation in 2018. One possible reason for this difference was that many registry data GLOBOCAN used came from high risk areas of upper gastrointestinal cancers. A previous publication on Cancer statistics in China in 2015 have been published by Chen W et al.1, but the result was predicted with data in 2009 to 2011 from 72 cancer registries, and the estimation are higher compared with this study due to the most registries were in high incidence areas, while 368 cancer registries’ data with larger population coverage and better representativeness were used for this study.
In recent years, effective primary and secondary prevention measures were implemented in China. In China, over 50% cancer deaths can attribute to all modifiable risk factors such as smoking, drinking, high calorie food intake, sedentary lifestyle, diabetes, chronic infectious agents and so on.10,11,12 On the bright side, we observed a significant decrease of the infection-related cancers, which was closely related to the remarkable achievement of the prevention and control of chronic infectious diseases in the last decades. For example, China has adopted several measures to control HBV13, including plasma-derived vaccine in 1985 and recombinant vaccine in 1992.14 HBV vaccination for infants became free since it was introduced into China's National Expanded Programme on Immunization (EPI) in 2002.15 The national hepatitis sero-survey in 2006 indicated that the prevalence of HBsAg was greatly reduced among children less than 15 years old.16 The first human papillomavirus (HPV) vaccine licensed for use has launched in China in 2017. It is expected that the infection-related cancer incidence will continue to diminish in the near future.
PM2.5 accounts for 23.9% of lung cancer deaths in China17, which is much higher than the global level of 16.5%.18 Marked decline (29%) of air pollution level in China in 2030 is needed to maintain the mortality at 2010 level.19 Aggressive policy action against air pollution is the most effective way to lower the disease burden of entire population. The energy conservation and emissions reduction (ECER) policy was implemented in late 2006 in China, which required a 20% reduction in energy usage by the year 2010. The overall reduction achieved was 19.06%.20 In 2013, Chinese government issued the Air Pollution Prevention and Control Action Plan (APPCAP). This milestone policy yielded substantial reduction in mortality related to ambient air pollution.21 However, pollution control does not happen overnight. There is still a long way to go for Chinese government to realize its commitment to environmental conservation.
China is both the largest producer and consumer of tobacco worldwide.22 The prevalence of current smoking and second-hand smoking were still high.23,24 During the past 15 years, lung cancer incidence in males maintained at high level while lung cancer incidence zoomed up in females. Chinese government has committed to achieve 100% smoke-free environments in public places in the document of The Outline of the 12th 5-year Plan for National Economic and Social Development. However, only a few cities adopted smoke-free legislations.25 China needs to set up comprehensive and effective national smoke-free laws to substantially reduce smoking in public places. Despite the existing national nutrition and fitness policies, the prevalence of overweight and obesity kept increasing significantly in Chinese adults and children26,27, and this may lead the increase of the incidence of colorectum cancer, breast cancer et al. in the future . More efforts should be put into promoting balanced diet and physical activities to combat the upcoming obesity endemic.
Cancer secondary prevention measures have also yielded significant benefits in China. Cancer screening programs in China firstly initiated in traditional high-risk areas. For example, screening for esophageal cancer in Lin county of Henan province started in 1950s.28 Screening for liver cancer in Qidong county of Jiangsu province started in 1970s.29 In 2005, China rural cancer early diagnosis and treatment program was initiated to prevent cancers in high risk areas on a large scale, providing screening services for upper gastrointestinal cancers in 194 counties, for colorectal cancers in 33 counties, for liver cancer in 13 counties, for lung cancer in 11 counties and for nasopharyngeal cancer in 8 counties. In 2007, Huaihe valley cancer early diagnosis and treatment program was initiated, providing screening services for upper gastrointestinal cancer and liver cancer. To expand the coverage of cancer screening programs in cities, China urban cancer early diagnosis and treatment program was initiated in 2012, providing screening services for lung cancer, colorectal cancer, upper gastrointestinal cancer, female breast cancer and liver cancer. This program now covered 42 cities in 20 provinces.
However, we should realize that the population coverage of the existing screening programs was still low. Considering the actual conditions of China, it is unrealistic to implement national cancer screening programs. Providing cancer screening services with universal coverage in high risk areas and encouraging opportunistic screening in non-high-risk areas might be the most efficient solution in the future.
The key strength of this study is the most representative and high-quality data in China, including the cancer incidence and mortality with 368 cancer registries covered about 22% of the national population, and this is the most representative data that can be obtained. Unfortunately, more information such as survival rate, stage at diagnosis are not yet available in this study, but the result should also be useful for studies of international comparisons of cancer rates. Although there may still have some unknown level of uncertainty in this estimation, the results may be more reasonable compared with previous estimates.1
In the next decade, the cancer burden may still increase in China and the cancer profile will contain both the features of developing country and developed country. Our country has issued a series of health policies to prioritize the promotion of cancer control, including the blueprint guide of “healthy China 2030”, 13th 5-year Plan for Medical and Health Service Development and China's Medium-Long Term Plan for Noncommunicable Chronic Diseases Prevention and Control (2017–2025). What's more, the state council has established the inter-ministerial joint conference system to prevent and control major chronic diseases. The nationwide cancer surveillance and follow-up network has been established, including 20 provincial cancer centers and 574 cancer registries. These methods will dampen the growth of cancer disease burden and lead to a healthier China.
Declaration of Competing Interest
The authors declare that they have no conflict of interests.
Acknowledgements
We thank the Bureau of Disease Control, National Health Commission of the People's Republic of China for their support of this study. We sincerely acknowledge staffs of population-based cancer registries for the effort they put in data collection and data quality control. The authors take full responsibility for data analysis and result interpretation of this paper. This study is supported by CAMS Innovation Fund for Medical Sciences (2018-I2M-3–003); National Key R&D Program of China (2018YFC1311704).
Footnotes
Given their roles as Editor in Chief and Editor, respectively, Jie He and Wenqiang Wei had no involvement in the peer-review of this article and had no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Huan He.
Supplementary material associated with this article can be found in the online version, at doi:10.1016/j.jncc.2020.12.001.
Contributor Information
Wenqiang Wei, Email: weiwq@cicams.ac.cn.
Jie He, Email: prof.hejie@263.net.
Appendix. Supplementary materials
References
- 1.Chen W., Zheng R., Baade P.D., et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 2.National Cancer Center . People’s Medical Publishing House; Beijing, China: 2016. Chinese Guideline for Cancer Registration [in Chinese] [Google Scholar]
- 3.Bray F., Parkin D.M. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45(5):747–755. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 4.Parkin D.M., Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45(5):756–764. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Bray F., Guilloux A., Sankila R., et al. Practical implications of imposing a new world standard population. Cancer Causes Control. 2002;13(2):175–182. doi: 10.1023/a:1014344519276. [DOI] [PubMed] [Google Scholar]
- 6.Chen W., Xia C., Zheng R., et al. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health. 2019;7(2):e257–e269. doi: 10.1016/s2214-109x(18)30488-1. [DOI] [PubMed] [Google Scholar]
- 7.Chen W., Sun K., Zheng R., et al. Cancer incidence and mortality in China, 2014. Chin J Cancer Res. 2018;30(1):1–12. doi: 10.21147/j.issn.1000-9604.2018.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bray F., Ferlay J., Soerjomataram I., et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 9.Zeng H., Chen W., Zheng R., et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6(5):e555–e567. doi: 10.1016/s2214-109x(18)30127-x. [DOI] [PubMed] [Google Scholar]
- 10.Islami F., Chen W., Yu X.Q., et al. Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol. 2017;28(10):2567–2574. doi: 10.1093/annonc/mdx342. [DOI] [PubMed] [Google Scholar]
- 11.Cogliano V.J., Baan R., Straif K., et al. Preventable exposures associated with human cancers. J Natl Cancer Inst. 2011;103(24):1827–1839. doi: 10.1093/jnci/djr483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Cancer Research Fund/American Institute for Cancer Research . World Cancer Research Fund/American Institute for Cancer Research 2018; Washington DC: 2018. Diet, nutrition, physical activity and cancer: A global perspective. Continuous update project expert report 2018. [Google Scholar]
- 13.Qu C., Chen T., Fan C., et al. Efficacy of neonatal HBV vaccination on liver cancer and other liver diseases over 30-year follow-up of the Qidong hepatitis B intervention study: a cluster randomized controlled trial. PLoS Med. 2014;11(12) doi: 10.1371/journal.pmed.1001774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goyal A., Murray J.M. Roadmap to control HBV and HDV epidemics in China. J Theor Biol. 2017;423:41–52. doi: 10.1016/j.jtbi.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Lu S.Q., McGhee S.M., Xie X., et al. Economic evaluation of universal newborn hepatitis B vaccination in China. Vaccine. 2013;31(14):1864–1869. doi: 10.1016/j.vaccine.2013.01.020. [DOI] [PubMed] [Google Scholar]
- 16.Liang X., Bi S., Yang W., et al. Epidemiological serosurvey of hepatitis B in China–declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009;27(47):6550–6557. doi: 10.1016/j.vaccine.2009.08.048. [DOI] [PubMed] [Google Scholar]
- 17.Song C., He J., Wu L., et al. Health burden attributable to ambient PM(2.5) in China. Environ Pollut. 2017;223:575–586. doi: 10.1016/j.envpol.2017.01.060. [DOI] [PubMed] [Google Scholar]
- 18.Cohen A.J., Brauer M., Burnett R., et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–1918. doi: 10.1016/s0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Apte J.S., Marshall J.D., Cohen A.J., et al. Addressing Global Mortality from Ambient PM2.5. Environ Sci Technol. 2015;49(13):8057–8066. doi: 10.1021/acs.est.5b01236. [DOI] [PubMed] [Google Scholar]
- 20.Lo K., Wang M.Y. Energy conservation in China’s Twelfth Five-Year Plan period: Continuation or paradigm shift? Renew Sust Energ Rev. 2013;18:499–507. doi: 10.1016/j.rser.2012.10.042. [DOI] [Google Scholar]
- 21.Huang J., Pan X., Guo X., et al. Health impact of China’s Air Pollution Prevention and Control Action Plan: an analysis of national air quality monitoring and mortality data. Lancet Planet Health. 2018;2(7):e313–e323. doi: 10.1016/s2542-5196(18)30141-4. [DOI] [PubMed] [Google Scholar]
- 22.Eriksen M., Mackay J., Rose H. 4th ed. American Cancer Society; Atlanta, Georgia: 2012. The Tobacco Atlas. [Google Scholar]
- 23.Li S., Meng L., Chiolero A., et al. Trends in smoking prevalence and attributable mortality in China, 1991-2011. Prev Med. 2016;93:82–87. doi: 10.1016/j.ypmed.2016.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiao L., Yang Y., Li Q., et al. Population-based survey of secondhand smoke exposure in China. Biomed Environ Sci. 2010;23(6):430–436. doi: 10.1016/s0895-3988(11)60003-2. [DOI] [PubMed] [Google Scholar]
- 25.Aresh Azizi A. Is this the end of the beginning for smoking in China? Challenges, context and change. Glob Health Promot. 2017;24(3):79–83. doi: 10.1177/1757975915623734. [DOI] [PubMed] [Google Scholar]
- 26.Jiang Y., Xu Y., Bi Y., et al. Prevalence and trends in overweight and obesity among Chinese adults in 2004–10: data from three nationwide surveys in China. The Lancet. 2015;386(Supplement 1):S77. doi: 10.1016/S0140-6736(15)00658-3. [DOI] [Google Scholar]
- 27.Jia P., Xue H., Zhang J., et al. Time trend and demographic and geographic disparities in childhood obesity prevalence in China-evidence from twenty years of longitudinal data. Int J Environ Res Public Health. 2017;14(4) doi: 10.3390/ijerph14040369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang C.S. Research on esophageal cancer in China: a review. Cancer Res. 1980;40(8 Pt 1):2633–2644. [PubMed] [Google Scholar]
- 29.Zhou X.D., Tang Z.Y., Yang B.H., et al. Hepatocellular Carcinoma: The Role of Screening. Asian Pac J Cancer Prev. 2000;1(2):121–126. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.