Abstract
Background
The National Cancer Center (NCC) of China regularly reports the nationwide statistics on cancer incidence and mortality in China. The International Agency for Research on Cancer (IARC) calculates and publishes the cancer burden of countries around the world every two years. To ensure consistency between the actual surveillance data in China and the data published by IARC, NCC has received approval from the National Health Commission and IARC to simultaneously release the cancer burden data for China in GLOBOCAN 2022.
Methods
There were a total of 700 registries reporting high-quality data on cancer incidence and mortality across China in 2018, of which 106 registries with continuous monitoring from 2010 to 2018 were used to establish an age-period-cohort model to simulate the trend of cancer incidence and mortality and to estimate the incidence and mortality in China in 2022. In addition, we analyzed the temporal trends of age-standardized cancer incidence and mortality from 2000 to 2018 using data from 22 continuous cancer registries.
Results
It was estimated about 4,824,700 new cancer cases and 2,574,200 new cancer deaths occurred in China in 2022. Cancers of the lung, colon-rectum, thyroid, liver and stomach were the top five cancer types, accounting for 57.42% of new cancer cases. Cancers of the lung, liver, stomach, colon-rectum and esophagus were the five leading causes of cancer deaths, accounting for 67.50% of total cancer deaths. The crude rate and age-standardized incidence rate (ASIR) were 341.75 per 100,000 and 201.61 per 100,000, respectively. The crude mortality rate was 182.34 per 100,000 and the age-standardized mortality rate (ASMR) was 96.47 per 100,000. The ASIR of all cancers combined increased by approximately 1.4% per year during 2000–2018, while the ASMR decreased by approximately 1.3% per year. We observed decreasing trends in ASIR and ASMR for cancers of the esophagus, stomach, and liver, whereas the ASIR increased significantly for cancers of the thyroid, prostate, and cervix.
Conclusions
Cancer remains a major public health concern in China, with a cancer profile that reflects the coexistence of developed and developing regions. Sustained implementation of prevention and control measures has resulted in significant reductions in the incidence and mortality rates of certain historically high incidence cancers, such as esophageal, stomach and liver cancers. Adherence to the guidelines of the Healthy China Action Plan and the Cancer Prevention and Control Action Plan, along with continued efforts in comprehensive risk factor control, cancer screening, early diagnosis and treatment, and standardization of diagnostic and therapeutic protocols, are key strategies to effectively mitigate the increasing cancer burden by 2030.
Keywords: Cancer registry, Incidence, Mortality, Statistics, China
1. Introduction
Cancer has become a major public health problem in China, seriously affecting the health of Chinese residents, the national economy and the social development. Cancer registries can be used for continuous and dynamic monitoring of cancer incidence and mortality. Population-based cancer registries have been in operation in China for about 60 years.1 Cancer incidence, mortality and survival data provide scientific evidence to develop cancer prevention and control strategies, and to evaluate the effectiveness of the quality of medical and health work. China has already established a cancer surveillance system, and basically achieved a full coverage of all districts/counties. The cancer registration has greatly improved the cancer prevention and control in China. The National Cancer Center (NCC) is responsible for data collection and quality control, including the assessment of the validity, completeness and comparability of all cancer registry data based on the criteria of the “Guideline for Chinese Cancer Registration”2 and the criteria of the International Agency for Research on Cancer/International Association of Cancer Registries (IARC/IACR).3,4
In 2024, the IARC is preparing to release the GLOBOCAN 2022 report. Prior to this, the NCC collaborated with IARC to estimate the cancer incidence and mortality data in this report with the actual and updated surveillance data in China, to ensure the consistency of the cancer burden in China released by IACR and NCC. This study provided the latest estimated statistics of new cancer incidence and mortality in China in 2022. We further updated the trends of cancer incidence and mortality from 2000 to 2018. These results can provide scientific evidence for cancer prevention and control in China.
2. Materials and methods
2.1. Data source
Both incidence and mortality data used in calculations originated in cancer registries. After data quality control (including assessment of validity, completeness, and comparability), a total of 700 cancer registries from 31 provinces (autonomous regions and municipalities) and Xinjiang Production and Construction Corps submitted qualified data of 2018 to NCC. A total of 523 million people were covered in those registries, accounting for 37.22% of the total population in China in 2018. All diagnosed cancer cases were coded according to the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) and the International Statistical Classification of Diseases 10th Revision (ICD-10).
Temporal trends in age-standardized rates by world standard population from 2000 to 2018 for cancer incidence and mortality of all cancers and selected cancer types were analyzed using data from 22 continuous cancer registries representing 3.34% of the Chinese population (Supplementary Table 1). More details about these registries have been reported in a previous study.5
The National Bureau of Statistics of China provided the total number of population of China in 2022, stratified by area (urban/rural) and sex. The age-specific population of 2022 was estimated according to the population structure of the data of the seventh National Census, which provided the data of the total population in groups (0–84 by 5 years and 85+ years).
2.2. Statistical analysis
We fitted the Bayesian age-period-cohort model based on data of 106 registries from 2010 to 2018 to obtain the age-specific (0–84 by 5 years and 85+ years) annual percentage changes by urban and rural areas, sex, and cancer sites, and estimated the predicted age-specific incidence and mortality rates for 2022. Then we calculated the age-specific numbers of new cases and deaths with the incidence and mortality rates combining the population of 2022. To correct the deviation of the modeling results, we used registration data from 700 cancer registries in 2018. We used the weights of the Segi's population for calculating age-standardized rates (Supplementary Table 2). The Joinpoint Regression Program (version 4.6.0.0) was used to calculate the annual percentage change (APC). We set a maximum of two Joinpoints and reported the average annual percentage change (AAPC) for three fixed intervals (2000–2018, 2009–2018 and 2014–2018). SAS software (Version 9.4, SAS Institute Inc., Cary, USA) was used for statistical analysis.
3. Results
3.1. Estimated numbers of new cancer cases and cancer incidence rates
Table 1 shows the estimated number of new cancer cases in China in 2022. Overall, an estimated number of 4,824,700 new cancer cases (2,533,900 males and 2,290,800 females) occurred in 2022. The crude incidence rate for all cancer sites was 341.75 per 100,000 in 2022 (351.44 per 100,000 in males, and 331.64 per 100,000 in females). The age-standardized incidence rate (ASIR) was 201.61 per 100,000.
Table 1.
Estimated numbers of new cancer cases and cancer incidence rates in China in 2022.
| Cancer sites | ICD-10 | All |
Male |
Female |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases (×104) |
Crude rate (1/105) |
ASIR (1/105) |
Cases (×104) |
Crude rate (1/105) |
ASIR (1/105) |
Cases (×104) |
Crude rate (1/105) |
ASIR (1/105) |
||
| Lip, oral cavity & pharynx | C00–10, 12–13 | 6.51 | 4.61 | 2.72 | 4.56 | 6.33 | 3.87 | 1.95 | 2.82 | 1.60 |
| Nasopharynx | C11 | 5.10 | 3.61 | 2.36 | 3.67 | 5.08 | 3.39 | 1.44 | 2.08 | 1.33 |
| Esophagus | C15 | 22.40 | 15.87 | 8.32 | 16.75 | 23.23 | 13.09 | 5.65 | 8.19 | 3.78 |
| Stomach | C16 | 35.87 | 25.41 | 13.72 | 24.66 | 34.20 | 19.47 | 11.21 | 16.23 | 8.29 |
| Colon-rectum | C18–21 | 51.71 | 36.63 | 20.10 | 30.77 | 42.67 | 24.74 | 20.94 | 30.32 | 15.70 |
| Liver | C22 | 36.77 | 26.04 | 15.03 | 26.79 | 37.16 | 22.72 | 9.98 | 14.44 | 7.42 |
| Gallbladder | C23 | 3.11 | 2.21 | 1.14 | 1.27 | 1.76 | 0.97 | 1.85 | 2.67 | 1.30 |
| Pancreas | C25 | 11.87 | 8.41 | 4.44 | 6.71 | 9.31 | 5.29 | 5.15 | 7.46 | 3.63 |
| Larynx | C32 | 2.95 | 2.09 | 1.16 | 2.72 | 3.77 | 2.19 | 0.23 | 0.33 | 0.17 |
| Lung | C33–34 | 106.06 | 75.13 | 40.78 | 65.87 | 91.36 | 52.03 | 40.19 | 58.18 | 30.34 |
| Melanoma of skin | C43 | 0.88 | 0.62 | 0.37 | 0.44 | 0.61 | 0.37 | 0.44 | 0.64 | 0.36 |
| Female breast | C50 | 35.72 | 51.71 | 33.04 | – | – | – | 35.72 | 51.71 | 33.04 |
| Cervix | C53 | 15.07 | 21.81 | 13.83 | – | – | – | 15.07 | 21.81 | 13.83 |
| Uterus | C54 | 7.77 | 11.25 | 6.84 | – | – | – | 7.77 | 11.25 | 6.84 |
| Ovary | C56 | 6.11 | 8.84 | 5.68 | – | – | – | 6.11 | 8.84 | 5.68 |
| Prostate | C61 | 13.42 | 18.61 | 9.68 | 13.42 | 18.61 | 9.68 | – | – | – |
| Testis | C62 | 0.35 | 0.48 | 0.41 | 0.35 | 0.48 | 0.41 | – | – | – |
| Kidney | C64 | 7.37 | 5.22 | 3.13 | 4.73 | 6.56 | 4.08 | 2.64 | 3.81 | 2.21 |
| Bladder | C67 | 9.29 | 6.58 | 3.44 | 7.32 | 10.15 | 5.67 | 1.97 | 2.85 | 1.39 |
| Brain, CNS | C70–72 | 8.75 | 6.20 | 4.17 | 4.24 | 5.88 | 4.13 | 4.51 | 6.53 | 4.20 |
| Thyroid | C73 | 46.61 | 33.02 | 24.64 | 12.49 | 17.32 | 13.25 | 34.12 | 49.40 | 36.51 |
| Lymphoma | C81–86, 88 | 8.52 | 6.03 | 3.77 | 4.81 | 6.68 | 4.34 | 3.71 | 5.36 | 3.21 |
| Leukemia | C91–95 | 8.19 | 5.80 | 4.54 | 4.70 | 6.52 | 5.14 | 3.50 | 5.06 | 3.94 |
| All other sites⁎ | Other | 31.69 | 22.45 | 13.31 | 16.73 | 23.20 | 14.42 | 14.96 | 21.66 | 12.28 |
| All sites⁎ | All | 482.47 | 341.75 | 201.61 | 253.39 | 351.44 | 209.61 | 229.08 | 331.64 | 197.03 |
Non-melanoma skin cancer (C44) was included.
Abbreviations: ASIR, age-standardized incidence rate by world standard population (Segi's population); CNS, central nervous system; ICD-10, International Statistical Classification of Diseases and Related Health Problems 10th Revision.
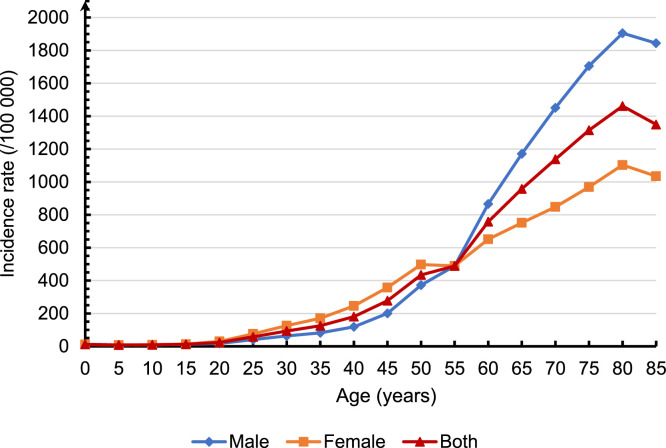
The incidence rate for all cancer sites was relatively low in the age group of 0–34 years, and dramatically increased from age group 35–39 years old (125.24 per 100,000), and peaked in the age group 80–84 years (1,461.63 per 100,000). Overall incidence rates for males were lower than those for females in the 25–54 age group and higher after 60 years of age (Fig. 1).
Fig. 1.
Estimated age-specific incidence rates for all cancers combined in China in 2022.
3.2. Leading causes of new cancer cases in China in 2022
Lung cancer was the most common cancer in China in 2022 (1,060,600 cases), followed by colorectal cancer (517,100 cases), thyroid cancer (466,100 cases), liver cancer (367,700 cases), and stomach cancer (358,700 cases), accounting for 57.42% of total new cancer cases. The top 5 cancers in males were lung cancer, colorectal cancer, liver cancer, stomach cancer and esophageal cancer, accounting for 65.05% of total new cancer cases in males. The most common cancer in females was lung cancer, followed by breast cancer, thyroid cancer, colorectal cancer, and cervical cancer, accounting for 63.75% of total new cancer cases in females (Table 1).
3.3. Estimated numbers of cancer deaths and cancer mortality rates
Table 2 shows the estimated number of cancer deaths in China in 2022. Overall, the estimated number of cancer deaths in 2022 was 2,574,200 (1,629,300 males and 944,900 females). The crude mortality rate for all cancer sites in 2022 was 182.34 per 100,000 (225.97 per 100,000 in males, and 136.79 per 100,000 in females). The age-standardized mortality rate (ASMR) was 96.47 per 100,000. The crude mortality rate and ASMR of all cancer sites were higher in males than those in females.
Table 2.
Estimated numbers of cancer deaths and cancer mortality rates in China in 2022.
| Cancer sites | ICD-10 | All |
Male |
Female |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deaths (×104) |
Crude rate (1/105) |
ASMR (1/105) |
Deaths (×104) |
Crude rate (1/105) |
ASMR (1/105) |
Deaths (×104) |
Crude rate (1/105) |
ASMR (1/105) |
||
| Lip, oral cavity & pharynx | C00–10, 12–13 | 3.52 | 2.49 | 1.33 | 2.58 | 3.58 | 2.06 | 0.94 | 1.35 | 0.63 |
| Nasopharynx | C11 | 2.84 | 2.01 | 1.18 | 2.13 | 2.95 | 1.81 | 0.71 | 1.03 | 0.56 |
| Esophagus | C15 | 18.75 | 13.28 | 6.68 | 14.04 | 19.47 | 10.70 | 4.71 | 6.82 | 2.92 |
| Stomach | C16 | 26.04 | 18.44 | 9.39 | 18.16 | 25.18 | 13.77 | 7.88 | 11.41 | 5.34 |
| Colon-rectum | C18–21 | 24.00 | 17.00 | 8.56 | 14.26 | 19.78 | 10.85 | 9.74 | 14.10 | 6.48 |
| Liver | C22 | 31.65 | 22.42 | 12.59 | 22.98 | 31.87 | 19.14 | 8.68 | 12.56 | 6.15 |
| Gallbladder | C23 | 2.45 | 1.74 | 0.87 | 0.98 | 1.36 | 0.74 | 1.47 | 2.13 | 0.99 |
| Pancreas | C25 | 10.63 | 7.53 | 3.88 | 6.11 | 8.47 | 4.73 | 4.52 | 6.55 | 3.06 |
| Larynx | C32 | 1.69 | 1.19 | 0.62 | 1.50 | 2.08 | 1.16 | 0.18 | 0.26 | 0.12 |
| Lung | C33–34 | 73.33 | 51.94 | 26.66 | 51.59 | 71.55 | 39.51 | 21.74 | 31.47 | 14.71 |
| Melanoma of skin | C43 | 0.54 | 0.38 | 0.20 | 0.29 | 0.40 | 0.23 | 0.25 | 0.36 | 0.18 |
| Female breast | C50 | 7.50 | 10.86 | 6.10 | – | – | – | 7.50 | 10.86 | 6.10 |
| Cervix | C53 | 5.57 | 8.06 | 4.54 | – | – | – | 5.57 | 8.06 | 4.54 |
| Uterus | C54 | 1.35 | 1.96 | 1.05 | – | – | – | 1.35 | 1.96 | 1.05 |
| Ovary | C56 | 3.26 | 4.73 | 2.64 | – | – | – | 3.26 | 4.73 | 2.64 |
| Prostate | C61 | 4.75 | 6.59 | 3.26 | 4.75 | 6.59 | 3.26 | – | – | – |
| Testis | C62 | 0.08 | 0.11 | 0.07 | 0.08 | 0.11 | 0.07 | – | – | – |
| Kidney | C64 | 2.40 | 1.70 | 0.91 | 1.64 | 2.27 | 1.30 | 0.76 | 1.10 | 0.54 |
| Bladder | C67 | 4.14 | 2.93 | 1.34 | 3.25 | 4.51 | 2.31 | 0.88 | 1.28 | 0.52 |
| Brain, CNS | C70–72 | 5.66 | 4.01 | 2.51 | 3.16 | 4.38 | 2.88 | 2.51 | 3.63 | 2.15 |
| Thyroid | C73 | 1.16 | 0.82 | 0.45 | 0.43 | 0.60 | 0.35 | 0.72 | 1.05 | 0.55 |
| Lymphoma | C81–86, 88 | 4.16 | 2.95 | 1.64 | 2.51 | 3.48 | 2.06 | 1.65 | 2.39 | 1.24 |
| Leukemia | C91–95 | 5.01 | 3.55 | 2.37 | 2.92 | 4.04 | 2.78 | 2.09 | 3.03 | 1.97 |
| All other sites⁎ | Other | 16.78 | 11.89 | 6.47 | 9.42 | 13.07 | 7.64 | 7.36 | 10.66 | 5.37 |
| All sites⁎ | All | 257.42 | 182.34 | 96.47 | 162.93 | 225.97 | 127.49 | 94.49 | 136.79 | 67.81 |
Non-melanoma skin cancer (C44) was included.
Abbreviations: ASMR, age-standardized mortality rate by world standard population (Segi's population); CNS, central nervous system; ICD-10, International Statistical Classification of Diseases and Related Health Problems 10th Revision.
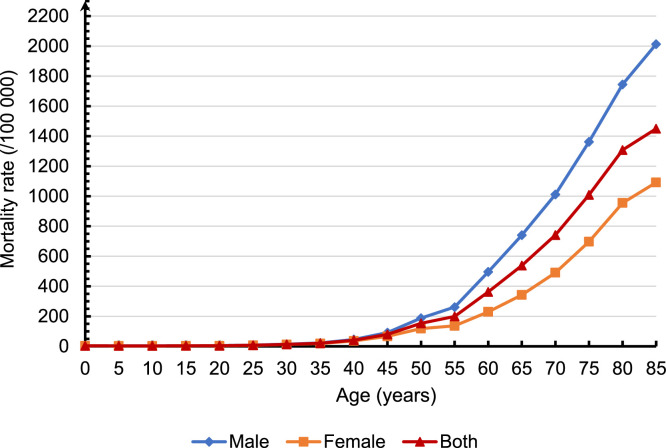
The mortality rate increased significantly after the age group of 40–44 years old and peaked in the age group 85 years and older, with a mortality rate of 1,449.71 per 100,000. In the population after the age of 40 years, the mortality rates were higher for males than for females (Fig. 2).
Fig. 2.
Estimated age-specific mortality rates for all cancers combined in China in 2022.
3.4. Leading causes of cancer death in China in 2022
For both sexes combined, the leading cause of cancer death was lung cancer (733,300 deaths), followed by liver cancer (316,500 deaths), stomach cancer (260,400 deaths), colorectal cancer (240,000 deaths), and esophageal cancer (187,500 deaths), accounting for 67.50% of total cancer deaths. For males, the top 5 causes of cancer deaths were lung cancer, liver cancer, stomach cancer, colorectal cancer, and esophageal cancer, accounting for 74.28% of total cancer deaths. For females, the top 5 causes of cancer deaths were lung cancer, colorectal cancer, liver cancer, stomach cancer, and breast cancer, accounting for 58.78% of total cancer deaths (Table 4).
Table 4.
Trends in age-standardized mortality rates for selected cancers by sex in China, 2000 to 2018.
| Sex | Site | Trend 1 |
Trend 2 |
Trend 3 |
AAPC, % (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC, % (95% CI) | Years | APC, % (95% CI) | Years | APC, % (95% CI) | 2000–2018 | 2009–2018 | 2014–2018 | ||
| Both | All sites | 2000–2004 | −2.2⁎ (−3.4 to −1.0) | 2004–2009 | −0.1 (−1.3–1.2) | 2009–2018 | −1.6⁎ (−2.0 to −1.3) | −1.3⁎ (−1.7 to −0.9) | −1.6⁎ (−2.0 to −1.3) | −1.6⁎ (−2.0 to −1.3) |
| Males | All sites | 2000–2018 | −1.2⁎ (−1.4 to −1.0) | – | – | – | – | −1.2⁎ (−1.4 to −1.0) | −1.2⁎ (−1.4 to −1.0) | −1.2⁎ (−1.4 to −1.0) |
| Esophagus | 2000–2004 | −5.6⁎ (−8.1 to −3.0) | 2004–2018 | −3.3⁎ (−3.7 to −2.9) | – | – | −3.8⁎ (−4.4 to −3.2) | −3.3⁎ (−3.7 to −2.9) | −3.3⁎ (−3.7 to −2.9) | |
| Stomach | 2000–2004 | −6.0⁎ (−7.9 to −3.9) | 2004–2010 | −1.9⁎ (−3.4 to −0.4) | 2010–2018 | −3.8⁎ (−4.5 to −3.1) | −3.7⁎ (−4.3 to −3.0) | −3.6⁎ (−4.1 to −3.0) | −3.8⁎ (−4.5 to −3.1) | |
| Colon-rectum | 2000–2018 | 1.2⁎ (0.9–1.6) | – | – | – | – | 1.2⁎ (0.9–1.6) | 1.2⁎ (0.9–1.6) | 1.2⁎ (0.9–1.6) | |
| Liver | 2000–2007 | −1.6⁎ (−2.9 to −0.2) | 2007–2018 | −3.5⁎ (−4.2 to −2.8) | – | – | −2.8⁎ (−3.4 to −2.2) | −3.5⁎ (−4.2 to −2.8) | −3.5⁎ (−4.2 to −2.8) | |
| Pancreas | 2000–2018 | 1.1⁎ (0.8–1.4) | – | – | – | – | 1.1⁎ (0.8–1.4) | 1.1⁎ (0.8–1.4) | 1.1⁎ (0.8–1.4) | |
| Lung | 2000–2018 | −0.6⁎ (−0.9 to −0.4) | – | – | – | – | −0.6⁎ (−0.9 to −0.4) | −0.6⁎ (−0.9 to −0.4) | −0.6⁎ (−0.9 to −0.4) | |
| Prostate | 2000–2010 | 5.7⁎ (4.5–6.9) | 2010–2018 | 2.0⁎ (0.4–3.7) | – | – | 4.1⁎ (3.1–5.0) | 2.4⁎ (1.1–3.8) | 2.0⁎ (0.4–3.7) | |
| Bladder | 2000–2018 | −0.1 (−0.5–0.3) | – | – | – | – | −0.1 (−0.5–0.3) | −0.1 (−0.5–0.3) | −0.1 (−0.5–0.3) | |
| Brain, CNS | 2000–2018 | −0.3 (−0.8–0.3) | – | – | – | – | −0.3 (−0.8–0.3) | −0.3 (−0.8–0.3) | −0.3 (−0.8–0.3) | |
| Leukemia | 2000–2010 | 2.0⁎ (0.9–3.1) | 2010–2018 | −2.0⁎ (−3.5 to −0.5) | – | – | 0.2 (−0.6–1.0) | −1.6⁎ (−2.8 to −0.3) | −2.0⁎ (−3.5 to −0.5) | |
| Females | All sites | 2000–2004 | −1.7⁎ (−2.8 to −0.6) | 2004–2010 | −0.3 (−1.0–0.5) | 2010–2018 | −1.9⁎ (−2.3 to −1.5) | −1.3⁎ (−1.7 to −1.0) | −1.7⁎ (−2.0 to −1.4) | −1.9⁎ (−2.3 to −1.5) |
| Esophagus | 2000–2018 | −6.2⁎ (−6.5 to −5.9) | – | – | – | – | −6.2⁎ (−6.5 to −5.9) | −6.2⁎ (−6.5 to −5.9) | −6.2⁎ (−6.5 to −5.9) | |
| Stomach | 2000–2004 | −6.0⁎ (−7.9 to −4.2) | 2004–2010 | −2.2⁎ (−3.6 to −0.9) | 2010–2018 | −4.9⁎ (−5.6 to −4.3) | −4.3⁎ (−4.9 to −3.7) | −4.6⁎ (−5.2 to −4.1) | −4.9⁎ (−5.6 to −4.3) | |
| Colon-rectum | 2000–2004 | −0.9 (−2.9–1.2) | 2004–2009 | 1.6 (−0.5–3.7) | 2009–2018 | −1.0⁎ (−1.6 to −0.4) | −0.3 (−1.0–0.4) | −1.0⁎ (−1.6 to −0.4) | −1.0⁎ (−1.6 to −0.4) | |
| Liver | 2000–2007 | −1.9⁎ (−2.9 to −0.8) | 2007–2018 | −4.2⁎ (−4.7 to −3.7) | – | – | −3.3⁎ (−3.8 to −2.8) | −4.2⁎ (−4.7 to −3.7) | −4.2⁎ (−4.7 to −3.7) | |
| Pancreas | 2000–2018 | 1.1⁎ (0.7–1.5) | – | – | – | – | 1.1⁎ (0.7–1.5) | 1.1⁎ (0.7–1.5) | 1.1⁎ (0.7–1.5) | |
| Lung | 2000–2012 | −0.3 (−0.7–0.1) | 2012–2018 | −3.0⁎ (−4.1 to −1.8) | – | – | −1.2⁎ (−1.6 to −0.8) | −2.1⁎ (−2.8 to −1.4) | −3.0⁎ (−4.1 to −1.8) | |
| Breast | 2000–2018 | 0.8⁎ (0.5–1.1) | – | – | – | – | 0.8⁎ (0.5–1.1) | 0.8⁎ (0.5–1.1) | 0.8⁎ (0.5–1.1) | |
| Cervix | 2000–2018 | 5.1⁎ (4.6–5.6) | – | – | – | – | 5.1⁎ (4.6–5.6) | 5.1⁎ (4.6–5.6) | 5.1⁎ (4.6–5.6) | |
| Ovary | 2000–2004 | 15.2⁎ (6.3–24.8) | 2004–2018 | 1.5⁎ (0.3–2.7) | – | – | 4.4⁎ (2.5–6.3) | 1.5⁎ (0.3–2.7) | 1.5⁎ (0.3–2.7) | |
| Brain, CNS | 2000–2018 | −0.6⁎ (−1.2 to −0.1) | – | – | – | – | −0.6⁎ (−1.2 to −0.1) | −0.6⁎ (−1.2 to −0.1) | −0.6⁎ (−1.2 to −0.1) | |
The APC or AAPC is significantly different from zero (P < 0.05).
Abbreviations: APC, annual percentage change; AAPC, average annual percentage change; CNS, central nervous system; CI, confidence interval.
3.5. Trends in cancer incidence for selected cancer sites
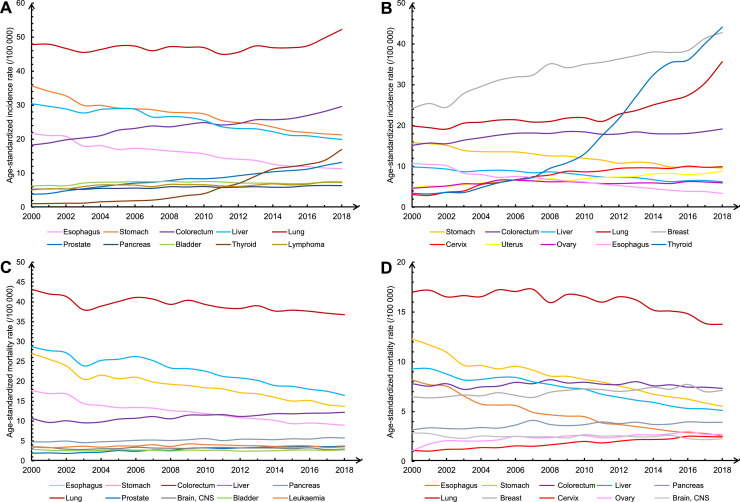
During 2000–2018, the ASIR of all cancers increased significantly by about 1.4% per year. Fig. 3 and Table 3 show the trends of incidence for all cancers combined and selected cancers by sex. The ASIR for all cancers combined remained stable during 2000–2018 in males, but increased significantly by 2.6% per year in females, mainly due to more diagnoses of thyroid cancer (AAPC=15.7%) and cervical cancer (AAPC=7.3%). In addition, the ASIR also showed an increase for cancers of the uterus (3.4%), lung (3.1%), and breast (3.1%) in females, but with a decreasing trend for cancers of the esophagus (6.4%), stomach (2.8%), and liver (2.4%). During 2014–2018, the ASIR of thyroid cancer (AAPC=8.5%) and lung cancer (AAPC=8.3%) showed significant increases in females. The average annual growth rate of the ASIR for cervical cancer has decreased from 14.8% before 2008 to 1.7% in 2018. In males, the AAPC for incidence rates showed increasing trends for cancers of the thyroid (16.9%), prostate (7.0%), and colon-rectum (2.7%), and decreasing trends for cancers of the esophagus (3.5%), stomach (2.9%), and liver (2.3%). The trend for lung cancer was stable from 2000 to 2014. During 2014–2018, the ASIR of thyroid cancer (9.2%), prostate cancer (5.1%), colorectal cancer (3.5%) and lung cancer (2.7%) showed significant increases in males.
Fig. 3.
Trends in age-standardized incidence and mortality rates for selected cancers by sex in China, 2000 to 2018. (A) Male incidence. (B) Female incidence. (C) Male mortality. (D) Female mortality. CNS, central nervous system.
Table 3.
Trends in age-standardized incidence rates for selected cancers by sex in China, 2000 to 2018.
| Sex | Site | Trend 1 |
Trend 2 |
Trend 3 |
AAPC, % (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC, % (95% CI) | Years | APC, % (95% CI) | Years | APC, % (95% CI) | 2000–2018 | 2009–2018 | 2014–2018 | ||
| Both | All sites | 2000–2014 | 1.1⁎ (0.8–1.3) | 2014–2018 | 2.5⁎ (0.8–4.1) | – | – | 1.4⁎ (1.0–1.8) | 1.7⁎ (1.0–2.4) | 2.5⁎ (0.8–4.1) |
| Males | All sites | 2000–2018 | 0.3⁎ (0.1–0.4) | – | – | – | – | 0.3⁎ (0.1–0.4) | 0.3⁎ (0.1–0.4) | 0.3⁎ (0.1–0.4) |
| Esophagus | 2000–2018 | −3.5⁎ (−3.8 to −3.3) | – | – | – | – | −3.5⁎ (−3.8 to −3.3) | −3.5⁎ (−3.8 to −3.3) | −3.5⁎ (−3.8 to −3.3) | |
| Stomach | 2000–2004 | −4.6⁎ (−6.0 to −3.1) | 2004–2009 | −1.3 (−2.8–0.3) | 2009–2018 | −3.1⁎ (−3.6 to −2.7) | −2.9⁎ (−3.5 to −2.4) | −3.1⁎ (−3.6 to −2.7) | −3.1⁎ (−3.6 to −2.7) | |
| Colon-rectum | 2000–2006 | 4.3⁎ (3.5–5.1) | 2006–2014 | 1.1⁎ (0.5–1.7) | 2014–2018 | 3.5⁎ (2.0–5.0) | 2.7⁎ (2.2–3.1) | 2.2⁎ (1.5–2.8) | 3.5⁎ (2.0–5.0) | |
| Liver | 2000–2006 | −0.9 (−2.0–0.2) | 2006–2018 | −2.9⁎ (−3.3 to −2.6) | – | – | −2.3⁎ (−2.7 to −1.9) | −2.9⁎ (−3.3 to −2.6) | −2.9⁎ (−3.3 to −2.6) | |
| Pancreas | 2000–2018 | 1.0⁎ (0.8–1.2) | – | – | – | – | 1.0⁎ (0.8–1.2) | 1.0⁎ (0.8–1.2) | 1.0⁎ (0.8–1.2) | |
| Lung | 2000–2014 | −0.2 (−0.4–0.1) | 2014–2018 | 2.7⁎ (0.9–4.6) | – | – | 0.5⁎ (0.1–0.9) | 1.1⁎ (0.4–1.8) | 2.7⁎ (0.9–4.6) | |
| Prostate | 2000–2005 | 12.2⁎ (10.3–14.2) | 2005–2018 | 5.1⁎ (4.6–5.5) | – | – | 7.0⁎ (6.5–7.6) | 5.1⁎ (4.6–5.5) | 5.1⁎ (4.6–5.5) | |
| Bladder | 2000–2005 | 4.3⁎ (2.4–6.3) | 2005–2018 | −0.5⁎ (−1.0 to −0.1) | – | – | 0.8⁎ (0.3–1.4) | −0.5⁎ (−1.0 to −0.1) | −0.5⁎ (−1.0 to −0.1) | |
| Thyroid | 2000–2007 | 11.8⁎ (9.0–14.7) | 2007–2014 | 27.0⁎ (23.0–31.2) | 2014–2018 | 9.2⁎ (2.8–16.1) | 16.9⁎ (14.7–19.1) | 18.8⁎ (15.4–22.3) | 9.2⁎ (2.8–16.1) | |
| Lymphoma | 2000–2004 | 6.8⁎ (2.9–10.8) | 2004–2012 | −0.3 (−1.9–1.2) | 2012–2018 | 2.5⁎ (0.5–4.6) | 2.2⁎ (1.0–3.3) | 1.6⁎ (0.3–2.9) | 2.5⁎ (0.5–4.6) | |
| Females | All sites | 2000–2006 | 2.8⁎ (1.8–3.8) | 2006–2011 | 1.4 (−0.4–3.2) | 2011–2018 | 3.2⁎ (2.4–4.0) | 2.6⁎ (1.9–3.2) | 2.8⁎ (2.1–3.4) | 3.2⁎ (2.4–4.0) |
| Esophagus | 2000–2004 | −8.0⁎ (−11.3 to −4.6) | 2004–2009 | −3.9⁎ (−7.4 to −0.3) | 2009–2018 | −7.0⁎ (−7.9 to −6.0) | −6.4⁎ (−7.5 to −5.2) | −7.0⁎ (−7.9 to −6.0) | −7.0⁎ (−7.9 to −6.0) | |
| Stomach | 2000–2018 | −2.8⁎ (−3.0 to −2.6) | – | – | – | – | −2.8⁎ (−3.0 to −2.6) | −2.8⁎ (−3.0 to −2.6) | −2.8⁎ (−3.0 to −2.6) | |
| Colon-rectum | 2000–2006 | 3.1⁎ (2.1–4.1) | 2006–2018 | 0.2 (−0.1–0.5) | – | – | 1.1⁎ (0.8–1.5) | 0.2 (−0.1–0.5) | 0.2 (−0.1–0.5) | |
| Liver | 2000–2009 | −1.7⁎ (−2.5 to −1.0) | 2009–2014 | −4.3⁎ (−6.8 to −1.6) | 2014–2018 | −1.5 (−4.1–1.2) | −2.4⁎ (−3.3 to −1.5) | −3.0⁎ (−4.7 to −1.4) | −1.5 (−4.1–1.2) | |
| Lung | 2000–2013 | 1.1⁎ (0.6–1.7) | 2013–2018 | 8.3⁎ (6.0–10.7) | – | – | 3.1⁎ (2.4–3.8) | 5.1⁎ (3.9–6.2) | 8.3⁎ (6.0–10.7) | |
| Breast | 2000–2006 | 5.2⁎ (3.6–6.8) | 2006–2018 | 2.1⁎ (1.6–2.7) | – | – | 3.1⁎ (2.6–3.7) | 2.1⁎ (1.6–2.7) | 2.1⁎ (1.6–2.7) | |
| Cervix | 2000–2008 | 14.8⁎ (12.5–17.0) | 2008–2018 | 1.7⁎ (0.3–3.1) | – | – | 7.3⁎ (6.2–8.4) | 1.7⁎ (0.3–3.1) | 1.7⁎ (0.3–3.1) | |
| Uterus | 2000–2005 | 5.5⁎ (3.2–7.9) | 2005–2018 | 2.6⁎ (2.0–3.1) | – | – | 3.4⁎ (2.7–4.1) | 2.6⁎ (2.0–3.1) | 2.6⁎ (2.0–3.1) | |
| Ovary | 2000–2006 | 6.3⁎ (4.8–7.9) | 2006–2011 | −2.8⁎ (−5.4 to −0.2) | 2011–2018 | 0.7 (−0.4–1.9) | 1.5⁎ (0.6–2.4) | −0.1 (−1.0–0.9) | 0.7 (−0.4–1.9) | |
| Thyroid | 2000–2004 | 8.3⁎ (1.9–15.2) | 2004–2014 | 21.8⁎ (19.7–24.0) | 2014–2018 | 8.5⁎ (2.1–15.3) | 15.7⁎ (13.5–17.9) | 15.7⁎ (12.8–18.7) | 8.5⁎ (2.1–15.3) | |
The APC or AAPC is significantly different from zero (P < 0.05).
Abbreviations: AAPC, average annual percentage change; APC, annual percentage change; CI, confidence interval.
3.6. Trends in cancer mortality for selected cancer sites
During 2000–2018, the ASMR decreased significantly by about 1.3% per year for all cancers combined, mainly due to decreases in esophageal cancer (3.8% in males and 6.2% in females), stomach cancer (3.7% in males and 4.3% in females), and liver cancer (2.8% in males and 3.3% in females). In males, the all-cancer ASMR decreased by about 1.2% per year. However, the rates for prostate cancer (AAPC = 4.1%), colorectal cancer (AAPC = 1.2%), and pancreatic cancer (AAPC = 1.1%) increased during this period. During 2014–2018, the ASMR of stomach cancer (AAPC = −3.8%), liver cancer (AAPC = −3.5%), and esophageal cancer (AAPC = −3.3%) showed significant decreases in males. In females, the all-cancer mortality rate presented an average annual decrease of 1.3% from 2000 to 2018. However, there was an upward trend in ASMR of cancers of the cervix (AAPC = 5.1%), ovary (AAPC = 4.4%). During 2014–2018, the ASMR of esophageal cancer (AAPC = −6.2%), stomach cancer (AAPC = −4.9%), and liver cancer (AAPC = −4.2%) and showed significant decreases in females (Table 4 and Fig. 3).
4. Discussion
In this study, we estimated the burden of cancer in China in 2022 using the most updated and comprehensive registration data for 2018 and continuous data from 106 cancer registries. We estimated that there would be approximately 4,824,700 new cancer cases and 2,574,200 cancer deaths in China in 2022. Lung cancer was the most common cancer in China as well as the first leading cause of cancer deaths in both males and females. During 2000–2018, the ASIR of all cancers increased significantly by about 1.4% per year. In contrast, the ASMR for all cancers combined decreased significantly by about 1.3% per year.
Compared with the GLOBOCAN 2020 estimate,6 the estimated incidence of all cancers in this study increased by approximately 256 thousand cases, with thyroid cancer contributing 245 thousand cases, and the patterns for specific cancer types were quite different. In addition, this study estimated a reduction of 429 thousand deaths compared to GLOBOCAN 2020. The source used to estimate the GLOBOCAN 2020 database was the cancer data provided by population-based cancer registries of IARC for Cancer Incidence in Five Continents (CI5) Vol. XI,7 which included only a few registries in China. It is worth mentioning that the cancer registration work in China has made great progress and development in recent years. By 2022, 2,806 districts/counties had established cancer registration network, accounting for 98.6% of all districts/counties in Chinese mainland. Especially in GLOBOCAN 2022, the estimated results of this study were used to present the incidence and mortality of cancer in China. We suggest not to consider the difference between GLOBOCAN 2020 and GLOBOCAN 2022 as a change in cancer incidence and mortality in China, but rather to refer to the results in Sections 3.5 and 3.6 of this study.
The projected numbers for new cancer cases and deaths in China in 2022 have increased compared to previous years.8,9 The increase in incidence can be attributed partly to the country's aging population, which is a recognized risk factor for cancer. China's population has been expanding over recent decades, which has contributed to the growing cancer burden.10 As cancer prevention awareness rise, so does the number of individuals actively seeking medical attention, leading to an increase in cancer detection rates. The crude mortality rate has increased compared to previous years (from 174.55 per 100,000 in 2016 to 182.34 per 100,000 in 2022), but the ASMR showed a downward trend (from 105.19 per 100,000 in 2016 to 96.47 per 100,000 in 2022), indicating that the increase in mortality was more due to the aging population.
Lung cancer was the leading cause of new cases and deaths in China, which may be attributed to the high prevalence of smoking. The National Health Commission released the “2020 Report on Health Hazards of Smoking in China”, highlighting that the global smoking rate for individuals aged 15 years and above declined from 2007 to 2017, reaching 19.2%. In contrast, China's smoking rate for individuals aged 15 years and above was 26.6% in 2018, with a staggering 68.1% of non-smokers exposed to second-hand smoke in public areas.11 In China, smoking is attributed to about 44.7% of male lung cancer deaths and about 6.4% of female lung cancer deaths.12
In China, the top ten prevalent cancers were lung cancer, colorectal cancer, thyroid cancer, liver cancer, stomach cancer, female breast cancer, esophageal cancer, cervical cancer, prostate cancer and pancreatic cancer. According to prior research, cancers of the lung, female breast, colon-rectum and prostate constitute half of the overall cancer burden in areas with the highest human development index (HDI). In medium HDI regions, cancers of the esophagus, stomach, and liver were common, and cervical cancer was more common in low HDI regions.13 Due to the large number of patients, besides lung cancer, the top five cancers in terms of deaths included liver cancer (316,500), stomach cancer (260,400) and esophageal cancer (187,500), which were of traditional high-incidence and poor-prognosis in China, as well as colorectal cancer (240,000), which was common in developed countries. These indicate that China has a cancer spectrum similar to both developed and developing countries.
The ASIR showed a noticeable rise in thyroid cancer (16.9% for males and 15.7% for females). This could be due to people having higher cancer prevention awareness, better access to healthcare and greater chances of receiving thyroid ultrasounds. The incidence of cervical cancer has been on the rise in China, but the upward trend has slowed down significantly since 2008. This decline is especially notable among younger generations, indicating the efficacy of recent cervical cancer prevention and control strategies in China.14,15
The ASMR decreased by 1.2% annually in males and decreased by 1.3% per year in females, mainly due to the continuous decrease in esophageal cancer, stomach cancer and liver cancer, reflecting the achievements of cancer prevention and control policies in China in recent decades. China has gradually promoted upper gastrointestinal cancer screening since 2005. As of 2019, two million people have benefited from standardized endoscopic screening, 32,000 patients have been detected by screening, achieving early detection rate and treatment rate of 72.64% and 83.38%, respectively.16 Previous studies provided robust evidence that endoscopic screening can reduce the mortality and incidence of esophageal cancer by 34% and 30%, respectively.17,18 Effective strategies for controlling risk factors, including reducing exposure to infectious agents such as H. pylori, hepatitis B, and hepatitis C, controlling tobacco use, reducing alcohol consumption, avoiding contaminated food containing aflatoxins, limiting pickled vegetable intake, and improving the quality of drinking water, also contribute to the declining trend of the burden of upper gastrointestinal cancers.19, 20, 21
There are limitations to this study as the data utilized in the trend analysis section is limited to 22 cancer registries, which represents a relatively small population of early registration work coverage and may not fully reflect the overall trend changes in China. Although the results of this study can reflect the overall incidence and mortality of cancer in China in 2022, it may differ from the actual results of cancer occurrence and cancer death, because the incidence and mortality rates of cancer was estimated values using an age-period-cohort model with 106 cancer registry data from 2010 to 2018. Future efforts will concentrate on improving the quality of cancer registration data in different geographic regions to achieve better representation and coverage of high-quality, long-term surveillance registry sites across China.
5. Conclusions
In conclusion, cancer remains a major public health problem in China, and the cancer spectrum still presents a coexistence of that in both developed countries and developing countries. The Chinese government has prioritized cancer control through a series of health policies, including the “the Healthy China 2030″ Outline, “Healthy China Action (2019–2030)”, “Medium and Long-Term Plan for Chronic Disease Prevention and Control in China (2017–2025)”, the “Healthy China Action - Implementation Plan for Cancer Prevention and Control (2019–2022)”, and the “Healthy China Action - Implementation Plan for Cancer Prevention and Control (2023–2030)”. These plans provide comprehensive guidelines to execute measures for cancer prevention and control. This study indicates that cancer burden in China has been increasing partly due to the aging population, greater awareness of cancer prevention among the public, and improved access to medical care. However, the burden of digestive system cancers presented a downward trend, revealing the achievements of long-term implementation of cancer prevention and control measures in China. Extensive efforts are necessary in fields like system construction, surveillance, early diagnosis, standardized treatment, medical security, medical aid, and scientific and technological breakthroughs, to help alleviate the increasing burden of cancer and improve the health of the Chinese population.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We thank the Department of Medical Emergency Response, National Health Commission of the People's Republic of China and International Agency for Research on Cancer, World Health Organization for their support of this study. We sincerely acknowledge staff of population-based cancer registries for the effort they put in data collection and data quality control. The authors take full responsibility of the data analysis and result interpretation of this paper. This study is supported by the CAMS Innovation Fund for Medical Sciences (grant numbers: 2021-I2M-1-010, 2021-I2M-1-046, 2021-I2M-1-011, 2021-I2M-1-023).
Author contributions
W.W. conducted the conceptualization. R.Z. and B.H. performed the data curation, methodology and formal analysis. B.H. wrote the original draft. R.Z., H.Z., S.W., K.S., R.C., L.L. and W.W. conducted writing, review and editing. W.W., R.Z. and S.W. acquired funding. W.W. and J.H. provided resource and conducted the project administration and supervision.
Footnotes
Given his role as Editor in Chief, Jie He had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Huan He.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jncc.2024.01.006.
Contributor Information
Wenqiang Wei, Email: weiwq@cicams.ac.cn.
Jie He, Email: prof.hejie@263.net.
Appendix. Supplementary materials
References
- 1.Wei W, Zeng H, Zheng R, et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol. 2020;21:e342–e349. doi: 10.1016/S1470-2045(20)30073-5. [DOI] [PubMed] [Google Scholar]
- 2.National Cancer Center . People's Medical Publishing House Co., LTD; Beijing, China: 2016. Chinese Guideline for Cancer Registration [in Chinese] [Google Scholar]
- 3.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45:747–755. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 4.Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45:756–764. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 6.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 7.Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: an overview. Int J Cancer. 2021;149:778–789. doi: 10.1002/ijc.33588. [DOI] [PubMed] [Google Scholar]
- 8.Zhang S, Sun K, Zheng R, et al. Cancer incidence and mortality in China, 2015. J Natl Cancer Cent. 2021;1:2–11. [Google Scholar]
- 9.Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Cent. 2022;2:1–9. [Google Scholar]
- 10.Chen WQ, Zheng RS, Zeng HM. Bayesian age-period-cohort prediction of lung cancer incidence in China. Thorac Cancer. 2011;2:149–155. doi: 10.1111/j.1759-7714.2011.00062.x. [DOI] [PubMed] [Google Scholar]
- 11.National Health Commission . 2020. Report on Health Hazards of Smoking in China. [Google Scholar]; https://www.gov.cn/xinwen/2021-05/30/content_5613994.htm [Accessed 21 October 2023].
- 12.Xia C, Zheng R, Zeng H, et al. Provincial-level cancer burden attributable to active and second-hand smoking in China. Tob Control. 2019;28:669–675. doi: 10.1136/tobaccocontrol-2018-054583. [DOI] [PubMed] [Google Scholar]
- 13.Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012;13:790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 14.Zhao F, Qiao Y. Cervical cancer prevention in China: a key to cancer control. Lancet. 2019;393:969–970. doi: 10.1016/S0140-6736(18)32849-6. [DOI] [PubMed] [Google Scholar]
- 15.Sun K, Zheng R, Lei L, et al. Trends in incidence rates, mortality rates, and age-period-cohort effects of cervical cancer - China, 2003-2017. China CDC Wkly. 2022;4:1070–1076. doi: 10.46234/ccdcw2022.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang G, Wei W. People’s Medical Publishing House Co., LTD; Beijing, China: 2020. Screening and Early Diagnosis and Treatment Techniques For Upper Gastrointestinal Cancer: 2020 Pilot Edition [in Chinese] [Google Scholar]
- 17.Chen R, Liu Y, Song G, et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: a multicentre population-based cohort study. Gut. 2021;70:251–260. doi: 10.1136/gutjnl-2019-320200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei WQ, Chen ZF, He YT, et al. Long-term follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China. J Clin Oncol. 2015;33:1951–1957. doi: 10.1200/JCO.2014.58.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cui F, Liang X, Gong X, et al. Preventing hepatitis B though universal vaccination: reduction of inequalities through the GAVI China project. Vaccine. 2013;31:J29–J35. doi: 10.1016/j.vaccine.2012.07.048. [DOI] [PubMed] [Google Scholar]
- 20.Cui F, Shen L, Li L, et al. Prevention of chronic Hepatitis B after 3 decades of escalating vaccination policy, China. Emerg Infect Dis. 2017;23:765–772. doi: 10.3201/eid2305.161477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng R, Qu C, Zhang S, et al. Liver cancer incidence and mortality in China: temporal trends and projections to 2030. Chin J Cancer Res. 2018;30:571–579. doi: 10.21147/j.issn.1000-9604.2018.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.