Highlights
-
•
Lung cancer is the leading cause of cancer incidence and mortality in China.
-
•
Men had higher incidence rates of lung cancer than women in China, but the burden of lung cancer for women in China was still very high and increased quickly.
-
•
The younger the age, the more obvious trend of lung cancer incidence rate descending in men, but more obvious increasing trend in women.
-
•
The numbers of new cases and deaths increased by about 162.6% and 123.6% in the past 17 years, which can be chiefly explained by changes in age structures.
Keywords: Lung cancer, Temporal trends, Cancer registry, China
Abstract
Background
Updated systematic statistics on lung cancer are the underpinning cornerstones for formulating prevention and control strategies for the disease. The incidence and mortality data of lung cancer in China in 2016 were estimated, and also used to analyze the temporal trends of lung cancer from 2000 up to 2016 in this study.
Methods
The burden of lung cancer in China in 2016 was estimated using data from 487 cancer registries, which were abstracted from the database of the National Cancer Center of China (NCC). The temporal trends were estimated with the data of 2000 to 2016 from 22 cancer registries.
Results
About 828,100 new lung cancer cases and 657,000 lung cancer deaths were estimated in China in 2016. The crude incidence and mortality rates in the eastern region were the highest nationwide. The incidence and mortality of lung cancer increased with age, and most of the new cases occurred in the age group of over 60 years. The age-standardized incidence increased by about 0.8% per year during 2000 to 2016, especially in woman, whose annual increase rate reached 2.1%. The age-standardized mortality rate decreased by about 0.6% per year, with a decrease of 1.3% per year in urban areas and an increase of 2.3% per year in rural areas. The numbers of new cases and deaths increased by 162.6% and 123.6%, respectively, during 2000 to 2016, which can be explained mainly by the change of the age structure.
Conclusions
The burden of lung cancer is serious in China, and increased especially rapidly for women in rural areas. The disease is expected to threaten the lives of more people in the future due to factors such as aging and population growth. Lung cancer prevention and control strategies and resources should be leveraged toward women and rural areas in the future.
1. Introduction
Lung cancer has been one of the most common cancers worldwide. With estimates of about 2,206,771 new cases (11.4% of all cancer new cases) and 1,796,144 deaths (18.0% of the all cancer deaths) resulted from this disease globally in 2020, lung cancer continued to rank as the first leading cause of cancer death and the most common cancer incidence worldwide.1 Coupling the global trend, lung cancer also ranks first among all cancer deaths among the Chinese population, with lung cancer ranking first among all cancer incidences in men and second in women. While the incidence of lung cancer in China has been on the rise in the past few decades, a steady decrease has been observed in the United States since the 1990s. China is home to about 20% of the world population, but is accounted for about 37% of all newly diagnosed cases and 40% of deaths from lung cancer, ranking 15th for incidence and 12th for mortality among 185 countries or territories of the world in 2020.1 Lots of risk factors such as cigarette smoking and air pollution have been proved as the risk factors of the disease.2, 3, 4, 5
The precise number of lung cancer cases diagnosed in the whole country is unknown because not the whole population in China is covered by existing population-based cancer registries (PBCR), and in some provinces only a few registries have been established. Moreover, reliable registry data can be available usually 3 to 5 years after a registry comes into being because enough time is needed for data collection and cleaning. Here, in this article, we provide updated estimates of lung cancer incidence, mortality and their temporal trends in China during 2000 to 2016 using 2016 statistics, the latest data from 487 PBCRs. This up-to-date comprehensive overview can offer evidences for future lung cancer prevention and control in China and may provide more detailed information on the prevalence of the disease in China for the international community.
2. Materials and methods
2.1. Data source and quality control
Lung cancer data were sourced from the database of the National Cancer Center of China (NCC), which is the highest authority designated for depositing and evaluating the data submitted by population-based cancer registries in China. All submitted data shall undergo quality control according to the criteria of Chinese Guideline for Cancer Registration (version 2016)6 and Cancer Incidence in Five Continents (CI5-XI)7,8 before they can be deposited or used for any purpose. This study only included qualified data. In detail, the data of a total of 487 verified cancer registries were included and analysed in this study, with 200 registries located in urban areas and 287 registries in rural areas. These registries covered 381,565,422 residents (193,632,323 men and 187,933,099 women), accounting for about 27.60% of the national population by the end of 2016. It should be of note that lung cancer in this study refers to cancers of the lung, bronchus and trachea, whose International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD10) code is C33-34.
2.2. Statistical analysis
All incidence and mortality data of lung cancer coded as C33-34 of ICD-10 were selected from the NCC database. Incidence and mortality rates were stratified by area, gender and age group (0, 1-4, 5 to 80 by 5 years, and 85+). The age-specific incidence (or mortality) rate was calculated using PBCRs and multiplied by corresponding national population, then added the number of new cases (or deaths) in each age group. Software SAS® 9.4 was used for the estimation.
The trends for lung cancer incidence and mortality from 2000 to 2016 were analysed using the data of 22 selected registries with continuous recordings through Joinpoint Regression Models, which were restricted to a maximum of 2 joinpoints to reduce the possibility of reporting spurious changes over the period.9 The age-standardized rates (ASR) were estimated using the Segi's population (1960).10 We apportioned lung cancer cases and deaths during 2000 to 2016 into the contribution from the change of risk and demographic component (including change in population size and age structure) according to methods described by Moller et al.11
3. Results
3.1. Lung cancer incidence and mortality in China, 2016
Lung cancer is the first leading cause of cancer death in China, with the incidence of lung cancer ranking first of all cancers in men and second in women. It was estimated that there were about 828,100 new lung cancer cases (549,800 men and 278,300 women) and about 657,000 lung cancer deaths (454,700 men and 202,300 women) in China in 2016. The crude and age-standardized incidence rates using world Segi's standard population (ASIR) were 59.89 and 36.46 per 100,000 population, respectively. The crude and age-standardized mortality rates using world Segi's standard population (ASMR) were 47.51 and 28.09 per 100,000, respectively. The incidence and mortality rates were higher in urban areas than those in rural areas. The comparison of incidence and mortality in different regions showed that the Eastern regions of China had the highest crude incidence and mortality rates, followed by Middle and Western regions (Table 1).
Table 1.
Estimated lung cancer incidence and mortality in China, 2016.
| Area | Sex | Incidence |
Mortality |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Prop. | Rates | ASIR | Rank | Deaths | Prop. | Rates | ASMR | Rank | ||
| (%) | (1/105) | (1/105) | (%) | (1/105) | (1/105) | ||||||
| All areas | Both sexes | 828,100 | 20.4 | 59.9 | 36.5 | 1 | 657,000 | 27.2 | 47.5 | 28.1 | 1 |
| Men | 549,800 | 24.6 | 77.6 | 49.8 | 1 | 454,700 | 29.7 | 64.2 | 40.6 | 1 | |
| Women | 278,300 | 15.2 | 41.3 | 23.7 | 2 | 202,300 | 22.9 | 30.0 | 16.2 | 1 | |
| Urban areas | Both sexes | 502,400 | 20.1 | 63.4 | 37.1 | 1 | 396,400 | 27.7 | 50.0 | 28.3 | 1 |
| Men | 331,300 | 24.5 | 81.9 | 50.3 | 1 | 274,200 | 30.4 | 67.8 | 40.9 | 1 | |
| Women | 171,100 | 14.9 | 44.1 | 24.4 | 2 | 122,200 | 23.2 | 31.5 | 16.3 | 1 | |
| Rural areas | Both sexes | 325,700 | 20.8 | 55.2 | 35.5 | 1 | 260,600 | 26.5 | 44.2 | 27.8 | 1 |
| Men | 218,500 | 24.7 | 72.0 | 49.0 | 1 | 180,500 | 28.7 | 59.5 | 40.0 | 1 | |
| Women | 107,300 | 15.7 | 37.5 | 22.7 | 1 | 80,100 | 22.6 | 28.0 | 16.2 | 1 | |
| Eastern areas | Both sexes | 332,900 | 20.0 | 64.1 | 36.4 | 1 | 260,600 | 27.3 | 50.2 | 27.3 | 1 |
| Men | 211,800 | 23.9 | 80.4 | 48.0 | 1 | 175,800 | 29.5 | 66.7 | 39.0 | 1 | |
| Women | 121,100 | 15.5 | 47.3 | 25.6 | 2 | 84,800 | 23.8 | 33.1 | 16.5 | 1 | |
| Middle areas | Both sexes | 268,200 | 20.2 | 57.8 | 36.2 | 1 | 218,400 | 27.1 | 47.1 | 28.8 | 1 |
| Men | 183,200 | 25.3 | 76.6 | 50.8 | 1 | 153,700 | 30.3 | 64.3 | 42.1 | 1 | |
| Women | 85,000 | 14.0 | 37.8 | 22.2 | 2 | 64,800 | 21.6 | 28.8 | 16.2 | 1 | |
| Western areas | Both sexes | 227,100 | 21.3 | 56.9 | 36.9 | 1 | 177,900 | 27.2 | 44.6 | 28.3 | 1 |
| Men | 154,900 | 24.9 | 75.4 | 51.3 | 1 | 125,200 | 29.3 | 61.0 | 41.0 | 1 | |
| Women | 72,200 | 16.3 | 37.4 | 22.8 | 1 | 52,700 | 23.3 | 27.3 | 15.9 | 1 | |
Abbreviations: ASIR, age-standardized incidence rate using Segi’s population; ASMR, age-standardized mortality rate using Segi’s population.
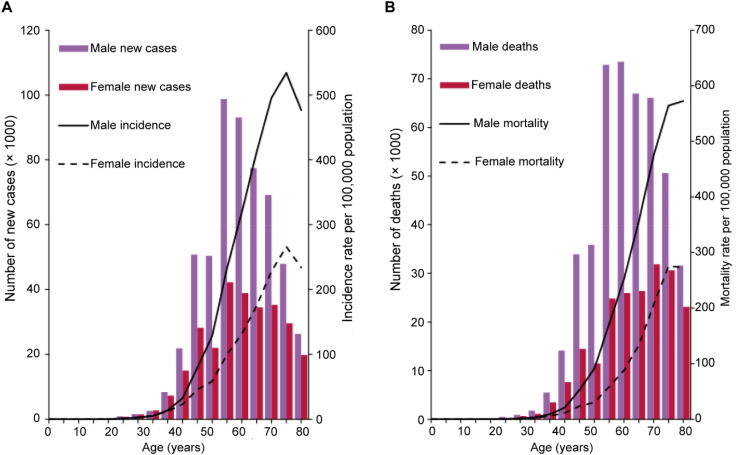
3.2. Age-specific incidence and mortality
The incidence rate of lung cancer increased with age, kept at a low rate before the age of 35 and reaching peak during 80-84 years. Different from the age-specific incidence rate, the number of new cases was the highest in the 60-64 age group for both men and women (Fig. 1A). The mortality rate also increased with age, maintained low before 40 years and peaked at 80-84 years for woman and at 85 years and above for men. The mortality rates in men was higher than that in woman in all age groups. The number of lung cancer deaths increased with age and tended to be plateaued for men in the 60-79 age group and for women after 60 (Fig. 1B).
Fig. 1.
Numbers of new cases or deaths and age-specific rate of lung cancer by age groups in China, 2016 (A) Incidence. (B) Mortality.
Results showed that about 25.0% of men and 28.0% of women were younger than 60 years at their time of onset of lung cancer. In urban areas, about 25.8% and 28.7% of new cases occurred in people under 60 for men and women, respectively, while the proportions were 23.7% and 26.9% in rural areas for both sexes, respectively. Most deaths of lung cancer occurred in people aged 60 years or older (79.8%), yet still about 20.4% of men and19.5% of women died from lung cancer were younger than 60 years.
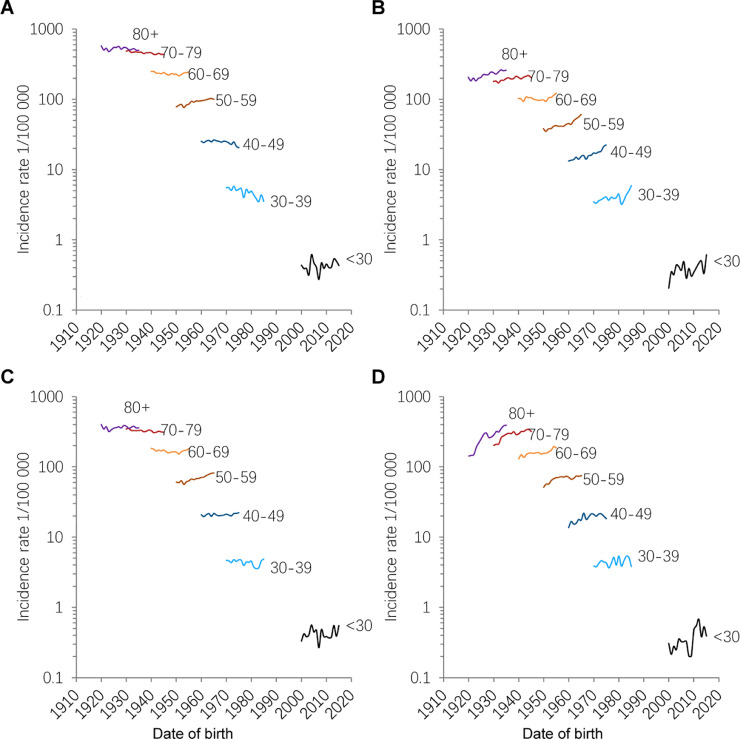
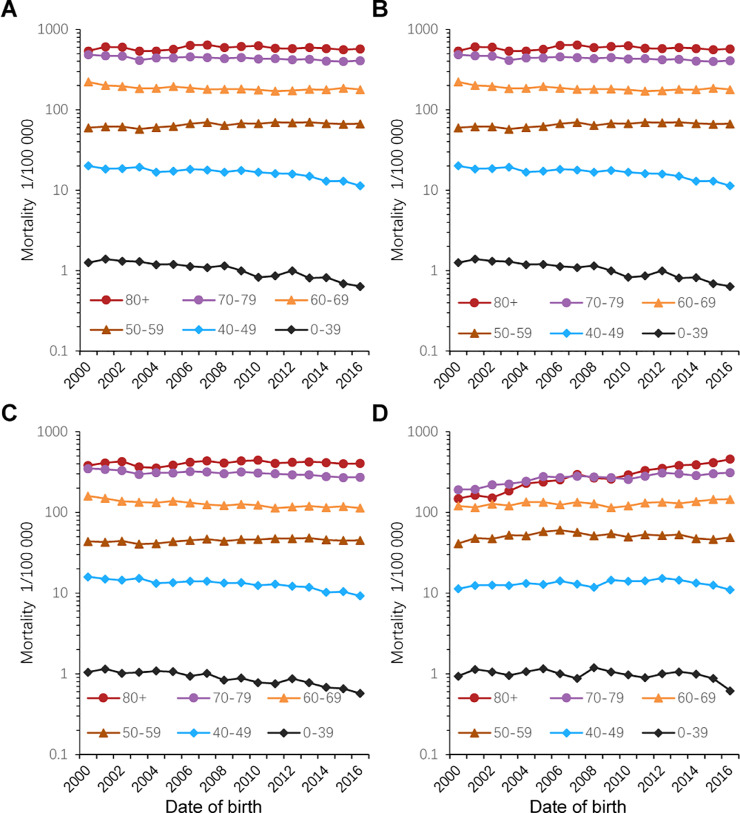
3.3. Trends for lung cancer incidence and mortality
The trends for age-specific lung cancer incidence and mortality rates from 2000 to 2016 in China are presented in Table 2, and accompanying birth-cohorts of lung cancer incidence and mortality are shown in Fig. 2, Fig. 3, respectively. The age-standardized incidence rates of lung cancer increased by about 0.8% annually from 2000 to 2016, with a stable trend for men and a year-on-year increase of 2.1% for women. A significant increase in incidence was observed in rural areas, especially for females, whose rate increased by about 3.9% per year, while the rate in urban areas only had an increase of about 0.5% per year. Trends of age-specific incidence rates showed that the upturn was mainly observed in middle-aged people (40-69 years), particularly in the group aged 50-59 years, for the male and female ones of which the increases were about 1.9% and 3.8%, respectively. The cohort-specific incidence rates also showed a trend of quick increase for the age group of 40-69 years. While the rates decreased by about 1.5% and 1.2% per year for men in the age groups of under 40 years and 40-49 years, the rate for the 50-59 age group increased by about 1.9% per year. The increases in cancer incidence among women in the under-40, 40-49, and 50-59 age groups were about 5.1%, 4.2% and 3.8% per year, respectively. In rural areas, the rate increased by about 3.6% in women younger than 40 years and 2.7% in women aged 40-49 compared with women in the urban areas (5.0% and 4.5%, respectively). The incidence of lung cancer for most age groups of men showed a downward trend, but showed an upward trend for most age groups of women, especially in age groups less than 60 years.
Table 2.
Trends for age-specific lung cancer incidence and mortality rates by area and gender in China, 2000 to 2016.
| Age group | All areas |
Urban areas |
Rural areas |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Men | Women | Both | Men | Women | Both | Men | Women | |
| Incidence | |||||||||
| ASIR | 0.8* | -0.1 | 2.1* | 0.5* | -0.6* | 1.7* | 3.1* | 2.4* | 3.9* |
| < 40 | 1.5 | -1.5* | 5.1* | 1.5 | -1.8* | 5.0* | 1.3* | -1.0 | 3.6* |
| 40-49 | 0.8* | -1.2* | 4.2* | 0.9* | -1.5* | 4.5* | 1.7* | 0.4 | 2.7* |
| 50-59 | 2.4* | 1.9* | 3.8* | 2.4* | 2.0* | 3.8* | 2.7* | 1.8* | 4.8* |
| 60-69 | 0.5* | 0.1 | 1.2* | 0.2 | -0.4 | 0.7 | 2.5* | 1.3* | 4.2* |
| 70-79 | -0.1 | -0.7* | 1.1* | -0.6* | -1.3* | 0.6* | 3.4* | 2.6* | 4.8* |
| 80+ | 0.9* | -0.4 | 2.1* | 0.1 | -1.2* | 1.3* | 7.2* | 6.3* | 7.6* |
| Mortality | |||||||||
| ASMR | -0.6* | -0.6* | -0.9* | -1.3* | -1.4* | -1.5* | 2.3* | 2.0* | 3.3* |
| < 40 | -3.6* | -4.3* | -1.5* | -3.6* | -4.6* | -2.2* | -1.4* | -5.0* | 1.4 |
| 40-49 | -2.5* | -3.2* | -0.9* | -3.1* | -3.6* | -1.4* | -0.2 | -0.7 | 1.3 |
| 50-59 | 0.3 | 0.9* | -0.8 | 0.1 | 1.2* | -0.8* | 0.7 | 0.2 | 1.9 |
| 60-69 | -1.2* | -1.2* | -2.6* | -2.0* | -1.6* | -3.4* | 1.4 | 0.7 | 1.9* |
| 70-79 | -0.6* | -0.9* | -0.4 | -1.6* | -1.4* | -1.3* | 3.1* | 2.4* | 4.2* |
| 80+ | 1.3* | 0.1 | 2.3* | 0.4 | -0.7* | 1.5* | 7.0* | 6.9* | 6.7* |
Average annual percent change during 2000 to 2016 is significantly different from zero (P < 0.05).
Abbreviations: ASIR, age-standardized incidence rate using Segi's population; ASMR, age-standardized mortality rate using Segi's population.
Fig. 2.
Birth cohort specific incidence rates for lung cancer by gender and areas. (A) Male. (B) Female. (C) Urban. (D) Rural.
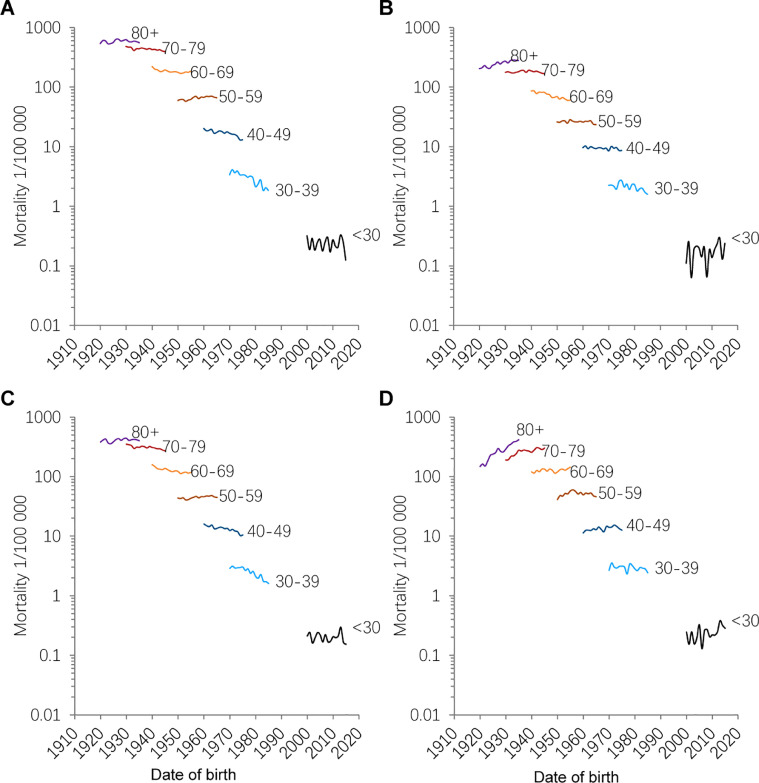
Fig. 3.
Birth cohort specific mortality rates for lung cancer by gender and areas. (A) Male. (B) Female. (C) Urban. (D) Rural.
The trends by gender and age group for lung cancer mortality during the period of 2000 to 2016 are also presented. The ASMR decreased by about 0.6% per year, with a decreasing rate of 1.3% per year in urban areas and an annual increasing rate of 2.3% per year in rural areas. The mortality rate of lung cancer showed a downward trend in urban areas except for the 50-59 and 80+ age groups, with a particularly quick decrease in the age group of under 50. The mortality rate for the 50-59 age group in urban areas increased by 1.2% per year in men, but decreased by about 0.8% per year in women. Different from the trend of mortality in urban areas, mortalities of most age groups in rural areas were increased, especially for women and people over 70 years.
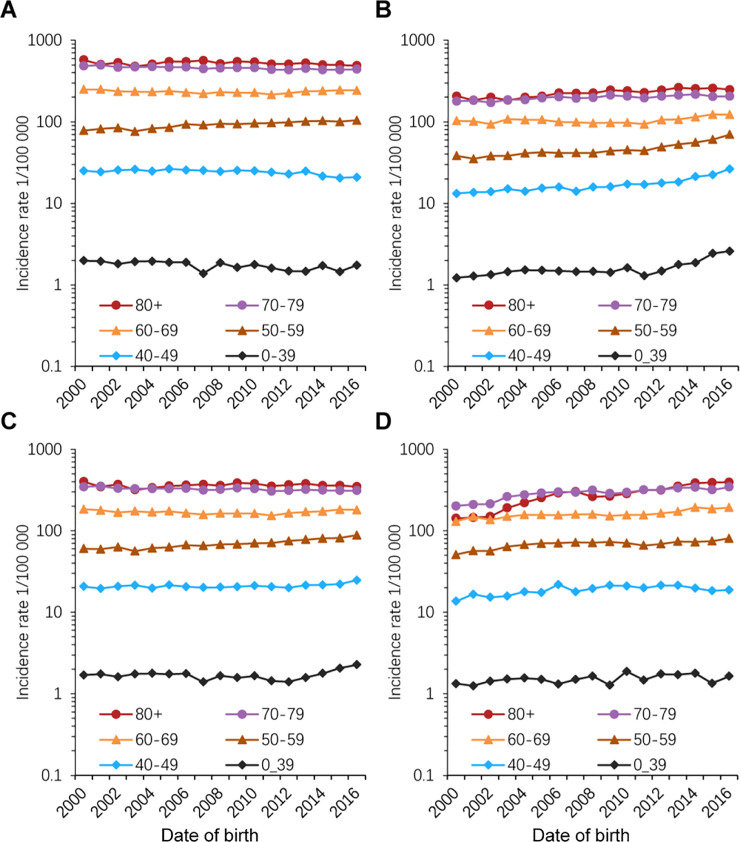
3.4. The contribution due to the changes of risk during 2000 to 2016
The incidence and mortality rates of lung cancer from 2000 to 2016 are shown in Fig. 4, Fig. 5 and the contribution from the change of risk and demographic component are presented in Table 3. The crude incidence and mortality rates increased nearly 30.0% and 19.0% between 2000 and 2016, respectively, while the ASIR increased by about 12.4% and the ASMR decreased by about 11.5% . The new cases of lung cancer increased by 162.6%, with changes due to risk (changing age-specific incidence rates) contributing 26.4%, changing age structures contributing 90.7%, and population growth contributing 45.5%. The lung cancer deaths increased by 123.6%, with changes due to risk contributing −14.1%, changing age structures contributing 92.2%, population growth contributing 45.5%. The changes of number of new lung cancer cases due to risk by about 4.8% and 108.4% in urban and rural areas, while the decreasing number of lung cancer deaths due to risk by about 37.5% and 80.7% in urban and rural areas, respectively.
Fig. 4.
Trends of age-specific incidence for lung cancer by gender and areas, 2000-2016. (A) Male. (B) Female. (C) Urban. (D) Rural.
Fig. 5.
Trends of age-specific mortality for lung cancer by gender and areas, 2000-2016. (A) Male. (B) Female. (C) Urban. (D) Rural.
Table 3.
The changes of number of new cases and deaths between 2000 and 2016 apportioned into changes because of risk and demographics by gender and areas*.
| Areas | Sex | Total changes, % | Changes due to risk, % | Changes due to demographic |
||
| Total, % | Age structure, % | Population size, % | ||||
| New cases | ||||||
| All areas | Both sexes | 162.6 | 26.4 | 136.2 | 90.7 | 45.5 |
| Men | 141.2 | -3.2 | 144.3 | 101.6 | 42.8 | |
| Women | 208.1 | 76.0 | 132.2 | 83.9 | 48.3 | |
| Urban areas | Both sexes | 161.7 | 4.8 | 156.9 | 100.6 | 56.3 |
| Men | 140.2 | -25.3 | 165.5 | 112.6 | 52.9 | |
| Women | 206.7 | 53.6 | 153.0 | 93.1 | 59.9 | |
| Rural areas | Both sexes | 167.8 | 108.4 | 59.4 | 51.1 | 8.3 |
| Men | 146.9 | 84.5 | 62.4 | 54.4 | 8.0 | |
| Women | 218.1 | 161.3 | 56.8 | 48.1 | 8.7 | |
| Deaths | ||||||
| All areas | Both sexes | 123.6 | -14.1 | 137.7 | 92.2 | 45.5 |
| Men | 122.9 | -22.8 | 145.8 | 103.0 | 42.8 | |
| Women | 125.2 | -9.7 | 134.9 | 86.6 | 48.3 | |
| Urban areas | Both sexes | 120.7 | -37.5 | 158.2 | 101.8 | 56.3 |
| Men | 122.5 | -44.2 | 166.7 | 113.8 | 52.9 | |
| Women | 116.8 | -38.6 | 155.3 | 95.4 | 59.9 | |
| Rural areas | Both sexes | 141.4 | 80.7 | 60.8 | 52.4 | 8.3 |
| Men | 125.2 | 61.9 | 63.3 | 55.3 | 8.0 | |
| Women | 188.2 | 129.2 | 59.0 | 50.3 | 8.7 | |
Data based 22 cancer registries.
4. Discussion
This study is an updated analysis of the lung cancer burden in China. It was estimated about 828,100 lung cancer new cases and 657,000 lung cancer deaths occurred in China in 2016. Lung cancer ranks as the first leading cause of cancer incidence and mortality in China, which is the same as other countries in the world.1,12 Notably, the incidence rate of lung cancer in Eastern areas of China is relatively high, while the incidence rate and mortality in the less developed Western areas of China are relatively low. The temporal trends in ASIR continued to increase during the period of 2000 to 2016, but the ASMR showed a slightly decreasing trend by about 0.6% per year during the past decades. However, compared with the previous publication,13 the numbers of new cases and deaths gradually increased due to the expanding whole population and the aging population. Health care expenses for lung cancer in China increased from 14,110 million RMB in 2011 to 24,310 million RMB in 2015,14 and may continue to grow in the future due to the rising trend of new incidences. Aging and population growth are the key causes of the increase of lung cancer burden, and the increasing burden manifested in this study period can be explained mainly by the aging population in China.
Compared with other cancer cites, lung cancer has a low age-standardized 5-year relative survival rate of about 19.7% in China.15 However, according to previous studies,15, 16, 17 the survival rates of this disease are also very low in other countries, such as US (21.2%), Canada(20.6%), Japan(32.9%) and Korea(25.1%). The poor prognosis may be accredited to the fact that most early symptoms of lung cancer are easily neglected. The overlook is especially evident in non-smokers, among whom risk factors related to lung cancer are generally ignored. Moreover, healthy people seldom accept lung cancer-related screening in China, unless doctors find that they have risk factors such as family history, long-term smoking, or other symptoms.
In China, the ASIR of lung cancer remained stable in men, but increased in women during the past 17 years. Our study revealed a distinct increase rate of 2.1% per year for women in rural China, and people aged 40–60 years, especially women, are more prone to an elevated risk for lung cancer. Unlike the increasing trend in China, lung cancer in developed countries such as US showed a decreasing trend since 1990s.18, 19, 20, 21
Most of the increasing burden of lung cancer in China could be attributed to risk factors such as lifestyle, coal burning, air pollution and smoking,22, 23, 24 and lung cancer may occur decades after exposure to its risk factors. Economic development in China has changed people's lifestyles; westernized lifestyles and unhealthy diet are more popular in this country than ever. Some lifestyle factors have been proved to be associated with lung cancer, including cigarette smoking and second-hand smoking. Previous studies have shown that current smokers have approximately 3 to 20 times the risk of lung cancer compared with non-smokers and the risk of lung cancer increases with the numbers of smoking years and smoked cigarettes per day. Luckily, some of these factors are modifiable, and previous studies have demonstrated nearly half of lung cancer can be attributed to those modifiable risk factors.25 Moderate, regular exercise have a significant impact on reducing the risk of developing cancer, including reducing the risk of lung cancer.26
The Chinese government has initiated a series of cancer control programmes in both rural and urban areas since 2005. Given that screening can promote early detection and diagnosis and enhance people's awareness of cancer prevention and control, more lung cancer cases and deaths could be prevented through increased screening coverage.27
The key strength for our study is the most representative data used for the lung cancer burden estimation, which included 487 cancer registries covering nearly about 28% of the national population, and data from 2000 to 2016 covering 22 continuous cancer registries were used for trend analysis. Although the estimated results of this study may still be affected by some unknown level of uncertainty factors, the results may be more reasonable compared with previous estimates.9 Moreover, the updated statistics and the trend analysis for lung cancer burden in China may assist healthcare administrators in drawing up more effective short- and long-term policies and strategies for lung cancer prevention and control.
5. Conclusions
Lung cancer is still the first leading cause of cancer death and the most common cancers in China. The incidence and mortality of lung cancer in urban areas were higher than those in rural areas. The burden of lung cancer increased in the past decades. The increase is mainly caused by the aging of the population in both urban and rural areas, and another part of the increase is due to changes in the risk. The presences of these risk factors may pose new challenges for China to prevent lung cancer and other cancers in the long future. Therefore, it is suggested that priority of strategies and resources for lung cancer prevention and control should be given to women and rural areas in the future. In addition, although the number of new cases of lung cancer is very small in people under 40 years, there may be a huge lag ranging from several years to decades between people's exposure to risk factors and their diagnosis of lung cancer. This suggests that lung cancer prevention should also keep an eye on young people under 40 years.
Declaration of competing interest
The authors declare that they have no conflict of interests.
Acknowledgments
Acknowledgments
The authors express their deep gratitude to all the local Cancer Registry staff in China for their contribution to data collection, validation, and routine analyses. This work was supported by CAMS Innovation Fund for Medical Sciences (grant number 2021-I2M-1-011), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (grant number 2019PT320027).
Author contributions
R.Z. and W.W. performed the study design. R.Z. and S.W. conducted the data analyses. R.Z. drafted the original manuscript. S.Z., S.W., R.C., K.S., H.Z., L.L. and W.W. performed the revision and edition. W.W. and J.H. supervised and led the study.
Footnotes
Given his role as Editor in Chief, Jie He had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Mei Wang.
Contributor Information
Wenqiang Wei, Email: weiwq@cicams.ac.cn.
Jie He, Email: hejie@cicams.ac.cn.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Kabir Z, Bennett K, Clancy L. Lung cancer and urban air-pollution in Dublin: a temporal association? Ir Med J. 2007;100(2):367–369. [PubMed] [Google Scholar]
- 3.Loomis D, Grosse Y, Lauby-Secretan B, et al. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14(13):1262–1263. doi: 10.1016/s1470-2045(13)70487-x. [DOI] [PubMed] [Google Scholar]
- 4.Moolgavkar SH, Holford TR, Levy DT, et al. Impact of reduced tobacco smoking on lung cancer mortality in the United States during 1975–2000. J Natl Cancer Inst. 2012;104(7):541–548. doi: 10.1093/jnci/djs136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pesch B, Kendzia B, Gustavsson P, et al. Cigarette smoking and lung cancer—relative risk estimates for the major histological types from a pooled analysis of case–control studies. Int J Cancer. 2012;131(5):1210–1219. doi: 10.1002/ijc.27339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Cancer Center; 2016. Chinese Guideline for Cancer Registration (version 2016) [Google Scholar]
- 7.Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45(5):756–764. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 8.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45(5):747–755. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 9.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 10.Bray F, Guilloux A, Sankila R, et al. Practical implications of imposing a new world standard population. Cancer Causes Control. 2002;13(2):175–182. doi: 10.1023/a:1014344519276. [DOI] [PubMed] [Google Scholar]
- 11.Moller B, Fekjaer H, Hakulinen T, et al. Prediction of cancer incidence in the Nordic countries up to the year 2020. Eur J Cancer Prev. 2002;11(Suppl 1):S1–96. [PubMed] [Google Scholar]
- 12.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, et al. The Global Burden of Cancer 2013. JAMA Oncol. 2015;1(4):505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China, 2013. Cancer Lett. 2017;401:63–71. doi: 10.1016/j.canlet.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 14.Cai Y, Xue M, Chen W, et al. Expenditure of hospital care on cancer in China, from 2011 to 2015. Chin J Cancer Res. 2017;29(3):253–262. doi: 10.21147/j.issn.1000-9604.2017.03.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6(5):e555–e567. doi: 10.1016/S2214-109X(18)30127-X. [DOI] [PubMed] [Google Scholar]
- 16.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet. 2015;385(9972):977–1010. doi: 10.1016/S0140-6736(14)62038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeSantis CE, Miller KD, Dale W, et al. Cancer statistics for adults aged 85 years and older, 2019. CA Cancer J Clin. 2019;69(6):452–467. doi: 10.3322/caac.21577. [DOI] [PubMed] [Google Scholar]
- 19.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–385. doi: 10.3322/caac.21565. [DOI] [PubMed] [Google Scholar]
- 20.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 21.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 22.Chen W, Xia C, Zheng R, et al. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health. 2019;7(2):e257–e269. doi: 10.1016/S2214-109X(18)30488-1. [DOI] [PubMed] [Google Scholar]
- 23.Hosgood HD, 3rd, Chapman R, Shen M, et al. Portable stove use is associated with lower lung cancer mortality risk in lifetime smoky coal users. Br J Cancer. 2008;99(11):1934–1939. doi: 10.1038/sj.bjc.6604744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu W, Downward GS, Reiss B, et al. Personal and indoor PM2.5 exposure from burning solid fuels in vented and unvented stoves in a rural region of China with a high incidence of lung cancer. Environ Sci Technol. 2014;48(15):8456–8464. doi: 10.1021/es502201s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Islami F, Chen W, Yu XQ, et al. Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol. 2017;28(10):2567–2574. doi: 10.1093/annonc/mdx342. [DOI] [PubMed] [Google Scholar]
- 26.Moore SC, Lee IM, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816–825. doi: 10.1001/jamainternmed.2016.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Z, Wang Y, Huang Y, et al. Challenges and research opportunities for lung cancer screening in China. Cancer Commun (Lond) 2018;38(1):34. doi: 10.1186/s40880-018-0305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]