Diabetic patients, particularly those with type 2 diabetes or proteinuria, are at considerable risk of excessive morbidity and mortality from cardiovascular, cerebrovascular, and peripheral vascular disease leading to myocardial infarction, strokes, and amputations. Much effort must be given to reducing the risk factors that predispose to major atheromatous arterial disease. The many available measures add to the complexity of treating diabetic patients, especially those with type 2 diabetes.
This article is adapted from the 5th edition of the ABC of Diabetes, which is published by BMJ Books (www.bmjbooks.com)
Factors increasing risk of developing CHD in diabetic patients
Smoking
Hypertension
Insulin resistance associated with obesity
Asian origin
Microalbuminuria
Diabetic nephropathy (macroalbuminuria)
Poor glycaemic control
Hyperlipidaemia
Coronary artery disease
Cardiovascular disease is substantially increased in diabetes, with hyperglycaemia an independent risk factor. It is the chief cause of death, and the focus on reducing the risk factors responsible strongly influences the management of diabetes.
Diabetes more than doubles the risk of cardiovascular disease. In the United Kingdom, 35% of deaths are due to cardiovascular causes, compared with about 60% in those with type 2 diabetes and 67% of type 1 diabetic patients over 40 years old. Diabetes increases the risk more in women than men, so that the risk of cardiovascular death is equal in both sexes in diabetic patients. The development of myocardial infarction over seven years in middle aged diabetic patients without known pre-existing coronary heart disease (CHD) is the same as that in non-diabetic patients with CHD. The presence of proteinuria and even microalbuminuria increases the risk of CHD and mortality from myocardial infarction.
Prevention of cardiovascular disease: effects of lowering blood pressure
Those with a high risk of cardiovascular disease stand to gain proportionately greater benefit from reducing risk factors. Two recent major trials show what can be achieved.
The United Kingdom prospective diabetes study (UKPDS) was published in 1998 and compared tight with less tight blood pressure control (mean 144/82 mm Hg v 154/87 mm Hg). Heart failure was reduced by 56%, strokes by 44%, and combined myocardial infarction, sudden death, stroke, and peripheral vascular disease by 34% (myocardial infarction alone was reduced non-significantly by 16%). Tight control also had considerable benefits on the development of retinopathy and proteinuria.
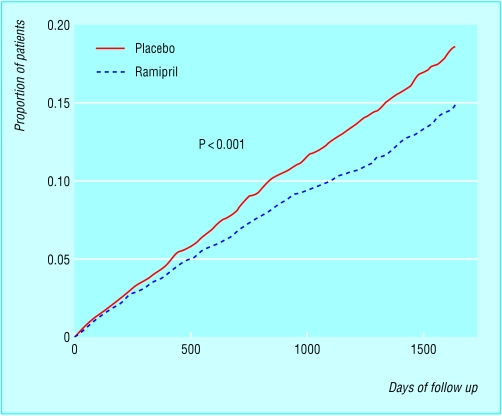
Heart outcomes prevention evaluation (HOPE) and microHOPE study—This study over 4.5 years comprised 9297 patients overall and included 3577 diabetic patients (98% with type 2 diabetes). Patients with diabetes and one other risk factor for cardiovascular disease were randomly treated with the angiotensin converting enzyme inhibitor ramipril 10 mg daily or placebo. Systolic blood pressure decreased by 2-3 mm Hg and reduced combined myocardial infarction, strokes, and deaths from cardiovascular diseases by 25%. The relative risk of myocardial infarction was reduced by 22%, the relative risk of stroke by 33%, and relative risk of cardiovascular death by 37%.
It was concluded that angiotensin converting enzyme inhibitors were the first line treatment for blood pressure control in diabetes. Despite some caveats relating to the handling of the study, this treatment might now be considered even for normotensive patients with high cardiovascular risks.
Blood pressure management
Blood pressure should be checked annually or more frequently as indicated. Borderline readings should be rechecked several times before starting drug treatment. Other factors may also help reduce blood pressure.
Factors that may lower blood pressure
Salt restriction
Weight reduction or exercise programmes
Reduction of excessive alcohol intake
Blood pressure >160/100 mm Hg should always be treated in those with and without diabetes aiming for a level of <140/80mm Hg (audit standard<140/90 mm Hg).
The target blood pressure is <140/80 mm Hg unless the patient has microalbuminuria or macroalbuminuria, when the aim is for 130/80 mm Hg.
Blood pressure of 140-159/90-99 mm Hg should be treated in all diabetic patients and aggressively in those with cardiovascular risk factors, especially if there is evidence of end organ damage; aim for <140/80 mm Hg.
Blood pressure <140/80 mm Hg should be treated if there is evidence of target organ damage or if the 10 year CHD risk exceeds 15%. The aim is for <140/80 mm Hg.
Blood pressure of >130/80 mm Hg should be treated in patients with microalbuminuria or macroalbuminuria.
Choice of antihypertensive drugs
The objective is to lower blood pressure by any means because most of the benefits relate to the blood pressure achieved rather than the drug used. However, angiotensin converting enzyme inhibitors or angiotensin 2 receptor antagonists have advantages over other drugs.
Guidelines for choice of antihypertensive drugs
Patients with heart failure should have an angiotensin converting enzyme inhibitor whenever possible, which can be combined with a diuretic
Conversion to an angiotensin 2 receptor blocker is helpful if a patient develops cough on an angiotensin converting enzyme inhibitor
Addition of an angiotensin 2 receptor blocker to an angiotensin converting enzyme inhibitor will have an additive effects on blood pressure but not on microalbuminuria
Blood pressure in some African and Caribbean patients may respond better to calcium channel antagonists and diuretics than to other drugs
The recent losartan intervention for end point reduction (LIFE) study showed additional benefits with the angiotensin 2 receptor antagonist losartan compared with the β blocker atenolol, despite comparable blood pressure reduction. Many, probably most, patients will need more or than one drug to achieve the intended goal. A pragmatic approach to treatment is therefore often needed.
Angiotensin converting enzyme inhibitors or angiotensin 2 receptor blockers are the first choice in patients with microalbuminuria. Angiotensin converting enzyme inhibitors, angiotensin 2 receptor blockers, cardioselective β blockers, or thiazide diuretics (small dose) are reasonable first line treatment in those without microalbuminuria. Long acting dihydropyridine calcium channel antagonists (for example, amlodipine) have an important role in treating hypertension and are second line drugs.
Lipids and diabetes
Hyperlipidaemias are common in patients with diabetes and further increase the risk of ischaemic heart disease, especially in type 2 diabetes. Detection and control of hyperlipidaemia can reduce myocardial infarction, coronary deaths, and overall mortality. Indeed, even when low density lipoprotein (LDL) cholesterol concentration is normal or slightly raised in type 2 diabetes (the major abnormalities being low HDL cholesterol and high triglyceride concentrations), the LDL particles may be qualitatively different and more atherogenic than those in non-diabetic patients.
Some causes of secondary hyperlipidaemia
| Causes | Main lipid abnormalities |
| Alcohol misuse | ↑Triglyceride, ↑HDL cholesterol |
| Therapeutic drugs* | ↑Triglyceride ± cholesterol, ↓HDL cholesterol |
| Hypothyroidism | ↑Cholesterol |
| Chronic renal failure | ↑Triglyceride |
| Nephrotic syndrome | ↑Cholesterol ± ↑triglyceride |
| Cholestasis | ↑Cholesterol |
| Bulimia | ↑Triglyceride |
| Anorexia nervosa | ↑Cholesterol |
| Pregnancy | ↑Triglyceride |
*Diuretics, oral contraceptives, retinoids, corticosteroids, anabolic steroids, or progestogens related to testosterone.
Screening for dyslipidaemia
Screening for dyslipidaemia is an essential aspect of the annual review. If the lipid profile is entirely normal, further screening could be postponed for three to five years unless circumstances change. Patients with a raised triglyceride concentration should have it confirmed when fasting.
Diabetic control
Optimising diabetic control often improves an abnormal lipid profile in patients with type 1 diabetes and sometimes those with type 2 diabetes.
Targets for blood lipid concentrations suggested by European Diabetes Policy Group
| Low risk | At risk | High risk | |
| Serum total cholesterol: | |||
| mmol/l | <4.8 | 4.8-6.0 | >6.0 |
| mg/dl | <185 | 184-230 | >230 |
| Serum LDL cholesterol: | |||
| mmol/l | <3.0 | 3.0-4.0 | >4.0 |
| mg/dl | <115 | 115-155 | >155 |
| Serum HDL cholesterol: | |||
| mmol/l | >1.2 | 1.0-1.2 | <1.0 |
| mg/dl | >46 | 39-46 | <39 |
| Serum triglycerides: | |||
| mmol/l | <1.7 | 1.7-2.2 | >2.2 |
| mg/dl | <150 | 150-200 | >200 |
Other medications and alcohol
Some drugs and also a high alcohol intake disturb plasma lipids, and this aspect of treatment must be examined and if necessary modified.
Lifestyle measures
Smoking, weight reduction, and exercise are important. Patients should be given advice on low fat diets. Hypertension must be treated.
Lipid modifying drugs
Statins are the first line treatment for hypercholesterolaemia and fibrates for hypertriglyceridaemia. Statins and fibrates can be used alone or together for treating mixed hyperlipidaemia. Specialist advice should be taken on resistant or complex hyperlipidaemic states.
Targets for treatment
The current targets for cholesterol and other lipid fractions are the same for primary prevention in diabetes as for secondary prevention in people without diabetes:
Total cholesterol, <5.0 mmol/l
Fasting triglyceride, <2.0 mmol/l
LDL cholesterol, <3.0 mmol/l
High density lipoprotein (HDL) cholesterol, >1.1mmol/l.
The ratio HDL cholesterol/(total cholesterol−HDL cholesterol) should be >0.25. Alternatively, total cholesterol/HDL cholesterol should be <3.0.
There is much debate as to whether lipid lowering drugs are of any value if started in patients over the age of 75.
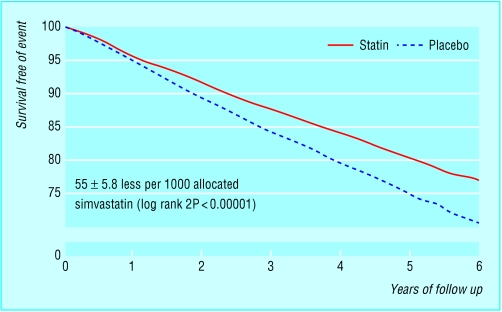
Heart protection study
This huge double blind trial of 20 000 people at increased risk of vascular disease examined the benefits of treatment with simvastatin 40 mg daily and reported its results in March 2002. The vascular event rate curves began to separate by the end of the first year, and the absolute benefits of treatment increased over time, becoming very obvious after five to six years. The benefits included:
Reduction in vascular deaths by 17%
Reduction in major vascular events by 24%
Reduction in strokes by 27%.
Treatment benefits were obvious not only among patients who had previously had a myocardial infarction but also in those with previous cerebrovascular or peripheral vascular disease. Benefits were also shown for diabetic patients without previous CHD. Both sexes benefited equally, and patients over 75 years benefited as much as younger patients.
The implications of these results for diabetic patients are obvious and offering statin treatment should be seriously considered.
Severe hyperlipidaemic states
Extreme mixed hyperlipidaemias are occasionally associated with uncontrolled diabetes. The plasma has a milky appearance, and xanthomata appear in the skin as bright yellow papules particularly at the elbows, knees, and buttocks. Even the retina assumes the pallor of lipaemia retinalis, described as “peaches and cream.” The condition normally resolves when glycaemic control is achieved; lipid concentrations often return to normal, and the xanthomata disappear. Most, but not all, patients have type 2 diabetes. The condition needs to be carefully monitored, and patients should take lipid lowering drugs until it resolves. Sometimes the drugs need to be continued indefinitely.
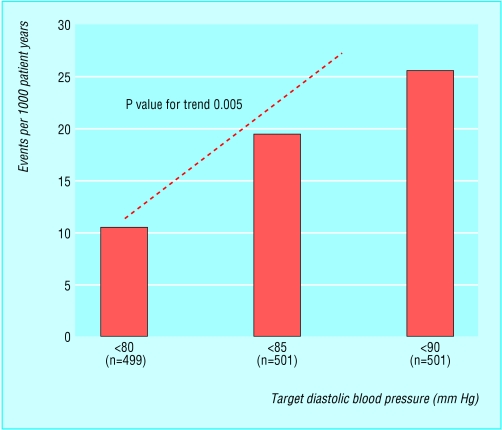
Figure.
Rates of serious cardiovascular events according to target diastolic blood pressure in 1500 patients with hypertension and type 2 diabetes
Figure.
Kaplan-Meier estimates of composite outcome of myocardial infarction, stroke, or death from cardiovascular causes in ramipril and placebo groups in HOPE study
Figure.
Simvastatin: vascular event by duration of follow up (from the heart protection study)
Figure.

Xanthomata on the knee from severe hyperlipidaemia
Acknowledgments
The histogram showing rates of serious cardiovascular events according to blood pressure in patients with hypertension and type 2 diabetes is adapted from Hansson, et al. Lancet 1998;351:1755-62. The figure showing Kaplan- Meier estimates of the composite outcome of myocardial infarction, stroke, or death from cardiovascular causes in the HOPE study is adapted from Yusuf et al. N Engl J Med 2000;342:145-53. The figure showing simvastatin: vascular event by follow up duration is adapted from the heart protection study website www.ctsu.ox.ac.uk/∼hps. The table showing some causes of secondary hyperlipidaemia is adapted from International Task Force for Prevention of Coronary Heart Disease. Nutr Metab Cardiovasc Dis 1992;2:113-56.
Footnotes
Peter J Watkins is honorary consultant physician, King's Diabetes Centre, King's College Hospital, London (peter.watkins1@virgin.net).