Abstract
Introduction
Cystic lesions in long bones are the radiological presentation of various bone pathologies, they can easily be misdiagnosed and thus mistreated; treatment varies from observation to aggressive surgical interventions based on the nature and characteristics of the lesion.
Case presentation
A 25-year-old male had a twisting injury to his ankle and his radiographs showed a cystic lesion in the distal tibia that was asymptomatic until he injured his ankle. he had persistent pain since then. and after conservative methods failure, a two-stage surgical intervention was done; first, we curetted the lesion and filled it with antibiotics cement; then the cement was removed with autologous bone grafting. The patient eventually healed and returned to his normal activity level.
Discussion
Brodie's abscess has a similar radiological appearance to other bone neoplasms and tumor-like lesions. Clinically, it is minimally symptomatic, and often initially misdiagnosed; surgical treatment is very effective, but it depends on the size, location, and aggressiveness of the lesion; the goal is to eliminate the infection, refill the residual gap, and restore the normal function, especially in weight-bearing bones.
Conclusion
Brodie's abscess is a hideous lesion that is hard to diagnose. It could mimic other tumor-like lesions. However, applying bone cement and a second stage of bone grafting might help maximize the treatment efficiency.
Keywords: Cystic lesions, Infection, Bone cement, Case report
Highlights
-
•
A distal tibial lesion discovered accidentally that could enter a vast differential diagnosis
-
•
Treated surgically in two stages utilizing the bone cement technique
-
•
Favorable outcome after 6 months follow-up
1. Introduction
1.1. Treatment of a Brodie's abscess manifesting as persistent pain after a twisting ankle injury: a case report
Cystic lesions in the appendicular skeleton constitute a significant percentage of musculoskeletal lesions [1]. These lesions may present incidentally and be diagnosed during medical consultation for unrelated issues and could be active asymptomatically until they manifest as a pathologic fracture such as a simple bone cyst. Alternatively, they can exhibit aggressive and destructive behavior like an aneurysmal bone cyst [2,3]. Additionally, cystic lesions could be caused by infections from various organisms: pyogenic or non-pyogenic bacteria, fungi, tuberculosis, or even parasites [4,5].
All these various pathologies may share a similar radiographic presentation on X-ray imaging. Due to the different management and treatment approaches based on the other pathology, it is crucial to make a correct diagnosis and follow a comprehensive approach to management. Since X-rays are not the most reliable method to distinguish between these, it is necessary to depend on other diagnostic criteria [3,6].
Therefore, a detailed history of complaint and a comprehensive clinical examination with a high index of suspicion are critical factors for establishing an accurate diagnosis. A radiological examination that starts with simple plain X-rays is beneficial but isn't sufficient on its own, as it has been reported that a malignant tumor like telangiectatic osteosarcoma could render a similar radiological picture to another benign lesion [7]. This article presents a case of a young patient with a lesion in the distal tibia that was incidentally discovered on post-trauma X-ray and later became symptomatic, necessitating surgical intervention, and it has been reported by SCARE 2023 standards [8].
2. Case presentation
A young, healthy 25-year-old smoker male with no past medical history complained of vague mild pain in his right ankle; during a soccer game, he had obtained a twisting injury to his right foot. He was able to bear weight, and considerable defined edema emerged on the lateral aspect of his ankle, he sought a medical consultant. He was diagnosed with an ankle ligament sprain in the emergency room. He was treated with an ankle brace with the classic RICE approach: rest, elevating the limb, ice, and compressive bandage application. But more importantly, a lesion in the distal tibia was identified, so he was asked to consult an orthopedic specialist for assurance. When he came to our clinic, he was normally walking a month after his initial injury. His ankle was stable, but a mild, ambiguous pain still existed in the anterior aspect of the distal tibia just above the ankle joint line.
On clinical examination, he had a normal pain-free range of motion of the ankle, no edema, local erythema, or redness was found, and his gait was normal, with a very mild uneasiness occasionally in his leg. The patient reported daily discomfort in his ankle; his AOFAS Ankle-Hindfoot Scale was 71. [9]
The rest of his musculoskeletal examination was unremarkable.
On plain x-ray, a cystic eccentric lytic well-defined lesion was identified in his distal tibia bone (Fig. 1). His labs were all within normal ranges. An MRI was ordered to evaluate the lesion further. It showed an osteolytic mass measuring 50*23*20 mm just above the distal tibia metaphysis with an eccentric location a heterogeneous content and no gadolinium enhancement. Erosion and thinning of the lateral cortex of the distal tibia were noticed with no evidence of soft tissue involvement.
Fig. 1.
Preoperative clinical and radiological images.
We, however, saw no need for a biopsy before definitive treatment, as our differential diagnosis was mainly composed of benign lesions due to the latent behavior of the lesion. The well-defined margins on the X-ray and no soft tissue involvement on MRI, so we suspected a chondromyxoid fibroma, non-ossifying fibroma, cold abscesses, and possibly an ABC.
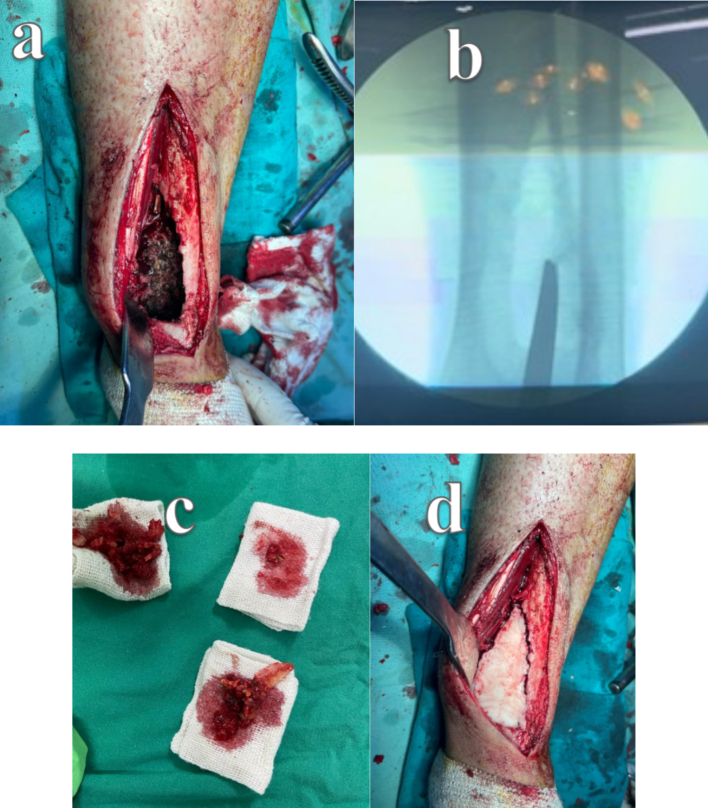
Under spinal anesthesia, with a tourniquet applied and inflated, an anterolateral approach to the distal tibia was made. After surgical dissection and periosteum elevation, a weak area of cortical bone was noticed, so we opened a window through it. A bloody yellowish tissue was curetted until a normal healthy bone was reached, and suspicion of an infection increased. The possibility of tuberculosis thrived, so after adequate aggressive curetting of the lesion, a hydrogen peroxide solution was used to clean the lesion further. A decision was made to fill the gap with cement as an initial stage until the result of histological study and cultures and sensitivity came out. So, a 40 g bone cement loaded with gentamycin was used to fill the gap, and closure was done (Fig. 2).
Fig. 2.
Intraoperative images from the first surgery: a: clinical image of the curetted lesion, b: intraoperative X-rays, c: the curettage material, d: a clinical image after filling the void with antibiotic bone cement.
Later, the histological study came in as bone fragments showing reactive changes and scanty acute inflamed fibrotic tissue, and no granulomas, necrosis, or neoplastic lesions were identified.
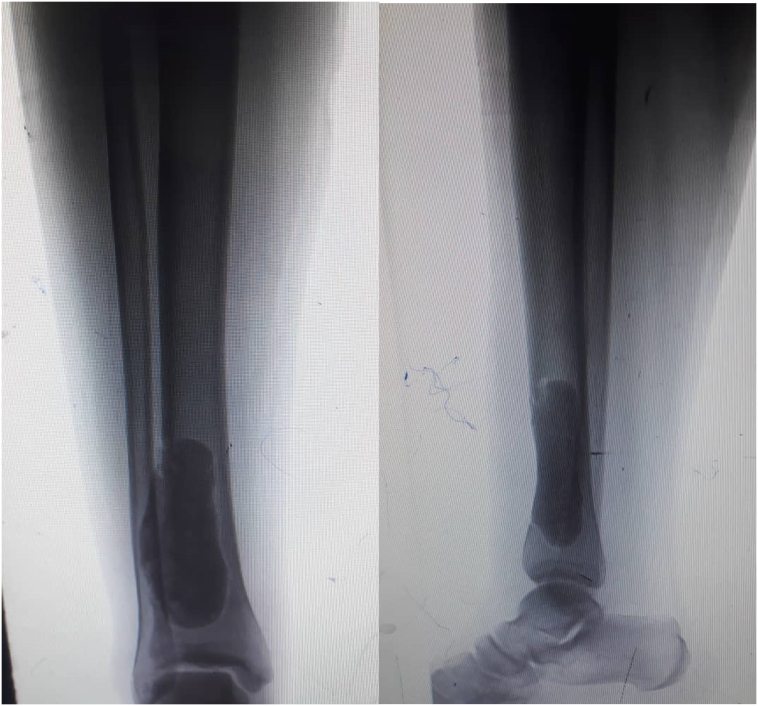
While the culture for tuberculosis came negative, it came positive for the growth of Staphylococcus aureus with sensitivity towards gentamycin, vancomycin, and linezolid, so an intravenous antibiotic regime was started after consultation with the infection control department. The patient took 1 g of vancomycin twice daily for a total of six weeks, and at that stage, the patient was cautiously weight-bearing with no pain and the radiographs showed no abnormalities (Fig. 3).
Fig. 3.
Follow-up anteroposterior and lateral X-rays 6 weeks after the surgery.
The patient underwent the second surgery three months after the first one when the bone cement was removed and an autologous cancellous bone graft from the iliac bone was utilized to fill the remaining gap (Fig. 4). (without prophylactic fixation). The patient was dismissed the next day of surgery with weight-bearing protection for six weeks and encouraged an immediate range of motion exercises. He followed a strengthening physiotherapy program, and two months after the second surgery, the graft showed progressive healing, and gradual weight-bearing was initiated. Until a normal gait was obtained six months after the surgery, his AOFAS became 90. His radiographs showed complete healing 9 months after the last surgery (Fig. 5).
Fig. 4.
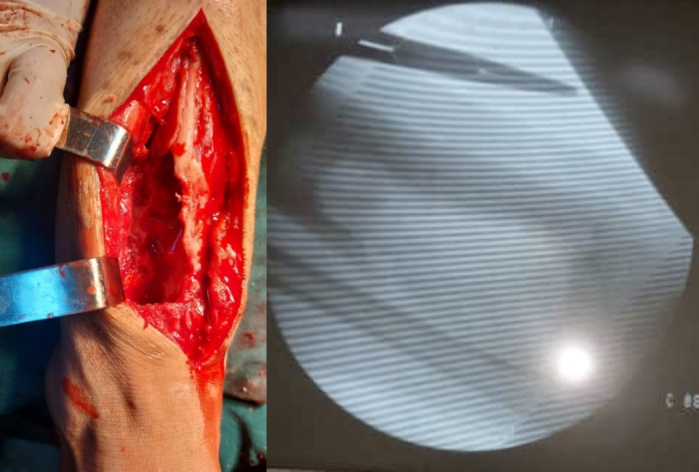
Intraoperative clinical and radiological images of the sec1ond surgery.
Fig. 5.
Follow-up radiographs 9 months after the last surgery showing full healing of the graft.
3. Discussion
It is well-known that infection is the great mimicker of orthopedic lesions, so having a high suspicion index is crucial. an infection should be in every differential diagnosis of a non-traumatic lesion in the musculoskeletal system [10].
In our case, we suspected infection, specifically considering tuberculosis as the challenging economic and health conditions in Syria made tuberculosis no longer a rare disease anymore and we previously encountered a similar case [11].
Since the lesion looked benign, we opted against an initial biopsy. Malignant tumors often exhibit more aggressive clinical behavior, rapid growth, more bone destruction, and potential invasion of surrounding soft tissues [12,13].
Our thought was chondromyxoid fibroma as the primary neoplastic given the patient's age and the heterogeneous content observed on the MRI. In contrast, non-ossifying fibroma tends to occur in immature skeletons. ABC has a more expansile appearance on X-rays and characteristic fluid levels on MRI [3,6]. Brodie's abscess was a possible diagnosis, but the very mild symptoms and normal labs with no history of an active infection did not take us that route.
Scott A. Alter Roy W. Sprinkle reported in 1995 a case of an 11-year-old female with a cystic lesion in the distal tibia involving the epiphysis of the medial malleolus. However, it was a little bit symptomatic with tenderness, redness, local temperature elevation, and elevated ESR that would raise the suspicion of infection. It was initially treated as a simple bone cyst, but during the curetting of the lesion, an amount of pus leaked through the bone window, so it was sent for culture and sensitivity and came back positive for Staph aureus. She was treated with Cefazolin for six weeks. After that, she underwent another surgery to fill the metaphyseal defect with a homogenous bone graft, which 9 months later showed good filling of the graft on x-rays [14].
In our case, a simple bone cyst was unlikely due to the patient's age and his skeletally mature. In the initial treatment stage, we preferred antibiotic-impregnated bone cement, which has proved effective in eradicating infection [15]. In the second stage, an autologous bone graft was used as the patient was skeletally mature and capable of providing enough bone graft without severe morbidity. However, we were dealing with a larger defect.
Cossio, A. et al. reported a bilateral Brodie's abscess in a 12-year-old male. The patient complained of pain in his left ankle following a sports injury, and he was diagnosed with a biopsy and treated accordingly with proper antibiotics. Still, he developed allergic reactions to the therapy. After the failure of this treatment, he was treated surgically with the curetting of the lesion and the application of an osteoconductive biomaterial in one stage. A good outcome was obtained at the final follow-up 17 months after the surgery [16].
It is advantageous to treat such cases in one stage. Biomaterials could be very helpful, but they are expensive and only available in some centers in third-world countries. Yet, it has been reported that the treatment of such infection with one stage without bone grafting as Lowe J et al. reported a case of a 14-year-old female with atraumatic constant tolerable pain in the proximal leg, x-rays revealed a lytic lesion in the proximal tibia, and after obtaining prober imaging modalities, a surgical procedure of one stage was done with debridement, irrigation, and antibiotics without bone grafting, but prolonged recovery was needed [17].
Chen, BC et al. reported a 50-year-old male who complained of atraumatic mild pain in his proximal tibia. Imaging and CT-guided biopsy confirmed the diagnosis of Brodie's abscess. He underwent surgical debridement and irrigation, and filling the gap with bone cement was the definitive treatment with proper antibiotics. With a favorable final outcome [18], we thought the definitive treatment with bone cement was risky in our case due to the young age and high level of activity of the patient and the enormous gap diameters, so we preferred to do a second bone grafting surgery and luckily it rendered an excellent outcome.
Staphylococcus aureus is the most common organism known to cause subacute osteomyelitis, frequently affects the tibia [19] but any bone could get infected, and cases have been reported in the humerus and the acromion [20,21].
Treatment mainly with curation, debridement, and antibiotics tailored to culture and sensitivity results often delivers successful treatment with a low recurrence rate [22], based on every case, a decision to apply antibiotics loaded, bone cement, or other biomaterials is made, and the need for a second stage to fill the gap is not necessary in all cases. It mainly depends on the size and location of the defects, as minor metaphyseal defects show good healing potentials.
4. Conclusion
Brodie's abscess is a hideous lesion that is hard to diagnose. It could mimic other tumor-like lesions, and adequate surgical debridement and irrigation with the correct antibiotics course could be an effective treatment. However, applying bone cement and a second stage of bone grafting might help enhance healing and recovery.
Consent
Written informed consent was obtained from the patient's parents/legal guardian for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
This study is exempt from ethical approval in our institution.
Funding
This research did not receive any specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Hakam Alasaad M.D: conceptualization, writing, and reviewing.
Doried al-diri M.D: investigation, data curation, writing, and editing.
Hassan ALSamman M.D: writing, and editing.
Jaber Ibrahim M.D PHD: conceptualization, investigation, data curation, writing, editing and reviewing.
Guarantor
Hakam al-asaad M.D.
Research registration number
N/A.
Declaration of competing interest
The author has no conflicts to disclose.
References
- 1.Uhl M., Adler C.P., Herget G.W. Tumorhnliche Knochenlsionen. Radiologe. 2004;44(10):1013–1025. doi: 10.1007/s00117-004-1114-9. [DOI] [PubMed] [Google Scholar]
- 2.Doganavsargil B., Ayhan E., Argin M., et al. Cystic bone lesions: histopathological spectrum and diagnostic challenges. Turkish Journal of Pathology. 2015 doi: 10.5146/tjpath.2014.01293. Published online. [DOI] [PubMed] [Google Scholar]
- 3.Subramanian S., Viswanathan V.K. 2022. Lytic Bone Lesions. [PubMed] [Google Scholar]
- 4.Rasool M.N. Osseous manifestations of tuberculosis in children. J. Pediatr. Orthop. 2001;21(6):749–755. [PubMed] [Google Scholar]
- 5.Abd El Bagi M.E., Sammak B.M., Al Shahed M.S., et al. Rare bone infections “excluding the spine”. Eur. Radiol. 1999;9(6):1078–1087. doi: 10.1007/s003300050794. [DOI] [PubMed] [Google Scholar]
- 6.Hipfl C., Schwabe P., Märdian S., Melcher I., Schaser K.D. Benigne zystische Knochenläsionen. Unfallchirurg. 2014;117(10):892–904. doi: 10.1007/s00113-014-2579-2. [DOI] [PubMed] [Google Scholar]
- 7.Zishan U.S., Pressney I., Khoo M., Saifuddin A. The differentiation between aneurysmal bone cyst and telangiectatic osteosarcoma: a clinical, radiographic and MRI study. Skeletal Radiol. 2020;49(9):1375–1386. doi: 10.1007/s00256-020-03432-w. [DOI] [PubMed] [Google Scholar]
- 8.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitaoka H.B., Alexander I.J., Adelaar R.S., Nunley J.A., Myerson M.S., Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 10.Lindenbaum S., Alexander H. Infections simulating bone tumors. A review of subacute osteomyelitis. Clin. Orthop. Relat. Res. 1984;184:193–203. [PubMed] [Google Scholar]
- 11.Alasaad H., Diri D., Mhana S.A.A., Muhammed H. Solitary distal tibia tuberculosis in a child, effectively treated by chemotherapy following surgery: a case report. Int. J. Surg. Case Rep. 2024;115 doi: 10.1016/j.ijscr.2024.109289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weber K., Damron T.A., Frassica F.J., Sim F.H. Malignant bone tumors. Instr. Course Lect. 2008;57:673–688. [PubMed] [Google Scholar]
- 13.von Eisenhart-Rothe R., Toepfer A., Salzmann M., Schauwecker J., Gollwitzer H., Rechl H. Primär maligne Knochentumoren. Orthopade. 2011;40(12):1121–1142. doi: 10.1007/s00132-011-1866-7. [DOI] [PubMed] [Google Scholar]
- 14.Alter S.A., Sprinkle R.W. Brodie’s abscess: a case report. J. Foot Ankle Surg. 1995;34(2):208–214. doi: 10.1016/S1067-2516(09)80047-1. [DOI] [PubMed] [Google Scholar]
- 15.Anderson G.M., Osorio C., Berns E.M., et al. Antibiotic cement utilization for the prophylaxis and treatment of infections in spine surgery: basic science principles and rationale for clinical use. J. Clin. Med. 2022;11(12):3481. doi: 10.3390/jcm11123481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cossio A., Graci J., Lombardo A.S., et al. Bilateral tibial Brodie’s abscess in a young patient treated with BAG-S53P4: case report. Ital. J. Pediatr. 2019;45(1):91. doi: 10.1186/s13052-019-0685-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lowe J., Bridwell R.E., Matlock A.G., Cibrario A., Oliver J. A case of Brodie’s abscess with tibial erosion and extravasation into surrounding soft tissue. Cureus. 2020 doi: 10.7759/cureus.8592. Published online June 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen B.C., Kobayashi T., O’Rourke H., Sekar P. Staphylococcus aureus osteomyelitis causing Brodie’s abscess of the tibia in an adult man. BMJ Case Rep. 2021;14(1) doi: 10.1136/bcr-2020-240836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kornaat P.R., Camerlinck M., Vanhoenacker F.M., de Praeter G., Kroon H.M. Brodie’s abscess revisited. JBR-BTR. 2010;93(2):81–86. [PubMed] [Google Scholar]
- 20.Vishwakarma N., Chauhan S., Binyala S.S., Singh S.K. Brodie’s abscess of the proximal humerus metaphysis: a case report. J Orthop Case Rep. 2021;11(9) doi: 10.13107/jocr.2021.v11.i09.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorter J., Rykov K., Ott P., van Raay J.J.A.M. Rare presentation of Brodie’s abscess in the acromion process and the value of the penumbra sign. BMJ Case Rep. 2017 doi: 10.1136/bcr-2016-217772. Published online January 30. bcr2016217772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olasinde A.A., Oluwadiya K.S., Adegbehingbe O.O. Treatment of Brodie’s abscess: excellent results from curettage, bone grafting and antibiotics. Singapore Med. J. 2011;52(6):436–439. [PubMed] [Google Scholar]