Abstract
BACKGROUND:
Reducing racial disparities in lung transplant outcomes is a current priority of providers, policymakers, and lung transplant centers. It is unknown how the combined effect of race and ethnicity, gender, and diagnosis group is associated with differences in 1-year mortality and 5-year survival.
METHODS:
This is a longitudinal cohort study using Standard Transplant Analysis Research files from the United Network for organ sharing. A total of 25,444 patients undergoing first time lung transplantation between 2006 and 2019 in the United States. The primary exposures were lung transplant recipient race and ethnicity, gender, and primary diagnosis group at listing. Multivariable regression models and cox-proportional hazards models were used to determine adjusted 1-year mortality and 5-year survival.
RESULTS:
Overall, 25,444 lung transplant patients were included in the cohort including 15,160 (59.6%) men, 21,345 (83.9%) White, 2,318 (9.1%), Black and Hispanic/Latino (7.0%). Overall, men had a significant higher 1-year mortality than women (11.87%; 95% CI 11.07–12.67 vs 12.82%; 95% CI 12.20%−13.44%). Black women had the highest mortality of all race and gender combinations (14.51%; 95% CI 12.15%−16.87%). Black patients with pulmonary vascular disease had the highest 1-year mortality (19.77%; 95% CI 12.46%−27.08%) while Hispanic/Latino patients with obstructive lung disease had the lowest (7.42%; 95% CI 2.8%−12.05%). 5-year adjusted survival was highest among Hispanic/Latino patients (62.32%) compared to Black (57.59%) and White patients (57.82%).
CONCLUSIONS:
There are significant differences in 1-year and 5-year mortality between and within racial and ethnic groups depending on gender and primary diagnosis. This demonstrates the impact of social and clinical factors on lung transplant outcomes.
Keywords: lung transplantation, disparities, clinical outcomes, lung transplant quality, lung transplant disparities
Achieving equitable organ allocation, distribution and post-transplant outcomes is a current priority of regulatory agencies, policymakers, and providers.1,2 Among the patient characteristics associated with lung transplant care and outcomes are underlying disease, gender, race, and ethnicity.3–7 For instance, prior studies of the Lung Allocation Score era have raised concern that women and racial and ethnic minorities have decreased odds of lung transplantation allocation and longer waitlist times.8 Additional work has demonstrated wide variation in lung transplant waitlist times and long-term outcomes by underlying disease.9 Furthermore, prior research has also raised concern that racial and ethnic minorities may have more severe underlying disease contributing to higher waitlist mortality and removal from the waitlist.10 However, to date, it is unknown how demographic factors, such as race and gender, intersect with underlying diagnosis to impact short-term surgical outcomes and long-term survival following lung transplantation.
Prior research assessing disparities in lung transplant outcomes have primarily focused on race, gender, or underlying disease in isolation with limited assessment of how these factors interact with each other. For instance, prior research has demonstrated that among older adults with idiopathic pulmonary fibrosis, men had significantly lower odds of survival compared to women.11 Furthermore, the only study to date assessing racial disparities in lung transplant outcomes have primarily compared White patients to non-White patients, without specific disaggregation of racial and ethnic groups, demonstrating no significant difference in lung transplant outcomes.12 However, given an increase in the number of racial and /ethnic minorities receiving lung transplants, there is a growing need for more granular evaluations of potential disparities in lung transplant post-operative mortality and survival. To date, no study has evaluated if there are differences in 1-year mortality and 5-year survival following lung transplant between and within racial and ethnic groups depending on primary diagnosis and gender.
The objective of this study is to evaluate how race and ethnicity, gender, and diagnosis group are associated with 1- and 5-year mortality following lung transplantation. We hypothesize that there is wide variation in outcomes between racial and ethnic groups and within a single racial and ethnic group depending on gender and primary diagnosis that have previously been underreported.
Methods
Data source and study population
We used the Organ Procurement and Transplant Network (OPTN) Standard Transplant Analysis and Research (STAR) file to identify patients who underwent lung transplantation from 2006 to 2019. The STAR file is a nationwide registry that collects transplant clinical characteristics and outcomes for all patients undergoing transplantation. Patients older than 18 years old undergoing either first time unilateral or bilateral lung transplantation were included. Patients undergoing multi-organ transplantation were excluded.
Patient race and ethnicity, gender, and diagnosis groups
All patient demographic and clinical information are collected at transplant centers in the United States using standardized worksheets by United Network for Organ Sharing (UNOS).13 The racial categories based on the Office of Management and Budget categories include White, Black, or African American, Native Hawaiian or Other Pacific Islander, American Indian, Asian and Hispanic/Latino on the candidate registration worksheet. For this analysis, only White, Black, Hispanic/Latino patients were included given small sample sizes of Native Hawaiian or Other Pacific Islander, American Indian and Asian patients, and due to the methodologic concerns of combining distinct racial and ethnic groups. Patient gender is also collected by the UNOS with male and female options. Prior research in lung transplantation have used either the terms sex or gender in analysis.10,13 In this study, we use the terms man/men and woman/women to represent the UNOS male and female respectively, given that there is no distinction between gender and sex on the registration forms. Primary diagnosis for each patient is defined at the time of listing and coded into 4 categories: obstructive, pulmonary vascular disease, cystic fibrosis, and restrictive disease.
Statistical analysis and outcomes
Outcomes
The primary outcomes of interest were 1-year mortality and 5-year survival. Dates of transplantation and patient outcomes were identified in the data set.
Analysis
We first assessed differences in baseline recipient and donor characteristics by racial group using ANOVA and chi-square test for continuous and categorical variables respectively. ANOVA was used to evaluate unadjusted differences in 1-and 5-year mortality differences between racial and ethnic groups, gender, and primary diagnosis. Next, we performed multivariable logistic regression to obtain adjusted predicted probability margins to assess differences in 1-year mortality between racial groups by gender and diagnosis groups. All 1-year outcome models have the same sample size of 22,641. We used interaction terms for race and ethnicity with gender as well as race and ethnicity with diagnosis group to assess the intersection of social and clinical factors. Additionally, we assessed trends in 1-year mortality by racial group over the study period by racial and ethnic group. Co-variates included in this model were both recipient, donor, and center level characteristics and were defined a priori based on clinical importance and prior investigations.10,12 Recipient characteristics included: age, LAS, HLA mismatch, medical condition (hospitalized in Intensive Care Unit, hospitalized non- Intensive Care Unit nonhospitalized), ischemic time, chronic steroid use, primary diagnosis group, transplant year. Donor characteristics included: age, body mass index, donor history of diabetes, creatinine. Center level volume (number of transplants done per year) was also included in our model.
Next, we performed time-to-event analysis using Cox proportional hazard regression analysis. For survival analyses, we started with 25,438 and then splitted the data to handle the interaction with time. The same recipient, donor and center level variables were included in order to generate adjusted Kaplan-Meier curves with survival functions. Proportional hazard assumptions were tested using Schoenfeld residuals for all co-variates included and demonstrated that recipient ischemic time, chronic steroid use, center volume and donor diabetes history and donor creatinine were not proportional over time. Therefore, we adjusted our model to account for these variables changing over time using log-transformed interaction with time for these co-variates. All statistical analyses were performed using STATA/MP 17.0 (State Corp., College Station, TX). Statistical significance was defined as p ≤ 0.05. This study was exempted by the University of Michigan Institutional Review Board.
Results
A total of 25,444 patients were included in the cohort including 15,160 (59.6%) men with a mean (SD) age of 56.0 (13.1) years old. The racial and ethnic composition of patients undergoing lung transplantation in the study period was 21,345 (83.9%) White, 2,318 (9.1%) Black, and 1,781 (7.0%) Hispanic/Latino. Patient characteristics for each racial and ethnic group are shown in Table 1. White patients had a significantly higher mean (SD) age (56.5[13.2]) compared to Black (53.4[11.0]) and Hispanic patients and 53.5(13.5); p < 0.001. Hispanic/Latino patients were less likely to have obstructive disease (White vs Black vs Hispanic/Latino: 30.7% vs 28.7% vs 8.0%; p < 0.001) and Black patients were less likely to have cystic fibrosis (White vs Black vs Hispanic/Latino: 12.3% vs 2.6% vs 6.0%; p < 0.001).
Table 1.
Recipient and Donor Characteristics by Race and Ethnic Group
| Total n = 25,444 | Non-Hispanic White n = 21,345 (83.9%) | Non-Hispanic Black n = 2,318 (9.1%) | Hispanic n = 1,781 (7.0%) | p-value | |
|---|---|---|---|---|---|
| Recipient characteristics | |||||
| Age (SD) | 56.0 (13.1) | 56.5 (13.2) | 53.4 (11.0) | 53.5 (13.5) | <0.001 |
| Body mass index (SD) | 25.3 (4.6) | 25.2 (4.6) | 26.1 (4.5) | 25.9 (4.5) | <0.001 |
| Male, n (%) | 15,160 (59.6%) | 13,038 (61.08%) | 1,077 (46.5%) | 2,045 (58.7%) | <0.001 |
| Diagnosis group, n (%) | |||||
| Obstructive lung disease | 7,371 (29.0%) | 6,562 (30.7%) | 666 (28.7%) | 143 (8.0%) | <0.001 |
| Pulmonary vascular disease | 881 (3.5%) | 650 (3.1%) | 138 (6.0%) | 93 (5.2%) | |
| Cystic fibrosis | 2,793 (11.0%) | 2,627 (12.3%) | 59 (2.6%) | 107 (6.0%) | |
| Restrictive lung disease | 14,399 (56.6%) | 11,506 (53.9%) | 1,455 (62.8%) | 1,438 (80.7%) | |
| Medical condition at transplant, n (%) | |||||
| ICU | 2,933 (11.5%) | 2,368 (11.1%) | 277 (12.0%) | 288 (11.5%) | <0.001 |
| Hospitalized | 2,394 (9.4%) | 1,945 (9.1%) | 252 (10.9%) | 197 (11.1%) | |
| Not-hospitalized | 2,0117 (79.1%) | 17,032 (79.8%) | 1,789 (77.2%) | 1,296 (72.8%) | |
| Clinical status at transplant | |||||
| Creatinine (SD) | 0.9 (0.4) | 0.9 (0.4) | 0.9 (0.4) | 0.8 (0.3) | <0.001 |
| Total bilirubin (SD) | 0.61 (1.0) | 0.61 (1.0) | 0.58 (0.8) | 0.61 (1.1) | 0.33 |
| LAS (SD) | 42.5 (15.2) | 41.8 (14.9) | 44.8 (15.6) | 47.7 (16.3) | <0.001 |
| FEV1 % predicted (SD) | 39.3 (20.9) | 39.2 (21.3) | 38.7 (18.7) | 41.4 (18.4) | <0.001 |
| Number of HLA mismatches(SD) | 4.6 (1.1) | 4.6 (1.1) | 4.9 (1.0) | 4.7 (1.1) | <0.001 |
| Ischemic time (SD) | 5.3 (1.9) | 5.3 (1.9) | 5.4 (1.9) | 5.0 (1.7) | <0.001 |
| Requiring mechanical ventilation, n (%) | 1,625 (6.4%) | 1,356 (6.4%) | 122 (5.3%) | 147 (8.25%) | <0.001 |
| Diabetes, n (%) | 5,048 (19.8%) | 4,048 (19.0%) | 504 (21.7%) | 496 (27.9%) | <0.001 |
| Dialysis after listing, n (%) | 117 (0.5%) | 87 (0.4%) | 12 (0.5%) | 18 (1.0%) | 0.004 |
| Chronic steroid use, n (%) | 11774 (46.3%) | 94,68 (44.4%) | 1,371 (59.2%) | 935 (52.5%) | <0.001 |
| Functional status at transplant, n (%) | |||||
| Total independence (%) | 22.0% | 23.1% | 17.5% | 14.20% | <0.001 |
| Some or total assistance (%) | 78.0% | 76.8% | 82.5% | 85.80% | |
| Donor characteristics | |||||
| Age (SD) | 34.8 (14.0) | 34.7 (14.1) | 35.1 (13.7) | 35.4 (14.2) | 0.07 |
| Body mass index (SD) | 26.2 (5.4) | 26.1 (5.4) | 26.4 (5.7) | 26.2 (5.6) | 0.11 |
| Creatinine (SD) | 1.4 (1.5) | 1.4 (1.5) | 1.4 (1.5) | 1.4 (1.6) | 0.96 |
| Donor PO2 on 100% oxygen | 379.1 (145.1) | 380.0 (144.6) | 378.9 (145.8) | 369.1 (150.5) | 0.01 |
| Diabetes, n (%) | 1,972 (7.8%) | 1,657 (7.8%) | 173 (7.5%) | 142 (8.0%) | 0.82 |
| Donor cause of death, n (%) | |||||
| Anoxia | 5,488 (21.6%) | 4,633 (21.7%) | 479 (20.7%) | 376 (21.1%) | <0.001 |
| Cerebrovascular accident | 8,119 (31.9%) | 6,613 (31.0%) | 820 (35.4%) | 686 (38.5%) | |
| Head trauma or CNS tumor | 11,261 (44.3%) | 9,603 (45.0%) | 966 (41.7%) | 692 (38.9%) | |
| Other | 575 (2.3%) | 495 (2.3%) | 53 (2.3%) | 27 (1.5%) |
Overall, there were significant differences in unadjusted 1-year mortality by race, gender, and diagnosis groups (Table S1). Specifically, there was significant differences in unadjusted 1-year mortality for Black (13.63%) White (12.99%) and Hispanic/Latino (11.06%) patients (p < 0.037). Women had lower mortality than men (12.08% vs 13.47%; p < 0.001). Lastly, there was a significant difference in 1-year mortality by primary disease: pulmonary vascular disease (15.89%) restrictive disease (14.17%), obstructive disease (11.25%), cystic fibrosis (9.8%) (p < 0.001).
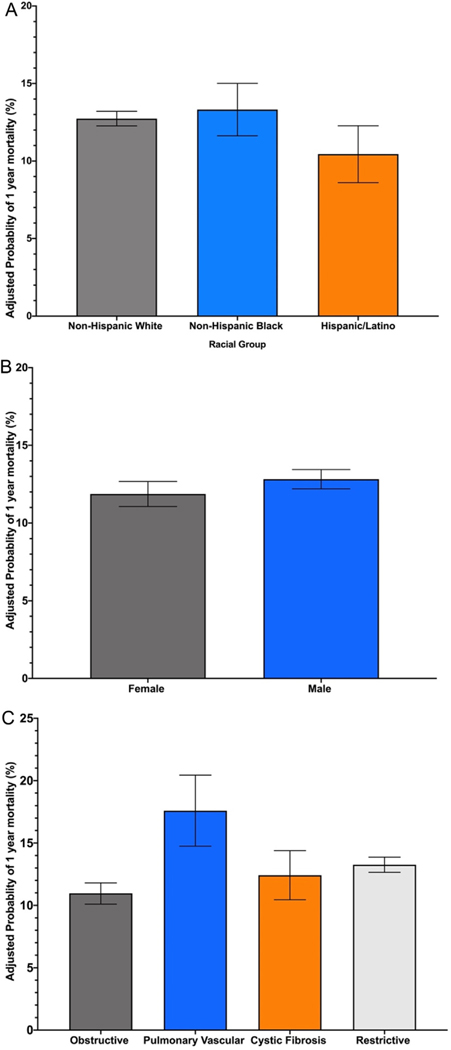
On adjusted analysis, we also found significant differences by racial and ethnic group, gender, and primary diagnosis (Figures 1A–1C). Black patients had higher 1-year mortality (13.32%; 95% CI 11.63%−15.01%) compared to White (12.75%; 95% CI 12.27%−13.21%) and Hispanic/Latino (10.45%; 95% CI 8.61%−12.28%) patients. Men had higher mortality compared to women (11.87%; 95% CI 11.07–12.67 vs 12.82%; 95% CI 12.20%−13.44%). There was also significant variation by diagnosis group with patients with pulmonary vascular disease having the highest mortality (17.59%; 95% CI 14.74%−20.44%) followed by restrictive disease (13.26%; 95% CI 12.65%−13.87%), cystic fibrosis (12.42%; 95% CI 10.45%−14.39%), and obstructive disease (10.96%; 95% CI 10.10%−11.81%).
Figure 1.
A. Adjusted 1-year mortality by race and ethnicity. B. Adjusted 1-year mortality by gender. C. Adjusted 1-year mortality by primary diagnosis group.
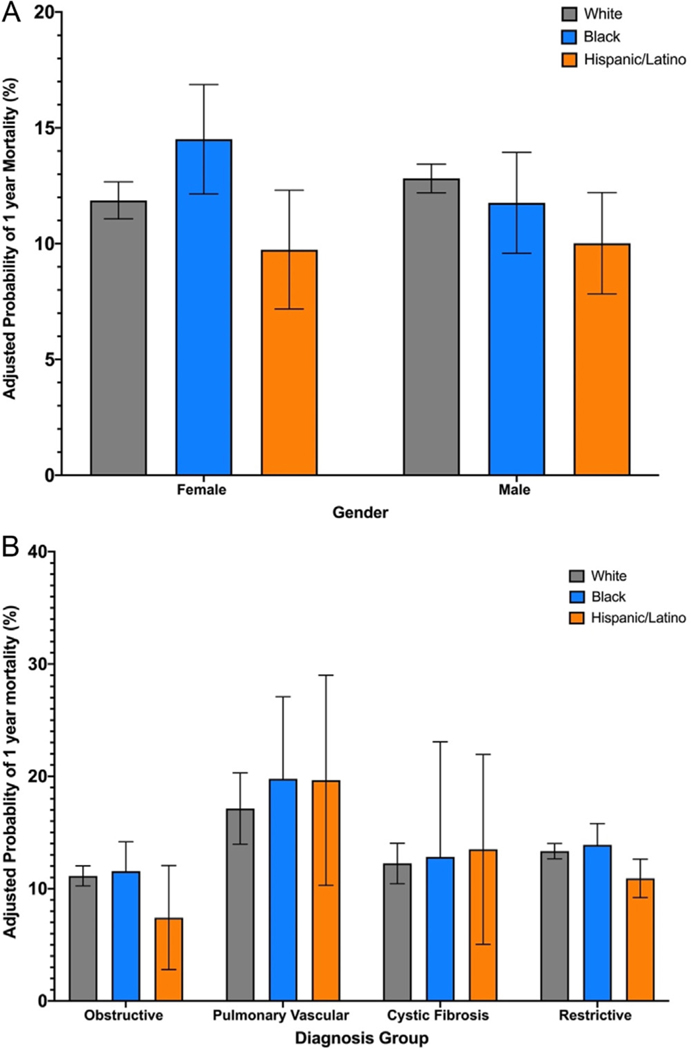
The differences in 1-year mortality when assessing the intersection of race with gender and diagnosis group demonstrated additional variation. The intersection of race and ethnicity and gender is demonstrated in Figure 2A. Black women had the highest mortality of all gender and race and ethnicity combinations (14.51%; 95% CI 12.15%−16.87%), which was higher than Black men (11.76%; 95% CI 9.59%−13.94% vs 11.76%; 95% CI 12.15–16.87%) as well as White women (11.87%; 95% CI 11.07%−12.67%) and Hispanic/ Latino women (9.7%; 95% CI 7.18%−12.31%). Among men, White men had the highest mortality rate among men (12.82%; 95% CI 12.20%−13.44%). The intersection of race and diagnosis group is demonstrated that Black patients with pulmonary vascular disease had the highest mortality (19.77%; 95% CI 12.46%−27.08%) while Hispanic/Latino patients with Obstructive lung disease had the lowest mortality (7.42%; 95% CI 2.8%−12.05%) (Figure 2B). Notably, for all diagnosis groups besides cystic fibrosis, Black patients had higher 1-year mortality. Overall, there was a significant change in 1-year mortality among all racial/ethnic groups in the study period (Figure S1).
Figure 2.
A. Adjusted 1-year mortality by race, ethnicity and gender. B. Adjusted 1-year mortality by race, ethnicity and primary diagnosis group.
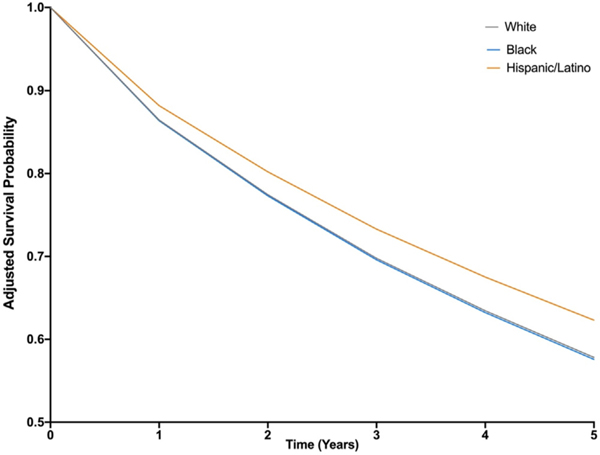
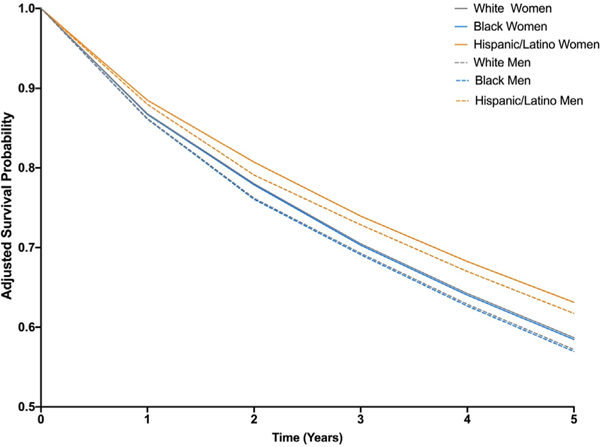
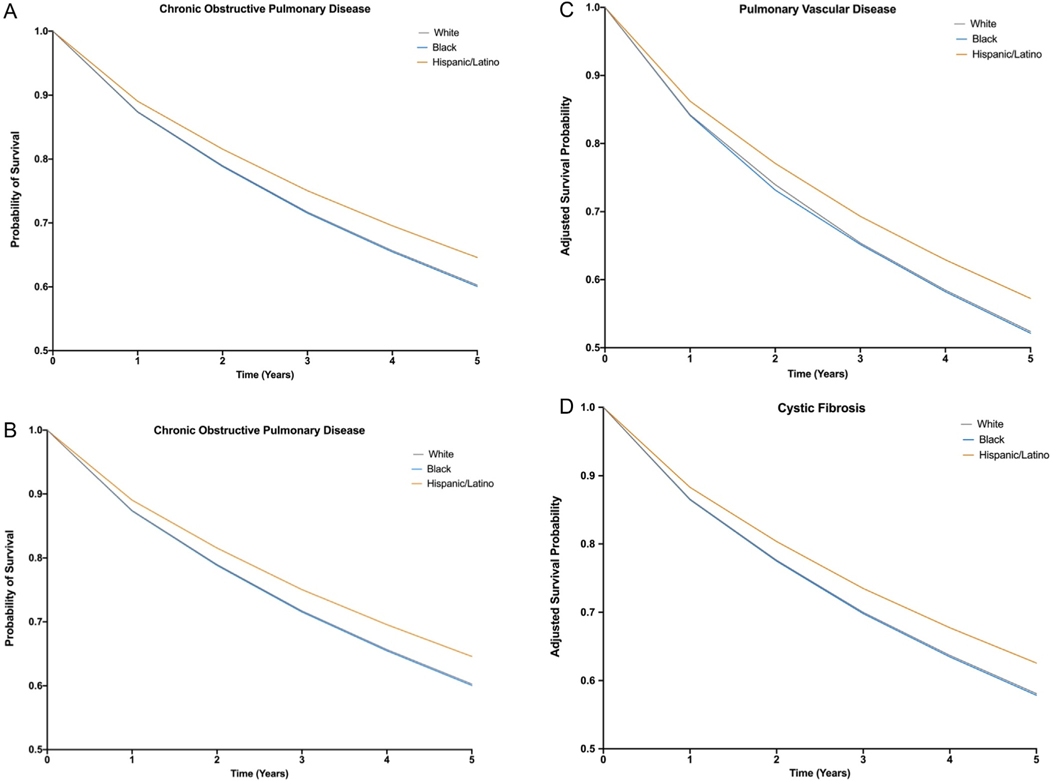
On assessment of 5-year survival, we found significant differences by race and ethnicity. Adjusted 5-year survival for Black patients was 57.59% compared to 57.82% for White patients and 62.32% for Hispanic/Latino patients (Figure 3). A similar trend of Black patients having the lowest survival 5-year survival and Hispanic/Latino patients with the highest survival was seen within each gender (Figure 4) and diagnosis group [Figure 5A–D]. However, there was significant variation in 5-year survival between diagnosis groups. Diagnosis of pulmonary vascular disease was associated with lowest 5-year survival for Black (52.14%), White (52.39%) and Hispanic/Latino patients (57.23%). Diagnosis of obstructive disease had the highest 5-year survival for Black (60.05%), White (60.28%) and Hispanic patients (64.40%).
Figure 3.
Adjusted 5-year survival curve by race and ethnicity.
Figure 4.
Adjusted 5-year survival curve by race, ethnicity, and gender.
Figure 5.
A. Adjusted 5-year survival curve by race and ethnicity among patients with chronic obstructive pulmonary disease. B. Adjusted 5-year survival curve by race and ethnicity among patients with restrictive lung disease. C. Adjusted 5-year survival curve by race and ethnicity among patients with pulmonary vascular lung disease. D. Adjusted 5-year survival curve by race and ethnicity among patients with cystic fibrosis.
Lastly, there were several recipient and donor factors with significant associations to 5-year survival (Table S2). Recipient characteristics associated with decreased survival included age (HR 1.01; 95% CI 1.01–1.01), chronic steroid use (HR 1.16; 95% CI 1.11–1.22%), lung allocation score (1.01; 95% CI 1.00–1.01; p < 0.001), number of HLA mismatches (HR1.07;95% CI 1.04–1.09; p < 0.001). Compared to obstructive disease, pulmonary vascular disease (HR 1.17; 95% 1.03–1.32; p < 0.001) and restrictive disease (HR 1.16; 95% CI 1.11–1.22; p < 0.001) were associated with lower 5-year survival. Donor age (HR 1.00; 95% CI 1.00–1.01) and diabetes (HR 1.19; 95% CI 1.10–1.28; p < 0.001) were associated with lower recipient 5-year survival as well.
Discussion
Our findings improve our understanding of lung transplantation disparities by assessing the intersection of race, gender, and diagnosis group. First, evaluation of the combined effect of race and gender on 1-year mortality found that Black women had the highest overall 1-year mortality followed by white men, despite men broadly having an overall higher mortality rate compared to women. Second, we found that for all racial groups’ women had higher 5-year survival compared to men. Third, we found that Black and White patients had similar 5-year survival for all diagnosis groups but that their survival was lower than Hispanic/Latino patients. Last, we found that patients with pulmonary vascular disease and restrictive disease had the lowest survival.
Prior work evaluating gender and racial and ethnic disparities lung transplant outcomes has primarily focused on these social factors independently with limited assessment of both 1-year mortality and 5-year survival. For instance, Liu et al previously demonstrated no differences in lung transplant survival between non-White and White patients between the years of 2005 and 2009. We expand upon this work by disaggregating Black and Hispanic/Latino patients for more granular assessment of survival by racial and ethnic group.12 In addition, we present the first assessment demonstrating within racial group differences in both 1-year mortality and 5-year survival depending on gender and diagnosis group. Specifically, we found that Black women had the highest overall mortality across all combinations of race and gender despite frequently cited papers detailing that women overall have lower post-transplant mortality and higher survival compared to men.14 So, while overall our findings replicate prior work demonstrating that overall men have higher 1-year mortality, the additional evaluation of the interaction of gender, race and ethnicity highlights that Black women have the worst short-term lung transplantation outcomes. This is particularly important given that a majority of Black lung transplant recipients were women in our cohort. This highlights how assessment of disparities by gender or race alone may underestimate true disparities by small sub-populations. To date, no prior investigation in lung transplantation has demonstrated this finding that Black women have the highest short-term mortality. However, prior assessments of other solid organ transplantation have demonstrated higher rates of early graft failure in liver transplant among Black women and overall worst survival and graft function among Black patients broadly for heart, liver, and kidney transplant.15–18 Future work is needed to understand how recipient characteristics may interact with provider and system factors contributing to worse outcomes among Black women. Lastly, this finding highlights the need to move beyond the assessment of isolated social and clinical factors on outcomes and rather evaluate their intersection to identify the most at-risk populations, who should be targeted for quality initiatives within transplantation care.
In our cohort, Hispanic/Latino patients had the lowest 1-year mortality and highest 5-year survival following lung transplantation. Prior work has demonstrated that waitlist mortality is higher among Hispanic/Latino candidates after adjusting for diagnosis, age, and gender, which may be related to the lower 1-year mortality and higher survival seen in our cohort.10 This raises concern of selection bias in our transplant cohort due to an underrepresentation of the broader population of Hispanic/Latino patients listed given higher mortality of waitlist candidates. In addition, there are well documented disparities in access to renal and liver transplantation among Hispanic and Latino patients and it is possible that similar barriers to lung transplantation exist upstream skewing the clinical and social characteristics of Hispanic and Latino patients who undergo lung transplantation.19 Prior work in renal and liver transplantation have demonstrated similar finding termed the “Hispanic Paradox”.20–22 This is a phenomenon that finds that Hispanic/Latino patients experience similar or better outcomes across a range of disease and health contexts compared to non-Hispanic White patients.22 Prior assessment of this phenomena in renal transplant has identified young age at transplant, receiving higher proportion of living donor grafts, and higher proportion of primary compared re-transplant in addition to protective social and cultural factors as reasons potentially contributing to this finding in renal transplant outcomes.20 Our findings highlight the need for future investigations into why this pattern in lung transplantation exist, especially with further assessment into how outcomes may vary between specific Hispanic/Latino ethnic sub-groups given the large heterogeneity that exist among Hispanic/Latino patient cohorts.
Our findings that racial disparities exist in mortality and mortality have important implications for clinical practice and policy. First, it provides the first insight into previously undescribed disparities that providers should be aware of and assess within their own transplant centers. Second, our findings demonstrate the need for standardized stratification of transplantation outcomes in order to unmask potential disparities.23 Assessing health equity in transplantation using unitary social factors such as race, or gender alone may be ineffective in identify true disparities occurring within subgroups. Recently, the Center for Medicaid and Medicare services has moved towards presenting clinical outcomes and quality measures by intersectional groups and it possible that UNOS would benefit from a similar process.24 Notably, over the study period, it was found that 1-year mortality following lung transplantation improved for all racial and ethnic groups. Therefore, ongoing efforts to improve lung transplantation quality through policy or quality improvement efforts should evaluate the effect of initiatives on both overall quality and mitigation of disparities.
Limitations
Our results should be considered in light of several limitations. First, the Organ Procurement and Transplant Network Standard Transplant Analysis and Research data used for this analysis is collected and reported by each transplant center. It is possible that errors in data collection or entry may exist at transplant centers leading to some missing values for lung transplant recipients. However, this data is heavily audited for reporting and is the most reliable source of transplant data that we currently have in the United States. Second, our analysis included White, Black and Hispanic/Latino patients limiting the generalizability to other racial and ethnic groups. However, given that this is the first analysis to disaggregate racial and ethnic minority groups, our work supplements prior literature assessing disparities in presurgical transplantation outcomes among these particular racial and ethnic groups. Third, while race, and ethnicity data is collected by each individual transplant center with standardized recipient forms, there may be variability in how this data is collected at each center. Fourth, while we included clinical important donor and recipient characteristics in our analysis, it is possible that unmeasured confounding could explain differences found between groups.
Conclusions
In summary, we found that significant variation in mortality and survival occurred between White, Black, and Hispanic patients and within each individual racial and ethnic group depending on gender as well as primary diagnosis. Contrary to prior literature, we found that Black women the worst 1-year mortality rates after lung transplantation. Future analysis of transplantation outcomes should continue to evaluate how the combination of both social and clinical factors impact the continuum of lung transplantation care and out-comes to ensure that high quality medical and surgical care are achieved for all patients.
Supplementary Material
Financial support
Sidra Bonner receives funding from the NIH T32 Multidisciplinary Program in Lung Disease at the University of Michigan (NHLBI T32HL007749). Valeria Valbuena is supported by the Institute for Healthcare Policy and Innovation Clinician Scholars Program and the National Institutes of Health (5T32HS000053-29)
Footnotes
Disclosure statement
The authors have no disclosures to report.
Supplementary materials
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.healun.2023.02.1496.
References
- 1.Stewart DE, Wilk AR, Toll AE, et al. Measuring and monitoring equity in access to deceased donor kidney transplantation. Am J Transplant 2018;18:1924–35. 10.1111/ajt.14922. [DOI] [PubMed] [Google Scholar]
- 2.National Research Council. Realizing the promise of equity in the organ transplantation system. Washington, DC: The National Academies Press; 2022. [PubMed] [Google Scholar]
- 3.Lingaraju R, Pochettino A, Blumenthal NP, et al. Lung transplant outcomes in white and African American recipients: special focus on acute and chronic rejection. J Heart Lung Transplant 2009;28:8–13. 10.1016/j.healun.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Lehr CJ, Skeans M, Dasenbrook E, et al. Effect of including important clinical variables on accuracy of the lung allocation score for cystic fibrosis and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2019;200:1013–21. 10.1164/rccm.201902-0252OC. [DOI] [PubMed] [Google Scholar]
- 5.Yusen RD, Lederer DJ. Disparities in lung transplantation. J Heart Lung Transplant 2013;32:673–4. 10.1016/j.healun.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 6.Lederer DJ, Benn EK, Barr RG, et al. Racial differences in waiting list outcomes in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2008;177:450–4. 10.1164/rccm.200708-1260OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lederer DJ, Caplan-Shaw CE, O’Shea MK, et al. Racial and ethnic disparities in survival in lung transplant candidates with idiopathic pulmonary fibrosis. Am J Transplant 2006;6:398–403. 10.1111/j.1600-6143.2005.01205.x. [DOI] [PubMed] [Google Scholar]
- 8.Riley LE, Lascano J. Gender and racial disparities in lung transplantation in the United States. J Heart Lung Transplant 2021;40:963–9. 10.1016/j.healun.2021.06.004. [DOI] [PubMed] [Google Scholar]
- 9.OPTN/SRTR 2020 Annual data report: lung. Available at: https://onlinelibrary.wiley.com/doi/10.1111/ajt.16991 Published March 10, 2022. Accessed March 16, 2022. [Google Scholar]
- 10.Mooney JJ, Hedlin H, Mohabir P, Bhattacharya J, Dhillon GS. Racial and ethnic disparities in lung transplant listing and waitlist outcomes. J Heart Lung Transplant 2018;37:394–400. 10.1016/j.healun.2017.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mason DP, Brizzio ME, Alster JM, et al. Lung transplantation for idiopathic pulmonary fibrosis. Ann Thorac Surg 2007;84:1121–8. 10.1016/j.athoracsur.2007.04.096. [DOI] [PubMed] [Google Scholar]
- 12.Liu V, Weill D, Bhattacharya J. Racial disparities in survival after lung transplantation. Arch Surg 2011;146:286–93. 10.1001/archsurg.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United Network of Organ Sharing Transplant Forms. Lung transplant registrant forms. Available at: https://unos.org/wp-content/uploads/Adult-TCR-Lung.pdf [Google Scholar]
- 14.Loor G, Brown R, Kelly RF, et al. Gender differences in long-term survival post-transplant: a single-institution analysis in the lung allocation score era. Clin Transplant 2017;31. 10.1111/ctr.12889.10.1111/ctr.12889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dave S, Dodge JL, Terrault NA, Sarkar M. Racial and ethnic differences in graft loss among female liver transplant recipients. Transplant Proc 2018;50:1413–23. 10.1016/j.transproceed.2018.02.059. PMID: 29880364; PMCID: PMC6545290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris AA, Kransdorf EP, Coleman BL, Colvin M. Racial and ethnic disparities in outcomes after heart transplantation: a systematic review of contributing factors and future directions to close the outcomes gap. J Heart Lung Transplant 2016;35:953–61. 10.1016/j.healun.2016.01.1231. Epub 2016 Feb 12. PMID: 27080415; PMCID: PMC6512959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ross-Driscoll K, Kramer M, Lynch R, Plantinga L, Wedd J, Patzer R. Variation in racial disparities in liver transplant outcomes across transplant centers in the United States. Liver Transpl 2021;27:558–67. 10.1002/lt.25918. Epub 2020 Dec 11. PMID: 33037711; PMCID: PMC8201428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gordon EJ, Ladner DP, Caicedo JC, Franklin J. Disparities in kidney transplant outcomes: a review. Semin Nephrol 2010;30:81–9. 10.1016/j.semnephrol.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gordon EJ, Lee J, Kang R, et al. Hispanic/Latino disparities in living donor kidney transplantation: role of a culturally competent transplant program. Transplant Direct 2015;1:e29.. 10.1097/TXD.0000000000000540. PMID: 27500229; PMCID: PMC4946478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon EJ, Caicedo JC. Ethnic advantages in kidney transplant outcomes: the Hispanic Paradox at work? Nephrol Dial Transplant 2009;24:1103–9. 10.1093/ndt/gfn691. Epub 2008 Dec 15. PMID: 19075197; PMCID: PMC2721429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atiemo K, Mazumder NR, Caicedo JC, et al. The Hispanic Paradox in patients with liver cirrhosis: current evidence from a large regional retrospective cohort study. Transplantation 2019;103:2531–8. 10.1097/TP.0000000000002733. PMID: 30951016; PMCID: PMC6774922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health 2013;103(3):e52–60. 10.2105/AJPH.2012.301103. Epub 2013 Jan 17. PMID: 23327278; PMCID: PMC3673509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014;110:10–7. [DOI] [PubMed] [Google Scholar]
- 24.The Centers for Medicare and Medicaid Services:Office of Minority Health. Stratified reporting CMS. Last modified 01/03/2022. Accessed March 20, 2022. Available at: https://www.cms.gov/About-CMS/Agency-Information/OMH/research-and-data/statistics-and-data/stratified-reporting
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.