Abstract
Background
The role of biceps tenodesis (BT) during open reduction internal fixation (ORIF) of proximal humerus fractures (PHFs) remains unclear. A subset of patients undergoing ORIF have persistent pain with unclear etiology. The purpose of our study was to compare outcomes of ORIF of PHFs with and without concomitant BT. We hypothesize patients undergoing BT at the time of ORIF will have improved patient-reported outcome scores with fewer secondary procedures related to treatment of the biceps.
Methods
In this retrospective cohort study, all patients undergoing ORIF for a PHF at a single level one trauma center from January 2019 to June 2022 were reviewed. Patients under the age of 18 were excluded. Primary outcomes were patient-reported outcomes measurement information system physical function, depression, and pain interference scores at 5 time points up to final follow-up. Secondary outcomes included total operative time, complications, subsequent procedures, steroid injections, and range of motion. Chi-square tests were performed for categorical values and paired t-tests for continuous variables.
Results
71 patients met inclusion criteria: 41 undergoing ORIF without BT and 30 undergoing ORIF with BT. Average follow-up was 11 months. There were no statistically significant differences in patient demographics between groups. There were no differences in patient-reported outcomes measurement information system scores at any time point postoperatively. At final follow-up patients in the ORIF with BT group had higher forward flexion than those who did not undergo BT (142 vs. 123 degrees, respectively, P < .02). There were no differences in surgical time, revision rates, postsurgical complications, or postoperative injections between groups.
Conclusion
BT performed during ORIF of PHFs did not result in significantly different functional or patient-reported outcomes between groups, except for greater forward flexion at final follow-up. Although BT was done more commonly in severe PHFs, patients in both groups had similar rates of subsequent biceps-related procedures and revision surgery.
Keywords: Biceps tenodesis, Open reduction internal fixation, Proximal humerus, Fracture, PROMIS scores, Outcomes, Surgical treatment
Proximal humerus fractures (PHFs) comprise 5% of fractures in adults and typically occur following a low-energy mechanical fall.12 These fractures are increasing with an aging society, and as a result are projected to increase 15% per year.3 Fracture follow typical patterns which are closely related to the rotator cuff insertion sites.5 Fracture “parts” include the articular head, greater and/or lesser tuberosities, and the humeral shaft, all of which displace in the direction of muscular pull.6 Although typically fracture lines do not cross the bicipital groove, long head biceps entrapment is possible and extra-articular biceps ruptures have been reported after PHF.9
Surgical treatment of PHFs with open reduction internal fixation (ORIF) can improved healing and fracture alignment; however, consistent improvements in range of motion (ROM) and postsurgical pain can be variable.10 Biceps tenotomy/tenodesis is routinely performed during total shoulder arthroplasty, and in cases of arthroplasty to treat fractures, tenotomy/tenodesis is done to avoid tendon entrapment and mitigate risks of further surgery. A level 1 prospective study showed significantly lower pain scores and higher Constant scores when biceps tenodesis (BT) was performed during hemiarthroplasty for severe PHFs.4 However, rates of BT/tenotomy during ORIF of PHF are variable and rarely reported.2 A histological study evaluating immunohistochemical changes to the long head of the biceps tendon (LHBT) in the setting of PHFs found cellular changes including increased neural differentiation and neoangiogenesis, indicating it as a potential source of pain.12
Perhaps utility exists in intervening on the biceps tendon at the time of index ORIF, ideally avoiding a secondary BT for biceps-related pain. However, evidence has not been well defined regarding concomitant treatment of the biceps during surgical treatment of displaced PHF. In the present study, we aim to investigate patient-reported outcome scores, pain, and ROM following ORIF of PHF with and without BT. We hypothesize patients undergoing BT at the time of ORIF will have improved patient-reported outcomes, pain, and ROM postoperatively with fewer secondary procedures related to treatment of the biceps.
Methods
Patient selection
Following institutional review board approval, all patients undergoing ORIF for PHF at a single level-one trauma center were retrospectively reviewed. Patients undergoing surgery from 1/1/2019 through 6/1/2022 were included. The following Current Procedural Terminology codes were used to determine our initial study population for study eligibility: 23615 (Open treatment of proximal humeral fracture, includes internal fixation, when performed, includes repair of tuberosity(s), when performed), 23616 (Fracture and/or Dislocation Procedures on the Shoulder), 23430 (Repair, Revision, and/or Reconstruction Procedures on the Shoulder), and 29828 (Endoscopy/Arthroscopy Procedures on the Musculoskeletal System).
Patient charts were reviewed to determine if they had undergone concurrent BT with ORIF. Patients were then divided into two groups, those undergoing ORIF without BT or ORIF with concurrent BT. Demographics, medical comorbidities, fracture characteristics, and outcome data were collected from hospital records. Patients under the age of 18 and those with less than 3 months of follow-up were excluded from the study.
Surgical technique (ORIF and biceps tenodesis/tenotomy)
Patients underwent surgical intervention by one of six orthopedic attending surgeons fellowship trained in orthopedic trauma or shoulder surgery. Patient positioning and surgical approach varied based on surgeon preference. Patients were positioned either supine, semi-lateral with a beanbag, or in beach-chair. Deltopectoral or anterolateral approaches were both used based on surgeon-preference. The LHBT was evaluated intraoperatively, at which point the decision to proceed with tenodesis was at the discretion of the operating surgeon. Soft tissue tenodesis of the LHBT was performed to the pectoralis major at the level of its insertion or to the subscapularis tendon using nonabsorbable suture. An intraoperative depiction of open tenodesis is demonstrated in Figure 1.
Figure 1.
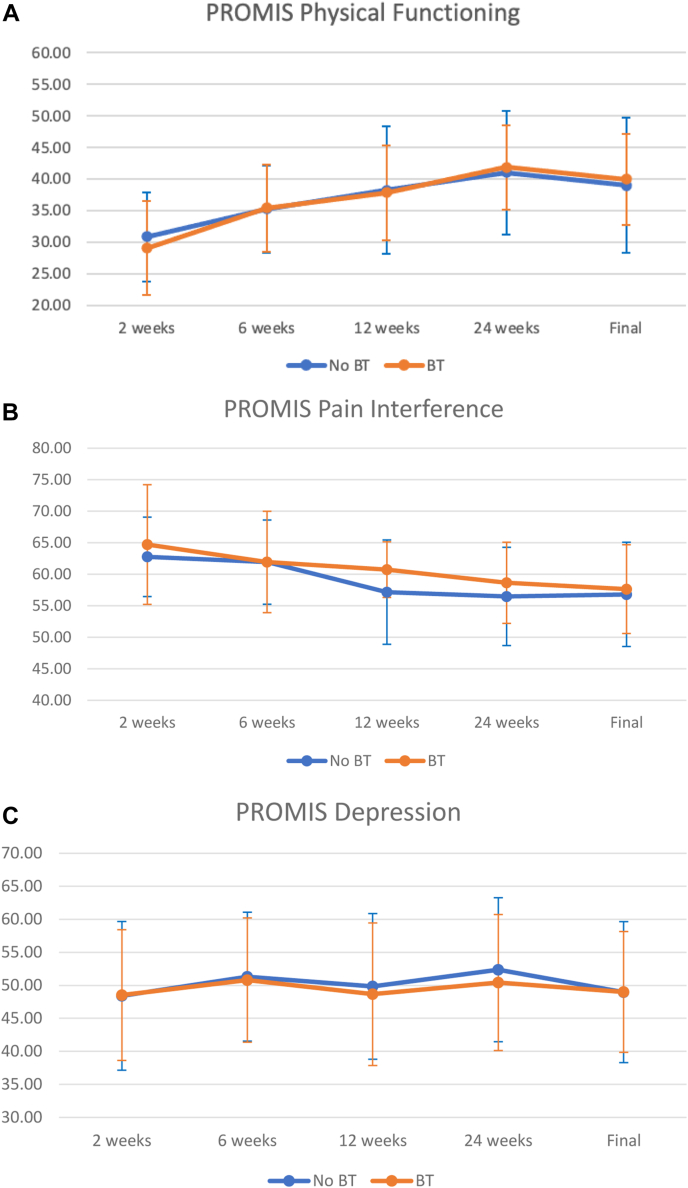
PROMIS scores: (A) Physical Function, (B) Pain Interference, (C) Depression. BT, biceps tenodesis; PROMIS, patient-reported outcome measurement information system.
Intramedullary fibular strut grafts were used in cases of significant metaphyseal comminution and/or medial calcar disruption and in all cases locking anatomic proximal humerus plates were used (Synthes, Warsaw, IN, USA). If rotator cuff tendons were tagged at the beginning of the case for additional exposure, tagged sutures were then passed through the plate and secured for additional stability. Reduction and final plate position were confirmed using multiplanar fluoroscopy was used routinely.
Postoperatively, patients were placed into a sling for two weeks with immediate initiation of gentle stretching and ROM of the ipsilateral elbow, wrist, and hand. At two weeks postoperatively, passive and active-assisted ROM in the scapular plane was initiated. Patients continued use of the sling when not working with physical therapy and weightbearing was restricted to one pound. At six weeks postoperatively, sling use was discontinued and weightbearing was advanced to five pounds. Active ROM was also initiated at this time with the goal of achieving full ROM by 12 weeks. Strengthening was initiated at 8 weeks and advanced according to each patient’s endurance and comfort.
Outcomes
Primary outcomes included patient-reported outcomes measurement information system (PROMIS) scores for physical function (PF), depression (DP) and pain interference. These scores were standardized to the national average with a t-score mean of 50 and standard deviation of 10. Secondary outcomes including pain scores and ROM was also collected at the same time intervals as PROMIS scores. The visual analog scale was utilized to measure pain. In addition, ROM based on the documented physical examination of the attending surgeon was also recorded at each follow-up visit. All outcomes were evaluated at the following postoperative time points: two weeks (time point 1), four weeks (time point 2), twelve weeks (time point 3), six months (time point 4), and the last recorded time point within each patient’s chart (time point final) throughout the study.
Operative data including operative time and procedures performed were collected from chart review of the operative record. Total operative time for the procedure was defined as the initial incision to beginning of closure recorded by the operative staff within the surgical encounter. Follow-up information on patients including revision rates, complications, and steroid injections in the affected shoulder, was also collected.
Statistics
Demographic variables were compared across groups using chi-squared tests for categorical variables and t-tests for continuous variables. Paired t-tests were performed to compare changes from timepoint 1 to time points 2, 3, 4, and final within each group. Both complete case and sensitivity analyses carrying forward the initial outcome measure were performed to assess the reliability of the results. All statistical analyses were performed using R software (R Core Team (2022) R: A language and environment for statistical computing; R Foundation for Statistical Computing, Vienna, Austria).
Results
Our final cohort included 71 patients – 41 in the ORIF group (with biceps retained) and 30 in the ORIF with BT group. Though performing BT was surgeon-dependent, reasons for proceeding with BT included facilitating fracture exposure, subluxation or degeneration of the tendon, presence of a fracture line in the bicipital groove, or for the elimination of a potential generator of postoperative pain. One patient underwent tenotomy. The remaining 29 underwent soft tissue tenodesis. Follow-up in the ORIF group was a mean 10.49 months (range 3-30 months) vs. 11.33 months in ORIF with BT group (range 3-27 months).
There were no statistically significant differences in demographics between ORIF and ORIF with BT (Table I). Patients in the ORIF with BT group had more complex fracture morphology evidenced by higher number of fracture parts according to the Neer classification. For AO fracture classification, the majority of the ORIF with BT patients were classified as 11B1 (46.7%), while most of the ORIF group were classified as either 11A3 (39%) or 11B1 (29.3%). Of the patient’s undergoing BT, 17/29 (58.6%) patients underwent soft tissue tenodesis to the subscapularis tendon, while 12/29 (41.4%) patients underwent tenodesis to the pectoralis major tendon. One patient underwent biceps tenotomy.
Table I.
Demographics tables and figures.
| ORIF |
ORIF with BT |
P value | |
|---|---|---|---|
| Mean (min-max/%) | Mean (min-max/%) | ||
| Demographics | |||
| N | 41 | 30 | |
| Age | 57 (18-84) | 63 (17-92) | .23 |
| BMI | 26.3 (16.4-53.8) | 26.0 (19.4-35.2) | .82 |
| Female | 24 (58.5) | 20 | .49 |
| Race | .45 | ||
| White | 31 (75.6) | 27 (90.0) | |
| Hispanic | 3 (7.3) | 1 (3.3) | |
| Asian | 2 (4.8) | 2 (6.7) | |
| Black | 3 (7.3) | 0 | |
| Other | 2 (4.9) | 0 | |
| Laterality | .98 | ||
| Left | 22 (53.7) | 16 (53.3) | |
| Right | 19 (46.3) | 14 (46.7) | |
| Neer fracture parts | .02∗ | ||
| 2 | 23 (56.1) | 8 (26.7) | |
| 3 | 16 (39.0) | 16 (53.3) | |
| 4 | 2 (4.9) | 6 (20.0) | |
| AO fracture classification | .02∗ | ||
| 11A1 | 3 (7.3) | 2 (6.7) | |
| 11A2 | 3 (7.3) | 2 (6.7) | |
| 11A3 | 16 (39.0) | 3 (10.0) | |
| 11B1 | 12 (29.3) | 14 (46.7) | |
| 11B2 | 5 (12.2) | 2 (6.7) | |
| 11B3 | 1 (2.4) | 0 | |
| 11C1 | 0 | 2 (6.7) | |
| 11C2 | 1 (2.4) | 5 (16.7) | |
| Fracture dislocation | 4 (9.8) | 3 (10.0) | 1.00 |
| Head split | 0 | 0 | |
| Length of surgery, minutes | 120.3 (35-231) | 128.8 (53-343) | .56 |
BT, biceps tenodesis; ORIF, open reduction internal fixation.
Statistically significant difference (P < .05).
At the final time point, only forward flexion was found to be significantly greater in the ORIF with BT group than the ORIF group (142.3 vs. 123.1, P < .02). All other outcomes at the final time point did not show a statistically significant difference in ROM (Table II). Within group comparisons revealed that PROMIS PF scores improved significantly over time in both groups. PROMIS pain interference scores improved significantly from time point 1 to time points 3, 4 and the final follow-up for both groups. PROMIS DP scores did not improve significantly over time in either group. PROMIS scores did not statistically differ at each time point recorded between either groups (Fig. 1). Visual analog scale scores significantly improved in both groups (Table II).
Table II.
Range of motion and patient reported outcome scores.
| ORIF |
ORIF with BT |
P value | |
|---|---|---|---|
| Mean (SD) | Mean | ||
| ROM (°) | |||
| Forward flexion | 123.1 (38.1) | 142.3 (24.8) | .02∗ |
| Abduction | 110.4 (35.7) | 123.1 (39.0) | .30 |
| External rotation | 54.38 (21.5) | 42.0 (13.6) | .07 |
| PROMs | |||
| VAS | 2.6 (2.6) | 2.1 (2.2) | .41 |
| PROMIS physical Function | 38.9 (10.7) | 40.0 (7.2) | .68 |
| PROMIS pain Interference | 56.8 (8.3) | 57.6 (7.0) | .69 |
| PROMIS upper Extremity | 39.3 (11.0) | 36.8 (4.3) | .73 |
| PROMIS depression | 49.0 (10.7) | 49.0 (9.2) | .99 |
ROM, range of motion; PROM, patient reported outcome measures; VAS, visual analog scale; PROMIS, patient-reported outcomes measurement information system.
Statistically significant difference (P < .05).
There were a total of 7 revision operations, 3 (7.3%) in the ORIF group and 4 (13.3%) in the ORIF with BT group (Table III). Additionally, no statistically significant differences in complications or length of surgery were seen between the two groups. While the ORIF group had more postoperative injections performed in the operative shoulder than the ORIF with BT group (7 vs. 2, respectively), the difference was not statistically significant (Table III).
Table III.
Revisions and complications.
| ORIF |
ORIF with BT |
P value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Complications | |||
| Required revision | 3 (7.3) | 4 (13.3) | .446 |
| Postsurgical complications | 7 (17.1) | 6 (20.0) | .753 |
| Postoperative injections | 7 (17.1) | 2 (6.7) | .285 |
ORIF, open reduction internal fixation; BT, biceps tenodesis.
Discussion
In our retrospective analysis of operatively treated PHFs, we found no significant differences in reoperations, postoperative injections, or PROMIS scores between those treated ORIF with BT, vs. ORIF alone. Pain and functional scores were similar between the two groups at all time points; however, there was significantly higher forward flexion in the ORIF with BT group at final follow-up. Additionally, there was no significant difference in operative time between groups.
There are limited amount of literature investigating the impact of BT during ORIF in PHF. Greve et al found that in a cohort of 56 patients, patients undergoing ORIF with BT had statistically greater flexion, external rotation, and the capacity to throw a softball better than the ORIF group.4 Our results show similar improvements in motion with better forward flexion in the ORIF with BT group at final follow-up. However, significant differences in external rotation were not seen. Differences in these results can potentially be attributed to differences in methodology including patient reported outcome measures and sample size. A prior report by Soliman et al demonstrated similar ROM in patients undergoing BT concurrently with shoulder hemiarthroplasty for PHFs, further providing evidence that tenodesis may not play a significant role in enhancing postoperative ROM.11 This notion is further supported by our PROMIS score data, as we found no difference in physical functioning, pain, and DP scores compared between groups.
In our study, there were no significant differences in operative time between ORIF with or without BT. Typically the biceps should be assessed for involvement in the fracture as this could be a potential source of postoperative pain or restrictions in ROM. In cases where BT was performed, this did not result in a significantly different operative time than ORIF alone. Due to the high variability in operating room time (ranging from 35-343 minutes) in our study, this could account for additional time performing the biceps procedure. The consideration for additional operative time to perform BT should be weighed with the risks of performing this procedure which may include loss of fixation, infection, hematoma, neurologic injuries, vascular injuries, and reflex sympathetic dystrophy which have been reported after BT procedures.7,8,14 In addition, patients may report biceps cramping and pain at the tenodesis site following tenodesis, but this is rare.13 Of note, we did not find a difference in revision or complication rates between patients undergoing ORIF with or without concurrent BT. Thus, without more clarity on the superiority of one approach vs. the other, the decision to proceed with BT may best be made by consideration of fracture morphology, intraoperative evaluation of the LHBT and reported risks of tenodesis.
Improvements in pain and PF in both groups were seen over time; however, the differences were not significantly different between groups. There was no statistical improvement seen in PROMIS DP score in either group. This may also reflect the multifactorial nature of DP and the variability in expected improvements in mental health scores. In addition, changes in physical functioning may not correlate to improvements in overall mental health. This is evidenced by the work of Beleckas et al, who found that early improvement in PROMIS PF scores is not associated with change in PROMIS DP scores.1
The strengths of this study are its larger patient cohort compared to prior reports and novel use of PROMIS scores in patient outcome data following treatment of PHFs. Our investigation has several limitations. Firstly, retrospective study design subjects our data to bias – methods of fracture fixation and tenodesis among different surgeons can potentially confound our results due to differences in technique and indications for operative treatment. In addition, our groups differed in severity of injury (as evidenced by AO classification and Neer classification). Subgroup sample sizes were not sufficient to perform statistical matching by fracture classification; however, this may be important in understanding severity of injury and the role of BT. In addition, PROMIS upper extremity data was not available and may further inform the patient-reported outcomes within our study cohort. Future prospective studies are warranted evaluating BT during ORIF procedures for displaced PHFs, and may investigate fracture severity in further delineating the role of this potentially useful adjunctive procedure.
Conclusion
BT performed during ORIF of PHFs did not result in significantly different functional or patient-reported outcomes between groups, except for greater forward flexion at final follow-up. Although BT was done more commonly in severe PHFs, patients in both groups had similar rates of subsequent biceps-related procedures and revision surgery.
Disclaimers:
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
This study was approved by the Office of Research Compliance and Quality Improvement, 6500 Wilshire Blvd., Suite 1800, Los Angeles, CA 90048, USA: STUDY00002202.
Institutional review board approval was received from Cedars-Sinai Office of Research Compliance and Quality Improvement, 6500 Wilshire Blvd., Suite 1800, Los Angeles, CA 90048 (IRB protocol ID STUDY00002202).
References
- 1.Beleckas C.M., Guattery J., Chamberlain A.M., Khan T., Kelly M.P., Calfee R.P. Using patient-reported outcomes measurement information system measures to understand the relationship between improvement in physical function and depressive symptoms. J Am Acad Orthop Surg. 2018;26:e511–e518. doi: 10.5435/JAAOS-D-17-00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Branca Vergano L., Corsini G., Monesi M. Long head of biceps in proximal fractures of the humerus: an underestimated problem? Acta Biomed. 2020;91:69–78. doi: 10.23750/abm.v91i4-S.9634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buecking B., Mohr J., Bockmann B., Zettl R., Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res. 2014;472:1576–1585. doi: 10.1007/s11999-013-3415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greve F., Beirer M., Zyskowski M., Cronlein M., Muller M., Pesch S., et al. Prospective outcome analysis following tenodesis of the long head of the biceps tendon along with locking plate osteosynthesis for proximal humerus fractures. Injury. 2019;50:681–685. doi: 10.1016/j.injury.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Hasan A.P., Phadnis J., Jaarsma R.L., Bain G.I. Fracture line morphology of complex proximal humeral fractures. J Shoulder Elbow Surg. 2017;26:e300–e308. doi: 10.1016/j.jse.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Neer C.S., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 7.Nho S.J., Reiff S.N., Verma N.N., Slabaugh M.A., Mazzocca A.D., Romeo A.A. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–768. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Nho S.J., Strauss E.J., Lenart B.A., Provencher M.T., Mazzocca A.D., Verma N.N., et al. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18:645–656. doi: 10.5435/00124635-201011000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Ramos Poroes F., Desmarchelier R., Bauer S. Atypical biceps-related complication of proximal humerus fracture leading to internal shoulder impingement due to tendon stump dislocation. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2019-232124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solberg B.D., Moon C.N., Franco D.P., Paiement G.D. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23:113–119. doi: 10.1097/BOT.0b013e31819344bf. [DOI] [PubMed] [Google Scholar]
- 11.Soliman O.A., Koptan W.M. Proximal humeral fractures treated with hemiarthroplasty: does tenodesis of the long head of the biceps improve results? Injury. 2013;44:461–464. doi: 10.1016/j.injury.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 12.Tosounidis T., Hadjileontis C., Georgiadis M., Kafanas A., Kontakis G. The tendon of the long head of the biceps in complex proximal humerus fractures: a histological perspective. Injury. 2010;41:273–278. doi: 10.1016/j.injury.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Virk M.S., Nicholson G.P. Complications of proximal biceps tenotomy and tenodesis. Clin Sports Med. 2016;35:181–188. doi: 10.1016/j.csm.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Werner B.C., Brockmeier S.F., Gwathmey F.W. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43:570–578. doi: 10.1177/0363546514560155. [DOI] [PubMed] [Google Scholar]