Abstract
Background/purpose
The etiology of the ectopic eruption (EE) of the maxillary first permanent molars (FPM) remains unclear and controversial. This study was designed to explore the dental and skeletal factors for EE of the FPM in children.
Materials and methods
Children aged 6–10 years were recruited to this study. Subjects were assigned to the ectopic eruption group (EEG) and the normal eruption group (NEG). Lateral cephalometric radiographs and panoramic radiographs were measured by angular and linear indices.
Results
The prevalence of EE of maxillary FPM was higher in males and at younger ages. Subjects with skeletal class III malocclusion were more likely to be diagnosed with EE of maxillary FPM. The SNA, ANB, FMIA, Wits, Ptm-A, ANS-PNS, overbite, and overjet were significantly different between the EEG and the NEG. The length of the posterior region of the maxillary alveolar bone, U6-OP, and eruptive angulation of the maxillary FPM were statistically different between the two groups.
Conclusion
Male sex, skeletal class III malocclusion, mesial inclination of the maxillary FPM, hypoplasia of the maxilla, and insufficient length of the posterior region of the maxillary alveolar bone were related to EE of the maxillary FPM.
Keywords: Ectopic eruption, Maxillary first permanent molars, Posterior maxillary alveolar bone, Skeletal class III malocclusion
Introduction
Ectopic eruption (EE) of the first permanent molars (FPM) occurs due to the molar’s abnormal mesioangular eruption path, resulting in an impaction at the distal prominence of the primary second molar’s crown.1 EE of the FPM is more common in the maxilla and the prevalence of EE of the maxillary FPM ranges between 0.75 % and 8.7 % in different locations according to previous studies.1, 2, 3, 4, 5, 6, 7, 8
EE of the maxillary FPM may lead to pathological absorption at the distal roots of maxillary second primary molars, the early exfoliation of maxillary second primary molars, and even space loss of lateral dentition.9,10 In addition, EE of the maxillary FPM usually occurs at an early age, increasing the possibility of other dental and maxillofacial problems, such as maxillary hypoplasia and severe sagittal and transverse crowding.3 These problems might increase the difficulty of subsequent orthodontic treatments, leading to poor occlusal relationships and reduced masticatory efficiency.11 Additionally, due to the mesial inclination of the maxillary FPM, food residue can easily fill the triangular spaces created by the distal surfaces of the maxillary second primary molars and the proximal surfaces of the maxillary FPM, enhancing the risk of caries.12 Therefore, EE of maxillary FPM warrants attention by dentists, and early detection, diagnosis, and intervention are needed to prevent severe consequences.
The etiology of EE of the maxillary FPM is not yet clear. According to previous studies, it may be associated with genetic and local factors, including heredity, sex, oversized maxillary second primary molars, a smaller maxilla, posterior position of the maxilla, an abnormal eruptive angulation of the maxillary FPM, and delayed calcification of teeth.6,7,13, 14, 15, 16, 17, 18 Bjerklin found that the prevalence increased in siblings.17 Some studies have reported no significant sex difference,4,15,18 while some other studies showed a higher prevalence in males.3,8,19 Mucedero et al. found that the mesiodistal crown widths of the maxillary second primary molars and maxillary FPMs were greater in patients with EE of the maxillary FPM.3 Becktor et al. suggested that irreversible EE of the maxillary FPM with severe maxillary second primary molar resorption was related to abnormal canine eruption and subsequent lateral or central incisor root resorption.11 A deficiency of bony growth or change in the timeline of bone growth at the tuberosity region was found linking to EE of the maxillary FPM5,20 In Salbach’s study, a significant relation was found between the EE of the maxillary FPM and class III malocclusion.4 However, the number of patients included in most of the previous studies was usually small, making the findings less representative. Therefore, recruiting larger numbers of patients is necessary to determine the risk factors for the EE of the maxillary FPM.
The maxillary tuberosity is the posterior inferior extension of the maxilla, bounded mesially by the last erupted molars and maxillary sinus and distally by the pterygopalatine fissure and pyramidal process of the palatine bone.21 In previous studies, the posterior contour of the maxillary tuberosity in subjects with forward growth of the maxillary complex was reported to have greater periosteal apposition.22,23 It was inferred from Hwang’s study that proper eruption of the maxillary second permanent molars was facilitated by forward growth of the maxilla and sufficient bone apposition at the maxillary tuberosity region.24 However, the correlation between the maxillary tuberosity region and EE of the maxillary FPM has not been systematically assessed.
Our study was conducted to identify the risk factors for EE of the maxillary FPM through epidemiological and radiographic analyses.
Materials and methods
The subjects were recruited from patients who visited the West China Hospital of Stomatology from 2014 to 2018 and the flow chart is showed as followed (Fig. 1). The West China Hospital of Stomatology, University’s Institutional Review Board gave its approval for this study. All subjects gave their informed consent in writing, and the Declaration of Helsinki was rigorously followed in this study.
Fig. 1.
Flow chart of inclusion and exclusion of subjects.
The inclusion criteria were as follows: 1) 6–10 years old, with the maxillary FPM erupting or erupted; 2) panoramic radiographs and lateral cephalometric radiographs available; and 3) at least one maxillary second primary molar in the maxillary dentition.
The exclusion criteria were as follows: 1) loss of bilateral maxillary second primary molars; 2) presence of systemic diseases that can cause EE of the maxillary FPMs, such as cranioclavicular dysplasia syndrome and mutation of parathyroid hormone receptor 1; 3) EE of mandibular FPM; 4) maxillary second primary molars with cavities on their distal proximal surfaces; 5) supernumerary teeth or congenital absence of the maxillary second primary molars or the maxillary FPM; 6) alveolar bone injury or tooth loss caused by trauma; 7) impacted maxillary FPM caused by other reasons, such as odontoma or cyst; 8) without available panoramic radiographs or lateral cephalometric radiographs; or 9) panoramic radiographs and/or lateral cephalometric radiographs excessively distorted or otherwise insufficiently clear for the measurements.
The subjects with EE of the maxillary FPM were assigned as the ectopic eruption group (EEG). The subjects with normal eruption of bilateral maxillary FPM were randomly recruited by systematic sampling as the normal eruption group (NEG).
The same x-ray machine (Veraviewepocs, Morita, Tokyo, Japan) was used to take all of the panoramic and lateral cephalometric radiographs. Children were guided by radiologists maintaining the standard head position. Lateral cephalometric radiographs were evaluated with 6 angular and 10 linear indices (Fig. 2) with Dolphin Imaging Software (version 11.8; California, USA).
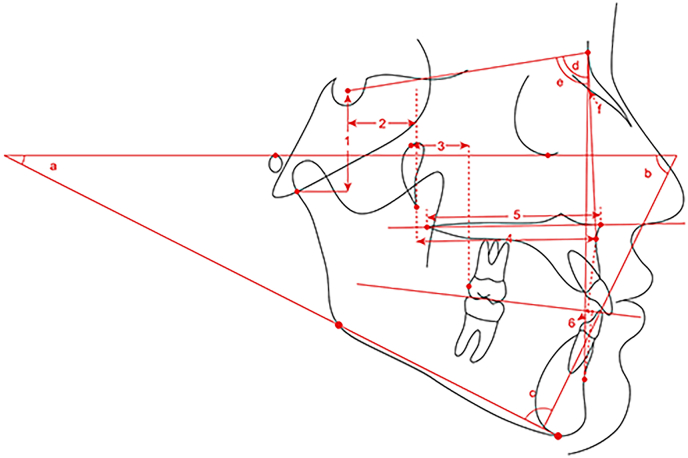
Fig. 2.
Methods of measuring in a lateral cephalometric radiograph: 1. S–Ar, the vertical distance between the point sella (S) and the point articulare (Ar); 2. Ptm-S, the distance between the perpendicular projections from the point pterygomaxillary fissure (Ptm) and point S onto the Frankfort horizontal (FH) plane; 3. U6-PTV, the distance between the perpendicular projections from point Ptm and the distal point of the maxillary first molar onto the FH plane; 4. Ptm-A, the distance between the perpendicular projections from the point Ptm and the point subspinable (A) onto the FH plane; 5. ANS-PNS, the distance between the point anterior nasal spine (ANS) and the point posterior nasal spine (PNS); 6. Wits, the distance between the perpendicular projections from the point A and point supramental (B) onto the occlusal plane; a, FMA, the angle formed by the intersection of the FH plane and the mandibular plane; b, FMIA, the angle formed by the intersection of the extension line of the long axis of the lower central incisor and the FH plane; c, IMPA, the angle formed by the intersection of the extension line of the long axis of the lower central incisor and the mandibular plane; d, SNA, the angle formed by the point S, the point nasion (N) and the point A; e, SNB, the angle formed by the point S, the point N and the point B; f, ANB, the angle formed by the point A, the point N and the point B.
Based on the reported accuracy of panoramic radiographs25 and a previous similar study,16 panoramic radiographs were used to measure the length of the posterior region of maxillary alveolar bone, the crown width of the maxillary second primary molars, the perpendicular distance from the lowest point of the distal cusp of the maxillary FPM to the occlusal plane (U6-OP) and the eruptive angulation (EA) of the maxillary FPM in a picture-archiving and communication system (Marosis Enterprise PACS; INFINITT Healthcare System, Seoul, Korea) (Fig. 3). We defined the length of the posterior region of maxillary alveolar bone as a representation of the length of the maxillary tuberosity. The occlusal plane (OP) was defined as the average plane of the occlusal contacts of posterior teeth, modified from the OP described in the study by Chen et al.16 The crown width of the maxillary second primary molars was measured as the distance between the perpendicular lines from the protruding points on the mesial surface and the distal surface to the OP. Since the ectopically erupted maxillary FPM were mesially bounded by the maxillary second primary molars, we drew vertical lines from the distal point of a maxillary second primary molar and from the distal point of the pterygopalatine fissure to the OP, the distance between the two lines represented the length of the posterior region of maxillary alveolar bone. The U6-OP and the EA formed by the long axis of the maxillary FPM and the OP were used to represent the eruption position of the maxillary FPM. In subjects with unilateral EE of the maxillary FPM, the values of the length of the posterior region of maxillary alveolar bone, U6-OP, and EA were all taken from the side of EE. For subjects with bilateral EE of the maxillary FPM and with normally erupted maxillary FPM, we averaged the measurements from each side.
Fig. 3.
Methods of measuring in a panoramic radiograph. OP: occlusal plane, the average plane of the occlusal contacts of posterior teeth (yellow line) 1. U6-OP: the perpendicular distance from the lowest point of the distal cusp of the maxillary first permanent molar to OP (black line); 2. the length of the posterior region of the maxillary alveolar bone: the perpendicular distance from the distal point of the maxillary secondary primary molar to the distal point of the pterygopalatine fissure (blue line); 3. the crown width of the second primary molar: the perpendicular distance from the mesial point to the distal point of the maxillary secondary primary molar’s crown (green line); a, EA: eruptive angulation, the distal angle formed by the long axis of the maxillary first permanent molar and OP.
All evaluations and measurements were performed by Kun Zhang and Yun Zhang, supervised by Yiran Peng and Jian Pan. The interrater reliability between the examiners was assessed, and the Kappa value was 0.82, indicating that these measurements were reliable. All statistical analyses were performed in SPSS (IBM SPSS 23, IBM Corp). The Kolmogorov-Smirnov test and Q-Q plots were used to exam continuous variables’ normality. Differences between the NEG and EEG were determined by independent-sample t-tests, chi-square tests, and Wilcoxon rank sum tests. Variables associated with EE of the maxillary FPM according to the univariate analyses were included in the binary logistic regression analysis.
Results
Characteristics of the subjects
A total of 2806 patients met the inclusion criteria, including 101 patients with EE of the maxillary FPM. The prevalence of EE of the maxillary FPM in this study was 3.6 %. Three patients whose radiographs were excessively distorted were excluded, and the remaining 66 males and 32 females with EE of the maxillary FPM were assigned to the EEG. Ninety-eight subjects with normal eruption of the maxillary FPM were randomly recruited by systematic sampling for the NEG, which was comprised of 39 males and 59 females. The chi-square test revealed a statistically significant difference in sex composition between the NEG and EEG (Table 1, P < 0.001). The average age analysis showed that subjects in the EEG were younger than those in the NEG (Table 1, P = 0.015).
Table 1.
Epidemiological characteristics of subjects.
| Variable | NEG | EEG | P value |
|---|---|---|---|
| Sex | |||
| Male | 39 | 66 | < 0.001∗∗∗ |
| Female | 59 | 32 | |
| Age | 7.93 ± 0.96 | 7.56 ± 1.14 | 0.015∗ |
EEG, ectopic eruption group; NEG, normal eruption group.
∗P < 0.05, ∗∗∗P < 0.001.
Subjects in the EEG had insufficient maxillary development according to lateral cephalometric radiograph analysis.
Based on the lateral cephalometric radiograph analysis (Table 2), there were significant group differences in the SNA angle (P = 0.001), the ANB angle (P < 0.001) and the FMIA angle (P = 0.08). There were no significant group differences in the FMA angle, the IMPA angle, or the SNB angle. Statistical difference was found between the two groups in the linear values of Wits (P < 0.001), Ptm-A (P < 0.001), ANS-PNS (P < 0.001), overjet (P < 0.001) and overbite (P = 0.002). Linear values of S–Ar, Go-Me, Ptm-S, U6-PTV, and UⅤ-PTV did not significantly differ between the two groups.
Table 2.
Factors associated with ectopic eruption (EE) of the maxillary first permanent molars (FPM) in cephalometric radiograph analysis.
| Measurement | NEG | EEG | P value |
|---|---|---|---|
| S–Ar (mm) | 30.03 ± 3.20 (30.05) | 29.65 ± 3.00 (29.70) | 0.415 |
| Go-Me (mm) | 56.19 ± 4.06 (56.10) | 55.12 ± 4.01 (55.55) | 0.098 |
| FMA (°) | 27.81 ± 5.43 (27.35) | 26.61 ± 5.96 (27.25) | 0.291 |
| FMIA (°) | 59.20 ± 7.88 (59.05) | 62.19 ± 7.58 (62.25) | 0.008∗∗ |
| IMPA (°) | 92.98 ± 7.89 (93.35) | 91.19 ± 6.60 (91.70) | 0.140 |
| SNA (°) | 80.68 ± 3.56 (80.25) | 78.83 ± 3.75 (78.45) | 0.001∗∗ |
| SNB (°) | 76.38 ± 3.75 (75.85) | 76.81 ± 4.26 (76.80) | 0.417 |
| ANB (°) | 4.30 ± 3.35 (4.60) | 2.02 ± 3.30 (1.75) | <0.001∗∗∗ |
| Wits (mm) | −1.02 ± 4.68 (−1.35) | −4.16 ± 4.77 (−4.40) | <0.001∗∗∗ |
| Ptm-S (mm) | 16.96 ± 2.16 (16.95) | 17.66 ± 2.50 (17.60) | 0.068 |
| U6-PTV (mm) | 8.23 ± 2.42 (8.15) | 8.45 ± 2.78 (8.30) | 0.474 |
| UV-PTV (mm) | 17.87 ± 2.84 | 17.22 ± 3.15 | 0.105 |
| Ptm-A (mm) | 42.78 ± 3.06 (42.35) | 41.00 ± 3.18 (40.65) | <0.001∗∗∗ |
| ANS-PNS (mm) | 49.28 ± 3.71 (49.05) | 47.18 ± 3.43 (47.00) | <0.001∗∗∗ |
| Overjet (mm) | 3.62 ± 3.39 (4.55) | 0.54 ± 3.74 (−0.30) | <0.001∗∗∗ |
| Overbite (mm) | 2.41 ± 2.00 (2.00) | 1.51 ± 2.00 (1.60) | 0.002∗∗ |
S–Ar, the vertical distance between the point sella (S) and the point articulare (Ar); Go-Me, the distance between the point gonion (Go) and the point menton (Me); SNA, the angle formed by the point S, the point nasion (N) and the point subspinable (A); SNB, the angle formed by the point S, the point N and the point supramental (B); ANB, the angle formed by the point A, the point N and the point B; Wits, the distance between the perpendicular projections from the point A and point B onto the occlusal plane (OP); Ptm-S, the distance between the perpendicular projections from the point pterygomaxillary fissure (Ptm) and point S onto the Frankfort horizontal (FH) plane; U6-PTV, the distance between the perpendicular projections from the point Ptm and the distal point of the maxillary first molar onto the FH plane; UV-PTV, the distance between the perpendicular projections from the point Ptm and the distal point of the maxillary second primary molar onto the FH plane; Ptm-A, the distance between the perpendicular projections from the point Ptm and the point A onto the FH plane; ANS-PNS, the distance between the point anterior nasal spine (ANS) and the point posterior nasal spine (PNS); Overjet, the anteroposterior distance between the most labial surface of the upper incisor and the most labial surface of the lower incisor when the teeth are in maximum intercuspal position; Overbite, the vertical overlap of the upper and lower incisors when the teeth are in maximum intercuspal position.
∗∗P < 0.01; ∗∗∗P < 0.001.
Subjects in the EEG were more likely to be diagnosed with skeletal class III malocclusion
Subjects were divided into skeletal class I, II, and III malocclusions according to the value of the ANB angle. According to the chi-square test, there was a significant difference in the proportion of skeletal malocclusions between the EEG and NEG (Table 3, P < 0.001). Skeletal class III malocclusion accounted for the largest proportion of subjects in the EEG, while in the NEG, skeletal class I malocclusion accounted for the largest proportion.
Table 3.
Subjects’ classifications of skeletal malocclusions in the NEG and the EEG.
| Classification | NEG | EEG | P value |
|---|---|---|---|
| Skeletal class I (2° ≤ ANB ≤ 6°) | 46 | 36 | <0.001∗∗∗ |
| Skeletal class II (ANB > 6°) | 29 | 10 | |
| Skeletal class III (ANB < 2°) | 23 | 52 | |
| Total | 98 | 98 |
∗∗∗P < 0.001.
Subjects in the EEG had insufficient development of the posterior region of the maxillary alveolar bone according to panoramic radiograph analysis.
From the panoramic radiograph analysis (Table 4), there was a statistically significant difference in the length of the posterior region of the maxillary alveolar bone between the EEG and NEG (P < 0.001). No significant difference was observed in the crown width of maxillary second primary molars between the two groups. Considering the possible distortion of panoramic radiographs, the ratio of the length of the posterior region of the maxillary alveolar bone to the crown width of maxillary second primary molars was used to analyze more precisely. The results also showed a statistically significant difference between the two groups (P = 0.005). Besides, the values of U6-OP (P < 0.001) and EA (P = 0.002) revealed differences between the two groups that were statistically significant.
Table 4.
Factors associated with EE of the maxillary FPM in panoramic radiograph analysis.
| Measurement | NEG | EEG | P value |
|---|---|---|---|
| The length of the posterior region of maxillary alveolar bone (mm) | 25.56 ± 4.95 | 21.26 ± 4.60 | <0.001∗∗∗ |
| The crown width of the maxillary second primary molars (mm) | 10.98 ± 1.84 | 10.52 ± 2.02 | 0.097 |
| Ratio | 2.34 ± 0.40 | 2.09 ± 0.81 | 0.005∗∗ |
| U6-OP (mm) | 0.38 ± 1.40 | 1.74 ± 1.66 | <0.001∗∗∗ |
| EA (°) | 93.93 ± 7.40 | 89.77 ± 11.08 | 0.002∗∗ |
Ratio, the ratio of the length of the posterior region of maxillary alveolar bone to the crown width of the maxillary second primary molars; U6-OP, the perpendicular distance from the lowest point of the distal cusp of the maxillary first permanent molar to the OP; EA, eruptive angulation, the angle formed by the long axis of the maxillary first permanent molar and OP.
∗∗P < 0.01; ∗∗∗P < 0.001.
Binary logistic regression analysis
The binary logistic regression analysis showed that sex, the length of the posterior region of the maxillary alveolar bone, U6-OP, overbite, overjet, and the EA were significantly related to the EE of the maxillary FPM (Table 5).
Table 5.
Binary analysis of factors associated with EE of the maxillary FPM.
| Variable | Binary analysis |
|
|---|---|---|
| Odds ratio (95 % confidence interval) | P value | |
| Sex | 4.798 (1.922–11.979) | 0.001∗∗ |
| The length of the posterior maxillary alveolar bone (mm) | 0.796 (0.703–0.900) | <0.001∗∗∗ |
| U6-OP (mm) | 1.769 (1.300–2.407) | <0.001∗∗∗ |
| Overbite (mm) | 0.791 (0.633–0.987) | 0.038∗ |
| Overjet (mm) | 0.788 (0.676–0.918) | 0.002∗∗ |
| EA (°) | 0.927 (0.886–0.970) | 0.001∗∗ |
∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001.
Discussion
With parents’ awareness of oral health care increasing, EE of the maxillary FPM has received more attention in children during the early stage of mixed dentition. EE of maxillary FPM often causes damage to the roots of the maxillary second primary molars, which increases the difficulty of maintaining oral health.5 However, the specific etiology of this anomaly remains unclear. Our study aimed to determine the correlations between EE of the maxillary FPM and alveolar and maxillary characteristics, providing more evidence for clinical practice.
The prevalence of EE of the maxillary FPM in this study was 3.6 % (101/2806). Ninety-eight children with EE of the maxillary FPM and 98 children with the normal eruption of maxillary FPM were included. The proportion of males in the EEG (66/98) was much higher than that in the NEG (39/98), while some researchers’ studies showed that there was no significant difference between sex.3,8,15 The discrepancy might be due to the larger sample size and inclusion of different races in this study. The subjects in the EEG were significantly younger on average than those in the NEG, which revealed a possible effect of age on EE of the maxillary FPM, suggesting that dentists should pay more attention to the eruption of the maxillary FPM in younger children.
Our results in lateral cephalometric radiograph analysis indicated that the children diagnosed with skeletal class III malocclusion might have a higher risk of EE of the maxillary FPM. This result could be supported by Dabbagh et al.26 although some others reported no significant differences in lateral cephalometric radiograph analysis between the NEG and EEG.2,15 In our results, the SNA and ANB angles of the subjects in the EEG were statistically smaller than those in the NEG, indicating sagittal skeletal discrepancies between the maxilla and the mandible and hypoplasia in the maxilla compared to the mandible. Results of some previous studies indicated a posterior position of the maxilla relative to the cranial base,7,13 however, our study showed that the SNB angle and the Ptm-S value were not significantly different between the two groups. Besides, smaller Ptm-A and SNA in the EEG were observed in this study and this result suggested that the discrepancies between the maxilla and the mandible were mainly attributable to the posterior position of point A instead of the posterior position of the maxilla, which was consistent with the study by Yujin Rah.27 The results in our study also showed statistically smaller Ptm-A and ANS-PNS lengths in the EEG, indicating an insufficient length of the maxilla, which was similar to the results reported by Mucedero, Pulver and Yuen.3,7,28 In addition, the statistically smaller Wits, smaller IMPA angle, decreased overjet, and decreased overbite further indicated the trend of skeletal class III malocclusion in the EEG. The labial inclination of the maxillary incisors and lingual inclination of the mandibular incisors were extrapolated from the smaller IMPA angle, decreased overjet, and decreased overbite, which was the consequence of dental compensation arising from skeletal class III malocclusion. Therefore, it could be reasonably inferred that children with skeletal class III malocclusion are more susceptible to EE of the maxillary FPM and that this anomaly might mainly result from the insufficient length of the maxilla instead of the posterior position of it, probably on account of the insufficient capacity of the maxilla to accommodate the maxillary FPM in the early mixed dentition period.
Panoramic radiography is one of the routine examinations in orthodontic clinics and plays an important role in clinical and basic oral research. This method clearly shows the upper and lower dentition and tooth germs, and it can evaluate the structure of the maxilla. When compared to other teeth, the molars’ angular distortion on panoramic radiographs was least impacted by the head’s position, according to a study by Samawi et al.29 Another study by Stramotas et al. revealed that panoramic radiography was accurate for linear and angular measurements provided that the occlusal plane was kept at a similar angulation25 Therefore, it is reliable to make measurements in the molar segmentation on panoramic radiographs. Meanwhile, panoramic radiography had a relatively lower radiation dosage (11.3 μSv) compared to the cone-beam computed tomography (CBCT) (17.8–60 μSv),29 thus dentists prefer to choose panoramic radiography examination for children’s early examination in the primary and mixed dentition period. Given the accuracy and the lower radiation dose of panoramic radiography compared to CBCT, we chose panoramic radiographs instead of CBCT in our study.
From the panoramic radiograph analysis, we observed no statistical difference in the crown width of the maxillary second primary molars between the EEG and the NEG. Similar findings were observed in previous studies.2,17 There was a statistical difference in the EA of the maxillary FPM between the two groups, it also showed that EA in the EEG was smaller than that in the NEG. The results indicated that children with maxillary FPM erupting in a mesial direction might be more likely to suffer from EE of the maxillary FPM, which was consistent with previous studies.2,7,14,16,28 The U6-OP value was greater in the EEG, which revealed the eruption deficiency of the maxillary FPM in the vertical direction.
To determine whether there was a difference in the area of the maxillary tuberosity region between the EEG and NEG, the length of the posterior region of maxillary alveolar bone was measured on panoramic radiographs to represent the length of the maxillary tuberosity. The results showed that the length of the posterior region of maxillary alveolar bone in the EEG was significantly smaller than that in the NEG, suggesting the hypoplasia of the maxillary tuberosity, which might partially explain the insufficient length of the whole maxilla in children with EE of the maxillary FPM. In order to remove any potential impact of panoramic radiograph distortion, the length of the posterior region of maxillary alveolar bone to the crown width of the maxillary second primary molars ratio was calculated, and this ratio was also significantly smaller in the EEG than in the NEG, which further confirmed the insufficient development of the maxillary tuberosity region in children in the EEG.
Binary logistic regression analysis identified male sex, decreased overbite, decreased overjet, a decrease in the length of the posterior region of maxillary alveolar bone, decreased EA of the maxillary FPM, and an increase in the U6-OP as key factors related to EE of maxillary FPM (Table 5). Therefore, male children with a relatively smaller overbite, smaller overjet, smaller EA of the maxillary FPM, and a relatively smaller length of the posterior region of maxillary alveolar bone are more susceptible to EE of the maxillary FPM and warrant greater attention by dentists. Of course, there are limitations in our study, such as the lack of longitudinal observation on the subjects. Further prospective and long-term studies are needed to provide more accurate and comprehensive identification of the risk factors of EE.
In conclusion, EE of the maxillary FPM was more likely to occur in males, and EE of the maxillary FPM was significantly related to skeletal class III malocclusion, mesial eruption of the maxillary FPM, maxillary hypoplasia and hypoplasia of the posterior region of the maxillary alveolar bone. Dentists are advised to direct more attention to children with the above characteristics to ensure follow-up observations or provide early treatment.
Declaration of competing interest
The authors declare there is no conflict of interest relevant to this study.
Acknowledgements
This work was supported by the Chengdu Municipal Science and Technology Program [2019-YF05-00763-SN], the National College Students Innovation and Entrepreneurship Training Program [C2019106655] and the Natural Science Foundation of Sichuan Province [2022NSFSC1462]. None of the funders played a role in the design of the study, data collection, analyses, interpretation of the results or writing of the manuscript.
Contributor Information
Jian Pan, Email: jianpancn@scu.edu.cn.
Yiran Peng, Email: ortho_peng@hotmail.com.
References
- 1.American Academy of Pediatric Dentistry . The reference manual of pediatric dentistry. American Academy of Pediatric Dentistry; Chicago, Ill: 2021. Management of the developing dentition and occlusion in pediatric dentistry; pp. 408–425. [Google Scholar]
- 2.Chintakanon K., Boonpinon P. Ectopic eruption of the first permanent molars: prevalence and etiologic factors. Angle Orthod. 1998;68:153–160. doi: 10.1043/0003-3219(1998)068<0153:EEOTFP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Mucedero M., Rozzi M., Cardoni G., Ricchiuti M.R., Cozza P. Dentoskeletal features in individuals with ectopic eruption of the permanent maxillary first molar. Korean J Orthod. 2015;45:190–197. doi: 10.4041/kjod.2015.45.4.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salbach A., Schremmer B., Grabowski R., Stahl de Castrillon F. Correlation between the frequency of eruption disorders for first permanent molars and the occurrence of malocclusions in early mixed dentition. J Orofac Orthop. 2012;73:298–306. doi: 10.1007/s00056-012-0083-2. [DOI] [PubMed] [Google Scholar]
- 5.Barberia-Leache E., Suarez-Clúa M.C., Saavedra-Ontiveros D. Ectopic eruption of the maxillary first permanent molar: characteristics and occurrence in growing children. Angle Orthod. 2005;75:610–615. doi: 10.1043/0003-3219(2005)75[610:EEOTMF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Bjerklin K., Kurol J. Prevalence of ectopic eruption of the maxillary first permanent molar. Swed Dent J. 1981;5:29–34. [PubMed] [Google Scholar]
- 7.Pulver F. The etiology and prevalence of ectopic eruption of the maxillary first permanent molar. ASDC (Am Soc Dent Child) J Dent Child. 1968;35:138–146. [PubMed] [Google Scholar]
- 8.Caliskan S., Tuloglu N., Ozdemir C., Kizilaslan S., Bayrak S. Ectopic eruption of maxillary permanent first molars: predictive factors for self-corrected and impacted outcome. Int J Clin Pract. 2021;75 doi: 10.1111/ijcp.13880. [DOI] [PubMed] [Google Scholar]
- 9.Yaseen S.M., Naik S., Uloopi K.S. Ectopic eruption - a review and case report. Contemp Clin Dent. 2011;2:3–7. doi: 10.4103/0976-237X.79289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hennessy J., Al-Awadhi E.A., Dwyer L.O., Leith R. Treatment of ectopic first permanent molar teeth. Dent Update. 2012;39(656–8):60–61. doi: 10.12968/denu.2012.39.9.656. [DOI] [PubMed] [Google Scholar]
- 11.Becktor K.B., Steiniche K., Kjaer I. Association between ectopic eruption of maxillary canines and first molars. Eur J Orthod. 2005;27:186–189. doi: 10.1093/ejo/cjh075. [DOI] [PubMed] [Google Scholar]
- 12.Pomarico L., Primo L.G., Noce D. Ectopic eruption of the maxillary central permanent incisors and mandibular first permanent molars: report of an unusual case. Quintessence Int. 2006;37:677–683. [PubMed] [Google Scholar]
- 13.Canut J.A., Raga C. Morphological analysis of cases with ectopic eruption of the maxillary first permanent molar. Eur J Orthod. 1983;5:249–253. doi: 10.1093/ejo/5.3.249. [DOI] [PubMed] [Google Scholar]
- 14.Bjerklin K., Kurol J. Ectopic eruption of the maxillary first permanent molar: etiologic factors. Am J Orthod. 1983;84:147–155. doi: 10.1016/0002-9416(83)90179-3. [DOI] [PubMed] [Google Scholar]
- 15.Helm A., Martín-Vacas A., Molinero-Mourelle P., Caleya A.M., Gallardo N.E., Mourelle-Martínez M.R. Ectopic eruption of maxillary first permanent molars: preliminary results of prevalence and dentoskeletal characteristics in Spanish paediatric population. Children. 2021;8:479. doi: 10.3390/children8060479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen X., Huo Y., Peng Y., Zhang Q., Zou J. Ectopic eruption of the first permanent molar: predictive factors for irreversible outcome. Am J Orthod. 2021;159:e169–e177. doi: 10.1016/j.ajodo.2020.09.020. [DOI] [PubMed] [Google Scholar]
- 17.Bjerklin K. Ectopic eruption of the maxillary first permanent molar. An epidemiological, familial, aetiological and longitudinal clinical study. Swed Dent J Suppl. 1994;100:1–66. [PubMed] [Google Scholar]
- 18.Mooney G.C., Morgan A.G., Rodd H.D., North S. Ectopic eruption of first permanent molars: presenting features and associations. Eur Arch Paediatr Dent. 2007;8:153–157. doi: 10.1007/BF03262586. [DOI] [PubMed] [Google Scholar]
- 19.Güven Y. Prevalence of ectopic eruption of first permanent molars in a Turkish population. Eur Oral Res. 2018;52:1–5. doi: 10.26650/eor.2018.45227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheyne V.D., Wessels K.E. Impaction of permanent first molar with resorption and space loss in region of deciduous second molar. J Am Dent Assoc. 1947;35:774–787. doi: 10.14219/jada.archive.1947.0391. [DOI] [PubMed] [Google Scholar]
- 21.Apinhasmit W., Chompoopong S., Methathrathip D., Sangvichien S., Karuwanarint S. Clinical anatomy of the posterior maxilla pertaining to Le Fort I osteotomy in Thais. Clin Anat. 2005;18:323–329. doi: 10.1002/ca.20131. [DOI] [PubMed] [Google Scholar]
- 22.Björk A., Skieller V. Growth of the maxilla in three dimensions as revealed radiographically by the implant method. Br J Orthod. 1977;4:53–64. doi: 10.1179/bjo.4.2.53. [DOI] [PubMed] [Google Scholar]
- 23.Björk A. Sutural growth of the upper face studied by the implant method. Acta Odontol Scand. 1966;24:109–127. doi: 10.3109/00016356609026122. [DOI] [PubMed] [Google Scholar]
- 24.Hwang S., Choi Y.J., Lee J.Y., Chung C., Kim K.H. Ectopic eruption of the maxillary second molar: predictive factors. Angle Orthod. 2017;87:583–589. doi: 10.2319/020917-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stramotas S., Geenty J.P., Petocz P., Darendeliler M.A. Accuracy of linear and angular measurements on panoramic radiographs taken at various positions in vitro. Eur J Orthod. 2002;24:43–52. doi: 10.1093/ejo/24.1.43. [DOI] [PubMed] [Google Scholar]
- 26.Dabbagh B., Sigal M.J., Tompson B.D., Titley K., Andrews P. Ectopic eruption of the permanent maxillary first molar: predictive factors for irreversible outcome. Pediatr Dent. 2017;39:215–218. [PubMed] [Google Scholar]
- 27.Rah Y., Lee J., Ra J. Association between ectopic eruption of the maxillary first permanent molar and skeletal malocclusion. J Korean Acad Pediatr Dent. 2017;44:147–153. [Google Scholar]
- 28.Yuen S., Chan J., Tay F. Ectopic eruption of the maxillary permanent first molar: the effect of increased mesial angulation on arch length. J Am Dent Assoc. 1985;111:447–451. doi: 10.14219/jada.archive.1985.0135. [DOI] [PubMed] [Google Scholar]
- 29.Samawi S.S., Burke P.H. Angular distortion in the orthopantomogram. Br J Orthod. 1984;11:100–107. doi: 10.1179/bjo.11.2.100. [DOI] [PubMed] [Google Scholar]