Highlights
-
•
Medical cannabis use increased from 4 % to 11 % between 2014 and 2019.
-
•
Recreational cannabis use increased from 9 % to 15 % between 2014 and 2019.
-
•
Younger age was associated with an increased likelihood of medical cannabis use without medical authorization.
-
•
Fair or poor self-perceived health was associated with a decreased likelihood of medical cannabis use without medical authorization.
-
•
Recreational cannabis legalization was associated with an increased likelihood of medical and recreational cannabis use.
Keywords: Canada, Cannabis, Marijuana use, Marijuana smoking, Medical use, Policy
Abstract
Objectives
We characterized trends in medical cannabis use; examined characteristics associated with medical cannabis use without medical authorization; and examined the association between recreational cannabis legalization and medical cannabis use in Ontario, Canada.
Methods
Data were from a repeated, population-based, cross-sectional survey of adults (N = 19,543; 2014–2019). Cannabis use was categorized as either medical cannabis use, recreational cannabis use or no cannabis use. The analytical strategy included jointpoint regression, logistic regression and multinomial logistic regression.
Results
Medical cannabis use increased from 4 % to 11 % (Annual Percentage Change [APC]: 25 %, 95 % Confidence Interval [CI]: 17 %–33 %) and recreational cannabis use increased from 9 % to 15 % (APC: 9 %, 95 % CI: 3 %-15 %) between 2014 and 2019. Being 18 to 29 years old compared with being 65+ years old was associated with an increased likelihood of medical cannabis use without medical authorization (Odds Ratio [OR]: 4.05, 95 % CI: 2.12–7.72), while being of fair or poor self-perceived health compared with excellent, very good or good self-perceived health (OR: 0.61, 95 % CI: 0.40–0.95) was associated with a decreased likelihood of medical cannabis use without medical authorization. Recreational cannabis legalization was associated with an increased likelihood of medical cannabis use compared with no cannabis use (OR: 1.48, 95 % CI: 1.19–1.85) and of recreational cannabis use compared with no cannabis use (OR: 1.35, 95 % CI: 1.11–1.65).
Conclusions
Although medical cannabis use increased, it was largely used without medical authorization. Guidance and education that encourages medical usage under clinical supervision is recommended, and mitigation of known barriers to medical cannabis authorization.
1. Background
Medical cannabis use is authorized by clinicians in Canada to relieve symptoms associated with various disorders that have not responded to conventional medical treatments (Health Canada, 2016). It can be accessed through home cultivation or mail-order shipment from Licensed Producers, which are approved and regulated by Health Canada. Federal regulations have evolved in three distinct stages in Canada, ultimately resulting in the broadening of accessibility and availability of products: The Marihuana Medical Access Regulations (2001), Marihuana for Medical Purposes Regulations (2014) and Access to Cannabis for Medical Purposes Regulations (2016) (Shim et al., 2023).
Little is known about the extent of medical cannabis use in Canada. Health Canada’s administrative records pertaining to number of patients with medical authorization indicate significant overall growth in medical cannabis use between 2003 and 2021 (Shim et al., 2023). These findings represent underestimates because the vast majority of those engaging in medical cannabis use do not possess medical authorization (66 % to 85 %) (Government of Canada, 2019, Hamilton et al., 2017). Population-based surveys represent one avenue to address this limitation. Prevalence of medical cannabis use in lifetime was estimated to be 25 % among those 16 to 65 years old in Canada in 2018 (Leung et al., 2022). In contrast, prevalence of medical cannabis use in the past 12 months was estimated to be 4 % among those ≥18 years old in Ontario in 2013/2014 (Hamilton et al., 2017), and increased from 12 % to 14 % among those ≥16 years old in Canada between 2017 and 2019 (Government of Canada, 2019). Likewise, prevalence of medical cannabis use in the past 12 months among those who used cannabis increased from 24 % to 36 % among those ≥15 years old in Canada between 2015 and 2019 (Health Canada, 2017, Health Canada., 2023). These findings are subject to some limitations, including examination of lifetime medical cannabis use as opposed to recent or current medical cannabis use (Leung et al., 2022), as well as potential participation bias since those who used cannabis versus those who did not use cannabis may have been more likely to participate due to the cannabis-specific content of the surveys (Government of Canada, 2019). In addition, most of these studies have not examined longer term trends in medical cannabis use, which is important as other patterns of cannabis consumption have been rising over the past decade (Nigatu et al., 2020).
Few studies have examined characteristics associated with medical cannabis use without medical authorization (i.e. medical cannabis use without the approval of a clinician). In a population-based survey of those engaging in medical cannabis use post-recreational cannabis legalization in Canada, younger age, female gender, lower educational attainment, lower household income and smaller size of city were associated with an increased likelihood of medical cannabis use without medical authorization (Balneaves et al., 2023). Other surveys demonstrated that those engaging in medical cannabis use without versus with medical authorization were more likely to indicate depression or anxiety as the primary conditions for which treatment was sought, and less likely to indicate home cultivation or licensed producers as avenues of access (Walsh et al., 2013). Similar findings have been noted in Israel and Australia (Sznitman, 2017, Lintzeris et al., 2022). Additional domains (e.g. physical health, mental health and substance use patterns) have not been considered, hindering a broader profile of those engaging in medical cannabis use without medical authorization. This information is required to obtain a better understanding of this pattern of cannabis consumption and to develop and implement targeted interventions.
The association between recreational cannabis legalization and medical cannabis use warrants further attention. Indeed, recreational cannabis legalization was associated with increases in patterns of cannabis consumption and cannabis related harms in Ontario and Canada (Government of Canada, 2019, Rotermann 2020, Imtiaz et al., 2023b, Imtiaz et al., 2023a, Myran et al., 2022, Myran et al., 2023b). As such, there may have been spillover effects on medical cannabis use as well. Among adults that engaged in medical cannabis use pre-recreational cannabis legalization in Ontario, changes were observed in the trajectories of medical cannabis use and dual medical and recreational cannabis use post-recreational cannabis legalization (AminiLari et al., 2022). Notably, 24 % of those who engaged in exclusive medical cannabis use transitioned to dual medical and recreational cannabis use, and 24 % of those who engaged in dual medical and recreational cannabis use transitioned to exclusive recreational cannabis use (AminiLari et al., 2022). Health Canada’s administrative records further demonstrate that recreational cannabis legalization was associated with reductions in mail-order shipments of medical cannabis pre-post recreational cannabis legalization in Canada (Nguyen et al., 2023). Specifically, mail-order shipments were 48 % lower in the first annual quarter of 2020 compared with a counterfactual scenario with absence of recreational cannabis legalization (Nguyen et al., 2023). The reliance on administrative records that captured mail-order shipments once again depicts an incomplete image (Nguyen et al., 2023), as medical cannabis may have been sourced from elsewhere (i.e. illegal cannabis market or legal recreational cannabis market).
We accordingly addressed these knowledge gaps by drawing upon a population-based survey of adults residing in Ontario (2014 to 2019). Our specific objectives were to: (1) characterize trends in medical cannabis use; (2) examine characteristics associated with medical cannabis use without medical authorization; and (3) examine the association between recreational cannabis legalization and medical cannabis use. Collectively, the findings will contribute to broadening our understanding of medical cannabis use in Canada.
2. Methods
2.1. Data source
Data were sourced from the Centre for Addiction and Mental Health (CAMH) Monitor Survey, a repeated, population-based, cross-sectional telephone survey of adults ≥18 years old in Ontario (Nigatu et al., 2020). The sampling methodology was comprised of regional stratification by six geographical units with equal sample size allocation, and two-stage (telephone number, household respondent) probability selection of telephone numbers using random-digit-dialing methods (Nigatu et al., 2020). In order to mitigate the impacts of non-coverage due to households with cell phones only, a dual sampling frame including a province-wide list-assisted random-digit-dialing sampling frame and a province-wide cell phone random-digit-dialing sampling frame was used starting in 2017 (Nigatu et al., 2020).
More than 19,500 respondents participated in the surveys between 2014 and 2019, with an average response rate of 38 % (Range: 28 % to 46 %) (see Table S1 in Supplementary Appendix for survey administration dates, sample sizes and response rates) (Nigatu et al., 2020). Following the provision of informed consent for participation, computer-assisted telephone interviewing was used to collect responses to a questionnaire. Importantly, a mixed matrix interview design with two-split ballot panels was operationalized in the data collection to reduce response burden (Nigatu et al., 2020). Further information regarding the survey is available elsewhere (Nigatu et al., 2020). All observations from the different iterations of the survey were aggregated into a pooled database (N = 19,543).
2.2. Measures
A three-category cannabis use measure was derived based on responses to two items. First, participants were asked about their cannabis use in the past 12 months, “How often, if ever, have you used cannabis, marijuana or hash during the past 12 months?” (Responses: never to more than once a day). Second, participants that indicated cannabis use in the past 12 months were further asked, “In the past 12 months have you ever used cannabis, marijuana or hash to manage pain, nausea, glaucoma, the symptoms of multiple sclerosis, or any other medical condition?” (Responses: yes, no). Responses to these two items were combined to reflect medical cannabis use (with or without recreational cannabis use), recreational cannabis use and no cannabis use. Medical cannabis use without medical authorization was ascertained based on responses to the item, “In the past 12 months, did you have medical authorization to use cannabis, marijuana or hash for medical purposes?” (Responses: yes, no).
Recreational cannabis legalization was coded as post-recreational cannabis legalization for all observations from and after October 2018 and pre-recreational cannabis legalization for all observations before October 2018. Additional covariates included survey iteration (2014–2016, 2017–2019), age (18–29, 30–39, 40–49, 50–64, 65+), sex (male, female), educational attainment (some post-secondary school or more, high school or less), household income (not stated or missing, <$70,000, ≥$70,000), rurality (non-rural, rural), immigration status (non-immigrant, immigrant), marital status (never married or previously married [widowed, divorced, separated], married or living with a partner), self-perceived physical health (excellent, very good or good, fair or poor), self-perceived mental health (excellent, very good or good, fair or poor), hazardous or harmful drinking (Alcohol Use Disorder Identification Test Score (AUDIT) Score < 8, AUDIT Score ≥ 8) (Babor et al., 2001) and current tobacco smoking (no current tobacco smoking, current tobacco smoking).
2.3. Statistical analyses
Descriptive statistics and cross-tabulations between recreational cannabis legalization and age, sex, educational attainment, income, rurality, immigration status and marital status were generated to describe the sample characteristics. Trends in medical cannabis use and recreational cannabis use were characterized next through Jointpoint regression analyses. The number of available data points (N = 6) permitted fitting of one linear segment to the time series. Annual percentage changes in medical cannabis use and recreational cannabis use were computed, which assumed the prevalence of a given year to change at a constant percentage of the prevalence of the previous year.
Associations between characteristics and medical cannabis use without medical authorization were then tested using logistic regression analyses. The model included age, sex, educational attainment, income, rurality, immigration status, marital status, self-perceived physical health, self-perceived mental health, hazardous or harmful drinking and current tobacco smoking. Odds ratios (ORs) for all characteristics were generated estimating the likelihood of medical cannabis use without medical authorization compared with medical cannabis use with medical authorization. Importantly, the analytical sample was restricted to those engaging in medical cannabis use.
Associations between recreational cannabis legalization and medical cannabis use and recreational cannabis use were subsequently tested using multinomial logistic regression analyses. The model included recreational cannabis legalization, survey iteration, age, sex, educational attainment, income, rurality, immigration status and marital status. ORs estimating the likelihood of medical cannabis use compared with no cannabis use, and recreational cannabis use compared with no cannabis use, pre-post recreational cannabis legalization were generated. Multiplicative interactions between recreational cannabis legalization and sex and age were tested to assess the presence of differential patterns of change.
A complete case analyses strategy was utilized, as data missingness amounted to ≤ 1 % for all measures other than income (24 %; missing data modeled as a separate category). All analyses accounted for the survey design, incorporated survey weights and applied the Taylor Series approximation in the variance estimation. All analyses were conducted using Jointpoint Regression Program (Version 4.9.1.0) and SUDAAN (Version 11.0.3).
2.4. Ethics approval
Informed consent was obtained from all participants included in the CAMH Monitor. Research ethics committee review and approval were obtained from the Research Ethics Board at CAMH (REB Number: 001-2021).
3. Results
The characteristics of the participants in the sample are presented in Table 1. The majority were under 50 years old (51 %), female (52 %) and had some post-secondary education (73 %). The majority were also non-rural (87 %), non-immigrants (77 %) and married or living with a partner (63 %), while half reported an income of ≥$70,000 (50 %).
Table 1.
Characteristics of adults in Ontario included in the centre for addiction and mental health monitor survey (2014–2019).
| Total Sample |
Stratification by Recreational Cannabis Legalization |
|||
|---|---|---|---|---|
| % (N) | Pre-Recreational Cannabis Legalization % (N) |
Post-Recreational Cannabis Legalization % (N) |
Chi-Square P-Value | |
| Age | <0.0001 | |||
| 65+ | 20 (6,964) | 19 (5,612) | 22 (1,352) | |
| 50–64 | 29 (6,086) | 29 (5,145) | 29 (941) | |
| 40–49 | 17 (2,746) | 18 (2,343) | 15 (403) | |
| 30–39 | 15 (1,701) | 15 (1,391) | 14 (310) | |
| 18–29 | 19 (1,872) | 19 (1,372) | 21 (500) | |
| Sex | 0.4084 | |||
| Male | 48 (7,901) | 48 (6,412) | 47 (1,489) | |
| Female | 52 (11,642) | 52 (9,602) | 53 (2,040) | |
| Educational Attainment | 0.3558 | |||
| Some post-secondary school or more | 73 (13,390) | 73 (10,961) | 72 (2,429) | |
| High school or less | 27 (5,977) | 27 (4,907) | 28 (1,070) | |
| Income | <0.0001 | |||
| Not stated or Missing | 25 (4,746) | 24 (3,800) | 28 (946) | |
| <$70,000 | 25 (6,361) | 25 (5,228) | 27 (1,133) | |
| ≥$70,000 | 50 (8,436) | 51 (6,986) | 45 (1,450) | |
| Rurality | <0.0001 | |||
| Non-rural | 87 (16,429) | 88 (13,599) | 83 (2,830) | |
| Rural | 13 (3,114) | 12 (2,415) | 17 (699) | |
| Immigration Status | 0.3450 | |||
| Non-immigrant | 77 (15,398) | 77 (12,648) | 76 (2,750) | |
| Immigrant | 23 (4,009) | 23 (3,241) | 24 (768) | |
| Marital Status | <0.0001 | |||
| Married or living with a partner | 63 (11,933) | 64 (9,966) | 59 (1,967) | |
| Never married or previously married (widowed, divorced or separated) | 37 (7,431) | 36 (5,903) | 41 (1,528) | |
Characteristics of the participants differed between the pre-recreational cannabis legalization and post-recreational cannabis legalization periods in regards to age, income, rurality and marital status. Specifically, proportions were higher of participants who were 18 to 29 years old and 65+ years old, reported a missing income and <$70,000 income, resided in a rural residence and were never married or previously married in the post-cannabis legalization period compared with the pre-cannabis legalization period.
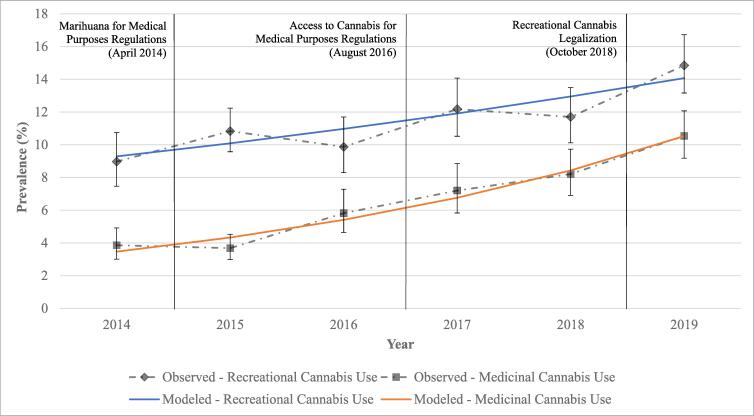
3.1. Trends in medical cannabis use and recreational cannabis use (2014–2019)
Trends in medical cannabis use and recreational cannabis use are displayed in Fig. 1. Medical cannabis use increased from 4 % (95 % Confidence Interval [CI]: 3 %, 5 %) in 2014 to 11 % (9 %, 12 %) in 2019, and recreational cannabis use increased from 9 % (7 %, 11 %) in 2014 to 15 % (13 %, 17 %) in 2019. Annual percentage change in medical cannabis use amounted to 25 % (95 % CI: 17 %, 33 %) and in recreational cannabis use amounted to 9 % (3 %, 15 %).
Fig. 1.
Prevalence of medical cannabis use and recreational cannabis use among adults in Ontario included in the Centre for Addiction and Mental Health Monitor Survey (2014–2019).
3.2. Characteristics associated with medical cannabis use without medical authorization
Medical cannabis use without medical authorization was predominant among those engaging in medical cannabis use (77 %). The logistic regression model examining the associations between characteristics and medical cannabis use without medical authorization is displayed in Table 2. Being 18 to 29 years old compared with being 65+ years old (OR, 95 % CI: 4.05, 2.12–7.72) was associated with an increased likelihood of medical cannabis use without medical authorization among those engaging in medical cannabis use. However, being of fair or poor self-perceived health compared with excellent, very good or good self-perceived health (0.61, 0.40–0.95) was associated with a decreased likelihood of medical cannabis use without medical authorization among those engaging in medical cannabis use.
Table 2.
Associations between characteristics and medical cannabis use without medical authorization among adults in Ontario included in the Centre for Addiction and Mental Health Monitor Survey (2014–2019).
|
Logistic Regression Model Medical Cannabis Use without Medical Authorization vs. Medical Cannabis Use with Medical Authorization OR (95 % CI) |
|
|---|---|
| Age | |
| 65+ (Reference) | |
| 50–64 | 1.55 (0.94–2.56) |
| 40–49 | 1.37 (0.70–2.69) |
| 30–39 | 1.72 (0.93–3.16) |
| 18–29 | 4.05 (2.12–7.72) |
| Sex | |
| Male (Reference) | |
| Female | 1.14 (0.77–1.69) |
| Educational Attainment | |
| Some post-secondary school or more (Reference) | |
| High school or less | 1.14 (0.75–1.74) |
| Income | |
| Not stated or Missing (Reference) | |
| <$70,000 | 1.43 (0.83–2.47) |
| ≥$70,000 | 1.75 (0.98–3.11) |
| Rurality | |
| Non-rural (Reference) | |
| Rural | 1.19 (0.69–2.04) |
| Immigration Status | |
| Non-immigrant (Reference) | |
| Immigrant | 0.68 (0.36–1.27) |
| Marital Status | |
| Married or living with a partner (Reference) | |
| Never married or previously married (widowed, divorced or separated) | 1.06 (0.70–1.61) |
| Self-Perceived Physical Health | |
| Excellent, very good or good (Reference) | |
| Fair or poor | 0.61 (0.40–0.95) |
| Self-Perceived Mental Health | |
| Excellent, very good or good (Reference) | |
| Fair or poor | 0.85 (0.51–1.40) |
| Hazardous or Harmful Drinking | |
| AUDIT < 8 (Reference) | |
| AUDIT ≥ 8 | 1.17 (0.76–1.81) |
| Current Tobacco Smoking | |
| No current tobacco smoking (Reference) | |
| Current tobacco smoking | 1.32 (0.85–2.04) |
Abbreviations: AUDIT, Alcohol Use Disorder Identification Test; CI, Confidence Interval; OR, Odds Ratio.
^Model includes age, sex, educational attainment, income, rurality, immigration status, marital status, self-perceived physical health, self-perceived mental health, hazardous or harmful drinking and current tobacco smoking.
3.3. Associations between recreational cannabis legalization and medical cannabis use and recreational cannabis use
The multinomial logistic regression model examining the associations between recreational cannabis legalization and medical cannabis use and recreational cannabis use is displayed in Table 3. Recreational cannabis legalization was associated with an increased likelihood of medical cannabis use compared with no cannabis use (OR, 95 % CI: 1.48, 1.19–1.85) and of recreational cannabis use compared with no cannabis use (1.35, 1.11–1.65). In regards to differential patterns of change by age and sex, multiplicative interactions with recreational cannabis legalization were non-significant (p = 0.3628 and p = 0.6656, respectively).
Table 3.
Associations between recreational cannabis legalization and medical cannabis use and recreational cannabis use among adults Ontario included in the Centre for Addiction and Mental Health Monitor Survey (2014–2019).
|
Multinomial Logistic Regression Model^ |
||
|---|---|---|
|
Recreational Cannabis Use vs. No Cannabis Use OR (95 % CI) |
Medical Cannabis Use vs. No Cannabis Use OR (95 % CI) |
|
| Recreational Cannabis Legalization | ||
| Pre-recreational cannabis legalization (Reference) | ||
| Post-recreational cannabis legalization | 1.35 (1.11–1.65) | 1.48 (1.19–1.85) |
| Survey Iteration | ||
| 2017–2019 (Reference) | ||
| 2014–2016 | 0.75 (0.63–0.88) | 0.52 (0.42–0.64) |
| Age | ||
| 65+ (Reference) | ||
| 50–64 | 3.36 (2.67–4.22) | 3.48 (2.68–4.53) |
| 40–49 | 4.22 (3.27–5.45) | 3.37 (2.45–4.64) |
| 30–39 | 7.33 (5.67–9.48) | 5.97 (4.32–8.25) |
| 18–29 | 14.48 (11.33–18.51) | 6.27 (4.57–8.60) |
| Sex | ||
| Male (Reference) | ||
| Female | 0.51 (0.44–0.58) | 0.47 (0.40–0.56) |
| Educational Attainment | ||
| Some post-secondary school or more (Reference) | ||
| High school or less | 1.00 (0.84–1.19) | 1.38 (1.14–1.67) |
| Income | ||
| Not stated or Missing (Reference) | ||
| <$70,000 | 1.66 (1.32–2.09) | 2.12 (1.63–2.75) |
| ≥$70,000 | 2.01 (1.63–2.48) | 1.43 (1.11–1.84) |
| Rurality | ||
| Non-rural (Reference) | ||
| Rural | 0.64 (0.52–0.79) | 0.87 (0.69–1.10) |
| Immigration Status | ||
| Non-immigrant (Reference) | ||
| Immigrant | 0.41 (0.33–0.51) | 0.28 (0.21–0.38) |
| Marital Status | ||
| Married or living with a partner (Reference) | ||
| Never married or previously married (widowed, divorced or separated) | 1.53 (1.29–1.82) | 1.59 (1.27–1.99) |
Abbreviations: CI, Confidence Interval; OR, Odds Ratio.
^Model includes recreational cannabis legalization, survey iteration, age, sex, educational attainment, income, rurality, immigration status and marital status.
4. Discussion
Medical cannabis use was examined using a population-based survey of adults in Ontario. Medical cannabis use increased between 2014 and 2019, with the annual percentage change approximating 25 %. However, the vast majority of those engaging in medical cannabis use did not possess medical authorization. Characteristics associated with an increased likelihood of medical cannabis use without medical authorization included younger age, while characteristics associated with a decreased likelihood of medical cannabis use without medical authorization included fair or poor self-perceived physical health. Recreational cannabis legalization was associated with increases in both recreational cannabis use and medical cannabis use.
The present findings pertaining to trends in medical cannabis use are consistent with previous research, which demonstrated an increase in medical cannabis use in the past 12 months in Canada from 12 % in 2017 to 14 % in 2019 (Government of Canada, 2019). However, the present findings suggest a lower prevalence, as the analogous estimates ranged from 7 % in 2017 to 11 % in 2019. The variation in prevalence may stem from the differences in the examined jurisdiction (Canada vs. Ontario) and the nature of the surveys (cannabis-specific content vs. substance use and mental health content) (Government of Canada, 2019). The latter difference has resulted in higher prevalence of cannabis consumption in comparison with other national population-based surveys, which may reflect potential participation bias due to the cannabis-specific content (Government of Canada, 2019).
In regards to the characteristics associated with medical cannabis use without medical authorization, the present findings are consistent with previous research that also highlighted the role of age (Balneaves et al., 2023). Indeed, the present findings indicated that those between 18 and 29 years old compared with those ≥65 years old had more than four-fold increased odds of engaging in medical cannabis use without medical authorization. However, sex, education, income and size of city were also previously identified as relevant characteristics (Balneaves et al., 2023), unlike the present findings. The difference in characteristics may be due to the differences in sampling strategy (non-probability-based vs. probability-based) and mode of survey administration (telephone vs. online) (Balneaves et al., 2023).
The present findings pertaining to the association between recreational cannabis legalization and medical cannabis use are not consistent with previous research. In contrast to the observed increased likelihood of medical cannabis use post-recreational cannabis legalization, previous research demonstrated that recreational cannabis legalization was associated with reductions in mail-order shipments of medical cannabis in Ontario and Canada (Nguyen et al., 2023). The difference in findings may be attributable to the differences in the data sources, as previous research was based on administrative records that captured medical cannabis use with medical authorization, whereas the present findings were based on population-based surveys that captured both medical cannabis use with and without medical authorization (Nguyen et al., 2023). Indeed, the vast majority of those engaging in medical cannabis use do not possess medical authorization (Government of Canada, 2019, Hamilton et al., 2017).
Although medical cannabis use has increased, it is largely being used without medical authorization. As such, those engaging in medical cannabis use may be self-medicating without clinical supervision, thereby potentially placing themselves at-risk of adverse health effects due to administration errors, dosing errors, drug-drug interactions and risk of use disorders (Leung et al., 2022). The observed associations between age and medical cannabis use without medical authorization further lends support to this point of view, as young adults are less likely to present with medical conditions that warrant medical cannabis use authorization. Indeed, medical cannabis use is often reported in the context of various diseases and symptoms, many of which lack a robust clinical evidence base. For example, among those engaging in medical cannabis use to treat diseases and manage symptoms in Canada, the most common conditions include chronic pain (67 %), sleep disorders (62 %), anxiety (64 %), stress (49 %) and depression (49 %) (Balneaves et al., 2023). In a systematic review of the efficacy of medical cannabis use, the evidence base was considered to be generally of very low quality or low quality in regards to sleep disorders, anxiety and depression (Whiting et al., 2015).
The increase in medical cannabis use post-recreational cannabis legalization may stem from the reduced stigma and broadened availability. Now that both medical cannabis use and recreational cannabis use are legal, there may be more willingness to experiment with medical cannabis use due to the increased social acceptability. However, the broadened availability has likely contributed to a greater degree to the increase in medical cannabis use post-recreational cannabis legalization, as more than 1,500 legal store fronts were operational in Ontario as of September 2022 (Myran et al., 2023a). Coupled with the known barriers to obtaining medical cannabis use authorization (e.g. lack of knowledge, too expensive, time consuming) (Balneaves et al., 2023), the evolving legal landscape may have facilitated access to medical cannabis from the unregulated or regulated cannabis market (Nguyen et al., 2023). After recreational cannabis legalization in Canada, the presence of the regulated cannabis market was among the foremost reasons for not obtaining medical authorization for medical cannabis use (Balneaves et al., 2023). Indeed, 54 % of those engaging in medical cannabis use changed the source of medical cannabis post-recreational cannabis legalization, with 80 % of them switching to the regulated cannabis market (Balneaves et al., 2023).
4.1. Limitations
Findings should be considered in the context of some limitations. First, certain segments of the target population were excluded from the sampling frame, including those who were homeless, hospitalized, incarcerated or living on military establishments. Second, the response rates of the surveys declined from 45 % in 2014 to 28 % in 2019, which is consistent with other telephone surveys (Wright, 2015). Pertinently, those who chose to participate versus those who chose not to participate may have differed in regards to cannabis use. In addition, changes in characteristics of participants that were included may have affected estimates of medical cannabis use and recreational cannabis use. A comparison of the participant characteristics that were included between 2014 and 2019 demonstrated that the samples were largely similar, with the exception of increases over time in participants 18–29 years and ≥65 years, participants with an income of ≤$70,000 and participants never married or previously married (see Table S2 in the Supplementary Appendix). It remains a possibility that the change in these characteristics may have contributed to the present findings pertaining to increases in medical cannabis use and recreational cannabis use. Importantly, the extent to which the nonresponse rate represents nonresponse bias is rarely known. As such, the nonresponse rate is best viewed as an indicator of the potential rather than the presence of nonresponse bias (Biemer and Lyberg, 2003, Groves and Peytcheva, 2008, Groves et al., 2004). These limitations related to exclusion of certain segments of the target population and declining response rates may have affected the generalizability of the findings. Third, the self-reported nature of the data was susceptible to social desirability and recall biases, which may have led to underestimation of cannabis use. However, self-reports of drug use have been shown to be valid (Darke, 1998). Fourth, the willingness to report cannabis consumption was not captured in the surveys, neither were chronic physical health conditions or mental health conditions. In regards to the willingness to report cannabis consumption, there may be ongoing impacts of cannabis normalization on cannabis consumption, resulting in more accurate self-reports of cannabis consumption over time. Indeed, evidence from other national surveys indicates that more than half of those who used cannabis during the past 12 months were more willing to disclose cannabis use since it was legal (Government of Canada, 2021). As such, the increases in medical cannabis use and recreational cannabis use observed pre-post cannabis legalization may reflect more accurate reporting rather than actual increases. Unfortunately, the extent of this limitation cannot be ascertained due to the absence of measures on cannabis normalization. In regards to chronic physical health or mental health conditions, they likely affect engagement with medical cannabis use. As such, the findings may be susceptible to residual confounding.
5. Conclusions
Medical cannabis use increased in Ontario, Canada. However, it continues to be largely used without medical authorization. Recreational cannabis legalization was associated with increases in medical cannabis use. As those engaging in medical cannabis use may be self-medicating, they may be at an increased risk of adverse health effects. As such, guidance and education that encourages medical usage under clinical supervision is recommended. In addition, mitigation of known barriers to medical cannabis use authorization is important to reduce procurement of medical cannabis from the unregulated or regulated cannabis market.
Disclosure of funding and conflict of interest
The authors acknowledge funding from the Canadian Institutes of Health Research’s and Canadian Centre on Substance Use and Addiction’s Partnerships for Cannabis Policy Evaluation Team Grant (Grant Number: 170394); and Canadian Institutes of Health Research’s Institute of Neurosciences, Mental Health and Addiction’s Canadian Research Initiative on Substance Misuse Ontario Node Grant (Grant Number: REN-181677). The authors declare no conflict of interest.
Role of funding source
The funding sources had no role in study design, data collection, analysis and interpretation, preparation of the manuscript or decision to publish the manuscript.
Sources of funding
The authors acknowledge funding from the Canadian Institutes of Health Research’s Institute of Neurosciences, Mental Health and Addiction’s Canadian Research Initiative on Substance Misuse Ontario Node Grant (Grant Number: REN-181677) and the Canadian Institutes of Health Research and Canadian Centre on Substance Use and Addiction’s Partnerships for Cannabis Policy Evaluation Team Grant (Grant Number: 170394).
CRediT authorship contribution statement
Sameer Imtiaz: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Conceptualization. Yeshambel T. Nigatu: Writing – review & editing, Validation, Methodology, Investigation, Data curation. Farihah Ali: Writing – review & editing, Resources, Funding acquisition. Tara Elton-Marshall: Writing – review & editing, Validation, Methodology, Investigation, Funding acquisition, Data curation. Jürgen Rehm: Writing – review & editing, Validation, Supervision, Resources, Methodology, Investigation, Funding acquisition. Sergio Rueda: Writing – review & editing, Validation, Methodology, Investigation, Funding acquisition. Hayley A. Hamilton: Writing – review & editing, Validation, Supervision, Methodology, Investigation, Funding acquisition, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2024.102805.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The data that has been used is confidential.
References
- Aminilari M., Busse J.W., Turna J., Mackillop J. Declared rationale for cannabis use before and after legalization for nonmedical use: A longitudinal study of community adults in Ontario. Cannabis Cannabinoid Res. 2022;1:1. doi: 10.1089/can.2021.0128. [DOI] [PubMed] [Google Scholar]
- Babor T.F., Higgins-Biddle J.C., Saunders J.B., Monteiro M.G. World Health Organization; Geneva, Switzerland: 2001. The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care. [Google Scholar]
- Balneaves L.G., Brown A., Green M., Prosk E., Rapin L., Monahan-Ellison M., McMillan E., Zaid J., Dworkind M., Watling C.Z. University of Manitoba, Medical Cannabis Canada, SheCann, Santé Cannabis, McGill University; Winnipeg, Manitoba: 2023. Medical cannabis access and experiences in Canada: Medical cannabis access survey summary report. [Google Scholar]
- Biemer P.P., Lyberg L.E. NY, Wiley; New York: 2003. Introduction to Survey Quality. [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. discussion 267–8. [DOI] [PubMed] [Google Scholar]
- Government of Canada, 2019. Canadian Cannabis Survey 2019: Summary. [Online]. Ottawa, Ontario: Government of Canada. Available: https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/canadian-cannabis-survey-2019-summary.html] [Accessed July 1 2020].
- Government of Canada, 2021. Canadian Cannabis Survey 2020: Summary [Online]. Ottawa, Ontario: Government of Canada. Available: https://www.canada.ca/en/health-canada/services/drugs-medication/cannabis/research-data/canadian-cannabis-survey-2020-summary.html] [Accessed November 22 2021].
- Groves R.M., Fowler F.J., Couper M.P., Lepkowski J.M., Singer E., Tourangeau R. Hoboken; NJ, Wiley: 2004. Survey Methodology. [Google Scholar]
- Groves R.M., Peytcheva E. The impact of nonresponse rates on nonresponse bias: A meta-analysis. Public Opin. Quart. 2008;72:167–189. [Google Scholar]
- Hamilton H.A., Brands B., Ialomiteanu A.R., Mann R.E. Therapeutic use of cannabis: Prevalence and characteristics among adults in Ontario, Canada. Can. J. Public Health. 2017;108:e282–e287. doi: 10.17269/CJPH.108.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HEALTH Canada . Health Canada; Ottawa, Ontario: 2016. Consumer Information—Cannabis (Marihuana, marijuana) [Google Scholar]
- Health Canada, 2017. Canadian Tobacco Alcohol and Drugs (CTADS): 2015 summary [Online]. Available: https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2015-summary.html [Accessed September 07, 2017].
- Health Canada, 2023. Canadian Alcohol and Drugs Survey (CADS): Summary of Results for 2019 [Online]. Ottawa, Ontario: Health Canada. Available: https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-summary.html#a3 [Accessed September 18 2023].
- Imtiaz S., Nigatu Y.T., Ali F., Douglas L., Hamilton H.A., Rehm J., Rueda S., Schwartz R.M., Wells S., Elton-Marshall T. Cannabis legalization and cannabis use, daily cannabis use and cannabis-related problems among adults in Ontario, Canada (2001–2019) Drug Alcohol Depend. 2023;244 doi: 10.1016/j.drugalcdep.2023.109765. [DOI] [PubMed] [Google Scholar]
- Imtiaz S., Nigatu Y.T., Sanches M., Ali F., Boak A., Douglas L., Hamilton H.A., Rehm J., Rueda S., Schwartz R.M., Wells S., Elton-Marshall T. Effects of cannabis legalisation on patterns of cannabis consumption among adolescents in Ontario, Canada (2001–2019) Drug Alcohol Rev. 2023 doi: 10.1111/dar.13786. [DOI] [PubMed] [Google Scholar]
- Leung J., Chan G., Stjepanovic D., Chung J.Y.C., Hall W., Hammond D. Prevalence and self-reported reasons of cannabis use for medical purposes in USA and Canada. Psychopharmacology (Berl) 2022;239:1509–1519. doi: 10.1007/s00213-021-06047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lintzeris N., Mills L., Abelev S.V., Suraev A., Arnold J.C., McGregor I.S. Medical cannabis use in Australia: consumer experiences from the online cannabis as medicine survey 2020 (CAMS-20) Harm Reduct. J. 2022;19:88. doi: 10.1186/s12954-022-00666-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myran D.T., Tanuseputro P., Auger N., Konikoff L., Talarico R., Finkelstein Y. Edible cannabis legalization and unintentional poisonings in children. N. Engl. J. Med. 2022;387:757–759. doi: 10.1056/NEJMc2207661. [DOI] [PubMed] [Google Scholar]
- Myran D.T., Friesen E.L., Dickson S., Konikoff L., Arora G., Tanuseputro P. Access to legal cannabis market in Canada over the four years following non-medical cannabis legalisation. Drug Alcohol Rev. 2023 doi: 10.1111/dar.13650. [DOI] [PubMed] [Google Scholar]
- Myran D.T., Gaudreault A., Konikoff L., Talarico R., Liccardo Pacula R. Changes in cannabis-attributable hospitalizations following nonmedical cannabis legalization in Canada. JAMA Netw Open. 2023;6 doi: 10.1001/jamanetworkopen.2023.36113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen H.V., Grootendorst P., Mital S., Bishop L., Mcginty E.E. Changes in medical cannabis use after recreational cannabis legalization in Canada. Cannabis Cannabinoid Res. 2023 doi: 10.1089/can.2022.0227. [DOI] [PubMed] [Google Scholar]
- Nigatu Y.T., Elton-Marshall T., Adlaf E.M., Ialomiteanu A.R., Mann R.E., Hamilton H.A. Centre for Addiction and Mental Health; Toronto, Ontario: 2020. CAMH Monitor eReport 2019: Substance Use, Mental Health and Well-Being Among Ontario Adults. [Google Scholar]
- Rotermann M. What has changed since cannabis was legalized? Health Rep. 2020;31:11–20. doi: 10.25318/82-003-x202000200002-eng. [DOI] [PubMed] [Google Scholar]
- Shim M., Nguyen H., Grootendorst P. Lessons from 20 years of medical cannabis use in Canada. PLoS One. 2023;18 doi: 10.1371/journal.pone.0271079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sznitman S.R. Do recreational cannabis users, unlicensed and licensed medical cannabis users form distinct groups? Int. J. Drug Policy. 2017;42:15–21. doi: 10.1016/j.drugpo.2016.11.010. [DOI] [PubMed] [Google Scholar]
- Walsh Z., Callaway R., Belle-Isle L., Capler R., Kay R., Lucas P., Holtzman S. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int. J. Drug Policy. 2013;24:511–516. doi: 10.1016/j.drugpo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- Whiting P.F., Wolff R.F., Deshpande S., di Nisio M., Duffy S., Hernandez A.V., Keurentjes J.C., Lang S., Misso K., Ryder S., Schmidlkofer S., Westwood M., Kleijnen J. Cannabinoids for medical use: A systematic review and meta-analysis. JAMA. 2015;313:2456–2473. doi: 10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- Wright G. An empirical examination of the relationship between nonresponse rate and nonresponse bias. Stat. J. IAOS. 2015;31:305–315. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.