Key Points
Question
To what extent are Medicare and Medicaid integrated care plans (ICPs) associated with differences in quality, spending, utilization, and patient outcomes among dual-eligible beneficiaries?
Findings
This systematic review including 26 ICP evaluations found evidence of associations between ICPs and reductions in long-term nursing home stays in 2 of 3 of categories of ICPs and some evidence of ICP association with greater outpatient care. However, for 1 category of ICPs, studies primarily found higher Medicare spending, and across ICP categories, evidence was limited or inconsistent regarding Medicaid spending, hospital admissions, care coordination, patient satisfaction, and health.
Meaning
These findings suggest that despite evidence of some ICPs being associated with outcomes consistent with policymakers’ objectives (eg, reducing nursing home stays), the literature is limited and inconclusive regarding other outcomes.
Abstract
Importance
Most dual-eligible Medicare-Medicaid beneficiaries are enrolled in bifurcated insurance programs that pay for different components of care. Therefore, policymakers are prioritizing expansion of integrated care plans (ICPs) that manage both Medicare and Medicaid benefits and spending.
Objective
To review evidence of the association between ICPs and health care spending, quality, utilization, and patient outcomes among dual-eligible beneficiaries.
Evidence Review
A search was conducted of PubMed/MEDLINE (January 1, 2010, through November 1, 2023) and Google Scholar (January 1, 2010, through October 1, 2023) and augmented with reports from US federal and state government websites. Three categories of ICPs were evaluated: Programs of All-Inclusive Care for the Elderly (PACE), Medicare-Medicaid Plans (MMPs), and Fully Integrated Dual Eligible Special Needs Plans (FIDE-SNPs) and related models aligning Medicare and Medicaid coverage. The review included studies that evaluated beneficiaries dually eligible for and enrolled in full Medicaid; compared an ICP to a nonintegrated arrangement; and evaluated utilization, spending, care coordination, patient experience, or health for 100 or more beneficiaries.
Findings
In all, 26 ICP evaluations met the inclusion criteria and were included in the analysis: 5 of PACE, 13 of MMPs, and 8 of FIDE-SNPs and other aligned models. Evidence generally showed associated reductions in long-term nursing home stays in PACE (3 of 4 studies) and FIDE-SNPs and related aligned models (3 of 5 studies) but was mixed in evaluations of MMPs. Four of 9 studies of MMPs and 2 of 3 studies of FIDE-SNPs found higher outpatient use, although other studies showed no difference. Evidence on Medicaid spending was limited, whereas 8 of 10 studies of MMPs showed an association between these plans and higher Medicare spending. Evidence was mixed or inconclusive regarding care coordination and hospitalizations, and it was insufficient to evaluate patient satisfaction, health, and outcomes in beneficiary subgroups (eg, those with serious mental illness). Furthermore, studies had limited ability to control for bias from unmeasured differences between enrollees of ICPs compared with nonintegrated models.
Conclusions and Relevance
This systematic review found variability and gaps in evidence regarding ICPs and spending, quality, utilization, and outcomes. Studies found some ICPs were associated with reductions in long-term nursing home admissions, and several identified increases in outpatient care. However, MMPs were primarily associated with higher Medicare spending. Evidence for other outcomes was limited or inconclusive. Research addressing these evidence gaps is needed to guide ongoing efforts to integrate coverage and care for dual-eligible beneficiaries.
This systematic review assesses the evidence of the association between integrated care programs and health care quality, spending, utilization, and patient outcomes among Medicare-Medicaid dual-eligible beneficiaries.
Introduction
US state and federal policymakers are pursuing reforms to promote higher quality and fiscally sustainable care for the nation’s 12.5 million dual-eligible Medicare and Medicaid beneficiaries. A central focus of these reforms has been the expansion of integrated care programs (ICPs), which coordinate care for dual-eligible beneficiaries and bear risk for both Medicare and Medicaid spending.1,2,3
ICPs are intended to address concerns that a lack of coordination between Medicare and Medicaid results in poor quality and inefficient care.4 For dual-eligible beneficiaries, Medicare (a federal program) is the primary payer for outpatient, hospital, and postacute care, while Medicaid (administered by states) pays for long-term care, including nursing home care and home- and community-based services (HCBS) and some behavioral health care.5 However, 90% of dual-eligible beneficiaries are not enrolled in ICPs, meaning that their Medicare- and Medicaid-covered services and spending are managed by separate entities.6 Research has shown that a lack of integration hinders care coordination and produces unintended incentives to shift costs between Medicare and Medicaid.4,7,8,9 Additionally, there are concerns that nonintegrated care contributes to poor outcomes for beneficiaries with substantial needs, such as those with serious mental illness or receiving long-term services and supports.10,11
Policymakers have highlighted 3 distinct categories of ICPs as templates for integrated program expansion: Programs of All-Inclusive Care for the Elderly (PACE), Medicare-Medicaid Plans (MMPs), and Fully Integrated Dual Eligible Special Needs Plans (FIDE-SNPs).2 PACE is a managed care program that serves community-dwelling adults 55 years and older who need nursing home−level care, most of whom are dual-eligible beneficiaries.12 This program covers all Medicare and Medicaid services and provides supportive services in adult day health centers. MMPs receive blended capitation payments from Medicare and Medicaid. The plans were tested by 10 states starting in 2013 under the Centers for Medicare & Medicaid (CMS) Financial Alignment Demonstration, and continued to operate in 9 states in 2023 (all MMPs are scheduled to end by 2025).1,2 FIDE-SNPs are a subset of Dual-Eligible Special Needs Plans (D-SNPs), which are Medicare Advantage (MA) plans that exclusively serve dual-eligible beneficiaries.2 Unlike most D-SNPs, which only manage Medicare spending, FIDE-SNPs also bear risk for Medicaid spending through capitation contracts with Medicaid programs, or in some cases, through an affiliated Medicaid managed care plan.6
Proposals to expand ICPs have motivated an interest in understanding whether existing programs provide higher quality and efficient care.3,13 While there have been prior efforts to track and compile evidence on ICPs,14,15,16 to our knowledge, this literature has not been systematically reviewed. Therefore, we systematically reviewed evidence on the association of PACE, MMPs, and FIDE-SNPs with health care use, quality of care, spending, patient-reported experiences, and health outcomes across categories of ICPs and in subpopulations of dual-eligible beneficiaries. We also evaluated the quality of available evidence, including methods to address selection bias that can arise because enrollment in ICPs is voluntary and there may be unmeasured differences between beneficiaries who enroll in ICPs compared with other plans.16
Methods
We conducted this systematic review using the relevant sections of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines. We developed prespecified search criteria for PubMed and Google Scholar and augmented search results with evaluations published on government websites. The eMethods in Supplement 1 describes our search strategy and inclusion criteria. This review included studies that compared ICPs to nonintegrated arrangements. We included 3 types of ICPs: PACE, MMPs, and FIDE-SNPs and related models that align coverage across Medicare and Medicaid. Other aligned models included the Massachusetts Senior Care Options (SCO)17 and Minnesota Senior Health Options (MSHO)18 programs, which were precursors to FIDE-SNPs and are now classified as FIDE-SNPs,2 and arrangements in which beneficiaries enrolled in companion Medicare and Medicaid managed care plans operated by the same parent insurers (Tennessee19 and Oregon20). Evaluations of managed fee-for-service plans in Colorado and Washington under the CMS Financial Alignment Demonstration were not included because most proposals to expand ICPs focus on capitated models.3
Nonintegrated arrangements were those in which Medicare spending was managed separately from Medicaid and included fee-for-service Medicare, conventional MA plans, and coordination-only D-SNPs.1 Coordination-only D-SNPs were rarely assessed as the comparison group, and we did not classify these plans as ICPs because they do not manage Medicaid spending.
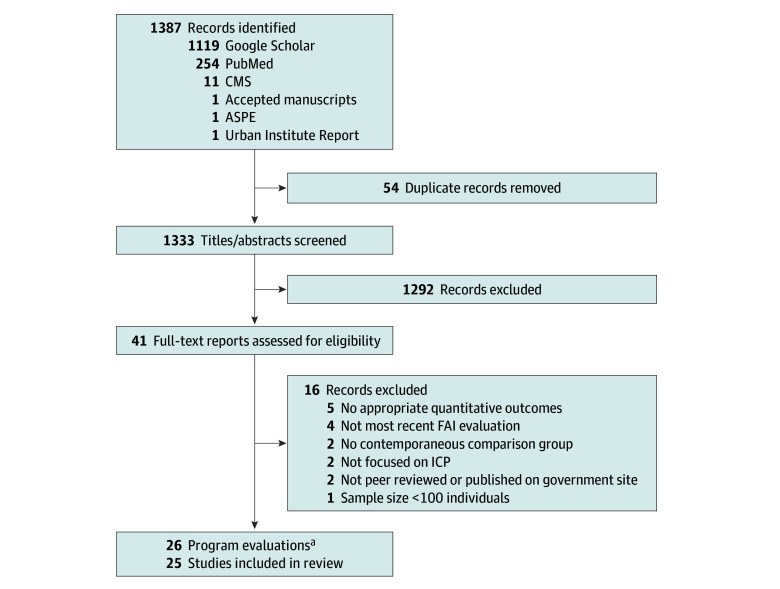
We limited this review to studies of dual-eligible beneficiaries with full Medicaid, who are the focus of integration policy because they qualify for all Medicaid-covered services, including long-term care.2 We further limited our review to studies with at least 100 participants; that reported quantitative findings for at least 1 quality, spending, utilization, patient experience, or health outcome; and that were published or accepted for publication from January 1, 2010, to October 1, 2023 (Google Scholar), and November 1, 2023 (PubMed and government websites). We incorporated updated findings from 3 federally funded MMP evaluations from December 2023. The Figure shows the PRISMA diagram for study inclusion.
Figure. Study Inclusion PRISMA Flow Diagram.
aIn all, 25 unique studies were included in this review: 24 that evaluated assessed a single type of ICP and 1 that assessed both PACE and FIDE-SNPs. For our review, we counted the latter study twice (1 set of findings for each program), producing 26 evaluations: 5 of PACE programs, 13 of MMPs, and 8 of FIDE-SNPs and similar managed care models. For 3 of the MMP evaluations, updated reports were published in December 2023, after our initial screening and data extraction was concluded. We incorporated updated findings from these latest evaluations to reflect the most recent set of reported results.
ASPE indicates the US Office of the Assistant Secretary for Planning and Evaluation; CMS, the US Centers for Medicare & Medicaid Services; FAI, Financial Alignment Initiative; FIDE-SNPs, Fully Integrated Dual Eligible Special Needs Plans; ICP, integrated care plan; MMPs, Medicare-Medicaid Plans; and PACE, Programs of All-Inclusive Care for the Elderly.
Data Abstraction
For each study, 1 author (E.T.R.) abstracted the following information: ICP evaluated; number and age of beneficiaries included scope (single state, several states, or national); research design (observational cross-sectional, observational longitudinal, or quasi-experimental); and findings. This author (E.T.R.) also evaluated the quality of evidence based on how each study addressed selection bias. A second author (C.E.D. or R.S.) independently checked this information (eMethods in Supplement 1 for details).
Based on the literature and conceptual frameworks for integrated coverage, we characterized the expected association between ICPs and spending, quality, utilization, patient experience, and health outcomes.21,22,23 These hypothesized associations include, for example, fewer long-term nursing home admissions, increased use of HCBS (ie, community-based long-term services and supports to assist older adults and people with a disability), and better patient-reported experience with health plans. We counted the number of studies whose results were consistent with, contrary to, and mixed or inconclusive regarding these hypothesized findings. Because of differences across ICPs, we reported findings separately for each ICP type and did not conduct a quantitative meta-analysis.
Results
Summary of Studies
Twenty-five unique studies were included in this review: 24 that evaluated a single type of ICP and 1 that evaluated both PACE and FIDE-SNPs.22 We counted the latter study twice (1 set of findings for each program) for a total of 26 program evaluations: 5 of PACE, 13 of MMPs, and 8 of FIDE-SNPs and other aligned models (Table 1).12,17,18,19,20,21,22,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41 Fourteen studies assessed ICPs over periods of less than 5 years (1 of PACE, 7 of MMPs, and 6 of FIDE-SNPs and other aligned models), and 12 assessed study periods of 5 years or longer (4 of PACE, 6 of MMPs, and 2 of FIDE-SNPs and other aligned models). Studies of PACE were limited to beneficiaries 55 years and older and evaluations of Massachusetts’ MMP were limited to those 65 years or younger, reflecting these programs’ eligibility criteria; other studies either included dual-eligible beneficiaries of all ages or only those 65 years and older. Twenty-four studies primarily used administrative data and 2 used survey data.
Table 1. Characteristics of Included Studies on Dual-Eligible Medicare-Medicaid Beneficiaries in Integrated Care Programs (ICP).
| Sourcea | No. of beneficiaries, stateb | Primary data source and years | ICP evaluation time, y | Beneficiaries’ age, y | Subgroups evaluated | Designc | Qualityd |
|---|---|---|---|---|---|---|---|
| PACE e | |||||||
| Chapin et al,34 2013 | 136 Enrolled, Kansas | Administrative, 2006-2011 | 5.5 | ≥65 | People eligible for NH-level caree; with frailty; with greater cognitive needs; or at end of life | Observational, longitudinal | 3 |
| Feng et al,22 2021 | 25 665 Enrolled, national | Administrative, 2015 | 1 | ≥55 | People eligible for NH-level caree | Observational, cross-sectional | 4 |
| Ghosh et al,12 2015 | 3725 Enrolled, 8 states | Administrative, 2006-2011 | 5.5 | ≥66 | People eligible for NH-level caree | Observational, longitudinal | 3 |
| Segelman et al,36 2017 | 4733 Enrolled, 12 states | Administrative, 2005-2009 | 3-5 | ≥55 | People eligible for NH-level caree | Observational, longitudinal | 3 |
| Wieland et al,35 2013 | 948 Enrolled, South Carolina | Administrative, 1994-2005 | 11 | ≥55 | People eligible for NH-level caree | Observational, longitudinal | 3 |
| MMPs f | |||||||
| Caswell et al,21 2023 | 16 680 eligible, Massachusetts | Administrative, 2016-2018 | 3 | ≤64 | Not evaluated | Quasi-experimental | 3 |
| Chen et al,39 2018 | 13 370 Enrolled, South Carolina | Administrative, 2011-2016 | 2 | ≥65 | Not evaluated | Observational, longitudinal | 3 |
| Chepaitis et al,26 2021 | 57 937 Eligible, Virginia | Administrative, 2012-2017 | 4 | ≥21h | Not evaluated | Quasi-experimental | 3 |
| Gattine et al,28 2023 | 118 443 Eligible, Massachusetts | Administrative, 2011-2019 | 6 | ≥21 to ≤64 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| Graham et al,38 2018 | 488 Enrolled, California | Survey, 2016-2017 | 6-22 mo | ≥21 | Not evaluated | Observational, cross-sectional | 4 |
| Griffin et al,24 2023 | 141 966 eligible, Ohio | Administrative, 2012-2020 | 6.5 | ≥18 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| Griffin et al,33 2023 | 157 348 eligible, Texas | Administrative, 2013-2020 | 6 | ≥21 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| Holladay et al,29 2022 | 109 548 eligible | Administrative, 2013-2018 | 4 | ≥21 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| Holladay et al,25 2022 | 263 128 eligible | Administrative, 2012-2019 | 5 | ≥21 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| Howard et al,27 2023 | 25 410 eligible, South Carolina | Administrative, 2013-2020 | 6 | ≥65 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| Snow et al,32 2023 | 22 488 eligible, New York | Administrative, 2014-2020 | 4.75 | ≥21 | People with intellectual and developmental disabilities | Quasi-experimental | 3 |
| Khatutsky et al,31 2023 | 479 461 eligible, California | Administrative, 2012-2019 | 6 | ≥21 | Not evaluated | Quasi-experimental | 3 |
| Gattine et al,30 2023 | 37 126 eligible, Rhode Island | Administrative, 2014-2020 | 4.5 | ≥21 | People receiving LTSS and populations with SPMI | Quasi-experimental | 3 |
| FIDE-SNPs and similar managed care models g | |||||||
| Anderson et al,18 2020 | 99 761 Enrolled, Minnesota | Administrative, 2010-2012 | 3 | ≥65 | Not evaluated | Observational, cross-sectional | 4 |
| Feng et al,22 2021 | 89 949 Enrolled, national | Administrative, 2015 | 1 | ≥21 | Not evaluated | Observational, cross-sectional | 4 |
| JEN Associates,17 2013 | 12 064 Enrolled, Massachusetts | Administrative, 2004-2009 | 6 | ≥65 | Not evaluated | Observational, longitudinal | 3 |
| Jung et al,40 2015 | 1090 Enrolled, Massachusetts | Administrative, 2007-2009 | 3 | ≥65 | People hospitalized with CHF or COPD | Observational, longitudinal | 3 |
| Keohane et al,19 2021 | 129 731 Eligible, Tennessee | Administrative, 2011-2017 | 6-7 | ≥21 | People receiving LTSS | Quasi-experimental | 3 |
| Kim et al,20 2019 | About 17 320 Enrolled | Administrative, 2011-2014 | 4 | ≥18 | Not evaluated | Observational, longitudinal | 3 |
| Meyers et al,41 2023 | 10 565 Enrolled, national | Survey, 2015-2018 | 4 | ≥21 | Not evaluated | Observational, cross-sectional | 4 |
| Roberts et al,37 2023 | 7967 Enrolled, Pennsylvania | Administrative, 2015-2020 | 3 | ≥21 | People eligible for NH-level care | Observational, longitudinal | 3 |
Abbreviations: CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; FIDE-SNPs, Fully Integrated Dual Eligible Special Needs Plans; LTSS, long-term services and supports; MMPs, Medicare-Medicaid Plans; NH, nursing home; PACE, Programs of All-Inclusive Care for the Elderly; SPMI, serious and persistent mental illness.
eTable 4 in Supplement 1 provides details on data extracted.
Either number of people ICP eligible or enrolled, per study design.
Cross-sectional compared dual-eligible beneficiaries with vs without ICP at a single point in time or pooled over multiple periods; longitudinal examined cohorts over multiple periods or trends in repeated cross-sections; quasi-experimental included difference-in-differences and regression discontinuity designs.
Rating scale: 1, randomized clinical trial or systematic review with meta-analysis; 2, controlled trial without randomization or prospective comparative cohort trial; 3, case-control or retrospective cohort study; 4, case series with or without intervention or cross-sectional study; 5, opinion of respected authorities or case reports.
All PACE beneficiaries are eligible for NH-level care.
Quantitative studies of capitated MMPs tested under the Financial Alignment Demonstration only; excluded managed fee-for-service plans.
Either fully integrate Medicare and Medicaid spending or have dual-eligible beneficiaries in aligned Medicare and Medicaid managed care plans operated by the same insurer.
Spending
Eleven studies evaluated Medicare spending (1 of PACE and 10 of MMPs) and 7 studies evaluated Medicaid spending (3 of PACE and 4 of MMPs); neither Medicare nor Medicaid spending was assessed in studies of FIDE-SNPs (Table 2). Eight evaluations found an association of MMPs implementation with increased Medicare spending of $36.98 to $118.05 per person-month during 4.0 to 6.5 years,24,25,26,27,28,29,30,31 whereas 2 MMP evaluations and 1 PACE study found no significant difference in Medicare spending.12,32,33 Two studies of PACE found lower Medicaid spending,34,35 1 study of PACE and 2 studies of MMPs found an increase in Medicaid spending,12,28,31 and 2 studies of MMPs found no difference.32,33 Only 1 study of PACE and 4 studies of MMPs analyzed both Medicare and Medicaid spending (eTable 1 in Supplement 1).
Table 2. Summary of Findings, by Type of Integrated Care Plan (ICP).
| Type | Studies assessing outcome, No. | Hypothesized ICP effecta | Principal findings | ||
|---|---|---|---|---|---|
| Support hypothesis | Contradict hypothesis | Null or mixed | |||
| PACE | |||||
| Spending | |||||
| Medicare spending | 1 | Reduction | 0 | 0 | 1 |
| Medicaid spending | 3 | Reduction | 2 | 1 | 0 |
| Utilization | |||||
| Long-term nursing home stays | 4 | Reduction | 3 | 0 | 1 |
| Hospital admissions, overall | 2 | Reduction | 1 | 0 | 1 |
| Skilled nursing facility use | 0 | Reduction | 0 | 0 | 0 |
| ED visits | 2 | Reduction | 1 | 0 | 1 |
| Outpatient visits (excluding ED) | 0 | Increase | 0 | 0 | 0 |
| HCBS | 0 | Increase | 0 | 0 | 0 |
| Coordination and quality of care | |||||
| Care coordination | 0 | Increase | 0 | 0 | 0 |
| Hospital readmissions | 0 | Reduction | 0 | 0 | 0 |
| Hospital admissions for ambulatory care-sensitive conditions | 0 | Reduction | 0 | 0 | 0 |
| Patient experience and health outcomes | |||||
| Patient satisfaction with care | 0 | Improvement | 0 | 0 | 0 |
| Mortality | 3 | Reduction | 1 | 0 | 2 |
| MMPs | |||||
| Spending | |||||
| Medicare spending | 10 | Reduction | 0 | 8 | 2 |
| Medicaid spending | 4 | Reduction | 0 | 2 | 2 |
| Utilization | |||||
| Long-term nursing home stays | 8 | Reduction | 4 | 2 | 2 |
| Hospital admissions, overall | 10 | Reduction | 2 | 2 | 6 |
| Skilled nursing facility use | 9 | Reduction | 3 | 2 | 4 |
| ED visits | 10 | Reduction | 1 | 3 | 6 |
| Outpatient visits (excluding ED) | 9 | Increase | 4 | 0 | 5 |
| HCBS | 2 | Increase | 1 | 0 | 1 |
| Coordination and quality of care | |||||
| Care coordination | 8 | Increase | 1 | 0 | 7 |
| Hospital readmissions | 8 | Reduction | 2 | 2 | 4 |
| Hospital admissions for ambulatory care-sensitive conditions | 8 | Reduction | 1 | 1 | 6 |
| Patient experience and health outcomes | |||||
| Patient satisfaction with care | 1 | Improvement | 0 | 0 | 1 |
| Mortality | 0 | Reduction | 0 | 0 | 0 |
| FIDE-SNPs and similar managed care models | |||||
| Spending | |||||
| Medicare spending | 0 | Reduction | 0 | 0 | 0 |
| Medicaid spending | 0 | Reduction | 0 | 0 | 0 |
| Utilization | |||||
| Long-term nursing home stays | 5 | Reduction | 3 | 0 | 2 |
| Hospital admissions, overall | 5 | Reduction | 1 | 1 | 3 |
| Skilled nursing facility use | 2 | Reduction | 0 | 0 | 2 |
| ED visits | 5 | Reduction | 1 | 1 | 3 |
| Outpatient visits (excluding ED) | 3 | Increase | 2 | 0 | 1 |
| HCBS | 4 | Increase | 2 | 0 | 2 |
| Coordination and quality of care | |||||
| Care coordination | 1 | Increase | 0 | 0 | 1 |
| Hospital readmissions | 2 | Reduction | 0 | 0 | 2 |
| Hospital admissions for ambulatory care−sensitive conditions | 2 | Reduction | 1 | 0 | 1 |
| Patient experience and health outcomes | |||||
| Patient satisfaction with care | 1 | Improvement | 1 | 0 | 0 |
| Mortality | 2 | Reduction | 2 | 0 | 0 |
Abbreviations: ED, emergency department; FIDE-SNPs, Fully Integrated Dual Eligible Special Needs Plans; HCBS, home- and community-based services; MMPs, Medicare-Medicaid Plans; PACE, Programs of All-Inclusive Care for the Elderly.
Hypothesized effect reflects the difference in the outcome expected compared with nonintegrated coverage for dual-eligible beneficiaries.
Health Service Utilization
Seventeen studies evaluated long-term nursing home stays (ie, stays exceeding 90-100 days), including 4 studies of PACE, 8 of MMPs, and 5 of FIDE-SNPs and other aligned models (Table 2). Three studies associated PACE with a lower likelihood of long-term nursing home placement.12,22,36 One study found that PACE enrollees had greater cognitive impairment on nursing home entry, suggesting that the program enabled beneficiaries to remain in the community longer before transitioning to a nursing home.36 Another study found PACE enrollees had a 2 to 4 percentage points (pp) lower risk of long-term nursing home stays in any 6-month interval compared to Medicaid enrollees in an HCBS waiver program, although it did not find a cumulative difference in long-term nursing home use. Using a broader comparison group of HCBS waiver and long-term nursing home-eligible enrollees, the study found lower 6-month and cumulative long-term nursing home use in PACE.12 Four studies found an association of MMPs with annual reductions in the probability of long-term nursing home stays of 0.5 to 4.2 pp (10.1% to 24.7% lower than baseline),24,27,28,33 while 2 associated MMPs with increases in nursing home stays and 2 reported null findings.21,30 Three studies found an association between FIDE-SNPs or other aligned programs and reductions in long-term nursing home use, 2 reported reductions of 16% to 68% relative to baseline, and 1 estimated that a 10-pp increase in aligned plan enrollment was associated with 0.3 fewer nursing home residents per month per 100 beneficiaries.17,19,22 Null findings for long-term nursing home use were reported in 1 study of PACE and 2 studies of FIDE-SNPs and other aligned models.18,34,37
Twelve studies evaluated outpatient care (9 of MMPs, 3 of FIDE-SNPs, and no studies of PACE). Increases in outpatient care were found in 4 studies of MMPs and 2 of FIDE-SNPs and other aligned models.18,20,25,28,29,30 Null findings were reported in 5 studies of MMPs and 1 study of an FIDE-SNP.21,24,27,33,37,38 No studies reported reductions in outpatient care.
HCBS use was assessed in 2 studies of MMPs and 4 studies of FIDE-SNPs and other aligned models. Two studies of FIDE-SNPs found that dual-eligible beneficiaries in these plans used substantially more HCBS than enrollees in nonintegrated plans.22,37 One study of Massachusetts’ MMP, which used a regression discontinuity design based on the age cutoff for program eligibility (which covered dual-eligible beneficiaries 64 years and younger) found that beneficiaries just under the program’s age eligibility threshold were 5.1% more likely to receive a health assessment to receive HCBS compared with individuals older than this threshold.21 However, a study of California’s MMP found no difference in enrollee-reported use of in-home support services compared to dual-eligible beneficiaries in California counties where the MMP was not offered.38 No studies of PACE evaluated HCBS use as an outcome, likely because supportive services in adult day health centers are embedded in this program’s design.
Studies of MMPs and FIDE-SNPs and other aligned models mostly reported inconsistent or null findings for hospital admissions, emergency department visits, and skilled nursing facility use.17,18,19,20,21,27,28,29,30,33,34,37,38,39 These outcomes were evaluated in few or no studies of PACE.
Coordination and Quality of Care
A process-related care coordination measure, such as having a follow-up outpatient visit after a hospital stay, was reported in 9 studies (8 of MMPs, 1 of an FIDE-SNP, and none of PACE). All but 1 of these studies24 found no difference in care coordination associated with ICPs.25,27,28,29,30,33,37,38 All-cause 30-day hospital readmissions were evaluated in 10 studies (8 of MMPs and 2 of FIDE-SNPs or other aligned models), which reported varying findings (fewer readmissions in 2 studies of MMPs,24,27 increases in 2 studies of MMPs,28,33 and no difference in 4 studies of MMPs and 2 of FIDE-SNPs20,21,25,29,30,40). Studies mostly reported null findings regarding hospitalizations for ambulatory care-sensitive conditions.21,24,25,29,30,33,37
Patient Experience
Only 2 studies evaluated patient-reported experiences with care. One study found few differences in care satisfaction between enrollees in California’s MMP compared with dual-eligible beneficiaries in California counties where the MMP was not offered.38 A study using national Consumer Assessment of Healthcare Providers and Systems data from 2015 to 2018 found that FIDE-SNP enrollees reported higher overall ratings of their health plan than dual-eligible beneficiaries in conventional MA plans and coordination-only D-SNPs. However, FIDE-SNPs received comparable or lower ratings in other care domains.41
Health Outcomes
The most common health outcome studied was mortality (assessed in 3 studies of PACE and 2 of FIDE-SNPs and other aligned models). Two studies reported no difference in mortality between enrollees of PACE compared with nonintegrated arrangements,22,34 while 2 studies of FIDE-SNPs and 1 of PACE associated these programs with lower mortality.12,17,22 However, researchers cautioned that mortality differences could reflect selection bias rather than a causal effect of integrated care.12,22 For example, Ghosh et al12 estimated that cohorts of new PACE enrollees had lower mortality rates over 5 years (8-17 pp) than matched comparison cohorts of dual-eligible beneficiaries entering nursing homes or HCBS waiver programs. This difference narrowed to 2 to 5 pp when PACE enrollees were compared only to HCBS waiver enrollees. Due to the sensitivity of estimates to the comparison group, and the potential that matching did not fully account for confounders, the researchers concluded that selection bias was a concern.12 No studies evaluated patient-reported health.
Subgroup Analyses
Fourteen studies evaluated beneficiaries with frailty or needing nursing home−level care,12,19,22,24,25,27,28,29,30,33,34,35,36,37 including all studies of PACE (reflective of the program’s eligibility criteria). Seven studies evaluated beneficiaries with a serious mental illness,24,25,27,28,29,30,33 and 2 studies evaluated people with cognitive impairment or an intellectual disability.32,34 Studies assessing these subgroups evaluated different outcomes, and there were often few subgroup-specific findings per outcome (eTable 3 in Supplement 1). Consequently, there was insufficient evidence to characterize the overall direction of findings for specific beneficiary subgroups.
Study Design and Quality of Evidence
Fourteen studies used observational designs that compared dual-eligible beneficiaries in ICPs vs nonintegrated arrangements (all studies of PACE, 2 of MMPs, and 7 of FIDE-SNPs and other aligned models) (Table 1). Five observational studies used cross-sectional designs that compared enrollees in ICPs vs nonintegrated plans, either at a single point in time or pooled over several periods.18,22,38,41 Nine observational studies used longitudinal designs that compared changes in outcomes between cohorts of beneficiaries enrolled in ICPs vs nonintegrated plans.12,17,20,34,35,36,37,39,40 In both categories of observational studies, researchers used propensity score weighting, matching, or covariate adjustment to control for observed enrollee characteristics (eg, chronic conditions) that differed across plans. However, the quality of this evidence was rated as limited because the studies could not control for unmeasured confounders, such as differences in frailty, mobility, or social support.
Twelve studies—all but 1 assessing MMPs19—used quasi-experimental methods to mitigate bias from unmeasured confounders. Ten MMP studies used difference-in-differences designs that compared outcome changes among dual-eligible beneficiaries in counties where MMPs were implemented vs counties where these plans were unavailable.24,25,26,27,28,29,30,31,32,33 This approach leverages policy-driven changes in availability of MMPs to identify treatment effects, which can reduce bias because these changes are unlikely to be correlated with unmeasured person-level confounders.16 Another study used a regression discontinuity design to compare beneficiaries across the age eligibility cutoff (≤64 years) for Massachusetts’ MMP.21 These authors showed that beneficiary characteristics were balanced across this cutoff, suggesting that outcome differences across the cutoff were associated with OneCare eligibility. However, this approach identifies treatment effects close to the cutoff, which may not generalize to the broader population of dual-eligible beneficiaries. Among quasi-experimental studies, the quality of evidence was rated as moderate due to bias concerns and generalizability limitations.
Discussion
This systematic review found considerable variability and gaps in evidence about the association of ICPs with health care quality, spending, utilization, and patient-reported and other health outcomes among dual-eligible beneficiaries. Six key themes emerged in this review. First, studies generally found reductions or delays in the onset of long-term nursing home care in PACE, FIDE-SNPs, and other aligned models, but evidence regarding long-term nursing home use was mixed in evaluations of MMPs. Second, several studies of MMPs and FIDE-SNPs or other aligned models found increased outpatient care and HCBS use, but other studies of these ICPs showed no difference. Third, across ICP categories, mostly null or inconsistent findings were reported for care coordination and hospitalizations. Fourth, most studies associated MMPs with higher Medicare spending, although few studies evaluated Medicaid spending, and no evaluations of FIDE-SNPs or similar aligned models evaluated spending, to our knowledge. Fifth, evidence was limited regarding patient satisfaction, beneficiary health, and outcomes in clinically important subpopulations of dual-eligible beneficiaries, such as those with serious mental illness. Sixth, studies often had limited ability to control for selection bias. Therefore, although the literature suggests that some ICPs are associated with outcomes aligned with policy goals (eg, reducing long-term nursing home care), it also highlights limitations of existing evidence that require urgent attention.
A notable limitation was that the availability of evidence varied across ICPs and was insufficient to evaluate outcomes for certain plan types. For example, patient satisfaction with care was evaluated in only 1 study of an MMP and 1 of FIDE-SNPs, spending was not evaluated in any study of FIDE-SNPs, and HCBS use was not analyzed in evaluations of PACE. However, this last omission may reflect that supportive services in adult day health centers are integral to PACE’s design, and thus, were not considered an outcome.
Furthermore, most studies relied on administrative data (eg, claims or encounter data), while few surveyed patients about their access to or experiences with care. This presents challenges for assessing whether utilization and spending changes reflected improved or worsened care. For example, it is not necessarily the case that better care management should lead to uniform increases or decreases in utilization and spending, and improved access to care could increase beneficiaries’ use of and spending on some services. Likewise, limited data on patient-reported outcomes (eg, getting help with activities of daily living or engagement with a care coordinator) made it difficult to assess whether ICPs addressed beneficiaries’ care needs.
Therefore, this review highlights several areas where research is needed to rigorously appraise the performance of ICPs. First, research is needed to evaluate combined Medicaid and Medicare spending. Second, assessment of patient-reported outcomes is critical for evaluating whether ICPs improve care in areas salient to dual-eligible beneficiaries, such as care coordination and quality of long-term care. Third, research is needed to assess outcomes in subgroups of dual-eligible beneficiaries with complex needs.
Fourth, our review highlights a need to address methodological limitations of the literature, most of which stem from the challenge of identifying appropriate comparison groups. Because enrollment in ICPs is voluntary, and beneficiaries may opt out of these plans if assigned to one, it is often difficult to identify a comparison group of beneficiaries that controls for selection bias. All evaluations of PACE and all but 1 study of FIDE-SNPs and aligned models used observational designs with propensity score weighting, matching, or covariate adjustment to account for observed enrollee characteristics across plan types. However, these designs are susceptible to bias from unmeasured differences between enrollees of ICPs and comparison plans. Some observational studies used longitudinal cohort designs that followed dual-eligible beneficiaries over time. Although longitudinal designs control for enrollee-level factors that remain constant over time, challenges arise if unobserved factors are correlated with outcome trends or mortality.12,37 Several studies used quasi-experimental designs to mitigate selection bias concerns; however, all but 1 of these studies evaluated MMPs. Further research that leverages policy-driven variation in ICP enrollment (eg, default enrollment into integrated plans) or randomized clinical designs could strengthen and broaden the evidence base on ICPs.
Limitations
Other gaps in evidence limit the conclusions of this review. Because studies varied in populations and outcomes evaluated, we were unable to make head-to-head comparisons of the performance of different ICPs. Furthermore, studies provided little or no detail on contextual factors that could have influenced plan performance, such as plans’ care management practices or prior experiences with integrated care. Research assessing these factors and their relationship to outcomes could help policymakers identify and disseminate features of ICPs that may be associated with better care for dual-eligible beneficiaries.
Conclusions
Findings from this systematic review highlight the variability in the association of ICPs with spending, utilization, and outcomes among dual-eligible Medicare beneficiaries, as well as gaps in the available evidence. Some studies associated some ICPs with reductions in long-term nursing home care, and several studies identified greater outpatient care use. However, evidence on spending—specifically on Medicaid—was limited for PACE and FIDE-SNPs, whereas MMPs were generally associated with higher Medicare spending. Evidence was mixed or insufficient to evaluate the association of ICPs with hospitalizations, care coordination, patient satisfaction, health, and outcomes among beneficiary subgroups in vulnerable situations. Research addressing these evidence gaps is urgently needed to guide integration policy for dual-eligible Medicare and Medicaid beneficiaries.
eMethods.
eTable 1. Evaluations Examining Both Medicare and Medicaid Spending
eTable 2. Subgroup Analyses
eTable 3. Data Extracted from Individual Studies
Data Sharing Statement.
References
- 1.Medicaid and CHIP Payment and Access Commission . Chapter 2 Integrating Care for Dually Eligible Beneficiaries. 2023. Accessed June 17, 2024. https://www.macpac.gov/wp-content/uploads/2023/06/Chapter-2-Integrating-Care-for-Dually-Eligible-Beneficiaries.pdf
- 2.Medicare Payment Advisory Commission . Chapter 9 Managed Care Plans for Dual-Eligible Beneficiaries. Accessed June 17, 2024. 2018. https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/jun18_ch9_medpacreport_sec.pdf
- 3.Cassidy B. Delivering Unified Access to Lifesaving Services (DUALS). 2024. Accessed June 17, 2024. https://www.cassidy.senate.gov/wp-content/uploads/2024/03/Duals-Legislation-One-Pager-Final.pdf
- 4.Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank Q. 2007;85(4):579-610. doi: 10.1111/j.1468-0009.2007.00502.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medicare Payment Advisory Commission . Data Book: Beneficiaries Dually Eligible for Medicare and Medicaid. MACPAC. Accessed November 8, 2023. https://www.macpac.gov/publication/data-book-beneficiaries-dually-eligible-for-medicare-and-medicaid-3/
- 6.Velasquez DE, Orav EJ, Figueroa JF. Enrollment and characteristics of dual-eligible Medicare and Medicaid beneficiaries in integrated care programs. Health Aff (Millwood). 2023;42(5):683-692. doi: 10.1377/hlthaff.2022.01321 [DOI] [PubMed] [Google Scholar]
- 7.Unruh MA, Grabowski DC, Trivedi AN, Mor V. Medicaid bed-hold policies and hospitalization of long-stay nursing home residents. Health Serv Res. 2013;48(5):1617-1633. doi: 10.1111/1475-6773.12054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh EG, Clark WD. Managed care and dually eligible beneficiaries: challenges in coordination. Health Care Financ Rev. 2002;24(1):63-82. [PMC free article] [PubMed] [Google Scholar]
- 9.Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. J Am Geriatr Soc. 2012;60(5):821-829. doi: 10.1111/j.1532-5415.2012.03920.x [DOI] [PubMed] [Google Scholar]
- 10.Kasper J, Watts MO, Lyons B. Chronic Disease and Co-Morbidity Among Dual Eligibles: Implications for Patterns of Medicaid and Medicare Service Use and Spending. Kaiser Family Foundation ; 2010. Accessed November 8, 2023. https://www.kff.org/wp-content/uploads/2013/01/8081.pdf
- 11.Frank RG, Epstein AM. Factors associated with high levels of spending for younger dually eligible beneficiaries with mental disorders. Health Aff (Millwood). 2014;33(6):1006-1013. doi: 10.1377/hlthaff.2013.0769 [DOI] [PubMed] [Google Scholar]
- 12.Ghosh A, Schmitz R, Brown R. Effect of PACE on Costs, Nursing Home Admissions, and Mortality: 2006-2011. Accessed June 17, 2024. https://aspe.hhs.gov/reports/effect-pace-costs-nursing-home-admissions-mortality-2006-2011-0
- 13.Cassidy B, Scott T, Cornyn J, Carper TR, Warner MR, Menendez R. Request for Information. Published online November 22, 2022. Accessed June 17, 2024. https://www.cassidy.senate.gov/download/duals-letter
- 14.Medicaid and CHIP Payment and Access Commission . Inventory of Evaluations of Integrated Care Programs for Dually Eligible Beneficiaries. Published October 2022. Accessed March 14, 2024. https://www.macpac.gov/publication/inventory-of-evaluations-of-integrated-care-programs-for-dually-eligible-beneficiaries/
- 15.Medicare Payment Advisory Commission . Chapter 14: Mandated Report: Dual-Eligible Special Needs Plans. MedPAC; 2024. Accessed June 17, 2024. https://www.medpac.gov/document/chapter-15-mandated-report-dual-eligible-special-needs-plan-march-2024-report/
- 16.Smith LB, Waidmann TA, Caswell KJ. Assessment of the Literature on Integrated Care Models for People Dually Enrolled in Medicare and Medicaid. Accessed June 17, 2024. https://www.urban.org/research/publication/assessment-literature-integrated-care-models-people-dually-enrolled-medicare-and-medicaid
- 17.JEN Associates. Massachusetts Senior Care Option 2005-2010 Impact on Enrollees: Nursing Home Entry Utilization August 14, 2013. Accessed June 17, 2024. https://www.mass.gov/doc/masshealth-sco-program-evaluation-nursing-facility-entry-rate-2004-through-2010-enrollment-0/download
- 18.Anderson WL, Long SK, Feng Z. Effects of integrating care for Medicare-Medicaid dually eligible seniors in Minnesota. J Aging Soc Policy. 2020;32(1):31-54. doi: 10.1080/08959420.2018.1485396 [DOI] [PubMed] [Google Scholar]
- 19.Keohane LM, Zhou Z, Stevenson DG. Aligning Medicaid and Medicare Advantage managed care plans for dual-eligible beneficiaries. Med Care Res Rev. 2022;79(2):207-217. doi: 10.1177/10775587211018938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim H, Charlesworth CJ, McConnell KJ, Valentine JB, Grabowski DC. Comparing care for dual-eligibles across coverage models: empirical evidence from Oregon. Med Care Res Rev. 2019;76(5):661-677. doi: 10.1177/1077558717740206 [DOI] [PubMed] [Google Scholar]
- 21.Caswell KJ, Waidmann T, Wei K, Smith LB. Do integrated care models for dual Medicare-Medicaid enrollees work? Evidence from Massachusetts’ one care financial alignment initiative demonstration. Urban Institute. Accessed June 20, 2024. https://www.urban.org/research/publication/do-integrated-care-models-dual-medicare-medicaid-enrollees-work
- 22.Feng Z, Wang J, Gadaska A, et al. Comparing outcomes for dual eligible beneficiaries in integrated care: final report. Published online September 2021. Accessed June 17, 2024. https://aspe.hhs.gov/reports/comparing-outcomes-dual-eligibles
- 23.Allen SM, Piette ER, Mor V. The adverse consequences of unmet need among older persons living in the community: dual-eligible versus Medicare-only beneficiaries. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 1):S51-S58. doi: 10.1093/geronb/gbu124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griffin E, Tyler D, Mulmule N, et al. Financial Alignment Initiative MyCare Ohio: Third Evaluation Report. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-oh-thirdevalrpt
- 25.Holladay S, Stockdale H, Palmer L, et al. Illinois Medicare-Medicaid Alignment Initiative: Third Evaluation Report. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-il-3rd-eval-report
- 26.Chepaitis AE, Hover S, Costilow E, et al. Financial Alignment Initiative Virginia Commonwealth Coordinated Care Evaluation Report; 2021. https://www.cms.gov/priorities/innovation/data-and-reports/2021/fai-va-ccc-eval-report
- 27.Howard JN, Toth M, Costilow E, et al. South Carolina Healthy Connections Prime Third Evaluation Report. Published online December 2023. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-sc-thirdevalrpt
- 28.Gattine E, Snow K, Toth M, et al. Massachusetts One Care Preliminary Fifth Evaluation Report. Published online April 2023. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-ma-5th-eval-report
- 29.Holladay S, Howard J, Toth M, et al. Michigan MI Health Link Second Evaluation Report. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2022/fai-mi-secondevalrpt
- 30.Gattine E, Ciolfi ML, Jiminez F, et al. Rhode Island Integrated Care Initiative: Third Evaluation Report. Published online December 2023. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-ri-thirdevalrpt
- 31.Khatutsky G, Tyler D, Bernacet A, et al. California Cal MediConnect: Preliminary Third Evaluation Report. Published online April 2023. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-ca-3rd-eval-report
- 32.Snow K, Gattine E, Kandilov A, et al. Financial Alignment Initiative New York Fully Integrated Duals Advantage for Individuals with Intellectual and Developmental Disabilities: Preliminary Third Evaluation Report. Published online October 2023. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-ny-fida-idd-prelim-thirdevalrpt
- 33.Griffin E, Hodge S, Palmer L, et al. Texas Dual Eligible Integrated Care Demonstration Preliminary Third Evaluation Report. Published online December 2023. Accessed June 19, 2024. https://www.cms.gov/priorities/innovation/data-and-reports/2023/fai-tx-thirdprelimevalrpt
- 34.Chapin RK, Wendel C, Lee R, et al. Program of All-Inclusive Care for the Elderly (PACE). Medicaid Cost-Benefit Study. Kansas Department for Aging and Disability Services; 2013. Accessed June 19, 2024. https://socwel.ku.edu/sites/socwel/files/documents/CRADO%20Website%20Docs/PACE%20Final%20Report.pdf
- 35.Wieland D, Kinosian B, Stallard E, Boland R. Does Medicaid pay more to a program of all-inclusive care for the elderly (PACE) than for fee-for-service long-term care? J Gerontol A Biol Sci Med Sci. 2013;68(1):47-55. doi: 10.1093/gerona/gls137 [DOI] [PubMed] [Google Scholar]
- 36.Segelman M, Cai X, van Reenen C, Temkin-Greener H. Transitioning from community-based to institutional long-term care: comparing Waiver and PACE enrollees. Gerontologist. 2017;57(2):300-308. doi: 10.1093/geront/gnv106 [DOI] [PubMed] [Google Scholar]
- 37.Roberts ET, Xue L, Lovelace J, et al. Changes in care associated with integrating Medicare and Medicaid for dual-eligible individuals. JAMA Health Forum. 2023;4(12):e234583. doi: 10.1001/jamahealthforum.2023.4583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graham CL, Liu PJ, Hollister BA, Kaye HS, Harrington C. Beneficiaries respond to California’s program to integrate Medicare, Medicaid, and long-term services. Health Aff (Millwood). 2018;37(9):1432-1441. doi: 10.1377/hlthaff.2018.0452 [DOI] [PubMed] [Google Scholar]
- 39.Chen BK, Yang YT, Gajadhar R. Early evidence from South Carolina’s Medicare-Medicaid dual-eligible financial alignment initiative: an observational study to understand who enrolled, and whether the program improved health? BMC Health Serv Res. 2018;18(1):913. doi: 10.1186/s12913-018-3721-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jung HY, Trivedi AN, Grabowski DC, Mor V. Integrated Medicare and Medicaid managed care and rehospitalization of dual eligibles. Am J Manag Care. 2015;21(10):711-717. [PMC free article] [PubMed] [Google Scholar]
- 41.Meyers DJ, Offiaeli K, Trivedi AN, Roberts ET. Medicare and Medicaid dual-eligible special needs plan enrollment and beneficiary-reported experiences with care. JAMA Health Forum. 2023;4(9):e232957. doi: 10.1001/jamahealthforum.2023.2957 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Evaluations Examining Both Medicare and Medicaid Spending
eTable 2. Subgroup Analyses
eTable 3. Data Extracted from Individual Studies
Data Sharing Statement.