Abstract
Introduction
Distal fibula osteoporotic comminuted fractures are challenging to treat and are often treated with periarticular locking plates. This study examined the biomechanical difference between locked plating and dual non-locked one-third tubular plating.
Methods
Using an osteoporotic Sawbones fibula model, simulated fracture were fixated with one-third tubular dual plating and locked periarticular plating. The samples were then torqued to failure and peak torque, stiffness, and displacement were recorded.
Results
The peak torque of the dual plating group was found to be statistically higher than the periarticular locked plating group (0.841 Nm and 0.740 Nm respectively; p = 0.024). However overall stiffness calculated at each 10° increment of displacement was noted to have no significant difference between the two constructs.
Conclusion
Dual non-locked plating of distal fibula osteoporotic comminuted fractures is biomechanically equivalent to locked periarticular plating.
Keywords: Dual plate, Double plate, One-third tubular plate, Distal fibula, Ankle fractures, Lateral locking plate distal fibula, Sawbone, Biomechanics, Osteoporotic
1. Introduction
1.1. Fractures of the distal fibula are common injuries with an incidence of 122–184 cases per 100,000 people/year which accounts for approximately 10 % of orthopedic fractures.1,2
With the current trend of increasing population age and life-expectancy, the incidence of osteoporotic ankle fractures is expected to also increase.3 Fixation of unstable distal fibula ankle fractures in the osteoporotic population has long presented a complex challenge to surgeons. Poor bone quality leads to poor screw purchase, resulting in weak and potentially unstable fixation.4 Many techniques have been proposed to try to overcome this challenge.
1.2. Locking plate technology frequently combined with contoured periarticular plating has seen a rapid rise in recent years because locking plate fixation strength is not dependent on bone mineral density.5,6
Some recent studies have found a biomechanical advantage to locking plate technology in patients with poor bone quality.7,8 This makes it a useful fixation method in osteoporotic fractures. However, locked contoured plates can cost over six times the amount of standard plating systems such as one-third tubular plating with non-locking screws.8, 9, 10 Dual plating has also been proposed in these situations as a lower cost alternative to more expensive locking plate technology.11
1.3. The purpose of this study was to evaluate the biomechanical properties of locking periarticular plates compared with dual plating using non-locking plates in a lateral bridging and posterolateral antiglide fashion in the treatment of osteoporotic comminuted distal fibula fractures
We hypothesize that there will be no difference between locked periarticular plating and dual one-third tubular plating of distal fibula fractures in Ref. 1 peak torque to failure and2 rotational stiffness measured in 10° increments.
2. Methods
2.1. We selected an osteoporotic fibular sawbones model, made with lower density foam to simulate decreased bone density in osteoporosis
This model was selected as it is frequently used in biomechanical studies, and it allows better standardization with decreased variables. We included ten osteoporotic fibula Sawbones models (Vashon, WA) in each construct group given that many other similar studies had at least ten samples per group.7,12, 13, 14, 15 All fibulas were left sided specimens. We used a saw to make a 45° cut starting 3 cm proximal to the anterior distal end of the fibula using an anterior inferior to posterior superior orientation simulating a Weber B fibular fracture. Next, we stabilized the fractures using a dual one-third tubular plate technique versus the lateral locking plate technique but leaving a 2 mm gap at the fracture site to simulate fracture comminution. The simulated fracture comminution neutralizes the stabilizing effect provided by cortical support of the fracture fragments.7,16,17
2.2. For the dual plating technique (Fig. 1) titanium one-third tubular plates were used (stryker Ltd, Kalamazoo, MI, USA)
Fig. 1.

Distal fibula dual plate non-locking construct.
An eight hole one-third tubular plate was secured on the lateral cortex in a bridging fashion with three bicortical non-locking cortical 3.5 mm screws proximally and three unicortical non-locking cortical 3.5 mm screws distally, with the middle two holes at the gapped fracture site remaining empty. The plate was contoured slightly to better fit the bony anatomy. We then applied a posterolateral one-third tubular six hole plate in an antiglide fashion. It was also contoured slightly for optimal placement. The posterior plate was offset so the screw holes did not interfere with the screws from the lateral plate. We then drilled and secured the posterior plate with two bicortical non-locking cortical 3.5 mm screws proximally and two unicortical non-locking cortical 3.5 mm screws distally, with the middle two holes at the gapped fracture site remaining empty.
2.3. The locking plate technique (Fig. 2) used a lateral four hole periarticular locking plate (stryker Ltd, Kalamazoo, MI, USA) in a bridging fashion
Fig. 2.

Distal fibula single locking plate construct.
It was secured with four locking screws distally in unicortical fashion and three non-locking cortical screws proximally in bicortical fashion. We again left the holes immediately adjacent to the gapped fracture site empty.
2.4. We then marked and cut the fibulas in both groups at 12 cm proximally from the distal end
The two ends were then potted in Smooth-Cast (Smooth-On, Inc, Macungie, PA) using a square silicone mold. Mold clay was used to protect the plates and screws from the mold material thereby decreasing the additional stabilization of the mold on the distal fibula piece. The molds were filled to approximately ten mm deep.
2.5. After the molds had dried, we then secured them upright in the instron biomechanical E10000 testing machine (norwood, MA)
A custom device was constructed to secure the distal mold and the proximal mold to the dynamo (Fig. 3). We then applied an external rotation force at 1° per second to the specimen while maintaining neutral unloaded axial force. Data was monitored at 100 Hz. The test was continued until crack propagation was visualized and significant decrease in the torque over time graph was noted.
Fig. 3.
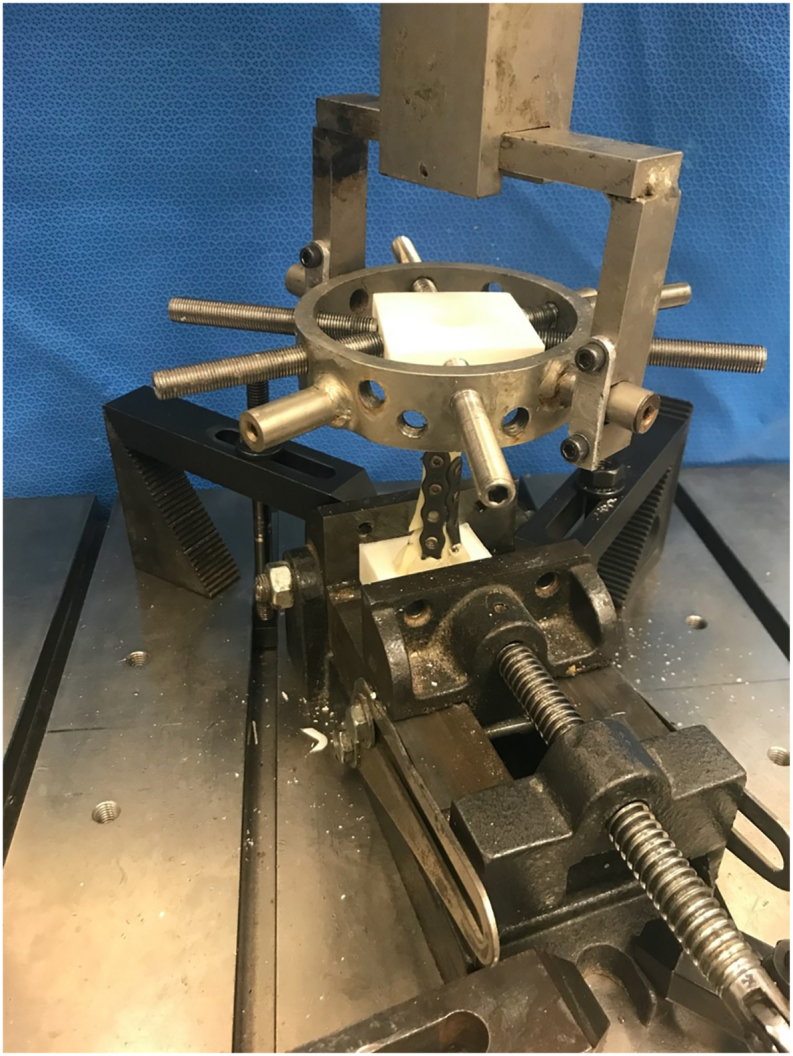
Instron E10000 testing set up.
2.6. We measured peak torque at 10° increments as well as peak torque at failure
We also measured the angle in degrees at each 10° increment and at failure. Evaluation of 10° increments was not continued after 60° because one of the locked plating groups was noted to have a significant decrease in stiffness along with crack propagation after 50°. We also did not continue after 60° because there is little significance at higher angle values as they would represent conditions beyond clinical failure.
2.7. We calculated a power analysis based on estimated mean peak torque of 635 N m (nm) for locked plating, assumed peak torque of 800 nm for dual plating, with standard deviation of 80 nm.7
Given alpha of 0.05 and beta 0.2 for 80 % power, we calculated that we needed at least four samples in each testing construct group.
2.8. Normality of our data was assessed using Kolmogorov-smirnov (KW) and shapiro-wilk (SW) testing
After confirming normal distribution, means were compared using the two-sample t-test at each 10° increment and at failure. Alpha was set at 0.05.
3. Results
3.1. Dual plating produced greater peak torque at failure (0.841 nm ± 0.073 nm) compared to locked plating (0.740 nm ± 0.108 nm, p = 0.024)
However, there was no difference in the amount of displacement at failure (dual plating: 79.7° ± 16.6°, locked plating: 68.0° ± 12.8°, p = 0.094) (Table 1).
Table 1.
Peak torque at failure and max rotation at failure.
| Parameters | Dual Plating | Locked plating | Mean Difference | p-value |
|---|---|---|---|---|
| Peak torque at failure (Nm) | 0.841 ± 0.073 | 0.740 ± 0.108 | 0.101 | a0.024 |
| Degrees at failure (°) | 79.7 ± 16.6 | 68.0 ± 12.8 | 11.7 | 0.094 |
Denotes statistically significant value.
3.2. Below the load to failure, analysis of torque at 10° increments revealed no differences between dual and locked plating
At 10°, torque of dual plating was 0.328 Nm ± 0.038 versus that of locked plating at 0.345 Nm ± 0.053 (mean difference: 0.017 Nm [95 % CI -0.0606 to 0.0259], p = 0.409). At 20°, torque of dual plating was 0.528 Nm ± 0.051 versus that of locked plating at 0.530 Nm ± 0.071 (mean difference: 0.001 Nm [95 % CI -0.0594 to 0.0569], p = 0.964). See Table 2 for all 10° intervals statistics (Table 2).
Table 2.
Stiffness at 10° increments.
| External rotation stiffness (Nm/°) | Dual plating | Locked plating | p-value |
|---|---|---|---|
| 10° | 0.033 ± 0.004 | 0.035 ± 0.005 | 0.409 |
| 20° | 0.026 ± 0.003 | 0.026 ± 0.004 | 0.964 |
| 30° | 0.021 ± 0.002 | 0.021 ± 0.003 | 0.76 |
| 40° | 0.017 ± 0.002 | 0.016 ± 0.002 | 0.458 |
| 50° | 0.014 ± 0.001 | 0.014 ± 0.002 | 0.277 |
| 60° | 0.013 ± 0.001 | 0.012 ± 0.002 | 0.138 |
| At failure | 0.011 ± 0.002 | 0.011 ± 0.003 | 0.687 |
4. Discussion
4.1. Osteoporotic and comminuted distal fibula fractures present a challenge for the orthopedic surgeon
Poor bone quality with osteoporosis and loss of cortical stability with comminution place added importance on the need for construct stability that will allow adherence to the AO orthopedic principles of stable fixation allowing early and safe mobilization of the injured ankle. Increasingly surgeons are choosing to use more expensive locking periarticular technologies to address these situations. We argue that a more cost-effective method to achieve this result can be by using simple non-locking one-third tubular plating systems in a lateral and posterolateral dual plating configuration.
4.2. Our primary aim was to determine if this dual plating treatment model was biomechanically equivalent to locked plating in torsional fatigue to failure testing
Stressing fixation models to failure is well documented as a viable tool to evaluate mechanical strength of various fixation constructs.18, 19, 20, 21, 22 We found that dual plating using conventional one-third tubular plates achieved a greater peak torque than did locked plating for distal fibular fractures in an osteoporotic comminuted fracture model when stressed to failure. This finding was statistically significant. Our secondary aim was to evaluate the stiffness of the two constructs in clinically relevant ranges of strain. In consecutive 10° intervals we found no difference in stiffness between the locked plating and dual plating techniques.
4.3. A recent meta-analysis of lateral plating techniques found there was essentially no difference between lateral locked plating and lateral nonlocked plating unless bone mineral density was taken into account
They noted that the strength of locked plating may be independent of bone mineral density and therefore may have a benefit in osteoporotic fractures.6 This evaluation of locked plating was continued by Switaj et al. when they compared the biomechanical strength of lateral periarticular locked plating with posterolateral one-third tubular plating using non-locking screws. They found that the periarticular lateral locking plate was superior to the nonlocked antiglide plate with a higher torque to failure and construct stiffness.21 The authors were unable to find similar research comparing locked plating to dual conventional plating in the literature. We have found that using conventional plating methods in a 90-90 configuration results in a construct that is biomechanically equivalent to locked contoured plating.
4.4. The advantage of contoured locked plating has been questioned in the literature
Davis et al. found little biomechanical advantage of periarticular plating over one-third tubular lateral plating. They noted that the periarticular plates were rotationally stiffer but there was no difference regarding torque to failure or axial stiffness. They also noted a statistically significant higher torque to failure in the nonlocking group compared to the locking group.23
4.5. Dual plating has been utilized with excellent effect in a number of situations where poor bone quality from osteoporosis and comminution was a concern and with good results.22,23
Double or dual plating has been presented in the literature in the treatment of distal radius, humerus and clavicle fractures.24, 25, 26 Savage et al. described a case of a severely displaced Weber B ankle fracture that was treated successfully with lateral and posterolateral dual plating using one-third tubular plates and non-locking screws. At 20 months postoperatively the patient was doing well without pain or complications.22 Another study retrospectively reviewed 25 patients that were treated with dual fixation of their distal fibular ankle fractures. Overall, the patients did well, and no patients experienced hardware irritation or wound problems necessitating repeat surgery. However, the significance of this finding was reduced due to a loss to follow up of 36 % with average long term follow up of 19.6 months.27 Vance et al. describes a series of 12 patients treated with dual distal fibular fixation. The indications for the second plate in their series were for such problems as diabetic nephropathy, osteopenia due to delayed fracture fixation, osteoporosis, and significant fracture comminution. All patients had uneventful fracture healing. One patient was lost to follow up and one patient had the hardware removed at 15 months due to pain from hardware prominence.11
4.6. An advantage to dual plating fibula fractures with compromised bone quality is the potential cost savings associated with using conventional nonlocked plates over locked contoured plates
One study out of the United Kingdom noted that a one-third tubular plate often used in distal fibula fractures cost on average £104.82 while noting that a locking contoured distal fibular plate cost £673.83, a difference of over six times.8 Costs also differ markedly between locking and conventional screws. Conventional screws have been noted to cost around $20 while locking screws can be five times more expensive.9 Cost savings from avoidance of locking contoured plating techniques in fibula fractures has been estimated at $40–50 million annually in the United States. Vance et al. presents a case series on distal fibula fracture fixation using dual plating methods. They note that the price of hardware is becoming increasingly important in our cost-conscious health care system.11
5. Limitations
5.1. A chief limitation of this study is that we studied a sawbones model rather than a human model
Using saw bones can downplay the dissection necessary for plate placement in a real patient, and it should be noted that a dual plate construct would typically require additional soft tissue stripping with its associated disadvantages compared to a locking plate. However, we feel that an advantage of the Sawbones model is the ability to provide a more standardized testing platform and lower variability throughout testing. Another limitation was the lack of cyclic testing. Bariteau et al. did not appreciate a difference between non-locked one-third tubular plating and locked plating of distal fibula fractures until they instituted a ramped cyclic testing model. Under the cycling testing model, they were able to show some biomechanical increased stiffness in the locked group.7 We were unable to perform cyclic testing due to logistical constraints. However, we still feel our results support the consideration of dual plating in situations where significant poor bone quality is a concern, as clinically substantiated in the literature.11,22,27 This conclusion is strengthened by the findings of Kim et al. They evaluated osteoporotic distal fibula fractures fixed with locking plates versus conventional plates and tested the constructs using cyclic and torque to failure testing. They noted that cycling did not reveal significant effect on fracture stiffness in either plating scenario.28 It should also be noted that given this is a biomechanical study and not in vivo the conclusions may not be significant clinically.
5.2. This topic remains an area of potential future research
Additional high quality clinical studies comparing dual plating to periarticular locked plating would be of interest to the medical community. Additionally, a cost benefit analysis would be of interest given the use of lower cost implants with the dual plating technique versus the potential operative room cost savings with periarticular locked plating if there is a time advantage to periarticular plating.
6. Conclusion
6.1. Our study shows that in an osteoporotic comminuted distal fibula model dual plating with non-locking one-third tubular plates has greater peak torque at failure than more expensive locked peri-articular plating methods
The two constructs are equivalent in terms of stiffness in consecutive 10° increments of external rotation. Further study is warranted to evaluate the clinical outcomes of this technique compared to locked plating.
Declaration of interest
There were no conflicts of interest by any authors involved in the study.
Funding
This research did not receive any specific grant from funding agencies in the public or commercial sectors.
CRediT authorship contribution statement
Scott Epperly: Conceptualization, Methodology, data collection, Writing – original draft. Allen Nedley: Data collection, Writing – original draft. Jun Ho Chung: Data collection, Writing – review & editing. Evelyn Rodrigues: Writing – review & editing. Joseph Johnson: Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Elisabeth Clarke, Loma Linda Orthopaedics Research Coordinator.
References
- 1.Moriarity A., Ellanti P., Mohan K., Fhoghlu C.N., Fenelon C., McKenna J. A comparison of complication rates between locking and non-locking plates in distal fibular fractures. J Orthop Traumatol: Surgery & Research. 2018;104(4):503–506. doi: 10.1016/j.otsr.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 2.El Fatayri B., Bulaïd Y., Djebara A.-E., Havet E., Mertl P., Massinissa D. A comparison of bone union and complication rates between locking and non-locking plates in distal fibular fracture: retrospective study of 106 cases. Injury. 2019;50(12):2324–2331. doi: 10.1016/j.injury.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Davis A.T., Israel H., Cannada L.K., Bledsoe J.G. A biomechanical comparison of one-third tubular plates versus periarticular plates for fixation of osteoporotic distal fibula fractures. J Orthop Trauma. 2013;27(9):e201–e207. doi: 10.1097/BOT.0b013e318281a565. [DOI] [PubMed] [Google Scholar]
- 4.McKean J., Cuellar D.O., Hak D., Mauffrey C. Osteoporotic ankle fractures: an approach to operative management. Orthopedics. 2013;36(12):936–940. doi: 10.3928/01477447-20131120-07. [DOI] [PubMed] [Google Scholar]
- 5.Zahn R.K., Frey S., Jakubietz R.G., et al. A contoured locking plate for distal fibular fractures in osteoporotic bone: a biomechanical cadaver study. Injury. 2012;43(6):718–725. doi: 10.1016/j.injury.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Dingemans S.A., Lodeizen O.A., Goslings J.C., Schepers T. Reinforced fixation of distal fibula fractures in elderly patients; A meta-analysis of biomechanical studies. Clin Biomech. 2016 Jul;36:14–20. doi: 10.1016/j.clinbiomech.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Bariteau J.T., Fantry A., Blankenhorn B., Lareau C., Paller D., Digiovanni C.W. A biomechanical evaluation of locked plating for distal fibula fractures in an osteoporotic sawbone model. Foot Ankle Surg. 2014 Mar;20(1):44–47. doi: 10.1016/j.fas.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Lyle S.A., Malik C., Oddy M.J. Comparison of locking versus nonlocking plates for distal fibula fractures. J Foot Ankle Surg. 2018 Jul-Aug;57(4):664–667. doi: 10.1053/j.jfas.2017.11.035. [DOI] [PubMed] [Google Scholar]
- 9.Moss L.K., Kim-Orden M.H., Ravinsky R., Hoshino C.M., Zinar D.M., Gold S.M. Implant failure rates and cost analysis of contoured locking versus conventional plate fixation of distal fibula fractures. Orthopedics. 2017 Nov 1;40(6):e1024–e1029. doi: 10.3928/01477447-20171012-05. [DOI] [PubMed] [Google Scholar]
- 10.Chang G., Bhat S.B., Raikin S.M., et al. Economic analysis of anatomic plating versus tubular plating for the treatment of fibula fractures. Orthopedics. 2018 Mar 1;41(2):e252–e256. doi: 10.3928/01477447-20180213-01. [DOI] [PubMed] [Google Scholar]
- 11.Vance D.D., Vosseller J.T. Double plating of distal fibula fractures. Foot Ankle Spec. 2017 Dec;10(6):543–546. doi: 10.1177/1938640017692416. [DOI] [PubMed] [Google Scholar]
- 12.Misaghi A., Doan J., Bastrom T., Pennock A.T. Biomechanical evaluation of plate versus lag screw only fixation of distal fibula fractures. J Foot Ankle Surg. 2015 Sep-Oct;54(5):896–899. doi: 10.1053/j.jfas.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Manoharan G., Singh R., Kuiper J.H., Nokes L.D.M. Distal fibula oblique fracture fixation using one-third tubular plate with and without lag screw - a biomechanical study of stability. J Orthop. 2018 Jun;15(2):549–552. doi: 10.1016/j.jor.2018.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hallbauer J., Klos K., Rausch S., et al. Biomechanical comparison of a lateral polyaxial locking plate with a posterolateral polyaxial locking plate applied to the distal fibula. Foot Ankle Surg. 2014 Sep;20(3):180–185. doi: 10.1016/j.fas.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Eckel T.T., Glisson R.R., Anand P., Parekh S.G. Biomechanical comparison of 4 different lateral plate constructs for distal fibula fractures. Foot Ankle Int. 2013 Nov;34(11):1588–1595. doi: 10.1177/1071100713496223. [DOI] [PubMed] [Google Scholar]
- 16.White N.J., Corr D.T., Wagg J.P., Lorincz C., Buckley R.E. Locked plate fixation of the comminuted distal fibula: a biomechanical study. Can J Surg. 2013;56(1):35. doi: 10.1503/cjs.012311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koval K.J., Petraco D.M., Kummer F.J., Bharam S. A new technique for complex fibula fracture fixation in the elderly: a clinical and biomechanical evaluation. J Orthop Trauma. 1997 Jan;11(1):28–33. doi: 10.1097/00005131-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Nguyentat A., Camisa W., Patel S., Lagaay P. A biomechanical comparison of locking versus conventional plate fixation for distal fibula fractures in trimalleolar ankle injuries. J Foot Ankle Surg. 2016 Jan-Feb;55(1):132–135. doi: 10.1053/j.jfas.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 19.Schaffer J.J., Manoli A., 2nd The antiglide plate for distal fibular fixation. A biomechanical comparison with fixation with a lateral plate. J Bone Joint Surg Am. 1987 Apr;69(4):596–604. [PubMed] [Google Scholar]
- 20.Minihane K.P., Lee C., Ahn C., Zhang L.Q., Merk B.R. Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma. 2006 Sep;20(8):562–566. doi: 10.1097/01.bot.0000245684.96775.82. [DOI] [PubMed] [Google Scholar]
- 21.Switaj P.J., Wetzel R.J., Jain N.P., et al. Comparison of modern locked plating and antiglide plating for fixation of osteoporotic distal fibular fractures. Foot Ankle Surg. 2016 Sep;22(3):158–163. doi: 10.1016/j.fas.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 22.Savage T.J., Stone P.A., McGarry J.J. Internal fixation of distal fibula fractures: a case presentation demonstrating a unique technique for a severely comminuted fibula. J Foot Ankle Surg. 1995 Nov-Dec;34(6):587–592. doi: 10.1016/S1067-2516(09)80084-7. ; discussion 96. [DOI] [PubMed] [Google Scholar]
- 23.Bevan W.P., Barei D.P., Nork S.E. Operative fixation of osteoporotic ankle fractures. Tech Foot Ankle Surg. 2006;5(4):222–229. [Google Scholar]
- 24.Rikli D.A., Businger A., Babst R. Dorsal double-plate fixation of the distal radius. Eur J Trauma Emerg Surg. 2007 Feb;33(1):99–109. doi: 10.1007/s00068-007-9155-1. [DOI] [PubMed] [Google Scholar]
- 25.Laux C.J., Grubhofer F., Werner C.M.L., Simmen H.P., Osterhoff G. Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res. 2017 Sep 25;12(1):137. doi: 10.1186/s13018-017-0639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaipel M., Majewski M., Regazzoni P. Double-plate fixation in lateral clavicle fractures-a new strategy. J Trauma. 2010 Oct;69(4):896–900. doi: 10.1097/TA.0b013e3181bedf28. [DOI] [PubMed] [Google Scholar]
- 27.Kwaadu K.Y., Fleming J.J., Lin D. Management of complex fibular fractures: double plating of fibular fractures. J Foot Ankle Surg. 2015 May-Jun;54(3):288–294. doi: 10.1053/j.jfas.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 28.Kim T., Ayturk U.M., Haskell A., Miclau T., Puttlitz C.M. Fixation of osteoporotic distal fibula fractures: a biomechanical comparison of locking versus conventional plates. J Foot Ankle Surg. 2007 Jan-Feb;46(1):2–6. doi: 10.1053/j.jfas.2006.09.009. [DOI] [PubMed] [Google Scholar]


