Abstract
Background
Epstein-Barr virus (EBV) is a common human Herpesvirus with worldwide distribution. Primary EBV infection usually occurs early in life and typically presents as infectious mononucleosis consisting of fever, pharyngitis, hepatosplenomegaly, and lymphadenopathy. Usually, the disease course is benign and most patients recover uneventfully without any consequent sequel.
Method and results
We present a case of an immunologically normal young male in whom an acute EBV infection caused severe pneumonitis. He was treated empirically with Paracetamol, intravenous Ceftriaxone 1 gr/day plus Azithromycin 500 mg/day.
Conclusion
EBV-associated pneumonitis is rare, and treatment is usually supportive, whether antiviral agents (such as acyclovir) or steroids would be beneficial remains to be determined.
Keywords: EBV, Pneumonia, Lung, Computed tomography scan
1. Introduction
Epstein-Barr virus (EBV) is a common worldwide herpesvirus that affects mainly humans occurring usually early in life and typically presents as infectious mononucleosis (fever, pharyngitis, hepatosplenomegaly, and lymphadenopathy). The usual course of the disease is benign and most patients recover uneventfully without any consequent sequel. Severe forms of infections are reported mainly in immunocompromised patients. About 5–10 % of cases of infectious mononucleosis present with mild, asymptomatic pneumonitis, however, a severe form of pneumonitis is sporadic, especially in immunocompetent individuals [1]. Here we present a case of an immunocompetent young male in whom an acute EBV infection led to admission to our hospital with severe pneumonitis.
2. Case report
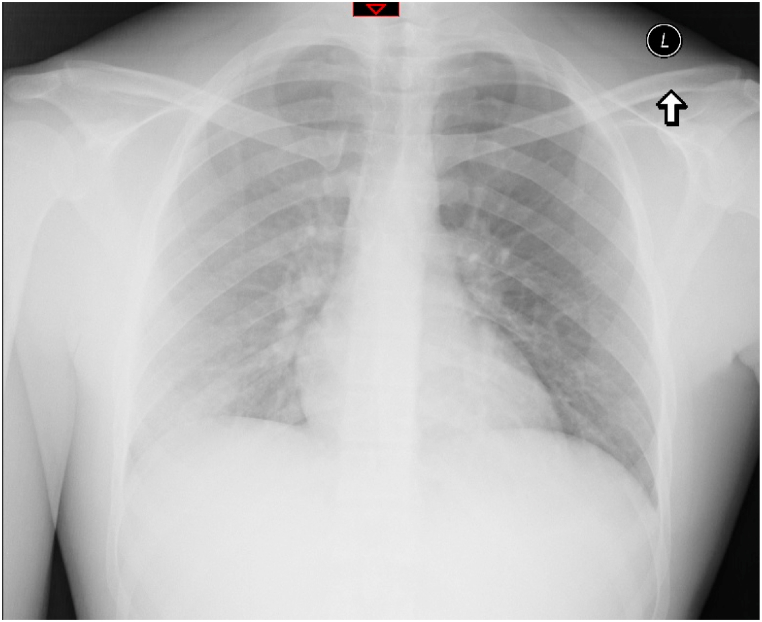
A 21-year-old previously healthy male was admitted to our emergency department complaining of shortness of breath, chest pain, hemoptysis, and fever with chills, all of which started four days before his admission. The patient stated that before his admission he was completely healthy, did not have any background co-morbidities, and was not taking any drugs whatsoever. Additionally, he mentioned that he returned from Turkey two months before his admission, and had not had any close contact or exposure to animals, or occupational hazardous substances. Upon arrival at the emergency department, his vital signs were as follows: Temperature 38.2 °C, blood pressure 112/60, pulse 111, respiratory rate 18 breaths per minute without hypoxemia. On physical examination he was alert but in marked discomfort. On auscultation to the lungs, reduced breath sounds in the right lung with bronchial breathing were noticed. Also, right upper quadrant tenderness was noticed with hepatosplenomegaly during the abdominal examination, the Murphy sign was negative. During palpation of the lymph nodes, we observed an enlarged and swelled right axillary lymph node about 3 cm in diameter. A chest radiograph (Fig. 1) was performed on admission and demonstrated a right lower lobe infiltrate, in keeping with the diagnosis of pneumonia. Initial blood analyses revealed elevated leucocytes with lymphocytosis consisting 66 % of the total white blood cells, atypical lymphocytes were observed on a direct blood smear, microcytic anemia with 11.50 g/dl Hemoglobin, elevated levels of C-reactive protein and slightly elevated liver enzymes, including GOT, GPT, Alkaline phosphates, GGT, LDH, and INR. Blood gases were within normal range. Since pulmonary embolism was a very unlikely diagnosis in this setting, we meant to exclude it by drawing another blood sample to test the levels of D-Dimer, surprisingly; its level was elevated at 1658 NG/mL.
Fig. 1.
Chest radiograph of the patient on admission, demonstrating a right lower lobe infiltrate.
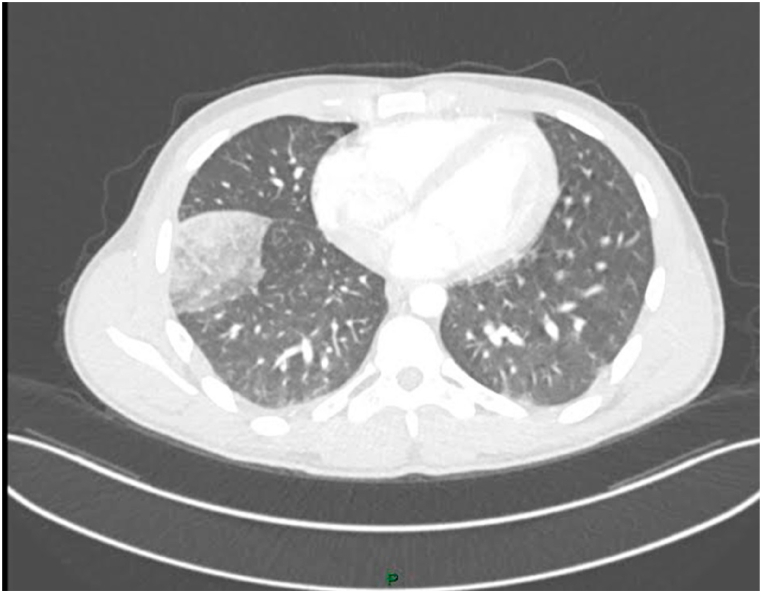
A chest Computed tomography pulmonary angiogram (CTPA) (Fig. 2) was performed and revealed confined opacity in the right lower lobe, pulmonary embolism was ruled out. Blood cultures were negative. PCR tests for the sputum for the following pathogens: Covid-19, Streptococcus pneumoniae, Haemophilus influenza, Mycoplasma pneumonia, Mycobacterium tuberculosis, Bordetella pertussis, Chlamydia pneumonia and Legionella pneumophila were all negative. The patient was treated with Paracetamol, intravenous Ceftriaxone 1 gr/day plus Azithromycin 500 mg/day for broad-spectrum antibiotics coverage. During hospitalization, the patient kept complaining of right upper quadrant abdominal pain and blood levels of liver enzymes were also rising, therefore, an abdominal Ultrasonography was performed which revealed hepatosplenomegaly with no other pathological finding (Fig. 3). Finally, additional blood tests for HIV and Hepatitis viruses were performed (including tests for CMV and EBV) which were conclusive with recent EBV infection with the following results: EBV-VCA IgM-B was positive 18.37 S/CO; EBNA IgG was negative, in consisting with the diagnosis of acute EBV pneumonitis was confirmed. HIV and CMV were ruled out. On day 4 of his admission, the fever subsided and the patient felt well. He was discharged home the day after in good condition; he was invited to our clinic for a follow-up 10 days after his discharge. The patient was feeling well, and had no fever, blood analysis demonstrated a marked decline in Leukocyte count, C-reactive protein, and liver enzymes in comparison to his admission. He was discharged with a recommendation for a repeat low-dose chest tomography scan in one month and later follow-up in our clinic thereafter, unfortunately, he did not show up for his routine checkup with no information regarding whether or not a repeat chest CT scan was performed.
Fig. 2.
Chest computed tomography pulmonary angiogram (CTPA) revealing confined opacity in the right lower lobe.
Fig. 3.
Abdomianl ultrasonography demonstrating splenomegaly.
3. Discussion
EBV infection disease course usually presents with fever, lymphadenopathy, pharyngitis, hepatosplenomegaly, and atypical lymphocytosis on blood examination. Yet, most infections are asymptomatic. The spectrum of disease is extremely variable and different manifestations can occur [2]. Lung involvement, on the other hand, has been rarely reported as the presenting manifestation of an acute EBV infection [[3], [4], [5]], especially in immunocompetent individuals [6]. This case is very uncommon in that the only manifestation on admission was pneumonia. EBV infection was suspected because of the atypical presentation and the finding of pronounced lymphocytosis and atypical lymphocytes in the blood smear. Serology remains the gold standard for the diagnosis of EBV-induced pneumonia [1], and the diagnosis was confirmed by the combination of positive serology and ruling out other possible infections that might have caused similar disease, especially since some patients with pneumonia and serologic evidence of current EBV infection also showed some other known respiratory pathogens (e.g. Mycoplasma pneumonia, adenovirus, etc) [1,7]. Our patient had negative PCR tests for these variant respiratory pathogens; therefore, it is confirmatory that the patient had recent EBV infection-associated pneumonitis. Our patient had anemia during hospitalization, we assume that the mechanism was hemolytic anemia induced by EBV by the production of heterophil antibodies, unfortunately, since our patient has not been in our clinic later on for follow-up, we cannot be sure about the preciseness of this assumption. The treatment approach for EBV-associated pneumonitis is mainly supportive, whether antiviral agents similar to Acyclovir or steroids would be beneficial remains to be determined and should be separately considered by each case of its own [1].
CRediT authorship contribution statement
Jawad Hindy: Conceptualization, Investigation, Methodology, Resources. Tova Rainis: Supervision, Validation.
Declaration of competing interest
No conflict.
Handling Editor: DR AC Amit Chopra
Contributor Information
Jawad Hindy, Email: jawad.hindy@b-zion.org.il.
Tova Rainis, Email: tova.rainis@b-zion.org.il.
References
- 1.Schooley R.T. In: Principles and Practice of Infectious Diseases. fifth ed. Mandell G.L., Bennet J.E., Dolin R., editors. Churchill Livingston; New York: 2000. Epstein-Bar virus (infectious mononucleosis) pp. 1599–1613. [Google Scholar]
- 2.American Academy of Pediatrics . 1997 Red Book: Report of the Committee on Infectious Diseases. 24th ed. 1997. pp. 199–200. [Google Scholar]
- 3.Lander P., Palayew M.J. Infectious mononucleosis: a review of chest roentgenographic manifestations. J. Can. Assoc. Radiol. 1974;25:303–306. [PubMed] [Google Scholar]
- 4.McCort J.J. Infectious mononucleosis with special reference to roentgenologic manifestations. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1949;62:645–654. [PubMed] [Google Scholar]
- 5.Arendt J. The roentgenological aspect of infectious mononucleosis. AJR 195;64:950-958. [PubMed]
- 6.Veal C., Carr M., Briggs Jr. D. Diffuse pneumonia and acute respiratory failure due to infectious mononucleosis in a milddle-aged adult. Am. Rev. Respir. Dis. 1990;141:502–504. doi: 10.1164/ajrccm/141.2.502. [DOI] [PubMed] [Google Scholar]
- 7.Weinstein M., O'Hare B. Hemoptysis and Epstein-Barr virus infection. Pediatr. Infect. Dis. J. 2000;8:760–761. doi: 10.1097/00006454-200008000-00019. [DOI] [PubMed] [Google Scholar]