If the American Medical Student Association has anything to do with it, relations between doctors and the pharmaceutical industry will soon look considerably different. Representing 30 000 students, interns, and residents throughout the United States, the association is running a campaign—PharmFree—calling for an end to gift giving, free lunches, sponsored education, and paid speaking.1
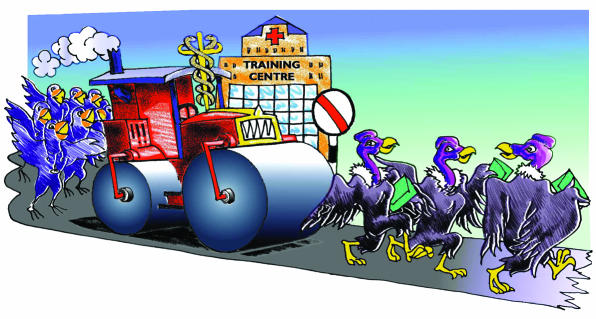
Figure 1.
SUE SHARPLES
Students are being urged to sign a PharmFree pledge to seek out unbiased sources of healthcare information and to take a recently revised Hippocratic oath, called a “model oath for the new physician,” which includes the commitments: “I will make medical decisions... free from the influence of advertising or promotion. I will not accept money, gifts, or hospitality that will create a conflict of interest in my education, practice, teaching, or research.”
The strange becomes familiar
The American Medical Student Association's campaign is inspired in part by the work of the New York based No Free Lunch, which boasts the motto “Just say no to drug reps,” hosts a pen amnesty,2 and, together with an Australian group called Healthy Skepticism, is urging doctors to turn away from industry backed education and information, towards independent materials.3 According to No Free Lunch, “Our quarrel is not with the pharmaceutical industry but with pharmaceutical industry promotion. The time has come to eliminate its influence from our practices.” These small campaigns are indications of a fundamental redefinition of the relationships between doctors and drug companies, as professional associations, standard setting bodies, and individual institutions around the world begin to disentangle some of the unhealthy flows of money and influence (box).
Moves towards disentanglement
Restrictions or prohibitions on drug representatives visiting doctors
Restrictions or prohibitions on educational events funded by industry
Prohibitions on individuals or organisations with conflicts of interest running accredited continuing medical education
Moves towards independently funded continuing medical education and reliance on independent sources of information
Campaigns to end acceptance of all gifts and trips
Campaigns to end acceptance of honorariums for speaking at educational conferences
Professional bodies reducing reliance on drug company sponsorship
Professional associations' prohibitions on researchers with conflicts of interest conducting research
Medical journals reducing reliance on advertising revenue and sponsored supplements
Calls to set up “blind trusts” at an institutional level to independently handle outside funding
Introduction into guidelines of the “rebuttable presumption” that researchers with conflicts of interest cannot do research using human subjects
Calls for new national bodies to conduct research driven by public interest
Calls for regulatory and advisory committee members to avoid conflicts of interest
Summary points
Medical reform groups and student associations are calling for disentanglement from pharmaceutical companies and independent education and sources of information
The University of California in San Francisco is considering plans to end free lunches sponsored by drug companies and to remove drug representatives
Professional associations and standard setting bodies are moving towards more distance in relations with industry
Industry defends the value of its educational sponsorship to patients and rejects the idea of a trend towards disentanglement
The old standard of disclosure has been supplemented with a growing demand for more distance in the relationships. According to the newly revised guidelines of the Association of American Medical Colleges on the financial interests of medical researchers, “Transparency, though necessary to sustain public confidence in academic research, is not sufficient to protect human subjects.”4 These guidelines, designed to help reshape the rules on more than 100 campuses throughout North America, have introduced a new presumption: “an individual who holds a significant financial interest in research involving human subjects may not conduct such research,” except where circumstances are compelling and the presumption can be successfully rebutted.
At the University of California in San Francisco (UCSF), a special committee convened by the dean of the medical school has just recommended an end to free lunches for doctors and a move away from direct company sponsorship of educational events. At the same time, the chief executive officer of the university's Medical Center—a complex with a turnover of $800m (£500m; €700m) a year and one million patient visits— wants to severely restrict representatives of drug companies having access to prescribing doctors and may remove representatives from the hospital system entirely. The university is not at the forefront of such reform, but size and prestige guarantee that their sea change in doctor-drug company relationships has a global audience.
Relationships with clinicians
“It's a reawakening within the academic world that we have to make sure our relationships are more appropriate,” says the dean of the UCSF's medical school and former university chancellor, Haile Debas. “Relationships with industry are critical, but they need redefining.” The report that Debas commissioned in 2002 has just recommended an end to free lunches sponsored by companies and an end to the direct sponsorship of all educational events on campus. Exactly how such new rules might work in practice, or whether indirect sponsorship will replace existing money flows, is not yet clear. Debas is confident though that a change in the relationship is coming: “I think there will be more distance.”
The chairman of the reporting committee, vice dean for academic affairs, Neal Cohen, says the movement for change is like a “steamroller” driven by many forces in the university, medical establishment, and wider community. An intensive care specialist, Cohen, like many established doctors, has been the beneficiary of entanglement with industry; he has fond memories of a paid visit to the antipodes. “Once I took a trip to Australia funded by a drug company, to talk about an anaesthetic.” Would he do it again now? “No. I'd like to go back to Australia, but I'll pay for it myself. I believe I gave objective advice, but it would be hard to convince someone else that my junket to Australia was not tainted. Now, I would think much more carefully about my relationship with industry. The concerns about conflicts of interest are much more at the top of my mind than they were 10 or 15 years ago.”
Across the road from the medical school is the administration of the university's medical centre, where chief executive officer Mark Laret works from his fifth floor office overlooking the Golden Gate park and the bridge beyond. “In some ways we are all addicts to big pharma's money,” he says, referring to the generous funding of free lunches and important educational events at the university, “but we are going to have to wean ourselves off a dependency that is generally inappropriate. This relationship is one of those things we need to clean up. The sooner the better.”
Like Haile Debas, Laret has become particularly concerned about the uncontrolled access the representatives of drug companies have to doctors, and in some cases to patients. Earlier this year Laret discussed with the dean of the school of pharmacy the possibility of developing educational materials for hospital doctors that could effectively “supplement or even supplant” those distributed by drug company representatives. He'd been shocked during discussions with resident doctors, still in training, about the extent to which many of them relied on the representatives of drug companies for their information about drugs. “I think this has to change. Patients want to be sure that the decisions their physicians are making are not unduly influenced by pharmaceutical company marketing.”
It is clear from conversations with many senior figures at UCSF that there is a plan taking shape to ultimately “kick out the reps,” but Laret says he won't prejudge where the current process is going. Given that representatives and their one to one visits account for a large part of the pharmaceutical industry's annual $19bn promotional budget in the United States, it is unlikely that drug companies will cede an influential campus like the UCSF without a fight. Asked whether his plans may ultimately stall, Laret says, “We're talking about a culture change in the organisation. It's a matter of when, not if.”
Laret, a professional hospital administrator, has thought a lot about the importance of relationships between doctors and drug companies, having sat on the special Association of American Medical Colleges taskforce that produced the new national guidelines. “The last thing we want to do is stifle creativity. The commercialisation of science is good for human beings,” he says. “We must not see big pharma as an enemy; it is a valued partner. But finding the right terms of that relationship is the real challenge.”
This theme is echoed by Cohen: “The real ethical dilemma is not about the free lunch, it's about keeping the opportunity for new developments, which require close relationships so new products match clinical need. The question is how to nurture those relationships without compromising the credibility of researchers.”
Relationships with researchers
The latest Association of American Medical Colleges guidelines—which feature the new presumption that a significant conflict of interest can disqualify a researcher from conducting research—offer some guidance to those academic institutions seeking to redefine their relationships with sponsors, but it is too early to see how they are being put into practice. Other guidance has come from the industry group Pharmaceutical Research and Manufacturers of America, which is currently promulgating a new set of principles for the relationships. Adopted last year, their principles state that “sponsors will not hire investigators to conduct clinical trials who have proprietary interests in the compound being studied,” though they contain no prohibition on the myriad other forms of financial ties between sponsors and researchers.5 Responding to rising public alarm about cases in which unflattering results have been suppressed—including a notorious example at UCSF in which data about a thyroid drug from a sponsored trial were buried for seven years—the new industry principles urge companies to report all findings from sponsored trials, even if they are unfavourable.6
As a member of the committee that reviews and manages the financial ties between academics at UCSF and their industry sponsors, associate professor Mary-Margaret Chren welcomes the current moves towards putting more distance into the relationships. “Disclosure is a highly limited tool for dealing with conflicts of interest,” she says, making an argument that medicine should move into line with other professions. “Our system would never tolerate judges taking money from those they judge, yet for some reason this doesn't apply in medicine, and doctors feel they should have complete freedom with no protection from potentially compromising relationships.”
Chren, a dermatologist attached to the San Francisco Veterans Affairs Medical Center, published an article almost a decade ago suggesting that an “independent not for profit institutional intermediary should be responsible for all interactions between physician scientists and companies.”7 Although ignored in 1994, Chren's idea may become more salient now if the current tentative moves towards disentanglement continue.
The Accreditation Council for Continuing Medical Education, the body that sets standards for continuing medical education throughout the United States, has just issued new draft guidelines stating that researchers or teachers with financial ties to drug companies or other sponsors may have conflicts of interest and would thus “be excluded from the roles of planning committee member, manager, teacher, and author” in relation to continuing medical education.8 The draft's preamble makes clear that it is proposing a big break with the past: “Now a conflict of interest will exclude a person or firm from controlling the content of CME. We recognise this is a major change.” The draft has provoked strong reactions from professional associations, who argue important educational activities would not take place without drug company support.
“Nonsense,” says Drummond Rennie, a deputy editor with JAMA and a professor of medicine at UCSF. “That argument presupposes that some of the most well off in our society can't afford to pay for their lunches, their education, or their conference. But guess what, all sorts of poorer people pay every step of the way. No one is handing out money to them. When I hear doctors crying poverty... and an inability to pay for their education, I feel ashamed of my profession because these are self evident lies.”
John Kelly, senior vice president of science and regulatory affairs at Pharmaceutical Research and Manufacturers of America, says his industry does not support the draft rules for continuing medical education, and in a recent interview he was confident that they would not be implemented. Kelly argues strongly that sponsored continuing medical education is in the interest of patients because it facilitates doctors' access to the “best available information,” but he would not be drawn on the question of why sponsored continuing medical education was in the interests of its sponsors. On the broader question of the nascent moves towards disentanglement, Kelly had this comment: “Be careful not to overinterpret either what's happening at a single institution or a single draft set of guidelines or see that as a trend. It is not a trend.” Certainly the draft report from UCSF's academic senate's task force on conflicts of interest, which is canvassing a loosening of the rules and potentially closer entanglement, would lend support to Kelly's assertion (see part 1 of this article).
Asked about the PharmFree campaign being mounted by the American Medical Student Association, Kelly said that unlike students, organisations representing practising doctors continue to acknowledge the important role of companies in underwriting educational activities. Yet some professional groups have already started to undo their financial dependency on pharmaceutical companies. The Society of General Internal Medicine introduced a policy last year limiting pharmaceutical company funding to 10% of the organisation's total annual budget, with no single company funding more than 5%. After implementation of the new rules, sponsorship of the society's annual conference by drug companies fell by more than $100 000 (almost 70%).
The president of the society and a professor at the University of California in Los Angeles, Martin Shapiro, says the changes were precipitated by a particular instance of sponsored research, against the backdrop of growing concern about the closeness between professional associations and their sponsors. “You just walk through the rooms of some other professional meetings and medical conferences and it just stinks with pharmaceutical propaganda and paraphernalia. And it's not enough to walk through those rooms and hold your nose—the company money is already in your pocket through the subsidy of your conference fees or association membership.”
Moves towards disentanglement
Behind the receptionists in the busy foyer of UCSF's medical centre a sign reads, “Our mission is caring, healing, teaching and discovering.” Much of that discovering is now run by drug companies, working in relationships with doctors, developing promising and profitable new therapies. The challenge for those who run hospitals, academic institutions, and health systems as a whole is to facilitate the best of those relationships of discovery, without letting the resulting flows of goodwill, money, and influence fundamentally distort the caring, healing, and teaching dimensions of the medical mission.
Developing new pharmaceuticals and promoting them are two very different pursuits, and increased scrutiny of the industry, driven largely by accelerating drug expenditure, will only make clearer where the boundaries between those different activities lie. Many individual doctors, and their professional associations, are facing difficult choices about whether they remain part of the industry's extended promotional machinery or should seek real distance in their relationships, to give prescribing, teaching, and advice that is truly independent. Growing moves towards genuine separation may well make previously acceptable conflicts of interest untenable.
In March 2003, in a room just around the corner from the dean of UCSF's office, a large group of first and second-year medical students were tucking into pizzas, hot dogs, and the ubiquitous burgers. Although a prime spot for some company networking with the next generation of prescribers, not a drug representative or logo were in sight. Confused, I found the organisers who told me this free lunch was paid for by the university and, like the line from the T shirt, was most definitely “not sponsored.”
I thank Alan Cassels, drug policy researcher at the University of Victoria, Canada, for thoughtful comments.
Competing interests: None declared.
References
- 1.American Medical Students Association. PharmFree campaign. AMSA, 2002. www.amsa.org/prof/pharmfree.cfm www.amsa.org/prof/pharmfree.cfm (accessed 8 May 2003).
- 2.No Free Lunch. http://nofreelunch.org/ (accessed 8 May 2003).
- 3.Healthy Skepticism. www.healthyskepticism.org (accessed 8 May 2003).
- 4.Task Force on financial conflicts of interest in clinical research. Protecting subjects, preserving trust, promoting progress. Association of American Medical Colleges, 2001: 9. www.aamc.org/members/coitf/start.htm (accessed 28 Apr 2003).
- 5.Pharmaceutical Research and Manufacturers of America. Principles on conduct of clinical trials and communication of clinical trial results. Washington, DC: PhRMA, 2002 www.phrma.org/publications/quickfacts/20.06.2002.428.cfm (accessed 8 May 2003).
- 6.Rennie D. Thyroid storm. JAMA 1997;277: 1238-43. [PubMed] [Google Scholar]
- 7.Chren M. Independent investigators and for-profit companies. Arch Dermatol 1994;130: 432-7. [PubMed] [Google Scholar]
- 8.Accreditation Council for Continuing Medical Education Standards to ensure the separation of promotion from education within the CME activities of ACCME accredited providers. Chicago: ACCME, 2003. www.accme.org/incoming/SCS_Draft_Jan_2003.pdf (accessed 8 May 2003).