Abstract
Objective
Pigmented fungiform papillae of the tongue (PFPT) are infrequently encountered and inadequately documented pigmented lesions that pose challenges in diagnosis and subsequent treatment planning. The study was aimed at analyzing dentists' knowledge and attitudes regarding PFPT morphologies, to determine diagnosis and subsequent treatment planning.
Methods
A cross-sectional study was conducted among dentists in East Java through an online questionnaire. Four clinical photographs of PFPT were presented, accompanied by seven questions assessing dentists' knowledge of PFPT, including lesion types, tongue structure involvement, Holzwanger classification, lesion patterns, suspected diagnoses and the nature of the lesion (benign or malignant). Additional questions to evaluate attitudes included prior experience with PFPT in practice, potential malignant transformation, diagnostic investigation and required treatment. Knowledge-associated attitude differences were statistically analyzed with the Mann–Whitney test with a threshold of p < 0.05.
Result
A total of 117 dentists participated, most of whom were women (69.23%) and were 26–30 years of age (44.44%). Dentists 41–50 years of age had superior knowledge to those 20–30 years of age (p = 0.005). Practitioners with 1–5 years of experience showed significant differences in knowledge regarding PFPT (p < 0.05). No significant differences in knowledge level and attitudes were observed, particularly regarding PFPT treatment and supporting investigation (p > 0.05). However, prior encounters with PFPT cases were significantly associated with treatment decisions and supporting investigations for diagnosis (p < 0.05).
Conclusion
Most participating dentists had substantial knowledge of PFPT cases. Dentists' understanding, as reflected in their attitudes toward investigating and treating PFPT, was notably influenced by prior encounters with PFPT cases.
Keywords: Attitude, Dentist, Knowledge, Malignant, PFPT, Tongue
الملخص
أهداف البحث
تمثل الحليمات الكمئية الملونة في اللسان آفة مصبوغة نادرة التواجد وغير موثقة بشكل كاف في الدراسات المنشورة، مما يشكل تحديات في التشخيص وخطط العلاج اللاحقة. تهدف الدراسة إلى تحليل معرفة وفهم وموقف أطباء الأسنان تجاه أشكال الحليمات الكمئية الملونة في اللسان لتحديد التشخيص وخطط العلاج اللاحقة.
طرق البحث
أجريت دراسة مقطعية بين أطباء الأسنان في جاوة الشرقية باستخدام استبانة عبر الإنترنت. تم تقديم أربع صور سريرية للحليمات الكمئية الملونة في اللسان، مع سبعة أسئلة لتقييم معرفة أطباء الأسنان بها، بما في ذلك نوع الآفة، وهياكل اللسان المتضمنة، وتصنيف هولزوانقر، ونمط الآفة، والتشخيص المشتبه به، وطبيعة الآفة (حميدة أو خبيثة). تضمنت أسئلة إضافية تجارب مع الآفة في الممارسة، والتحول المحتمل إلى الورم الخبيث، والتحقيقات التشخيصية، والعلاج المطلوب لتقييم المواقف. تم تحليل الفروقات في المواقف المرتبطة بالمعرفة إحصائيا باستخدام اختبار مان-ويتني.
النتائج
شارك ما مجموعه 117 طبيب أسنان، وكانت الغالبية من الإناث (69.23%) ومن الفئة العمرية 26-30 سنة (44.44%). أظهر أطباء الأسنان الذين تتراوح أعمارهم بين 41-50 عاما معرفة متفوقة مقارنة بأولئك الذين تتراوح أعمارهم بين 20-30 عاما. أظهر الممارسون الذين لديهم 1-5 سنوات من الخبرة فروقات كبيرة في المعرفة حول هذه الحالة. لم يلاحظ تباين كبير بين مستوى المعرفة والموقف، خاصة فيما يتعلق بالعلاج والتحقيق الداعم. ومع ذلك، كان لمواجهة حالات الحليمات الكمئية الملونة تأثير كبير على قرارات العلاج والتحقيقات الداعمة.
الاستنتاجات
يمتلك معظم أطباء الأسنان المشاركين مستوى جيد من المعرفة حول حالات الحليمات الكمئية الملونة. تتأثر معرفة أطباء الأسنان، كما يتضح من مواقفهم تجاه التحقيق والعلاج، بشكل ملحوظ بتجاربهم مع هذه الحالات.
الكلمات المفتاحية: طبيب أسنان, الحليمات الكمئية الملونة, معرفة, موقف, خبيث, لسان
Introduction
The oral cavity may present diverse variations including both normal variants and pseudo lesions that emulate pathological conditions. Unlike pathological lesions, normal variants are frequently encountered during routine examinations, and display clinical and morphological features that are similar to pathological variants, but do not require surgical or pharmacological interventions.1 Among normal tongue lesions, median rhomboid glossitis, geographic tongue, hairy tongue, fissured tongue, lingual varices, prominent papilla circumvallate and ankyloglossia are frequently encountered. However, a rare lesion called pigmented fungiform papillae of the tongue (PFPT) may notably be present.2
First documented by Leonard in 1905, PFPT manifests morphologically as a blackish-brown pigmentation lesion within fungiform papillae that typically evolves from childhood to young adulthood.3 PFPT has a prevalence ranging from 1% to 3%, and exhibits higher incidence among individuals with dark skin, particularly Black women.4 The lesion is prone to widespread development on the dorsum, lateral to the anterior region of the tongue, thus posing esthetic concerns during speech.5 Despite its clinical significance, PFPT remains inadequately reported and described in the literature, and thus often poses diagnostic dilemmas for dentists, and impede precise diagnostic investigations and treatment planning.2
Accurate diagnosis of PFPT requires extensive knowledge and clinical understanding.6 Core components in the clinical diagnosis of any oral disorder include comprehensive anamnesis and complete clinical examination, particularly tissue morphology. Whereas PFPT predominantly affects individuals with dark skin, some cases are found in people with light skin, including Asians,7,8 particularly in regions such as Indonesia.9 PFPT is considered a normal variant of the mucosa, characterized by its inert growth and lack of need for treatment.2 PFPT may be distributed extensively across the dorsum, lateral and anterior regions of the tongue,5 thereby potentially interfering with speech aesthetics and precipitating a condition known as cancer phobia.2
Inadequate knowledge among clinicians may lead to diagnostic errors, such as misdiagnosis and overdiagnosis. This study was aimed at analyzing dentists' knowledge and attitudes regarding PFPT, reflecting their understanding when encountering this condition, as well as their ability to decide on investigations to determine the correct diagnosis and proper treatment plans.
Materials and Methods
Study design and population
This descriptive research used a cross-sectional study design. The study population comprised dentists in East Java Province in 2020. The questionnaire was administered online via a Google form. The Indonesian Dental Association helped distribute questionnaires to registered member dentists in East Java regions.
Sample size and power analysis
The sample size was calculated with the Lemeshow formula.10 The number of registered dentists in East Java was 3978. The proportion value was specified to be 0.5 with an absolute error value of 0.1. The minimum number of dentists required was calculated to be 41.
Power analysis was conducted in G∗power software.11 The effect size (f) was determined to be 0.25, the α error probability was 0.05, and the total sample size was 117. From the analysis, it obtained that, the power analysis was 0.89.
Clinical photographs of PFPT
Clinical photographs of PFPT were selected on the basis of the criteria of one dentist and two consultant oral medicine specialists. The requirements for clinical photographs were as follows: (a) pigmentation lesions limited only to fungiform papilla type; (b) pigmentation lesions with a cobblestone pattern or rose-petal appearance observed in photographic analysis; and (c) no other lesions, such as depapilation, ulceration, erosion, fissure, plaques or nodules found on the anterior, lateral and dorsum surfaces of the tongue. Among the clinical photographs presented to dentists, cases 1 and 2 were type 1 PFPT, whereas cases 3 and 4 were type 2 PFPT.
Standardized questionnaire
The research questionnaire consisted of four clinical photographs of PFPT. Each image consisted of seven questions assessing dentists' knowledge of PFPT morphologies, including lesion type, involvement of the tongue structure, Holzwanger classification, lesion pattern, suspected diagnosis and nature of the lesion (benign or malignant).
The dentists' attitudes regarding PFPT were assessed through four questions pertaining to the experiences of encountering PFPT during practice, potential malignant transformation, diagnostic procedures and necessary treatment.
Questionnaire validity and reliability
Validity and reliability tests were conducted after trials of 58 dentists. The validity test used Pearson's product–moment correlation through calculation of the correlation between question item scores; the instrument was considered valid if p < 0.05. Reliability tests were performed with the Cronbach alpha coefficient. The instrument was considered reliable if Cronbach's alpha exceeded the calculated R-value (r = 0.2586).12 Cronbach's alpha for each question in case 1, case 2, case 3 and case 4 for was 0.341, 0.502, 0.612 and 0.630, respectively.
Questionnaire interpretation
Each correct answer was given a score of 1, whereas incorrect answers were given a score of 0. The data were tabulated and presented as percentages. Knowledge and attitudes were classified into four categories according to the total number of correct answers as follows: low (<25%), moderate (26–50%), good (51–75%) and excellent (>75%).13
Data analysis
The data are presented as distributions and frequencies. The differences in demographic characteristics (ages and time in practice), knowledge and attitudes were analyzed with one-way ANOVA and Tukey's HSD post hoc test, and a p value <0.05 was considered significant (IBM SPSS Statistics 24 for mac, New York, NY, USA).
Results
Dentists' demographic data
A total of 117 dentists participated in this research (response rate 2.9%). Most participants were women (69.23%) and were 26–30 years of age (44.44%). Most had been in practice 1–5 years (65.81%) (Table 1).
Table 1.
Dentists' characteristics.
| Number (%) | |
|---|---|
| Gender | |
| Male | 36 (30.77%) |
| Female | 81 (69.23%) |
| Age (years) | |
| 20–25 | 27 (23.08%) |
| 26–30 | 52 (44.44%) |
| 31–35 | 17 (14.53%) |
| 36–40 | 8 (6.84%) |
| 41–45 | 5 (4.27%) |
| 46–50 | 3 (2.56%) |
| 51–55 | 1 (0.85%) |
| 56–60 | 4 (3.42%) |
| Time in practice (years) | |
| 1–5 | 77 (65.81%) |
| 6–10 | 22 (18.80%) |
| 11–15 | 7 (5.98%) |
| 16–20 | 5 (4.27%) |
| >20 | 6 (5.13%) |
Knowledge of PFPT
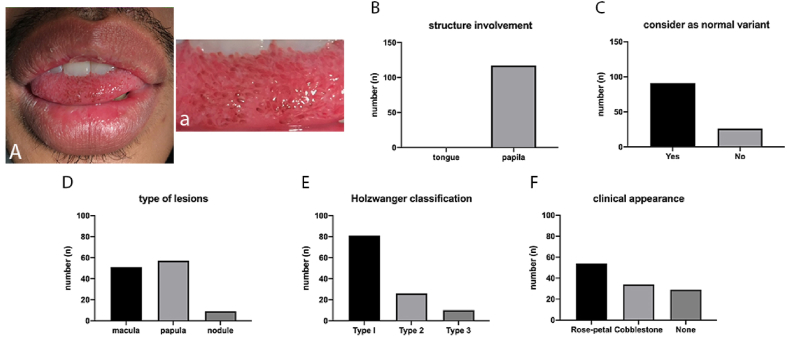
Case 1
Most dentists rated lesions in the anterior region of the tongue as papules (48.72%) involving the structure of the papillae of the tongue (100%). Most dentists stated that case 1 was type 1 in Holzwanger classification (69.23%), and the lesion pattern had a rose-petal appearance (45.30%) and represented normal variation of the oral mucosa (77.78%) (Figure 1).
Figure 1.
The clinical picture of case 1 (A and a); responses related to structure involvement (B), normal variant (C); type of lesions (D); Holzwanger classification (E) and lesion pattern (F).
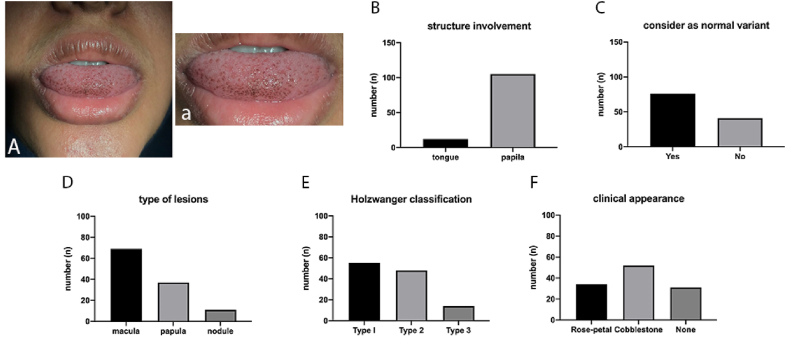
Case 2
The lesion in the anterior region of the tongue was assessed by most dentists as a macular lesion (58.97%) involving the tongue's papillae (74%). Most dentists stated that case 2 was type 1 in Holzwanger classification (47.01%), and the lesion pattern had a cobblestone appearance (44.44%) and represented normal variation of the oral mucosa (64.96%) (Figure 2).
Figure 2.
The clinical picture of case 2 (A and a); responses related to structure involvement (B), normal variant (C); type of lesions (D); Holzwanger classification (E) and lesion pattern (F).
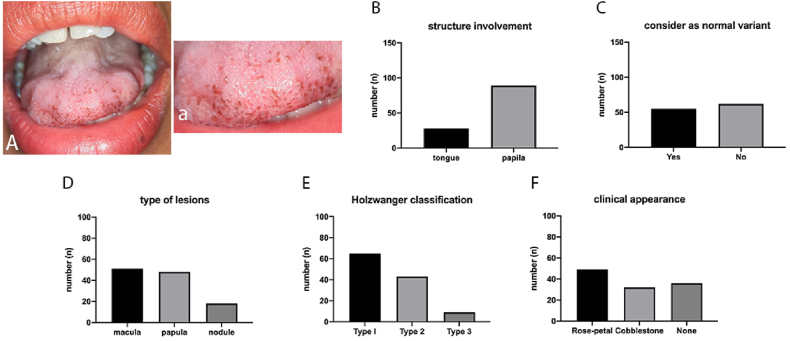
Case 3
Lesions in the anterior region of the tongue were rated as lesions of the macula (43.59%) involving papillae (76.07%). Most dentists stated that case 3 was type 1 in Holzwanger classification (55.56%), and the lesion pattern had a rose-petal appearance (41.88%) and represented normal variation of the oral cavity (52.99%) (Figure 3).
Figure 3.
The clinical picture of case 3 (A and a); responses related to structure involvement (B), normal variant (C); type of lesions (D); Holzwanger classification (E) and lesion pattern (F).
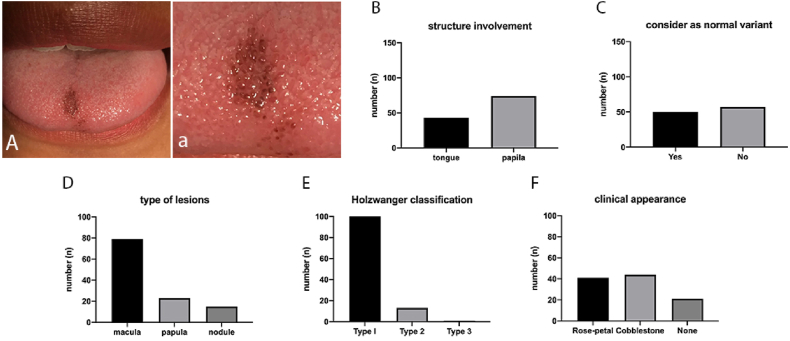
Case 4
The lesion on the anterior tongue was rated as a macular lesion (67.52%) involving the papillae of the tongue (63.25%). Most dentists stated that case 4 was type 1 in Holzwanger classification (88.03%), and the lesion pattern had a cobblestone appearance (47.01%) and represented normal variation of the oral cavity (51.28%) (Figure 4).
Figure 4.
The clinical picture of case 4s (A and a); responses related to structure involvement (B), normal variant (C); type of lesions (D); Holzwanger classification (E) and lesion pattern (F).
Knowledge of PFPT diagnosis
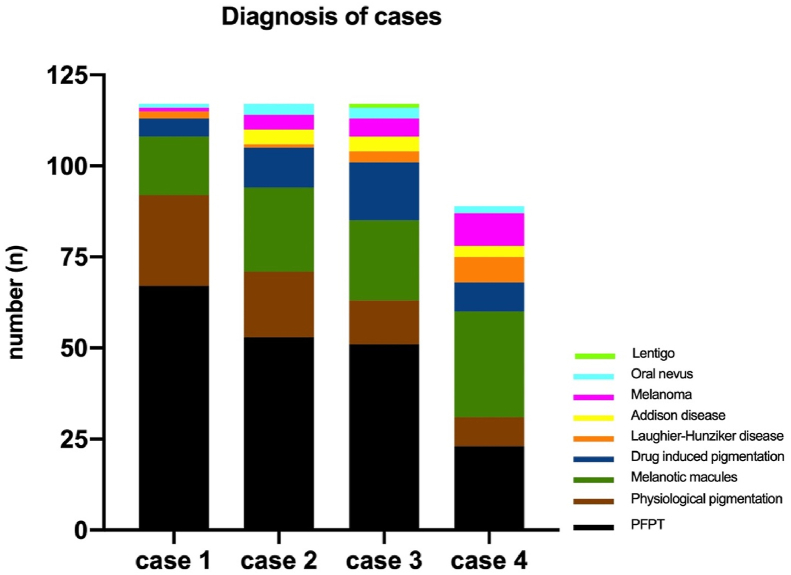
A total of 57.26% dentists determined that the clinical diagnosis in case 1 was PFPT. In contrast, 42.74% diagnosed physiological pigmentation, melanotic macula, pigmentation due to drugs, Laugier–Hunziker disease, melanoma or oral nevus (Figure 5).
Figure 5.
Dentists' responses related to the possible diagnosis of each case.
For case 2, 45.30% of dentists determined that the clinical diagnosis was PFPT, whereas 54.70% diagnosed melanotic macula, physiological pigmentation, pigmentation due to drugs, Addison disease, melanoma, oral nevus or Laugier–Hunziker disease. For case 3, 43.53% of dentists determined a clinical diagnosis of PFPT. For case 4, melanotic macula (24.79%) and oral nevus (24.79%) were the primarily diagnoses, whereas PFPF represented only 19.66% (Figure 5).
Most dentists had good (61.54%) knowledge of PFPT, whereas 32.48% had moderate knowledge, 5.13% had excellent knowledge, and 0.85% had low knowledge. Excellent knowledge was observed primarily among dentists 20–30 years of age (4.27%) in practice for 1–5 years (5.13%). Good knowledge predominated among dentists 20–30 years of age (46.15%) in practice for 1–5 years (44.44%) (Tables 2 and 3).
Table 2.
Knowledge of PFPT distribution by dentists' ages.
| Age (years) | Knowledge of PFPT |
|||
|---|---|---|---|---|
| Excellent | Good | Moderate | Low | |
| 20–30 | 5 (4.27%) | 54 (46.15%) | 20 (17.09%) | 0 |
| 31–40 | 1 (0.85%) | 14 (11.97%) | 9 (7.69%) | 1 (0.85%) |
| 41–50 | 0 | 2 (1.17%) | 6 (5.13%) | 0 |
| 51–60 | 0 | 2 (1.17%) | 3 (2.56%) | 0 |
| Total | 6 (5.13%) | 74 (61.54%) | 36 (32.48%) | 1 (0.85%) |
Table 3.
Knowledge of PFPT distribution by dentists' time in practice.
| Age (years) | Knowledge of PFPT |
|||
|---|---|---|---|---|
| Excellent | Good | Moderate | Low | |
| 1–5 | 6 (5.13%) | 52 (44.44%) | 18 (15.38%) | 1 (0.85%) |
| 6–10 | 0 | 14 (11.97%) | 8 (6.84%) | 0 |
| 11–15 | 0 | 3 (2.56%) | 4 (3.42%) | 0 |
| 16–20 | 0 | 1 (0.85%) | 4 (3.42%) | 0 |
| >20 | 0 | 2 (1.71%) | 4 (3.42%) | 0 |
| Total | 6 (5.13%) | 74 (61.54%) | 36 (32.48%) | 1 (0.85%) |
Knowledge of PFPT significantly differed between the groups 20–30 versus 41–50 years of age (p = 0.005). In contrast, the other group (31–40 and 51–60 years of age) showed a similar level of knowledge associated with PFPT (p > 0.05).
Significant differences in knowledge of PFPT were observed among groups with times in practice of 1–5 years versus 16–20 years and >20 years (p = 0.013 and p = 0.035, respectively). In comparison, the other group (6–10 and 11–15 years) showed a similar level of knowledge associated with PFPT (p > 0.05).
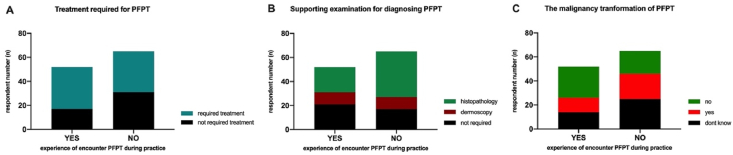
Attitudes regarding PFPT
During practice, only 44.44% of dentists had encountered PFPT, whereas 55.56% had never encountered PFPT. A total of 67.31% of the dentists who had encountered PFPT stated that this condition did not require treatment. Moreover, 52.31% of dentists who had never encountered PFPT also stated that this condition did not require treatment (Figure 6A). A total of 55.56% of dentists stated that PFPT did not require supporting investigations to establish a diagnosis. Meanwhile, 40.38% of dentists who had encountered PFPT stated that histopathological examination was necessary, and 40.38% of dentist who had encounter PFPT stated that supporting investigations were not required (Figure 6B).
Figure 6.
Responses regarding experience in encountering PFPT during practice and the treatment required (A); supporting investigations for diagnosis (B) and possible malignancy transformation of PFPT (C).
A total of 50.00% of dentists who had encountered PFPT cases stated that this condition cannot develop into a malignancy. In contrast, 38.46% of dentists who had never encountered PFPT stated that they did not know whether this condition could develop into malignancy (Figure 6C). There is no significant differences between the level of knowledges and the decision of treatment for PFPT, as well as in determining the supporting investigation (p = 0.101 and p = 0.737, respectively). Prior experience with PFPT was associated with the recommended treatment and supporting investigations (p = 0.045 and p = 0.000, respectively).
Discussion
PFPT presents as brown-black hyperpigmentation on the fungiform papillae.14 Although this condition is most commonly observed in individuals with dark skin, particularly those with Black ancestry, emerging reports indicate its occurrence among individuals with various ancestries, including Chinese.7,8 In Indonesia, the first cases were reported in 2020, in a 22-year-old man and a 21-year-old Javanese woman.9 PFPT can manifest widely on the dorsum, lateral to the anterior of the tongue, and esthetic concerns may arise when the lesions become prominent.5 Given its potential esthetic effects,2 dentists must be knowledgeable regarding this condition.
Although we expected, on the basis of overall demographic data, that the dentists would readily recognize the morphologies and identify PFPT, including its type, Holzwanger classification and lesion pattern, this study revealed unexpected differences in responses. The dentists had varied interpretations of the lesion type, Holzwanger classification and lesion pattern.
Understanding lesion type, including the morphology and structures involved, is essential for recognizing abnormalities within the oral mucosa. All presented cases were characterized by brown-black hyperpigmentation of the fungiform papillae in the anterior and/or dorsum area of the tongue. However, not all dentists identified hyperpigmentation occurring solely in the fungiform papillae, and some suggested involvement of the tongue muscle. Discrepancies were also observed in characterization of the lesion as a papule, macula or nodule. PFPT is sometimes considered a papular lesion. A case presentation by Adibi and Bouquot states that PFPT in women 44 years of age is considered papular.15
The dentists' interpretations of Holzwanger's classification, which categorizes PFPT according to the location and number of hyperpigmented papillae,16 showed divergence. The case presentations were categorized into types 1 (case 1 and case 2) and type 2 (case 3 and case 4). Type 1 is a pigmentation occurring only in the anterior region of the tongue, whereas type 2 occurs in the fungiform papillae in the tongue's dorsum.16 The dentists often misclassified cases; these imprecise predictions were attributed to insufficient knowledge.
PFPT exhibits distinct characteristics that differentiate it from other oral pigmentation lesions. Dermoscopy provides 10× magnification and clearly indicates the papillae's structure and specific pigmentation patterns17 such as a cobblestone18 or rose-petal19 appearance. Despite its potential for improving diagnostic accuracy, dermoscopy remains underused in oral pigmentation evaluations.20 Dentists did not precisely recognize lesion patterns, partly because of the limited use of dermoscopy. Each pattern, called a dermoscope, corresponds to histological features; therefore, dermoscopy can improve diagnostic accuracy. Moreover, dermoscopy substantially avoids unnecessary biopsy procedures for histopathological examination, thus increasing the sensitivity and specificity of the clinical examination. In cases of oral mucosa pigmentation, dermoscopy is rarely used to establish the diagnosis.21
Although most dentists demonstrated good knowledge of lesion types, Holzwanger classification and lesion patterns, less than 60% of dentists accurately diagnosed PFPT in the presented cases. Variations in clinical presentation led to erroneous diagnoses such as melanotic macula, oral nevus or melanoma. Three cases, case 1, case 2 and case 3, had similar clinical presentations involving brown-black hyperpigmentation macular lesions with clear boundaries appearing as dots scattered on the anterior part of the tongue. In contrast, case 4 showed clear differences, in which the brownish macular lesion was localized and had a fairly wide diameter with a clear boundary on the anterior part of the tongue. The large diameter of the lesion and the localized picture resulted in 80.34% of dentists making incorrect clinical diagnoses of melanotic macula, oral nevus or melanoma, all of which are usually large and localized. Notably, practitioners who had encountered PFPT during their practice were more likely to recognize the condition and opt for a no-treatment approach.
Experience with PFPT cases during practice significantly influenced dentists' attitudes toward treatment plans and supporting investigations. Dentists with no prior encounters tended to opt for histopathological examinations, whereas those experienced with PFPT tended to avoid additional investigations. This finding was supported by reports that PFPT does not require treatment because this condition is a normal variation.19,22, 23, 24 Such deviations from established practice underscore the influence of individual experiences on diagnostic and treatment decisions.
Although various reports have advocated for PFPT's benign nature and discouraged unnecessary treatments, a substantial proportion of dentists, particularly those lacking direct experience with PFPT, expressed a tendency toward overdiagnosis and a preference for histopathological examination. According to prior reports, PFPT can be diagnosed without histopathological examination.3,5,9,14,17,22,23,25, 26, 27, 28, 29, 30, 31, 32 The rarity of use of dermoscopy, despite its potential benefits, further contributes to diagnostic uncertainties. Low knowledge affects dentists' attitudes in determining the necessary diagnostic investigation and may lead to overdiagnosis, which is both costly and time-consuming for patients.
No reference has clearly delineated the supporting proceduresthat should be performed to establish a PFPT diagnosis. Of the 20 reported cases of PFPT, six received dermoscopy and histopathological examinations, seven received dermoscopy investigations, and nine received histopathological examinations to establish the diagnosis. Of the 13 cases that underwent dermoscopy investigation of PFPT, cobblestone appearance patterns were found in four cases, whereas a rose-petal appearance was found in nine cases. Fifteen cases undergoing histopathological examinations showed non-specific histopathological features of PFPT, including melanocytes containing brown melanin15,33; keratinocytes containing melanin34; melanophages in the lamina propria,35, 36, 37, 38, 39 sub-epithelial or sub-mucosal tissue,40 connective tissue,41 lymphocytic infiltrate,42 or chromatophores16; and dilated vascular spaces,42 all of which are common histological features of benign mucosal hyperpigmentation. Histopathological examination should be considered if the lesion develops, and other pigmentation is present in the skin.
Concerns regarding the potential malignancy of PFPT were evident, and the dentists had varying opinions on malignant transformation. Conflicting views persist, and some studies have suggested associations with concomitant conditions such as obesity,43 iron deficiency,40 Laugier–Hunziker syndrome44 and Addison disease.45 However, no conclusive evidence supports PFPT's propensity to evolve into malignancy24
PFPT is a normal variant condition that typically does not require treatment unless the lesion is widespread and aesthetically disturbing, thereby necessitating surgical and esthetic interventions. Dermatological examinations with dermatoscopy provide a non-invasive alternative to biopsy and histopathological examinations, particularly in children. Continuous education for dental professionals is imperative to reinforce understanding of the benign nature of PFPT and emphasize the avoidance of unnecessary invasive investigations in managing this condition.
Conclusion
Most participating dentists had substantial knowledge of PFPT cases. Dentists' understanding, as reflected in their attitudes toward investigating and treating PFPT, was notably influenced by their prior encounters with PFPT cases.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The ethical committee approved the design of this study in Research and Health, Faculty of Dental Medicine Universitas Airlangga (registration number 469/HRECC.FODM/X/2020; approved October 9, 2020).
Authors contributions
MDCS conceptualization, formal analysis, investigation, methodology, writing—original draft; IBPM formal analysis, investigation; MAC validation, writing—review and editing; ABRS writing—review and editing; DR supervision, validation; NH supervision, validation; NFA supervision, validation; AEP conceptualization, methodology, supervision, validation, writing—review and editing; DSE conceptualization, methodology, supervision, validation, writing—review and editing. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
The author thanks to Indonesian Dentist Association (Surabaya Region) and Dinas Kesehatan Provinsi Jawa Timur for their support.
Data availability statement
The data are available on request to Meircurius-2015@fkg.unair.ac.id (MDCS).
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work, the author used chatopenai for language checking. After using this tool, the author reviewed and edited the content as needed, and takes full responsibility for the content of the publication.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Vella F. della, Lauritano D., Lajolo C., Lucchese A., Di Stasio D., Contaldo M., et al. The pseudolesions of the oral mucosa: differential diagnosis and related systemic conditions. Appl Sci. 2019;9(12):2412. [Google Scholar]
- 2.Mukamal L.V., Ormiga P., Ramos-e-silva M. Dermoscopy of the pigmented fungiform papillae of the tongue. J Dermatol. 2012;39(April 2011):397–399. doi: 10.1111/j.1346-8138.2011.01328.x. [DOI] [PubMed] [Google Scholar]
- 3.Smogorzewski J.M., Armstrong P., Young L. Pigmented fungiform papillae of the tongue in an Indian male. Cutis. 2019;103(3):E16–E17. [PubMed] [Google Scholar]
- 4.Marcoval-Caus J. Response to: “pigmented fungiform papillae of the tongue in Laugier disease (or Laugier-Hunziker syndrome)”. Actas Dermo Sifiliogr. 2013;104(2):174. doi: 10.1016/j.ad.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Aqil N., Bennani M., Nassiri A., Meziane M., Gallouj S., Mernissi F.Z. Pigmented fungiform papillae of the tongue: clinical and dermoscopic features. Our Dermatol Online. 2019;10(2):213–214. [Google Scholar]
- 6.Mallikarjuna K., Gupta S., Shukla S., Chaurasia S. Unusual extensive physiologic melanin pigmentation of the oral cavity: a clinical presentation. J Indian Soc Pedod Prev Dent. 2013;31(2):121–125. doi: 10.4103/0970-4388.115718. [DOI] [PubMed] [Google Scholar]
- 7.Scarff C.E., Marks R. Pigmented fungiform papillae of the tongue in an Indian male. Australas J Dermatol. 2003;44:149–151. doi: 10.1046/j.1440-0960.2003.00664.x. [DOI] [PubMed] [Google Scholar]
- 8.Tan C., Liu Y., Min Z.S., Zhu W.Y. A clinical analysis of 58 Chinese cases of pigmented fungiform papillae of the tongue. J Eur Acad Dermatol Venereol. 2012;28(2):242–245. doi: 10.1111/j.1468-3083.2012.04684.x. [DOI] [PubMed] [Google Scholar]
- 9.Surboyo M.D.C., Ernawati D.S., Parmadiati A.E., Marsetyo R.I. Pigmented fungiform papillae of the tongue and lingual fimbriae as single presentation in adult: a case report and literature review. Eur J Dent [Internet]. 2020 Sep 9;14(4):702–706. doi: 10.1055/s-0040-1714041. http://www.thieme-connect.de/DOI/DOI?10.1055/s-0040-1714041 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pourhoseingholi M.A., Vahedi M., Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14–17. [PMC free article] [PubMed] [Google Scholar]
- 11.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G∗Power 3.1: tests for correlation and regression analyses. Behav Res Methods [Internet]. 2009 Nov;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. http://link.springer.com/10.3758/BRM.41.4.1149 Available from: [DOI] [PubMed] [Google Scholar]
- 12.Taber K.S. The use of Cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48(6):1273–1296. [Google Scholar]
- 13.Bhattacharya P.T., Sinha R., Pal S. Prevalence and subjective knowledge of tongue lesions in an Indian population. J Oral Biol Craniofac Res. 2016;6(2):124–128. doi: 10.1016/j.jobcr.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El Anzi O. Pigmented fungiform papillae of the tongue: Moroccan case. Our Dermatol Online. 2019;10(2):215–216. [Google Scholar]
- 15.Adibi S., Bouquot J.E. Papillary tip melanosis (pigmented fungiform lingual papillae) Tex Dent J. 2011;128(6):573–574. [PubMed] [Google Scholar]
- 16.Holzwanger J.M., Rudolph R.I., Heaton C.L. Pigmented fungiform papillae of the tongue: a common variant of oral pigmentation. Int J Dermatol. 1974;13:403–408. doi: 10.1111/j.1365-4362.1974.tb05073.x. [DOI] [PubMed] [Google Scholar]
- 17.Alzahrani N., Alharithy R. Pigmented fungiform papillae of the tongue in a Saudi woman. J Dermatol Dermatol Surg. 2018;22(1):39. [Google Scholar]
- 18.Chessa M.A., Patrizi A., Sechi A., Virdi A., Leuzzo M., Neri I. Pigmented fungiform lingual papillae: dermoscopic and clinical features. J Eur Acad Dermatol Venereol. 2018;32(6):935–939. doi: 10.1111/jdv.14809. [DOI] [PubMed] [Google Scholar]
- 19.Surboyo M.D.C., Santosh A.B.R., Hariyani N., Ernawati D.S., Cecilia P.H. Clinical utility of dermoscopy on diagnosing pigmented papillary fungiform papillae of the tongue: a systematic review. J Oral Biol Craniofac Res [Internet]. 2021 Oct 1;11(4):618–623. doi: 10.1016/j.jobcr.2021.09.008. https://linkinghub.elsevier.com/retrieve/pii/S2212426821000968 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jha A.K., Pathak J. Using a chalazion clamp to enhance dermoscopy of oral mucosal lesions. J Am Acad Dermatol. 2017;76(3):e91–e92. doi: 10.1016/j.jaad.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 21.Mordoh A., Casas G., Horacio C., Werner L., Aguas S.C., Lanfranchi H., et al. Dermoscopic evaluation improves clinical diagnosis of oral melanotic macules: a study in 50 patients with oral pigmented lesions. Am J Oral Med. 2018;4(1):1–9. [Google Scholar]
- 22.Radomska A., Sławińska M., Sobjanek M. Pigmented fungiform papillae of the tongue. Dermatol Rev Prz Dermatol [Internet]. 2021;108(3):191–193. doi: 10.5114/dr.2021.108613. Available from: [DOI] [Google Scholar]
- 23.Ross C.L., Ring C., Yang S. Pigmented fungiform papillae of the tongue. JAMA Dermatol [Internet]. 2020 Nov 1;156(11):1249. doi: 10.1001/jamadermatol.2020.2985. https://jamanetwork.com/journals/jamadermatology/fullarticle/2770558 Available from: [DOI] [PubMed] [Google Scholar]
- 24.Surboyo M.D.C., Samaranayake L., Santosh A.B.R., Ayuningtyas N.F., Wati S.M., Rahayu R.P., et al. Pigmented fungiform papillae (PFP) of the tongue: a systematic review of current aetiopathogenesis and pathophysiology. Pathophysiology [Internet]. 2022 Sep 9;29(3):555–569. doi: 10.3390/pathophysiology29030043. https://www.mdpi.com/1873-149X/29/3/43 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neri I., Evangelista V., Veronesi G., Guglielmo A., Chessa M.A. Oral pigmentation in children: a diagnostic challenge. Arch Dis Child. 2021;106(9):895. doi: 10.1136/archdischild-2020-320455. [DOI] [PubMed] [Google Scholar]
- 26.Sil A., Panigrahi A., Bhanja D.B. Tongue discoloration in a young girl. J Pediatr. 2020 Apr;219:276–277. doi: 10.1016/j.jpeds.2019.12.032. [DOI] [PubMed] [Google Scholar]
- 27.Kavak A., Topkarcı Z., Gür E.E., Erdoğan B., Yemişçi A. Pigmented fungiform papillae of the tongue: co-existence of two patterns in the same patient and associated dental pigmentation. Turkderm Turk Arch Dermatol Venereol. 2021;55(1):45–47. [Google Scholar]
- 28.Castellanos M.A., Echeverria A.E.B., Rosas G.M.A. Dermatoscopía en la pigmentación de papilas fungiformes de la lengua. Dermatol Cosmet Med Quir. 2018;16(3):206–207. [Google Scholar]
- 29.Özaslan M. Barwnikowe brodawki grzybowate języka. Dermatol Rev [Internet]. 2021;108(6):550–553. https://www.termedia.pl/doi/10.5114/dr.2021.114609 Available from: [Google Scholar]
- 30.Rice S.M., Lal K. Successful treatment of pigmented fungiform papillae of the tongue with Q-switched ruby laser. Dermatol Surg [Internet]. 2022 Mar;48(3):368–369. doi: 10.1097/DSS.0000000000003371. https://journals.lww.com/10.1097/DSS.0000000000003371 Available from: [DOI] [PubMed] [Google Scholar]
- 31.Sil A., Panigrahi A., Bhanja D. Rose petal appearance: the dermoscopic finding in pigmented fungiform papillae of the tongue. Indian Dermatol Online J [Internet]. 2021;12(3):490–491. doi: 10.4103/idoj.IDOJ_589_19. http://www.idoj.in/text.asp?2021/12/3/490/295470 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Piquero-Casals J., Morgado-Carrasco D. Pigmented fungiform lingual papillae. J Pediatr. 2020 Sep;224(September):177–178. doi: 10.1016/j.jpeds.2020.06.001. [DOI] [PubMed] [Google Scholar]
- 33.Pehoushek J.F., Norton S.A. Black taste buds. Arch Fam Med. 2000;9(3):219–220. [Google Scholar]
- 34.Belysheva T.S., Vishnevskaya Ya v., Kletskaya I.S., Michenko A.V., Volkova A.S., Valiev T.T., et al. Problems of clinical and morphologic diagnosis of orolabial melanosis in children. Russ J Pediatr Hematol Oncol [Internet]. 2021 Oct 19;8(3):116–122. https://journal.nodgo.org/jour/article/view/751 Available from: [Google Scholar]
- 35.Ogrum A., Takci Z., Yildiz Seckin H. Pigmented fungiform papillae: case report and review of the literature. Turk Klinikleri J Dermatol. 2018;28(1):32–34. [Google Scholar]
- 36.Robles-Mendez J.C., Ayala-Cortes A.S., Villarreal-Martinez A., Ocampo-Candiani J. Dermoscopy of the pigmented fungiform papillae of the tongue. J Dermatol. 2017;76(4):s40–s42. doi: 10.1016/j.jaad.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 37.Mizawa M., Makino T., Furukawa F., Torai R., Shimizu T. Efficacy of Q-switched ruby laser treatment for pigmented fungiform papillae of the tongue. J Dermatol [Internet]. 2022 Apr;49(4) doi: 10.1111/1346-8138.16270. https://onlinelibrary.wiley.com/doi/10.1111/1346-8138.16270 Available from: [DOI] [PubMed] [Google Scholar]
- 38.Chamseddin B., Vandergriff T. Pigmented fungiform papillae of the tongue: a clinical and histologic description. Dermatol Online J. 2019;25(9):1–3. [PubMed] [Google Scholar]
- 39.Maxim E., Dtefano D. de. Pigmented fungiform papillae of the tongue: an incidental finding in a patient with mycosis fungoides. J Am Acad Dermatol. 2018;79(3) [Google Scholar]
- 40.Sharma S.S., Sharma S.S. Pigmentation of the fungiform papillae of the tongue in a child secondary to iron deficiency anaemia: an uncommon occurrence and association. Int J Oral Health Dent. 2016;2(1):39–42. [Google Scholar]
- 41.Sugiyama Y., Hayashi K., Takayama T. Pigmented fungiform papillae of the tongue in a Japanese child. Clin Case Rep [Internet]. 2020 Jun 12;8(6):1104–1106. doi: 10.1002/ccr3.2830. https://onlinelibrary.wiley.com/doi/abs/10.1002/ccr3.2830 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garzón-Rivas V., Garzón-Aldás E. Papilas Fungiformes Pigmentadas de la Lengua. Características Clínicas, Histológicas y Dermatoscópicas de una Serie de Casos Ecuatorianos. Int J Odontostomatol. 2019 Dec;13(4):446–451. [Google Scholar]
- 43.Docx M.K.F., Vandenberghe P., Govaert P. Pigmented fungiform papillae of the tongue (PFPT) Acta Clin Belg. 2016;71(2):117–118. doi: 10.1179/2295333715Y.0000000067. [DOI] [PubMed] [Google Scholar]
- 44.Verma B., Bahra A., Ajmal A.K.M., Sen S. Laugier–hunziker syndrome in a young female. Indian Dermatol Online J. 2017;8:148–150. doi: 10.4103/2229-5178.202282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bugălă N.M., Carsote M., Stoica L.E., Albulescu D.M., Ţuculină M.J., Preda S.A., et al. New approach to Addison disease: oral manifestations due to endocrine dysfunction and comorbidity burden. Diagnostics [Internet]. 2022 Aug 28;12(9):2080. doi: 10.3390/diagnostics12092080. https://www.mdpi.com/2075-4418/12/9/2080 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available on request to Meircurius-2015@fkg.unair.ac.id (MDCS).